Abstract
Long term prognosis and 5-year survival for pancreatic adenocarcinoma (PDAC) remains suboptimal. Endoscopic ultrasound (EUS) guided RFA (EUS-RFA) is an emerging technology and limited data exist regarding safety and long-term outcomes. The aim of this study is to report safety-profile, feasibility and outcomes of EUS-RFA for advanced PDAC. Prospective review of patients with diagnosis of locally-advanced or metastatic PDAC undergoing EUS-RFA between October 2016 to March 2018 with long-term follow up (> 30 months). Study patients underwent a total of 1–4 RFA sessions. All patients were enrolled in longitudinal cohort study and received standard of care chemotherapy. 10 patients underwent EUS-RFA. Location of the lesions was in the head(4), neck(2), body(2), and tail(2). 22 RFA sessions were performed with a range of 1–4 sessions per patient. There were no major adverse events (bleeding, perforation, infection, pancreatitis) in immediate (up to 72 h) and short-term follow up (4 weeks). Mild worsening of existing abdominal pain was noted during post-procedure observation in 12/22 (55%) of RFA treatments. Follow-up imaging demonstrated tumor progression in 2 patients, whereas tumor regression was noted in 6 patients (> 50% reduction in size in 3 patients). Median survival for the cohort was 20.5 months (95% CI, 9.93–42.2 months). Currently, 2 patients remain alive at 61 and 81 months follow-up since initial diagnosis. One patient had 3 cm PDAC with encasement of the portal confluence, abutment of the celiac axis, common hepatic and superior mesenteric artery. This patient had significant reduction in tumor size and underwent standard pancreaticoduodenectomy. In our experience, EUS-RFA was safe, well-tolerated and could be concurrently performed with standard chemotherapy. In this select cohort, median survival was improved when compared to published survival based upon SEER database and clinical trials. Future prospective trials are needed to understand the role of EUS-RFA in overall management of PDAC.
Similar content being viewed by others
Introduction
Pancreatic ductal adenocarcinoma (PDAC) remains a leading cause of cancer death in the United States and is highly resistant to therapy1,2. Surgical resection remains the only curative option, but more than 80% of patients present with unresectable disease highlighting the urgent need for improved neoadjuvant therapeutic options3. Unfortunately, even among those who are candidates and undergo surgical resection, the reported median survival is 15–23 months, with a 5-year survival less than 20%4,5,6. These dismal survival rates over the past several decades remain disappointing. Despite improvements in diagnostic imaging, surgical technique and chemotherapeutic options, only modest improvements in PDAC survival have been reported. It remains clear that surgical resection is a prerequisite for achieving long-term survival; thus, innovative treatments to increase odds for R0 resection are needed to improve overall survival in PDAC7.
Currently patients diagnosed with locally-advanced, unresectable or metastatic PDAC are only candidates for systemic chemotherapy and/or chemoradiation or a clinical trial. As defined by the National Comprehensive Cancer Network (NCCN), locally-advanced pancreatic cancer (LAPC) criteria include: (1) > 180 degrees contact of superior mesenteric artery or common hepatic artery, (2) aortic involvement or (3) unreconstructable superior mesenteric vein/portal vein due to tumor involvement or occlusion8. In highly selected patients with locally-advanced disease, neoadjuvant chemotherapy (NAC) and chemoradiation has resulted in diagnostic downstaging resulting in surgical resection in 30–50% of cases9,10 and progression in 20% of cases. For patients that progressed after NAC, the median survival is < 18 months. These statistics highlight the incredible potential for PDAC to adapt and resist NAC in a subset of patients. In those eligible for surgical resection, NAC is highly recommended by the NCCN as probable benefits include tumor stage downsizing and increased probability of a margin-negative resection11,12,13.
At present, conventional treatment modalities for PDAC are limited to chemotherapy, radiation and surgery; these treatments have been used for the last 20 + years14. Recent advances in endoscopic therapy may provide an additional therapeutic modality. Several percutaneous and endoscopic ultrasound (EUS) guided ablative techniques have been explored for the treatment of pancreatic lesions such as alcohol injection, photodynamic therapy, and laser ablation15. These techniques are less-invasive which enhances feasibility and may be safer in patients who are poor candidates for surgical resection. EUS guided radiofrequency ablation (EUS-RFA) is one of the newer techniques currently available16. EUS-RFA application consists of alternating current with a frequency of 350–500 kHz (coincidentally the frequency range of radio broadcasts as well) to the target tissue via a special electrode located at the tip of the endoscope. Alternating current causes vibratory movement of ionic particles in the abutting and adjoining tissue resulting in generation of heat. RFA induces not only local disruption of the tumor by heat, but also produces intratumoral localized coagulation necrosis which results in the release of large amounts of cellular debris17. Local and systemic release of cellular debris is postulated to be a tumor antigen source that can trigger a host adaptive immune response targeting PDAC. The release of pathogenic “noxa” into the body induces a strong inflammatory response with elevated levels of IL-6, HGF, and VEGF18. RFA has recently been recognized for its potential in palliative treatment of malignant biliary strictures19,20. Based on published data, RFA appears to provide palliation and may increase survival21,22. These data suggest RFA may be considered as an additional neoadjuvant therapy for locally advanced pancreatic cancer as a novel method to combine local and systemic immune-modulatory effects. Our hypothesis is that EUS-RFA is a safe treatment modality and may improve survival for unresectable or locally-advanced pancreatic ductal adenocarcinoma.
Methods
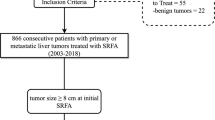
We evaluated adult patients with an established, histologically confirmed diagnosis of unresectable or locally-advanced PDAC. Inclusion criteria were: (1) diagnosis of PDAC, (2) locally-advanced or metastatic PDAC, (3) contraindication to radiation therapy, (4) refusal of radiation therapy, (5) stable/persistent disease following radiation therapy, (6) patients with stable advanced disease (defined as greater than 6 months treatment with systemic chemotherapy) and (7) concurrent systemic chemotherapy. Eligible patients underwent EUS-RFA at the University of Texas Health Sciences Center at Houston (UTHealth) between October 2016 to March 2018 with long term follow up (> 30 months). All patients were enrolled in a prospective EUS-RFA study (HSC-MS-18–0192) approved by the UTHealth Committee for the Protection of Human Subjects Institutional Review Board. Informed consent was obtained from all patients. These experimental procedures were performed in accordance with relevant institutional guidelines.
All patients were concurrently undergoing standard of care systemic chemotherapy, either modified FOLFIRINOX: Oxaliplatin 85 mg/m2 IV over 2 h, Leucovorin 400 mg/m2 IV over 2 h, Irinotecan 150 mg/m2 IV over 90 min, Fluorouracil 2400 mg/m2 IV continuous infusion (CI) over 46 h beginning on Day 1 and repeat this cycle every 14 days or Gemcitabine/nab-Pacliataxel: Gemcitabine 500–1000 mg/m2 over 30 min Nab-Paclitaxel 125 mg/m2 over 30 min + /- Cisplatin 25 mg/m2 over 1 h with 1L NS hydration. Weekly, 3 weeks on and one week off (Day 1,8, 15 every 28 days).
Patients in this study underwent upper endoscopy using therapeutic Pentax or Olympus scope. The EUS-RFA procedure was performed using the Habib 6500 ablation catheter (Boston Scientific, Marlborough, MA). Prior to RFA, a standard fine needle aspiration (FNA) was performed. After the FNA, a 19- or 22- gauge probe was advanced into the target lesion. Using ultrasound guidance, transduodenal or transgastric electrode needle probe placement into the target lesion was performed. Color Doppler scanning was performed in order to avoid nearby or adjacent blood vessels. The RFA parameters included treatment of target lesion (10–15 W) to a measured electrical resistance of 200 Ohm or a rapid change in Ohms. Treatment was confirmed by the gastroenterologist who noted either liquefaction or bubbling noted with real-time EUS. Patients received up to a total of 4 EUS-RFA sessions/treatments (1 session every 2–3 weeks) based upon the completeness of ablation as determined by the interventional gastroenterologist.
The primary endpoint of this study was technical success of the EUS-RFA procedure. Secondary endpoints included: (1) safety, side-effects, adverse events, (2) overall survival and (3) serum CA19-9 response to treatment. The date of PDAC diagnosis and date of death were used for Kaplan Meier analysis to measure survival and those patients who remain alive were right-censored (STATA 16, College Station, TX). Serum 19–9 response to treatment over time was estimated using one-way ANOVA. The Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST1.1) was used to evaluate radiographic treatment23.
Results
Patients
In this prospective study, a total of 10 patients (mean age 62 years) underwent EUS-RFA (Table 1). The majority of patients in this study were male (70%) and Caucasian (80%). At the time of RFA, a majority of the patients were AJCC stage III (70%). Based upon accepted definitions of PDAC tumor anatomy, 7 patients were locally-advanced and 3 patients were metastatic. In most cases, EUS-RFA was performed as an outpatient procedure. Location of the primary PDAC was in the head (4), neck (2), body (2), and tail (2) (Table 2). At diagnosis, mean CA19-9 was 2004.3 (SD 2736.8) and was elevated in 7 patients (70%). Systemic chemotherapy was used in all patients (mFOLFIRINOX = 2, gemcitabine/Abraxane = 1, both mFOLFIRINOX and gemcitabine/Abraxane = 6, mFOLFIRINOX and gemcitabine/Abraxane + Cisplatin = 1). Three patients also received external beam radiation in addition to EUS-RFA.
Procedure
In this patient cohort, a total of 22 EUS-RFA sessions were performed with a range of 1–4 RFA sessions per patient. There were no aborted endoscopic ablation procedures and all 10 patients were successfully treated with EUS-RFA (100% treatment rate). Mean time for the EUS RFA procedure was 32.6 min (range 18–66). There were no major adverse events (bleeding, perforation, infection, pancreatitis) in the immediate (up to 72 h) and short-term follow up (4 weeks) period. Mild worsening of existing abdominal pain was noted during post-procedure observation in 12/22 (55%) of RFA treatments. This was managed by short-term opioid therapy and extended post-procedure observation (1–4 h) in the recovery unit. None of the patients required hospital admission following EUS-RFA.
Outcome
Serum CA19-9 was measured in longitudinal fashion prior to and following EUS-RFA. A total of 7 patients were observed to have an elevated serum CA19-9. In these 7 patients a total of 15 RFA treatment sessions were performed. These treatments resulted in a serum 19–9 decrease following 12 RFA sessions (Fig. 1). A one-way repeated measures ANOVA test was performed on the elevated CA19-9 patients to determine if differences were associated RFA treatment. The results showed that following RFA there were statistically significant differences in CA19-9 over the time course (p-value < 0.0005.) This effect is most prominent in patient #5 (red line) and patient #8 (green line). Follow-up abdominal imaging after RFA treatment was available in 9 of the 10 patients. Primary tumor progression was noted in 2 patients, whereas tumor regression was noted in 7 patients (> 50% reduction in size in 3 patients). Kaplan–Meier survival analysis demonstrated median survival duration of 20.5 months (95% CI: 9.93–42.2) (Fig. 2). The median survival post-RFA was 13.4 months (95% CI: 0.9–27.8). Currently, 2 patients are still alive at 61 months and 81 months follow-up since initial cancer diagnosis. One of these patients had a 3 cm primary tumor with abutment of the portal confluence, abutment of the celiac axis, common hepatic artery and superior mesenteric artery. This patient was treated with extended systemic chemotherapy (mFOLFIRINOX 19 cycles), intensity modulated radiation therapy (50.4 Gy) and 3 EUS-RFA sessions. The tumor decreased in size with regression along the previously involved mesenteric vessels (Fig. 3). This patient tolerated all pre-operative treatment with minimal toxicity and subsequently underwent a margin negative (R0) pancreaticoduodenectomy (alive at 61 months). Another patient was initially thought to have metastatic PDAC with a histologically proven positive mediastinal node (Stage IV). This patient underwent extended chemotherapy (3 cycles mFOLFIRINOX, 32 cycles Gemcitabine/nab-Paclitaxel and 3 cycles of Gemcitabine/nab-Paclitaxel/Cisplantin) and 2 EUS-RFA treatments. Robotic-assisted laparoscopic pancreaticoduodenectomy was performed and the surgical pathology demonstrated an ampullary adenocarcinoma. This patient remains alive with no evidence of disease at 81 months from initial diagnosis.
CT scan images from PDAC patient pre- and post-therapy who underwent margin-negative pancreaticoduodenectomy. Representative computed tomography shows reduced PDAC lesion size post RFA. (A) Computed tomography (CT) with pancreas head mass and evidence of portal confluence encasement. (B) CT with pancreas head mass and evidence of superior mesenteric artery abutment. (C) CT post RFA with resolution of previously seen encasement of celiac axis as evidenced by a fat plane between tumor and celiac vessels. (D) Magnetic resonance imaging post RFA of PDAC with no further evidence of tumoral abutment of celiac axis, superior mesenteric artery and superior mesenteric vein.
Conclusions
In this single institution experience, EUS-RFA was safe, well-tolerated and concurrently performed with standard of care PDAC chemotherapy treatment. There were no significant side effects or adverse events noted in this small series. The observed overall survival (20.5 months) in this cohort is encouraging, despite advanced stage disease (III or IV) in all patients. This appears to be an improvement to published expected survival (9–12 months) for LAPC treated with chemotherapy alone24. These results are also comparable to locally-advanced patients treated with radiation dose escalation after induction chemotherapy (median overall survival 17.8 months)25. However, escalated radiation dose protocols resulted in higher rates of known side effects such as abdominal pain, nausea, vomiting, diarrhea or fatigue. In addition, escalated radiation dose results in anemia requiring transfusion in 13% of PDAC patients30. Thus, the feasibility and tolerance of > 50.4 Gy radiation treatment is likely limited in older, debilitated LAPC patients. Although median survival may be either equivalent or possibly better when comparing our small cohort to dose-escalated radiation, EUS-RFA may be both safer and better tolerated in LAPC patients with marginal performance status.
These data are timely as the widespread use of ablative techniques is employed in the management of other gastrointestinal cancers; however, RFA treatment of the pancreas has been very limited. Ablation has not been widely used as therapy for PDAC due to potential risk of complications from the increased sensitivity of pancreatic tissue to thermal injury, concerns for pancreatitis and proximity to critical vascular and biliary structures. Prior to the newer EUS approach, other options were either percutaneous of surgical which may be an aggressive modality in patients with advanced PDAC. Albeit a small sample size, EUS-RFA was technically feasible to perform and well-tolerated in this PDAC patient cohort.
Several investigators have demonstrated the feasibility of EUS-RFA in porcine and animal models26,27,28. In animal models of pancreatic RFA, short-term results appeared safe as most rodent or porcine patients survived unharmed until euthanized per the research protocol. Translation into clinical use has been hindered by both endoscopic and technologic challenges. Open surgical or laparoscopic approaches may not be well-tolerated with limited feasibility since most surgeons are not trained in pancreatic ablation. Thus, endoscopic RFA may be the ideal approach when compared to traditional open or laparoscopic pancreatic ablation in which postoperative complication rates approach 25%29. Endoscopy also has the advantage of concurrent EUS visualization and ultrasound mode scanning. The EUS technique has been used in pancreatic neuroendocrine tumors with similar results (< 10% complication rate)30. In a recent update from Barthet et al., 65% of patients that underwent EUS-RFA treatment of a neuroendocrine tumor of cystic neoplasm had complete disappearance of the index lesion31. The data from these studies suggest the EUS-RFA approach may be a durable alternative treatment modality for pancreatic neuroendocrine tumors (< 3 cm) and select cystic neoplasms.
PDAC-related mortality has not significantly declined over the past two decades, unlike other solid malignancies (lung, colon, breast). Multi-agent preoperative chemotherapy remains the current gold-standard, yet the majority of PDAC patients are not candidates for potentially curative surgery. At present, both chemotherapy and chemoradiation have been employed in borderline resectable and locally-advanced PDAC with mixed results32. As newer technologies emerge, local ablative treatments may play a role in the treatment of PDAC. As mentioned previously, EUS-RFA treatment in combination with standard chemotherapy may be beneficial for several reasons: (1) direct treatment of the PDAC through coagulative necrosis, (2) improved chemotherapeutic efficacy as the tumor may become more porous and allow systemic therapies to further penetrate into the tissues and (3) possibly enhanced, systemic antitumor immunity as necrotic PDAC released into the bloodstream may be recognized by the host immune system. Tumor ablation has been shown to enhance systemic immune-mediated effects33,34. These systemic effects may help to explain the patient in this series with stage IV ampullary carcinoma who remains alive at 73 months from date of diagnosis. Obviously, tumor biology plays a key role; however, it is possible that RFA sensitized the immune system to treat systemic disease.
There are several important limitations to discuss. This patient cohort is relatively heterogeneous with regards to tumor size, location and stage. This study was nonrandomized and the systemic treatment protocol was not equivalent in all patients. In this small cohort, there was no standardized approach to the timing of EUS-RFA in combination with chemotherapy and/or radiation. In addition, follow-up imaging was unavailable in 1 patient. In this small cohort, it is very possible that the treatment effect is biased favorably towards RFA. Only a future randomized control trial will be able to provide the least biased estimate of the actual EUS-RFA treatment effect. Despite these obvious limitations, this is a mature data set dating back to 2016. Notwithstanding the small sample size, this data adds to the available body of evidence and clinical experience that EUS-RFA appears to be a safe treatment modality for cancer localized to the pancreas. At present this data is only meant to demonstrate the feasibility of the procedure and to be hypothesis-generating as the quality of evidence by all accepted standards is low.
These results highlight our institutional EUS-RFA experience in the treatment of pancreatic cancers. This minimally-invasive procedure was well-tolerated in patients with advanced disease. In addition, two patients with locally-advanced disease responded to the RFA treatment and were able to undergo potentially curative pancreaticoduodenectomy. Of note, at the time of surgical resection there was no appreciable scarring or fibrosis observed by the operative team. This had been a significant operative concern as external beam radiation and fibrosis is known to interfere with radical surgery. In these two cases, the EUS-RFA did not appear to negatively influence the complex resection. This report of pancreatic RFA suggests this procedure may be a complementary treatment alongside standard chemotherapy. This new combination therapy may extend an effective treatment to a larger group of patients. This may provide an effective therapy to older and/or fragile patients that may not tolerate other treatments such as chemotherapy with dose-escalated radiation. This initial experience is promising and suggests future clinical trials are needed to understand the role and timing of EUS-RFA in the management of both localized and advanced pancreatic ductal adenocarcinoma. At present, our institution is currently conducting a single-arm, phase II trial (www.clinicaltrials.gov NCT04990609) of neoadjuvant chemotherapy plus EUS-RFA for resectable pancreas cancer (PANCARDINAL-1).
Data availability
The datasets used and/or analysed during the current study are deidentified and included in this published article as supplementary files. In addition, the deidentified datasets (in spreadsheet format) can be requested from the corresponding author on reasonable request.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 69(1), 7–34 (2019).
Mizrahi, J. D. et al. Pancreatic cancer. Lancet 395(10242), 2008–2020 (2020).
Li, D. et al. Pancreatic cancer. Lancet 363(9414), 1049–1057 (2004).
Neoptolemos, J. P. et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: A randomized controlled trial. JAMA 304(10), 1073–1081 (2010).
Yeo, C. J. et al. Pancreaticoduodenectomy for cancer of the head of the pancreas. 201 patients. Ann. Surg. 221(6), 721–31 (1995). discussion 731–3.
Yeo, C. J. et al. Pancreaticoduodenectomy for pancreatic adenocarcinoma: postoperative adjuvant chemoradiation improves survival. A prospective, single-institution experience. Ann. Surg. 225(5), 621–33 (1997). discussion 633–6.
Howard, T. J. et al. A margin-negative R0 resection accomplished with minimal postoperative complications is the surgeon's contribution to long-term survival in pancreatic cancer. J. Gastrointest. Surg. 10(10), 1338–45 discussion 1345–6 (2006).
Tempero, M. A. et al. Pancreatic adenocarcinoma, Version1. 2019. J. Natl. Compr. Canc. Netw. 17(3), 202–210 (2019).
Ferrone, C. R. et al. Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann. Surg. 261(1), 12–17 (2015).
Chatzizacharias, N. A. et al. Locally advanced pancreas cancer: Staging and goals of therapy. Surgery 163(5), 1053–1062 (2018).
Quiros, R. M., Brown, K. M. & Hoffman, J. P. Neoadjuvant therapy in pancreatic cancer. Cancer Invest. 25(4), 267–273 (2007).
Janssen, Q. P. et al. Neoadjuvant treatment in patients with resectable and borderline resectable pancreatic cancer. Front. Oncol. 10, 41 (2020).
Motoi, F. et al. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn. J. Clin. Oncol. 49(2), 190–194 (2019).
Varadhachary, G. R. et al. Borderline resectable pancreatic cancer: definitions, management, and role of preoperative therapy. Ann. Surg. Oncol. 13(8), 1035–1046 (2006).
Yokoyama, T. et al. Percutaneous and laparoscopic approaches of radiofrequency ablation treatment for liver cancer. J. Hepatobiliary Pancreat. Surg. 10(6), 425–427 (2003).
Song, T. J. et al. Initial experience of EUS-guided radiofrequency ablation of unresectable pancreatic cancer. Gastrointest. Endosc. 83(2), 440–443 (2016).
Rustagi, T. & Chhoda, A. Endoscopic radiofrequency ablation of the pancreas. Dig. Dis. Sci. 62(4), 843–850 (2017).
Fegrachi, S. et al. Safety of radiofrequency ablation in patients with locally advanced, unresectable pancreatic cancer: A phase II study. Eur. J. Surg. Oncol. 45(11), 2166–2172 (2019).
Bang, J. Y. et al. EUS-guided celiac ganglion radiofrequency ablation versus celiac plexus neurolysis for palliation of pain in pancreatic cancer: a randomized controlled trial (with videos). Gastrointest. Endosc. 89(1), 58-66 e3 (2019).
Scopelliti, F. et al. Technique, safety, and feasibility of EUS-guided radiofrequency ablation in unresectable pancreatic cancer. Surg. Endosc. 32(9), 4022–4028 (2018).
Cazacu, I. M. et al. Endoscopic ultrasound-guided treatment of pancreatic cancer. Curr. Gastroenterol. Rep. 22(6), 27 (2020).
Dhaliwal, A. et al. Efficacy of EUS-RFA in pancreatic tumors: Is it ready for prime time? A systematic review and meta-analysis. Endos. Int. Open 8(10), E1243–E1251 (2020).
Schwartz, L. H. et al. RECIST 11-update and clarification: From the RECIST committee. Eur. J. Cancer 62, 132–137 (2016).
Hammel, P. et al. Effect of chemoradiotherapy vs chemotherapy on survival in patients with locally advanced pancreatic cancer controlled after 4 months of gemcitabine with or without erlotinib: The LAP07 randomized clinical trial. JAMA 315(17), 1844–1853 (2016).
Krishnan, S. et al. Focal radiation therapy dose escalation improves overall survival in locally advanced pancreatic cancer patients receiving induction chemotherapy and consolidative chemoradiation. Int. J. Radiat. Oncol. Biol. Phys. 94(4), 755–765 (2016).
Goldberg, S. N. et al. EUS-guided radiofrequency ablation in the pancreas: Results in a porcine model. Gastrointest. Endosc. 50(3), 392–401 (1999).
Yachimski, P. & Varadarajulu, S. Endoscopic ultrasound-guided pancreatic cyst ablation: More peril than promise?. Gastroenterology 153(5), 1183–1185 (2017).
Carrara, S. et al. Endoscopic ultrasound-guided application of a new hybrid cryotherm probe in porcine pancreas: A preliminary study. Endoscopy 40(4), 321–326 (2008).
Girelli, R. et al. Results of 100 pancreatic radiofrequency ablations in the context of a multimodal strategy for stage III ductal adenocarcinoma. Langenbecks Arch. Surg. 398(1), 63–69 (2013).
Barthet, M. Endoscopic ultrasound-guided radiofrequency ablation for pancreatic neuroendocrine tumor. Ann. Endocrinol. (Paris) 80(3), 182–184 (2019).
Barthet, M. et al. Endoscopic ultrasound-guided radiofrequency ablation for pancreatic neuroendocrine tumors and pancreatic cystic neoplasms: A prospective multicenter study. Endoscopy 51(9), 836–842 (2019).
Katz, M. H. G. et al. Alliance for clinical trials in oncology (ALLIANCE) trial A021501: Preoperative extended chemotherapy vs. chemotherapy plus hypofractionated radiation therapy for borderline resectable adenocarcinoma of the head of the pancreas. BMC Cancer 17(1), 505 (2017).
Lemdani, K. et al. Local immunomodulation combined to radiofrequency ablation results in a complete cure of local and distant colorectal carcinoma. Oncoimmunology 8(3), 1550342 (2019).
Leuchte, K. et al. Microwave ablation enhances tumor-specific immune response in patients with hepatocellular carcinoma. Cancer Immunol. Immunother. 70(4), 893–907 (2021).
Acknowledgements
This research was supported by Carolyn Frost Keenan and Charlie Gaines Research Endowment Funds to the Center for Interventional Gastroenterology at UTHealth (iGUT), as well as by Atilla Ertan MD Endowment funding to Dr. Nirav Thosani.
Author information
Authors and Affiliations
Contributions
N.T.- manuscript draft and revision. P.C.- study design and manuscript revision. S.G.- manuscript revision and interpretation. J.R.- manuscript draft and revision. P.P.- data collection and analysis. J.B. – data analysis and interpretation. D.B. – Data collection and manuscript revision. C.W.- study design and manuscript revision.
Corresponding author
Ethics declarations
Competing interests
Dr. Nirav Thosani has received a grant from Emcision, royalties from UpToDate, consulting fees from Boston Scientific and Pentax America, and honorarium from Abbvie. Dr. Putao Cen has received honorarium from Eisai, Pfizer and Taohi, she also is on the advisory board for Seagen. Drs. Rowe, Guha, Bailey-Lundberg, Bhakta and Wray have no conflicts of interest or financial ties to disclose. Mr. Prithvi Patil has no conflicts of interest or financial ties to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thosani, N., Cen, P., Rowe, J. et al. Endoscopic ultrasound-guided radiofrequency ablation (EUS-RFA) for advanced pancreatic and periampullary adenocarcinoma. Sci Rep 12, 16516 (2022). https://doi.org/10.1038/s41598-022-20316-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20316-2
This article is cited by
-
Current Approaches to the Management of Locally Advanced Pancreatic Cancer
Current Surgery Reports (2023)
-
Role of Endoscopic Ultrasound in the Management of Pancreatic Cancer
Indian Journal of Surgical Oncology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.