Abstract
The aim of our study was to investigate whether self-reported feeling of loneliness (FoL) and COVID-19-specific health anxiety were associated with the presence of depressive symptoms during the first coronavirus disease 2019 (COVID-19) wave. Questionnaires of 603 persons of the Swiss Multiple Sclerosis Registry (SMSR) were cross-sectionally analyzed using descriptive and multivariable regression methods. The survey response rate was 63.9%. Depressive symptoms were assessed by the Beck Depression Inventory-Fast Screen (BDI-FS). COVID-19-specific health anxiety and FoL were measured using two 5-item Likert scaled pertinent questions. High scoring FoL (2.52, 95% confidence interval (CI) (2.06—2.98)) and/or COVID-19 specific health anxiety (1.36, 95% CI (0.87–1.85)) were significantly associated with depressive symptoms. Further stratification analysis showed that the impact of FoL on depressive symptoms affected all age groups. However, it was more pronounced in younger PwMS, whereas an impact of COVID-19 specific health anxiety on depressive symptoms was particularly observed in middle-aged PwMS. FoL and COVID-19-specific health anxiety were age-dependently associated with depressive symptoms during the first COVID-19 wave in Switzerland. Our findings could guide physicians, health authorities, and self-help groups to better accompany PwMS in times of public health crises.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is an ongoing major global health concern. For the first time in this century, mandatory public health interventions were broadly introduced by governments in many countries, including Switzerland, to control the pandemic during the first COVID-19 wave in spring 20201. These governmental interventions, like limiting social gatherings and travel, wearing facemasks, as well as complete lockdowns including inter alia strict stay at home, work from home advice, closure of all shops except grocery stores, closure of universities, schools and nursery schools and restriction of social contacts, had a major disruptive impact on daily life. Concurrently, a public discussion regarding limited health care resources and the need for triage ensued. This increased the uncertainty of getting access to possible limited intensive care unit capacities in populations with chronic diseases affecting the central nervous system, such as in persons with multiple sclerosis (PwMS), as definitions include inter alia “Severe and irreversible neurological event or condition” without giving a strict definition thus leaving room for speculations2.
Despite the unquestionable need for such restrictions, the impact of these measures on depressive symptoms and mental health, and the association of COVID-19 specific health anxiety and feeling of loneliness (FoL) with depressive symptoms are still unclear. A cross-sectional study prior to the pandemic based on self-reports found a significantly higher FoL in PwMS compared to healthy controls without MS3. Further, the degree of loneliness positively correlated with depressive symptoms3. In a recent analysis published by the UK MS Register, PwMS were also more likely to feel lonelier compared to healthy controls. FoL occurred more frequently in PwMS with anxiety and depression compared to those PwMS without. However, the levels of anxiety and depression did not change between the period during the COVID-19 outbreak compared to the previous year4. Moreover, general health anxiety was more frequently observed in PwMS5 and, if present, had a negative impact on “experienced disability” and generalized anxiety5. The effect of general health anxiety on health-related quality of life appears to be independent of physical disability in persons with relapsing remitting MS6, who were more afraid of relapses7. The UK MS Register study implemented the “General Anxiety Disorder-7 (GAD-7) Scale” to assess health anxiety of PwMS during the COVID-19 outbreak4, but data specifically targeting health anxiety related to infection with SARS-CoV-2 during the COVID-19 pandemic were and are still lacking.
Based on our registry data, we aimed to assess the association between FoL and COVID-19 specific health anxiety and depressive symptoms during the first COVID-19 wave. We hypothesized that high scores of both FoL and COVID-19 specific health anxiety would be associated with more severe depressive symptoms, and potentially even trigger them.
Methods
Sample
Study type and response rate
Our study reports on the results of a survey research investigating depressive symptoms of PwMS during the first COVID-19 wave in Switzerland. This wave led to a national lockdown. Our study was nested in the ongoing Swiss Multiple Sclerosis Registry (SMSR)8,9. Participants of the SMSR had the opportunity to either fill in a one-time survey or additionally complete regular, semi-annual surveys with varying topics, such as the COVID-19 survey. Invitations for the online survey were sent out on April 8, 2020 and the data collection for the current sample was closed on June 8, 2020. In total, 1759 invitations were sent out via the SMSR platform. Of the active participants of the SMSR (n = 1014), defined as active participation within the last 12 months, a response rate of 63.9% was achieved.
Data Source, study population and ethical approval
The SMSR, previously described elsewhere8,9, is a Swiss-based, patient-centered, longitudinal observational study initiated and financially supported by the Swiss MS Society (http://www.ClinicalTrials.gov; identifier: NCT02980640) and operated by the University of Zurich. Study recruitment started in June 2016. Persons aged 18 years and older with a diagnosis of clinically isolated syndrome or any type of MS (including relapsing remitting MS, primary progressive MS and secondary progressive MS) who are treated in Switzerland can participate after providing their informed consent and validation of the MS diagnosis by their treating physician. All questionnaires are self-completed either online or as paper–pencil questionnaires. The Ethics Committee of the Canton of Zurich approved the SMSR (No. PB-2016–00894). All assessments and analysis were performed in accordance with relevant guidelines and regulations.
Measures
Assessment of the main outcome variable depressive symptoms during the first COVID-19 wave
Depressive symptoms were assessed using the 7-item Beck Depression Inventory-Fast Screen Index (BDI)-FS10. The BDI-FS is a self-reported questionnaire containing the following seven subscales: (I) sadness, (II) pessimism, (III) past failure, (IV) self-dislike, (V) self-criticalness, (VI) suicidal thoughts or wishes, and (VII) loss of interest. Each item can be scored from 0 (absent) to 3 (severe) leading to a final score ranging from 0 to 21. The presence of clinically relevant depressive symptoms was assumed if the BDI-FS sum score was ≥ 4 points, indicative of at least mild depressive symptoms10.
Assessment of COVID-19 specific health anxiety and feeling of loneliness during the COVID-19 lockdown and patient related variables
Loneliness and COVID-19 specific health anxiety were each evaluated using pertinent statements that were arranged on a 5-items Likert scale (1: none—5: very severe). The wording of the questions on feelings of loneliness and COVID-19 specific health anxiety was: “How lonely do you feel at the moment?” and “How much do you currently suffer from a fear of having a serious disease (such as coronavirus) in addition to MS, without it already having been diagnosed by a physician?”. Loneliness and COVID-19 specific health anxiety were dichotomized using the cut-off ≥ 3 for defining feeling of loneliness or COVID-19 specific health anxiety, respectively. The cut-off of three was used to ensure that all patients with any feeling of loneliness or COVID-19 specific health anxiety were classified as such in our analysis. This should prevent a selection of extreme phenotypes. The variable age (categorized intro three classes: ≤ 35 years; 36—59 years; ≥ 60 years) was used for stratified analyses. Age and sex were considered as confounder variables in multivariable models.
Statistical analysis
Continuous variables were presented as means (± 95% confidence interval, 95% CI) or medians (25th/75th percentile) according to the scale of measurement. Categorical variables were reported as frequencies. Comparative statistics were performed using the Mann–Whitney test (MWT) for continuous variables or Chi2 test for categorical variables. We ran a first multivariable regression model with BDI-FS scores as the dependent variable and sex, age, FoL group, and COVID-19 specific health anxiety as independent variables. A second multivariable regression model was run separately for the age groups ≤ 35 years, 36–59 years, and ≥ 60 years, respectively. Furthermore within the same set of variables we run a multivariable logistic regression model with BDI-FS dichotomized (BDI-FS < 4 vs. ≥ 4 points).
Ethics approval and consent to participate
The Ethics Committee of the Canton of Zurich approved the SMSR (No. PB-2016-00894).
Results
Study population
In total, 847 PwMS responded to the survey. This survey included both PwMS only participating in this single survey and PwMS, who additionally had taken part in the longitudinal surveys. We focused only on those COVID-19 survey responders with any prior survey participation (that is, before the pandemic) in the SMSR in 2019 (n = 648) as the actual situation might have influenced the response rate of the survey. Of those, n = 603 had complete data sets in all variables needed for the main regression analysis. The mean age was 49.22 years with a female preponderance (70.80%, Table 1).
Feeling of loneliness and COVID-19-specific health anxiety
FoL, defined as a score ≥ 3 points, was present in 134/603 (22.20%) of the survey participants (Table 1). Severity of depressive symptoms was significantly higher in persons with FoL (mean (95% CI, n): 4.10 (3.46–4.74, 134) compared to those without FoL: 1.40 (1.24–1.56, 469, MWT p-value < 0.001). At least mild depressive symptoms (BDI-FS cut off: ≥ 4 points) were significantly more frequent in PwMS who felt lonely (59/134 (44.03%)) compared to those who did not (61/469 (13.00%), Chi2 p-value < 0.001; data not tabulated).
COVID-19-specific health anxiety, defined as a score ≥ 3 points, was reported by 113/603 (18.70%; Table 1). Severity of depressive symptoms (mean BDI-FS score (95% CI, n) was higher among PwMS with COVID-19 specific health anxiety 3.52 (2.86—4.18, 113) compared to those without anxiety: 1.65 (1.45–1.85, 490, MWT p-value < 0.001). Similarly, at least mild depressive symptoms (BDI-FS cut off: ≥ 4 points) were more frequent in PwMS with COVID-19-specific health anxiety (44/113 (38.94%) compared to those without anxiety 76/414 (18.36%, Chi2 p-value < 0.001; data not tabulated).
Depressive symptoms
During the first COVID-19 wave, 120/603 (19.90%) reported at least mild depressive symptoms with a homogeneous distribution within the seven subscales of the BDI-FS questionnaire (Table 1). BDI-FS scores increased in parallel with the FoL (Pearson correlation coefficient 0.51, p < 0.001, n = 603) and COVID-19-specific health anxiety (Pearson correlation coefficient 0.33, p < 0.001, n = 603; data not tabulated).
Associations of feeling of loneliness and COVID-19-specific health anxiety with depressive symptoms during the first COVID-19 wave
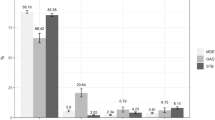
Multivariable regression analysis with BDI-FS scores as the dependent variable was run within the sample of PwMS (n = 603), showing that FoL (2.52 (2.06—2.98, (p < 0.001)) and COVID-19-specific health anxiety (1.36 (0.87–1.85, (p < 0.001)) were independently associated with higher BDI-FS scores during the first COVID-19 wave. Stratifying the analysis by age groups demonstrated that a significant effect of FoL was present in all age groups but stronger in PwMS with younger age (≤ 35 years), whereas the effect of COVID-19-specific health anxiety remained only significant in PwMS aged 36–59 years (Table 2).
Discussion
Our cross-sectional study investigated the associations of self-reported FoL and COVID-19-specific health anxiety with the presence of depressive symptoms during the first COVID-19 wave in a large registry sample of PwMS in Switzerland. We observed a robust association between high FoL scores and depressive symptoms, which was present in all age groups. A higher COVID-19-specific health anxiety in association with depressive symptoms might have an association with age as it was present in the middle aged group (36–59 years of age), which remains present also using 10-steps age categories (supplementary Table 1).
This study on PwMS during the first COVID-19 wave revealed an unfavorable association between the occurrence of FoL and depressive symptoms. Similarly, in a population study based on a nationally representative socioeconomic panel, the risk for FoL was nonlinearly distributed across age with elevated levels among young adults, but also among the oldest (> 86 years) of their sample11. This unfavorable effect for the young age group was explained elsewhere by less stable and committed relationships, typically characterizing this life span12. The FoL in very high age groups, on the contrary, might be reinforced by a higher occurrence of losing loved ones and difficulties in making new interpersonal contacts due to increased disability11. While our study sample of PwMS did not contain participants older than 84 years, we could not deduce viable conclusions pertaining to this age group. However, the explanation of less stable relationships could possibly also apply to our younger age group of PwMS. Indeed, the negative consequences of less stable relationships might have become more serious during the COVID-19 lockdown due to restrictions resulting in reduced personal contacts and group activities, canceled appointments, and working from home, leading to a drastic limitation in interpersonal exchanges. This assumption is further corroborated by recent COVID-19-specific research examining mental health in the general population.
A systematic review found that belonging to a younger age group (≤ 40 years) was a relevant risk factor for chronic / psychiatric illness during the COVID-19 pandemic12. This was partly explained by stressful situations related to the COVID-19 outbreak resulting in disproportional psychosocial burden for this age group: job loss, unpredictability, distress due to cancellation of social events, online courses, postponements of exams, detachment from peer groups and family-related care duties, especially applicable to women, were listed as possible examples13. However, further COVID-19-specific studies on PwMS confirmed that depressive symptoms were more severe in this group compared to matched controls without MS14.
Interestingly, the associations between COVID-19-specific health anxiety and depressive symptoms were only statistically significant in the middle-age group in our study. This might imply differential vulnerabilities depending on specific stages of life. The threat of getting infected with the virus may be of particular significance, especially if there is a danger of losing loved ones and/or suffering professional disadvantages. Interestingly, a previous study on PwMS in the pre COVID-19 era demonstrated that health anxiety was linked to younger age at onset, shorter time since MS diagnosis, and strongly related to social support15, which might reflect the diagnosis of a chronic neurological disease. Results cannot be directly compared as the latter study was carried out before the COVID-19 pandemic phase and thus not assessed COVID-19-specific health anxiety as we did. In the general population, younger age was also associated with higher COVID-19 anxiety. Although the reasons for these particular age differences are still to be clarified16 our study may add further evidence that the age distribution of loneliness might follow a bimodal distribution, while COVID-19-specific anxiety might represent an inverted U-shape distribution, showing its climax in the middle age.
Our study has several limitations. First, since our study did not consider a history of psychiatric disorders, we cannot exclude that our findings may be influenced by pre-existing vulnerabilities, since it is known that persons with psychiatric disorders are more prone to depression during the COVID-19 pandemic as seen in both PwMS17 and the general population18. Also, pre-existing generalized anxiety disorder was not assessed, despite the robust evidence of its comorbidity with depression19,20. Therefore, the association between COVID-19-specific anxiety and depressive symptoms could also be a result of these co-occurring disorders, and MS or COVID-19 specific statements cannot be drawn. Second, this was a cross-sectional study, limiting causal inferences. In addition, the complex inter-relations between FoL, COVID-19-specific anxiety, and depressive symptoms were also not considered and therefore some interactive effects could not be fully disentangled by our study design. In particular, a circularity of FoL might have been present. However, as FoL has been established as relevant risk factor of depression in pooled data21, the overlap does not exclude associations. Further both scales used for evaluation of FoL and COVID-19-specific health anxiety as well as the cut-off of ≥ 3 points on the corresponding Likert-scales have not been validated before, which should be taken into account while interpreting our data. Furthermore, the age stratification has to be highlighted which was mainly based on group sizes and run in two different settings to mutually validate each other. Moreover, in this regards we are adhering to open data policy and are willing to share our data set with others upon reasonable request.
Further, as social support and self-perceived loneliness are interrelated, it is likely that persons lacking social support also experience high levels of FoL22,23. The same holds for certain socio-demographic variables, such as education and civil status, which were excluded as they could change over time and were not available for all PwMS at the time of the first COVID-19 wave. Finally, we could neither determine whether the results differed from the year before the pandemic outbreak nor whether they were COVID-19- or MS-specific, as this appears to be the case in the general population. A healthy control group would be required to answer this latter question, which is not within the scope of the SMSR.
Conclusions
Our findings on PwMS indicate that FoL and COVID-19-specific health anxiety might be age-dependent factors associated with depressive symptoms during the first COVID-19 wave in Switzerland. Even though our cross-sectional data do not allow causal conclusions for the development of depression, it seems plausible that FoL and COVID-19-specific health anxiety might be associated with depressive symptoms and might represent targets for interventions. Hence, these differential vulnerabilities depending on specific periods of life require particular consideration regarding the needs of these subgroups of PwMS. As a consequence, while the focus of support for younger PwMS should be on maintaining social contacts, more emphasis must be placed on information about COVID-19-related health issues, to prevent affective disturbances emerging from lockdown-constraints in older subjects.
Additional studies focusing on age-dependent needs of PwMS are required to better prevent and treat depression in PwMS. These findings could be of specific interest for physicians, health authorities, and self-help groups to advance the support of PwMS during public health crises.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Brauner, J. M. et al. Inferring the effectiveness of government interventions against COVID-19. Science 371(6531), eabd9338 (2021).
Scheidegger, D., Fumeaux, T., Hurst, S. & Salathe, M. COVID-19 pandemic: Triage for intensive-care treatment under resource scarcity. Swiss Med. Wkly 150, 20229 (2020).
Balto, J. M., Pilutti, L. A. & Motl, R. W. Loneliness in multiple sclerosis: Possible antecedents and correlates. Rehabil. Nurs. 44(1), 52–59 (2019).
Garjani, A. et al. Mental health of people with multiple sclerosis during the COVID-19 outbreak: A prospective cohort and cross-sectional case-control study of the UK MS register. Mult. Scler. J. https://doi.org/10.1177/13524585211020435 (2021).
Kehler, M. D. & Hadjistavropoulos, H. D. Is health anxiety a significant problem for individuals with multiple sclerosis?. J. Behav. Med. 32(2), 150–161 (2009).
Hayter, A. L., Salkovskis, P. M., Silber, E. & Morris, R. G. The impact of health anxiety in patients with relapsing remitting multiple sclerosis: Misperception, misattribution and quality of life. Br. J. Clin. Psychol. 55(4), 371–386 (2016).
Khatibi, A., Weiland, T. J. & Dehghani, M. Fear of relapse in patients suffering from RRMS influence their quality of life. Mult. Scler. Relat. Disord. 54, 103137 (2021).
Puhan, M. A. et al. A digitally facilitated citizen-science driven approach accelerates participant recruitment and increases study population diversity. Swiss Med. Wkly. 148, w14623 (2018).
Steinemann, N. et al. The Swiss Multiple Sclerosis Registry (SMSR): Study protocol of a participatory, nationwide registry to promote epidemiological and patient-centered MS research. BMC Neurol. 18(1), 111 (2018).
Beck RAS, A.T., Brown, G.K. BDI—Fast Screen for Medical Patients Manual. The Psychological Corporation (2000).
Luhmann, M. & Hawkley, L. C. Age differences in loneliness from late adolescence to oldest old age. Dev. Psychol. 52(6), 943–959 (2016).
Xiong, J. et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 277, 55–64 (2020).
Cao, W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287, 112934 (2020).
Costabile, T. et al. COVID-19 pandemic and mental distress in multiple sclerosis: Implications for clinical management. Eur. J. Neurol. 28(10), 3375–3383 (2021).
Hanna, M. & Strober, L. B. Anxiety and depression in Multiple Sclerosis (MS): Antecedents, consequences and differential impact on well-being and quality of life. Mult. Scler. Relat. Disord. 44, 102261 (2020).
Lee, S. A. Coronavirus anxiety scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 44(7), 393–401 (2020).
Ramezani, N. et al. Fear and anxiety in patients with multiple sclerosis during COVID-19 pandemic; report of an Iranian population. Mult. Scler. Relat. Disord. 50, 102798 (2021).
Vindegaard, N. & Benros, M. E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 89, 531–542 (2020).
Moffitt, T. E. et al. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch. Gen. Psychiatry 64(6), 651–660 (2007).
Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R. & Walters, E. E. Prevalence, severity and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62(6), 617–627 (2005).
Solmi, M. et al. Factors associated with loneliness: An umbrella review of observational studies. J. Affect. Disord. 271, 131–138 (2020).
Bareket-Bojmel, L., Shahar, G., Abu-Kaf, S. & Margalit, M. Perceived social support, loneliness and hope during the COVID-19 Pandemic: Testing a mediating model in the UK, USA and Israel. Br. J. Clin. Psychol. 60(2), 133–148 (2021).
Grey, I. et al. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 293, 113452 (2020).
Acknowledgements
The authors wish to thank the Swiss Multiple Sclerosis Society for funding the Swiss MS Registry (SMSR). Moreover, we thank the study participants who not only contributed data but were also absolutely instrumental in all aspects of study design and conduct of the Swiss Multiple Sclerosis Registry. We further thank the members of the SMSR Data Centre at the Epidemiology, Biostatistics & Prevention Institute of the University of Zurich. The members of the SMSR are Bernd Anderseck, Pasquale Calabrese, Andrew Chan, Claudio Gobbi, Roger Häussler, Christian P. Kamm, Jürg Kesselring (President), Jens Kuhle (Chair of Clinical and Laboratory Research Committee), Roland Kurmann, Christoph Lotter, Marc Lutz, Kurt Luyckx, Patricia Monin, Stefanie Müller, Krassen Nedeltchev, Caroline Pot, Milo A. Puhan, Irene Rapold, Anke Salmen, Klaas Enno Stephan, Zina-Mary Manjaly, Claude Vaney (Chair of the Patient and Population Research Committee), Viktor von Wyl (Chair of the IT and Data Committee) and Chiara Zecca. The Swiss MS Registry is supported by the scientific advisory board of the Swiss MS Society.
Funding
This work was funded by the Swiss Multiple Sclerosis Society.
Author information
Authors and Affiliations
Contributions
Conceptualization, R.H., K.S., S.W., V.V.W., S.R.; methodology, R.H.; writing—original draft preparation, R.H., S.R., K.S., N.S., S.W., V.V.W.; writing—review and editing, N.S., C.H., P.C., Z.-M.M., A.S., J.K., C.Z., C.G., M.A.P., S.W., V.V.W. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Robert Hoepner received speaker/advisor honorary from Merck, Novartis, Roche, Biogen, Alexion, Sanofi, Janssen, Bristol-Myers Squibb, and Almirall. He received research support within the last 5 years from Roche, Merck, Sanofi, Biogen, Chiesi, and Bristol-Myers Squibb. He also received research grants from the Swiss MS Society und is a member of the Advisory Board of the Swiss MS Society. He also serves as associated editor for Journal of Central Nervous System disease. All conflicts are not related to this work. Stephanie Rodgers was funded by a grant from the Hartmann–Müller Foundation. Ente Ospedaliero Cantonale (employer) received compensation for Chiara Zecca’s speaking activities, consulting fees, or research grants from Abbvie, Almirall, Biogen Idec, Bristol Meyer Squibb, Genzyme, Lundbeck, Merck, Novartis, Teva Pharma, Roche. Ente Ospedaliero Cantonale (employer) received compensation for Claudio Gobbi’s speaking activities, consulting fees, or research grants from Abbvie, Almirall, Biogen Idec, Bristol Meyer Squibb, Genzyme, Lundbeck, Merck, Novartis, Teva Pharma, Roche. Sebastian Walther received honoraria from Lundbeck, Mepha, and Neurolite in the past 3 years for scientific talks in educational activities; all unrelated to this work. Katharina Stegmayer, Nina Steinemann, Christina Haag, Pasquale Calabrese, Zina-Mary Manjaly, Jürg Kesselring, Milo A. Puhan, and Viktor von Wyl declare no conflicts of interest. Salmen A received speaker honoraria and/or travel compensation for activities with Bristol Myers Squibb, Novartis, and Roche, and research support by Baasch Medicus Foundation and the Swiss MS Society. She serves on the Editorial Board of Frontiers in Neurology—Multiple Sclerosis and Neuroimmunology. All not related to this work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoepner, R., Rodgers, S., Stegmayer, K. et al. Feelings of loneliness, COVID-19-specific-health anxiety and depressive symptoms during the first COVID-19 wave in Swiss persons with multiple sclerosis. Sci Rep 12, 17829 (2022). https://doi.org/10.1038/s41598-022-22445-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22445-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.