Abstract
We compared the efficacy of tocilizumab and etanercept in inhibiting radiographic progression of joint destruction in rheumatoid arthritis. Overall, 187 patients treated with etanercept or tocilizumab were selected. To adjust for baseline patient characteristics between the tocilizumab and etanercept treatment groups, a propensity score matching was performed. Radiographic progression of joint destruction was compared between patients treated with tocilizumab or etanercept. Clinical disease activity index (CDAI) and modified health assessment questionnaire (mHAQ) scores at the administration of biologic treatment and after 12 months of tocilizumab and etanercept therapy were measured and compared to radiographical parameters between the groups. Levels of C-reactive protein (CRP), matrix metalloproteinase-3 (MMP-3), CDAI, and mHAQ scores improved after 12 months of treatment in the two groups. Proportion of patients with no Sharp erosion score progression was significantly higher with tocilizumab treatment than with etanercept treatment (p = 0.032). Multivariate analysis demonstrated that Sharp erosion score was significantly associated with baseline CDAI (odds ratio, 1.05; 95% confidence interval, 1.003–1.099, p = 0.037). Tocilizumab treatment suppressed joint erosion progression compared to etanercept, and the progression correlated with baseline CDAI.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is an autoimmune disease characterised by chronic inflammation of the synovial lining of the joint1 and is characterized by progressive joint destruction and systemic complications2. Radiographic damage is one of the most critical outcomes of RA, and effective therapy reduces the progression of joint destruction3. The destruction of joints is due to overproduction of pro-inflammatory cytokines, including tumour necrosis factor-alpha (TNF-α), interleukins (IL) -6 and -17, and macrophage colony-stimulating factor (GM-CSF) from immune cells in the synovium4. The drugs that inhibit cytokine productions have been investigated as possible treatments to halt the progression of joint destruction in RA5.
IL-6 plays a significant role in the pathogenesis of RA and disease activity6. The expression of serum IL-6 and IL-6 receptor is correlated with inflammation, clinical signs and symptoms, and radiographic signs of joint destruction7,8. IL-6 affects the function of neutrophils, T cells, B cells, monocytes, and osteoclasts, which are highly activated in RA. IL-6 also affects the hepatic acute phase response, which is a key feature of RA9. As a key regulator in osteoclast differentiation, IL-6 may promote erosive joint changes by activating osteoclast formation and accelerating bone resorption8. Several clinical studies have demonstrated that tocilizumab treatment (IL-6 inhibitor) is effective in inhibiting bone erosion10,11,12,13,14. The SAMURAI study reported that tocilizumab treatment is more effective in preventing the progression of bone erosion than conventional treatment with disease-modifying antirheumatic drugs (DMARDs); however, no significant difference in joint space narrowing (JSN) was observed between the two groups at 28 weeks10. The FUNCTION study reported that methotrexate (MTX)-only treatment caused greater progression of bone erosion than treatment with tocilizumab and MTX, but no significant difference in JSN was observed at 52 weeks12,13. Hashimoto and colleagues also reported that tocilizumab monotherapy was more effective in reducing radiographical progression of bone erosion in patients presenting with risk factors for rapid joint destruction14.
TNF inhibitors also play a role in the inhibition of radiographic progression of joint destruction15,16. TNF-α induces the secretion of multiple proinflammatory cytokines such as IL-1, -6, and -8; GCS-F; and dickkopf (DKK)-1, which regulate the Wnt pathway17,18. Previous reports showed that TNF inhibitors decrease serum DKK-1 levels in patients with RA18, and DKK-1 levels correlated with extent of the radiographic joint destruction19. Therefore, it is important to understand the role of Wnt pathway molecules including DKK-1 and sclerostin; however, data on the in vivo effect of TNF-α inhibitor on bone loss in patients with RA are limited20,21. The TEMPO study reported that mean changes in radiographic progression were significantly lower for patients receiving a combination of etanercept and MTX or etanercept monotherapy than for those receiving MTX monotherapy15. Mean changes from baseline in erosion scores of modified total Sharp score (mTSS) for the combination and etanercept groups were significantly lower than those in the MTX group; however, the significance of this finding has not been analysed15. These reports indicate that the IL-6 inhibitor or the TNF inhibitor reduced radiographic progression of joint destruction. However, none of the studies have compared the inhibitory effect of the IL-6 inhibitor and TNF inhibitor on the radiographic progression of joint destruction. Tocilizumab and etanercept are commonly used in the treatment of RA as biological drugs for inhibition of IL-6 and TNF, respectively22,23.
Therefore, the present study aimed to compare the efficacy of tocilizumab and etanercept in inhibiting the radiographic progression of joint destruction.
Materials and Methods
Ethics statement and patient consent
This study complies with the Declaration of Helsinki, and study protocols were approved by the ethics committee of the Research Institute of Joint Disease Kobe and Kobe University Graduate School of Medicine. All participants provided informed consent for participation.
Patient selection
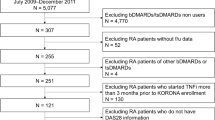
This was a retrospective cohort study. Medical records of 202 patients with RA who were treated with a TNF inhibitor (etanercept) or an IL-6 inhibitor (tocilizumab) at Matsubara Mayflower Hospital and Kobe University Hospital between October 2004 and September 2020 were analysed. All patients included in the study were qualified according to the 1987 American College of Rheumatology RA criteria24. Only patients who were treated with etanercept (96 patients) or tocilizumab (121 patients) for at least 12 months were included in this study. However, patients who had a treatment overlap between etanercept and tocilizumab were excluded. Finally, 187 patients were included and were divided into two groups with etanercept treatment (81 patients) or tocilizumab treatment (106 patients).
Clinical evaluation
Data were collected on variables such as age, duration of RA, MTX dose (mg/week), glucocorticoid dose (mg/day), C-reactive protein (CRP) level, and matrix metalloproteinase-3 (MMP-3) at the time of introduction of the tocilizumab or etanercept therapy. The duration of RA was determined between the time of RA diagnosis and administration of tocilizumab or etanercept. Data of mHAQ25 and CDAI26 were obtained as clinical outcomes at the initiation of treatment and after 12 months of tocilizumab or etanercept therapy.
Radiographic evaluation
The x-rays were taken at the start of the drug treatment and also after 12 months. Radiographs of the hands and feet were assessed according to the Sharp method27. The scores for 187 radiographs (from 187 patients) were determined by two experienced rheumatologists who were blinded to the clinical data. Sixteen and six areas were considered for assessing erosions and JSN for the hands and feet, respectively. The maximum erosion score of the hands and wrists was 160 and that of the feet was 120 (maximum total erosion score: 280). Accordingly, the maximum JSN score of the hands and wrists was 120 and that of the feet was 48 (maximum total JSN score: 168). The sum of the erosion and JSN scores was calculated as the total Sharp/van der Heijde score (mTSS) (maximum: 448)28. The average score of the readings was used as the radiographic score. The proportion of patients showing no radiographic progression was determined using thresholds set at changing from the baseline mTSS (delta mTSS), changing from the baseline Sharp erosion score (delta Sharp erosion score), or changing from the baseline Sharp JSN score (delta JSN) ≤ 0, ≤ 0.5, and ≤ the smallest detectable change (SDC). The SDC values at each timepoint were estimated with the SD of the differences between delta mTSS, delta erosion, or delta JSN assigned by the two blinded image assessors29.
Propensity score‑matched analysis
To adjust for baseline patient characteristics between the tocilizumab and etanercept treatment groups, a propensity score matching was performed30. Propensity scores were calculated from logistic regression models. In the present study, patient characteristics data (sex, age, RA duration, CDAI, mHAQ, first bDMARDs or more, CRP levels, MTX dose, and glucocorticoid dose) and radiographic scores (Total Sharp score) at biological drug administration were used to calculate a propensity score; matching of one patient with tocilizumab treatment to another patient with etanercept treatment with the same propensity score was performed. The pairing was achieved with the caliper tolerance of 20% of standard deviation of propensity score, and a random selection was made among the patients with the same propensity score. Finally, 38 pairs of patients were matched in two groups. The patient characteristics before and after propensity matching are shown in Table 1.
Statistical analysis
Demographic and clinical characteristics of patients treated with tocilizumab or etanercept are provided in Tables 1, 2, 3, 4, and 5. All data are expressed as mean ± standard deviation unless otherwise indicated. Patients' background characteristics and radiographic progression between the two groups were compared using Mann–Whitney U test and paired t-test before and after propensity matching, respectively (Table 1). To assess the improvement in laboratory parameters (CRP levels and MMP-3) and clinical scores (mHAQ and CDAI), we compared values at biological drug administration and those after 12 months using paired t-test (Table 2). In addition, to assess the radiographic progression and risk factor of Sharp erosion score progression for treatment with tocilizumab and etanercept, Fisher’s exact test for nominal variables were performed (Tables 3 and 5). Correlations between clinical parameters and Sharp erosion score progression were analyzed using Pearson’s correlation value (Tables 4). Additionally, we performed a multivariate analysis to test the association between CDAI, mHAQ, or treatment with tocilizumab or etanercept and radiographic progression of Sharp erosion score (Table 6). Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for multivariate analysis. Data were analysed using SPSS, version 19 J (IBM Japan, Tokyo, Japan).
Results
Treatment with biological drugs improved laboratory parameters and clinical outcomes
Laboratory data and clinical outcomes of our study are provided in Table 2. Treatment with etanercept or tocilizumab for 12 months significantly improved laboratory data (CRP levels and MMP-3) and clinical outcomes (mHAQ and CDAI) in both treatment groups (Table 2).
Radiographic progression was different between etanercept and tocilizumab treatment group
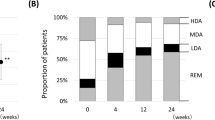
Radiographic progression in structural joint damage was evaluated using cumulative distribution of mTSS, Sharp erosion score, and Sharp joint space narrow score change from baseline to 12 months after drug administration (Fig. 1). A proportion of patients with no radiographic progression defined by delta mTSS (delta mTSS), delta Sharp JSN (delta JSN), and delta Sharp erosion score (delta erosion) are shown in Table 3. Significant differences in progression for Sharp erosion score using thresholds of delta erosion ≤ 0, ≤ 0.5, and ≤ SDC were found between the tocilizumab and etanercept groups (Table 3). However, no significant difference was found in progression based on delta mTSS and delta JSN (Table 3).
Predictive factors for radiographic progression of erosion for treatment with biological drugs
We have analyzed the predictive factors including age, RA duration, baseline CRP, MMP-3, CDAI, mHAQ, glucocorticoid dose, first biological drug or more, etanercept or tocilizumab treatment, and sex of patients in relation with the progression of Sharp erosion score (Tables 4 and 5). The baseline CDAI and mHAQ were significantly correlated with delta erosion (Table 4), and the proportion of patients with delta erosion differed significantly in the etanercept or tocilizumab treatment groups (Table 5). Predictive factors may be dependent on multiple confounders. Therefore, the significant predictive factors detected by univariate analysis (baseline CDAI, mHAQ, and treatment with etanercept or tocilizumab) were used as covariates for multivariate analysis. We demonstrated that the radiographic delta erosion was significantly associated with baseline CDAI (OR, 1.05; 95% CI, 1.003–1.099, p = 0.037) (Table 6).
Discussion
In the present study, we demonstrated that the radiographic progression of joint erosion with tocilizumab treatment was significantly lower than that with etanercept treatment for RA. Multivariate analysis demonstrated that radiographic progression of joint erosion was associated with the baseline CDAI.
Bone erosion depends on osteoclast formation in the joint31. Monocyte/macrophage lineages infiltrate into inflamed joints and differentiate into osteoclasts, which play an important role in bone resorption31. Receptor activation of the NF-κB ligand (RANKL) is the primary factor in osteoclast differentiation and promotes osteoclast differentiation mainly through controlling gene expression by activating its receptor, RANK32. It is conceivable that drugs that suppress joint inflammation also inhibit monocyte/macrophage infiltration and, consequently, osteoclast formation.
IL-6 is considered a key molecule in driving osteoclastogenesis and bone resorption in RA8,33. RANKL is induced by IL-6 in mesenchymal cells, and IL-6 also influences T lymphocytes to support osteoclastogenesis34,35. Interaction of IL-6 with IL-6R on osteoclast precursors directly influences osteoclast formation without RANKL signalling36. Consequently, IL-6R directly affects osteoclast formation independent of its anti-inflammatory effects37. TNF-α also stimulates osteoclastogenesis through osteoclast precursors primed by a sufficient level of RANKL38. TNF-α binds to its receptors on stromal or osteoblastic cells and enhances RANKL expression39. Thus, TNF-α plays a pivotal role in enhancing the pathogenesis of inflammatory bone erosion in the presence of RANKL. These differences in mechanism underlying the stimulation of osteoclastogenesis may be one of the reasons that explain our finding that the inhibitory effect on progression of joint erosion was higher with the IL-6 inhibitor than with the TNF-α inhibitor.
Several clinical trials demonstrated that seropositivity for anti-citrullinated protein (CCP) antibodies, rheumatoid factor, inflammatory markers including CRP, baseline erosion, swollen joint count, and persistent disease activity were associated with rapid joint destruction in patients with RA40,41. A recent report showed that patients who achieve clinical remission within six months, as defined based on the DAS28-CRP, SDAI, CDAI, and ACR/EULAR Boolean criteria, have a high likelihood of remaining free of radiographic structural progression42. Welsing et al. investigated the longitudinal relationship between inflammatory disease activity and radiologic progression and demonstrated that high disease activity at base line causes progression of radiologic damage43. The results of these studies support our findings of multivariate analysis that the radiographic progression of joint erosion was associated with the baseline CDAI.
The limitations of this study are as follows: First, the sample sizes in subgroups of the cohort were not large, and power was limited. Therefore, the data must be accumulated and re-analysed in the future. Second, the database used in the analysis was obtained retrospectively. Third, the present study focused on results for 12 months after drug administration. Long-term outcomes with more than 12 months are yet to be elucidated. Fourth, the study only enrolled patients from two hospitals in one country therefore our results may be subject to geographical bias.
Conclusions
We demonstrated that tocilizumab is more effective in suppressing radiographic progression of joint erosion compared to etanercept, and the radiographic progression of joint erosion was associated with baseline CDAI.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Klareskog, L., Catrina, A. I. & Paget, S. Rheumatoid arthritis. Lancet 373(9664), 659–672 (2009).
Radner, H., Smolen, J. S. & Aletaha, D. Comorbidity affects all domains of physical function and quality of life in patients with rheumatoid arthritis. Rheumatology 50(2), 381–388 (2011).
Smolen, J. S. et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann. Rheum. Dis. 79(6), 685–699 (2020).
Harre, U. & Schett, G. Cellular and molecular pathways of structural damage in rheumatoid arthritis. Semin. Immunopathol. 39(4), 355–363 (2017).
Smolen, J. S. et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann. Rheum. Dis. 76(6), 960–977 (2017).
Walsh, N. C., Crotti, T. N., Goldring, S. R. & Gravallese, E. M. Rheumatic diseases: The effects of inflammation on bone. Immunol. Rev. 208, 228–251 (2005).
Dasgupta, B., Corkill, M., Kirkham, B., Gibson, T. & Panayi, G. Serial estimation of interleukin 6 as a measure of systemic disease in rheumatoid arthritis. J. Rheumatol. 19(1), 22–25 (1992).
Kotake, S. et al. Interleukin-6 and soluble interleukin-6 receptors in the synovial fluids from rheumatoid arthritis patients are responsible for osteoclast-like cell formation. J. Bone Miner. Res. 11(1), 88–95 (1996).
Ozaki, K. et al. Functional SNPs in the lymphotoxin-alpha gene that are associated with susceptibility to myocardial infarction. Nat. Genet. 32(4), 650–654 (2002).
Nishimoto, N. et al. Study of active controlled monotherapy used for rheumatoid arthritis, an IL-6 inhibitor (SAMURAI): Evidence of clinical and radiographic benefit from an x ray reader-blinded randomised controlled trial of tocilizumab. Ann. Rheum. Dis. 66(9), 1162–1167 (2007).
Teitsma, X. M. et al. Radiographic joint damage in early rheumatoid arthritis patients: Comparing tocilizumab- and methotrexate-based treat-to-target strategies. Rheumatology 57(2), 309–317 (2018).
Genovese, M. C. et al. Efficacy and safety of ABT-494, a selective JAK-1 inhibitor, in a phase IIb study in patients With rheumatoid arthritis and an inadequate response to methotrexate. Arthr. Rheumatol. 68(12), 2857–2866 (2016).
Nam, J. L. et al. Efficacy of biological disease-modifying antirheumatic drugs: A systematic literature review informing the 2016 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann. Rheum. Dis. 76(6), 1113–1136 (2017).
Hashimoto, J. et al. Humanized anti-interleukin-6-receptor antibody (tocilizumab) monotherapy is more effective in slowing radiographic progression in patients with rheumatoid arthritis at high baseline risk for structural damage evaluated with levels of biomarkers, radiography, and BMI: Data from the SAMURAI study. Mod. Rheumatol. 21(1), 10–15 (2011).
van der Heijde, D. et al. Disease remission and sustained halting of radiographic progression with combination etanercept and methotrexate in patients with rheumatoid arthritis. Arthr. Rheum. 56(12), 3928–3939 (2007).
van der Heijde, D. et al. Low rates of radiographic progression of structural joint damage over 2 years of baricitinib treatment in patients with rheumatoid arthritis. RMD Open 5(1), e000898 (2019).
Butler, D. M., Maini, R. N., Feldmann, M. & Brennan, F. M. Modulation of proinflammatory cytokine release in rheumatoid synovial membrane cell cultures. Comparison of monoclonal anti TNF-alpha antibody with the interleukin-1 receptor antagonist. Eur. Cytokine Netw. 6(4), 225–230 (1995).
Haworth, C. et al. Expression of granulocyte-macrophage colony-stimulating factor in rheumatoid arthritis: Regulation by tumor necrosis factor-alpha. Eur. J. Immunol. 21(10), 2575–2579 (1991).
Chin, J. E., Winterrowd, G. E., Krzesicki, R. F. & Sanders, M. E. Role of cytokines in inflammatory synovitis. The coordinate regulation of intercellular adhesion molecule 1 and HLA class I and class II antigens in rheumatoid synovial fibroblasts. Arthr. Rheum. 33(12), 1776–1786 (1990).
Choy, E. H. & Panayi, G. S. Cytokine pathways and joint inflammation in rheumatoid arthritis. N. Engl. J. Med. 344(12), 907–916 (2001).
Bazzoni, F. & Beutler, B. The tumor necrosis factor ligand and receptor families. N. Engl. J. Med. 334(26), 1717–1725 (1996).
Best, J. H., Vlad, S. C., Tominna, L. & Abbass, I. Real-world persistence with tocilizumab compared to other subcutaneous biologic disease-modifying antirheumatic drugs among patients with rheumatoid arthritis switching from another biologic. Rheumatol. Ther. 7(2), 345–355 (2020).
Kilcher, G. et al. Rheumatoid arthritis patients treated in trial and real world settings: Comparison of randomized trials with registries. Rheumatology 57(2), 354–369 (2018).
Arnett, F. C. et al. The american rheumatism association 1987 revised criteria for the classification of rheumatoid arthritis. Arthr. Rheum. 31(3), 315–324 (1988).
Pincus, T., Summey, J. A., Soraci, S. A. Jr., Wallston, K. A. & Hummon, N. P. Assessment of patient satisfaction in activities of daily living using a modified stanford health assessment questionnaire. Arthr. Rheum. 26(11), 1346–1353 (1983).
Felson, D. T. et al. American college of rheumatology/european league against rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthr. Rheum. 63(3), 573–586 (2011).
Sharp, J. T. et al. How many joints in the hands and wrists should be included in a score of radiologic abnormalities used to assess rheumatoid arthritis?. Arthr. Rheum. 28(12), 1326–1335 (1985).
van der Heijde, D. How to read radiographs according to the Sharp/van der heijde method. J. Rheumatol. 27(1), 261–263 (2000).
Bruynesteyn, K., Boers, M., Kostense, P., van der Linden, S. & van der Heijde, D. Deciding on progression of joint damage in paired films of individual patients: Smallest detectable difference or change. Ann. Rheum. Dis. 64(2), 179–182 (2005).
Rosenbaum, P. R. & Rubin, D. B. The central role of the propensity score in observational studies for causal effects. Biometrika 70(1), 41–55 (1983).
Gravallese, E. M. et al. Identification of cell types responsible for bone resorption in rheumatoid arthritis and juvenile rheumatoid arthritis. Am. J. Pathol. 152(4), 943–951 (1998).
Teitelbaum, S. L. Bone resorption by osteoclasts. Science 289(5484), 1504–1508 (2000).
Dai, J. et al. Chronic alcohol ingestion induces osteoclastogenesis and bone loss through IL-6 in mice. J. Clin. Invest. 106(7), 887–895 (2000).
Wong, P. K. et al. Interleukin-6 modulates production of T lymphocyte-derived cytokines in antigen-induced arthritis and drives inflammation-induced osteoclastogenesis. Arthr. Rheum. 54(1), 158–168 (2006).
Liu, X. H., Kirschenbaum, A., Yao, S. & Levine, A. C. Cross-talk between the interleukin-6 and prostaglandin E(2) signaling systems results in enhancement of osteoclastogenesis through effects on the osteoprotegerin/receptor activator of nuclear factor-{kappa}B (RANK) ligand/RANK system. Endocrinology 146(4), 1991–1998 (2005).
Kudo, O. et al. Interleukin-6 and interleukin-11 support human osteoclast formation by a RANKL-independent mechanism. Bone 32(1), 1–7 (2003).
Axmann, R. et al. Inhibition of interleukin-6 receptor directly blocks osteoclast formation in vitro and in vivo. Arthr. Rheum. 60(9), 2747–2756 (2009).
Lam, J. et al. TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J. Clin. Invest. 106(12), 1481–1488 (2000).
Quinn, J. M., Horwood, N. J., Elliott, J., Gillespie, M. T. & Martin, T. J. Fibroblastic stromal cells express receptor activator of NF-kappa B ligand and support osteoclast differentiation. J. Bone Miner. Res. 15(8), 1459–1466 (2000).
Visser, K. et al. A matrix risk model for the prediction of rapid radiographic progression in patients with rheumatoid arthritis receiving different dynamic treatment strategies: post hoc analyses from the BeSt study. Ann. Rheum. Dis. 69(7), 1333–1337 (2010).
Vastesaeger, N., Xu, S., Aletaha, D., St Clair, E. W. & Smolen, J. S. A pilot risk model for the prediction of rapid radiographic progression in rheumatoid arthritis. Rheumatology 48(9), 1114–1121 (2009).
Legrand, J., Kirchgesner, T., Sokolova, T., Vande Berg, B. & Durez, P. Early clinical response and long-term radiographic progression in recent-onset rheumatoid arthritis: Clinical remission within six months remains the treatment target. Jt. Bone Spine 86(5), 594–599 (2019).
Welsing, P. M. J. et al. The relationship between disease activity and radiologic progression in patients with rheumatoid arthritis: A longitudinal analysis. Arthr. Rheum. 50(7), 2082–2093 (2004).
Author information
Authors and Affiliations
Contributions
S.H. participated in the study design, drafting of the manuscript, and data collection. TMatsu carried out data collection, drafting of the manuscript and helped to revised the manuscript. TMae participated in the data collection and drafting of the manuscript. KF participated in the study design and helped to revised the manuscript. MH participated in the data collection and drafting of the manuscript. KT carried out data collection and drafting of the manuscript. TK participated in the data collection and drafting of the manuscript. ST participated in the data collection and analysis. TK participated in the data collection and analysis. YT participated in the data collection and analysis. TM participated in the data collection and analysis. RK participated in the study design and helped to revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hayashi, S., Matsubara, T., Maeda, T. et al. Comparison of the inhibitory effect of tocilizumab and etanercept on the progression of joint erosion in rheumatoid arthritis treatment. Sci Rep 12, 17524 (2022). https://doi.org/10.1038/s41598-022-22152-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22152-w
This article is cited by
-
Cost-consequence analysis of tocilizumab versus adalimumab and etanercept among rheumatoid arthritis patients in Saudi Arabia: a single-center study
Cost Effectiveness and Resource Allocation (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.