Abstract
The pressure reactivity index (PRx) is a parameter for the assessment of cerebrovascular autoregulation, but its calculation is affected by artifacts in the source biosignals—intracranial pressure (ICP) and arterial blood pressure. We sought to describe the most common short-duration artifacts and their effect on the PRx. A retrospective analysis of 935 h of multimodal monitoring data was conducted, and five types of artifacts, characterized by their shape, duration, and amplitude, were identified: rectangular, fast impulse, isoline drift, saw tooth, and constant ICP value. Subsequently, all types of artifacts were mathematically modeled and inserted into undisturbed segments of biosignals. Fast impulse, the most common artifact, did not alter the PRx index significantly when inserted into one or both signals. Artifacts present in one signal exceeded the threshold PRx in less than 5% of samples, except for isoline drift. Compared to that, the shortest rectangular artifact inserted into both signals changed PRx to a value above the set threshold in 55.4% of cases. Our analysis shows that the effect of individual artifacts on the PRx index is variable, depending on their occurrence in one or both signals, duration, and shape. This different effect suggests that potentially not all artifacts need to be removed.
Similar content being viewed by others
Introduction
The pressure reactivity index (PRx) is one of the recognized parameters for the assessment of cerebrovascular autoregulation, with a more than 20-year history in neurointensive care. PRx is determined as the moving-window Pearson’s correlation coefficient between arterial blood pressure (ABP) and intracranial pressure (ICP). There is a strong association between PRx-detected impaired cerebrovascular autoregulation (CAR) and unfavorable outcomes following severe traumatic brain injury (TBI)1. Patients with impaired autoregulation may also profit from a different treatment strategy. Moreover, in an experimental setting, PRx possibly allows for calculation of the optimal cerebral perfusion pressure2,3. However, it is a very noisy parameter with several limitations4.
The reliability of the PRx calculation is crucial for its potential clinical use. In a pilot study by Dias et al.5, the quality of the captured signals and calculated PRx were always inspected before the recommended optimal cerebral perfusion pressure (CPPopt) was considered by the attending physician.
The presence of artifacts in source biosignals poses a significant challenge. Manual artifact removal is laborious and delayed, which limits PRx use as a real-time clinical tool. The software ICM+ (Cambridge Enterprise Ltd, Cambridge, UK), commonly used for research in neurocritical care, has an embedded tool for the detection of aberrant signals6,7. The authors of this software recommend treating artifacts as missing values rather than substituting them with the results of calculations from surrounding values6. Embedded online artifact detection is based on the identification of signal values outside the set range or vanishing of the pulse wave amplitude in signals with a pulsatile character. The artifact detection algorithm can also be personalized by the user within the secondary calculations6,7.
Several attempts have been made to identify the sources of the artifacts. Apart from the artifacts originating from disconnection of the monitors and from technical issues, there are several situations common in an intensive care unit that can distort the waveforms and values (patient positioning, coughing, etc.). Previous studies have investigated the pattern8 and the origin9 of the artifacts in the arterial blood pressure signal; some studies have also attempted to detect them10,11,12,13 or even to eliminate them9,14, mainly using artificial intelligence tools and neural networks.
Automated artifact detection and removal from both ICP and ABP signals in patients with traumatic brain injury was proposed by Lee et al.15. Their system based on a stacked convolutional autoencoder and convolutional neural network was able to detect artifacts with high sensitivity (97.3% for ABP and 96.2% for ICP). The study also proved the effect of artifact removal on the incidence of four major clinical events in TBI patients: systemic hypotension, intracranial hypertension, cerebral hypoperfusion, and impaired cerebrovascular reactivity. Among these clinical events, poor cerebrovascular reactivity (defined as PRx > 0.3) was the most frequently observed before and even after artifact removal. The authors speculated that the real incidence of these events might be lower in biosignals without artifacts, which can have serious treatment consequences.
The aim of this study was to investigate the effect of common artifacts in ABP and ICP signals on the calculation of PRx. Specifically, the identified artifacts were further analyzed to evaluate how relevant it is to remove these segments from the signals and how they alter the PRx value.
Methods
Type of study
This study was a retrospective analysis of high-frequency multimodal monitoring data records of patients with intracranial pressure monitoring from an anonymized database. Monitoring of these brain modalities was a part of an ongoing project of the TBI registry. Extracted data were fully anonymized, and no data on patient identifiers were available. All methods were performed in accordance with the relevant guidelines and regulations.
Data
In total, 935 h of anonymized data from seven patients with acute brain injury and invasive intracranial pressure monitoring were analyzed. The average length of recording was 133 h (range 48–256 h). The data were recorded in the Neurointensive Care Unit at the Department of Anesthesiology, Perioperative and Intensive Medicine, Masaryk Hospital in Usti nad Labem, Czech Republic. The datasets comprised only variables of vital sign parameters, and no patient characteristics (e.g., sex, age, date of admission, diagnosis, outcome) were available.
Equipment
All patients had continuous synchronized data collected via ICM+ software (version 8.6, Cambridge Enterprise Ltd., Cambridge, UK): ABP, ICP, electrocardiography and carbon dioxide waveforms. The physiological parameters were monitored using a Carescape B850 vital signs monitor (GE Healthcare, Helsinki, Finland). All signals were sampled at 200 Hz. The pressure transducer for APB measurement was placed at the level of the tragus16. ICP was monitored with a multimodal sensor (Neurovent PTO, Raumedic AG, Helmbrechts, Germany) measuring ICP, brain tissue partial pressure of oxygen, and brain temperature and logged by a Raumedic MPR 2 logO monitor (Raumedic AG, Helmbrechts, Germany).
Data analysis
The primary data analysis was conducted using ICM+ software. The PRx index was calculated as linear (Pearson’s) moving correlation coefficients between 30 past consecutive 10 s-averaged values of ICP and ABP using a 60 s moving window. For every 300 s, the 30 averaged values of arterial blood pressure and intracranial pressure were available4.
First, all available raw data, sampled with the frequency of 200 Hz, were manually inspected for artifacts. The recognized artifacts were cataloged and described in terms of their shape, duration, incidence, presence in one or both signals, and the percentage of increase or decrease in the signal amplitude (i.e., ABP change from 100 to 125 mmHg was considered a 25% amplitude rise).
Subsequently, data segments including undisturbed blood and intracranial pressure waveforms lasting at least 10 min without any artifacts were identified. The criteria for these segments were ICP 7–15 mmHg with a physiological trifold waveform, mean arterial pressure 90 ± 5 mmHg and PRx below 0.3. In total, twenty 10-min segments fulfilling all these criteria were selected from all available data and used for further analysis.
All selected undisturbed signal segments were exported using csv format into MATLAB (version R2019a, MathWorks, Natick, Massachusetts, USA). In this software, the calculation of the PRx index was conducted in the same standardized manner as in the ICM + software. The most common artifacts were modeled in MATLAB software and inserted into the undisturbed segments of ABP and ICP waveforms. The lengths and amplitudes of individual artifacts were modeled based on the native artifacts.
Into each of these undisturbed segments at the time point of 4 min 1 s, one modeled artifact was inserted. The artifacts were inserted into either one or both pressure signals. Following that, the PRx index was calculated in a standard way. The individual artifacts modeled in MATLAB software are depicted in Supplementary Material 1.
For each of these twenty undisturbed segments, six pairs of PRx indexes were calculated before and after artifact insertion (see Supplementary Fig. 2, S1). In the event of the presence of artifacts lasting less than one minute, just five out of six PRx coefficients were affected by the artifacts. For artifacts lasting more than one minute, all six coefficients were affected, as the artifact had an impact on more segments (see Supplementary Fig. 3, S1). From each segment with an inserted artifact, one PRx value was randomly chosen. This randomly chosen PRx index was then paired with a PRx index from a corresponding part of the undisturbed segment. This process was then repeated for all twenty segments and all defined artifacts.
The first part of the analysis evaluated the main characteristics of the artifacts in the measured signals and consequently their effect on the PRx value. In the second part, the increase in PRx over the limit value was calculated. PRx threshold of 0.3 was considered clinically relevant1,4,17,18.
The sets of computed PRx were tested for normality of distribution using the Lilliefors test. Some sets of PRx coefficients lack the normal distribution. Therefore, Wilcoxon signed-rank test was performed on all data sets. A p-value of < 0.05 was considered significant. The results are expressed as median [interquartile range].
Compliance with ethical standards
The study was approved by the Ethics Committee of the Masaryk Hospital in Usti nad Labem, Czech Republic (Reference number 298/1). The need for patient consent was waived.
Results
Observed artifacts
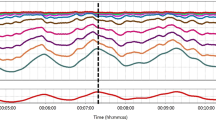
The whole dataset contained two main groups of artifacts, described as “stereotyped” or “complex.” Stereotyped artifacts could have been described in terms of their shape, duration and amplitude. Unlike this, complex artifacts lacked the above mentioned properties and could not be described and characterized for the analysis used in this study. The stereotyped artifacts were categorized according to their shape, as rectangular artifacts, fast impulses, saw tooth-shaped signals, isoline drifts, and constant ICP values (see Fig. 1). In Table 1, the characteristics of the artifacts are presented: the occurrence in the signals of ABP and ICP and parameters of the signals modeled based on these observed artifacts. The average number of artifacts per patient in a 24 h signal segment was 166 with a standard deviation of 41. The lengths and amplitudes of individual artifacts were modeled based on the common duration and shape of the native artifacts. For this reason lengths and amplitudes of the different types of artifacts vary.
The most common artifact appearing solely in the arterial blood pressure signal with a normal ICP waveform was the artifact with a rectangular shape. In some cases, this artifact was present in both signals. The duration of the rectangular artifact was on average 4 s, but a longer time span was also observed.
The fast impulse—lasting only 0.04 s—was frequent in both signals. Only in a minority of data recordings did the fast impulse affect either ABP or ICP signals.
In contrast to the ubiquitous fast impulse and rectangular artifact, the saw tooth signal was recorded only in just a few data segments. It was observed mainly in arterial line signals but also simultaneously in both signals.
An artifact that always occurred in both pressure waveforms was the simultaneous isoline drift. Compared to previously mentioned artifacts, this artifact belonged to the longest noncomplex artifacts, lasting up to 2 min. The identification of this artifact was based on an observation of simultaneous amplitude increases in both ABP and ICP with no apparent periodicity. As this artifact is close to a physiological waveform behavior, the doubtful signal segments were discussed with two clinicians experienced in neurocritical care. Only in cases when both clinicians agreed on the artificial origin of the segments, the signals were evaluated as isoline drifts. In total, 24 doubtful drifts were initially identified and both clinicians agreed on an artificial origin in 4 cases.
The single artifact present only in the intracranial pressure waveform was the constant value of ICP, lasting 3 to 4 s. The displayed constant value was within the pressure range recorded before this artifact appeared but with a complete loss of the typical trifold waveform.
Artifact effect analysis
Four artifacts were inserted into both signals—arterial and intracranial pressure: the rectangular artifact, the fast impulse, the saw tooth artifact and the isoline drift. Even the shortest and smallest rectangular artifact lasting 4 s with only a 25% increase in amplitude caused an increase in PRx over 0.3 (PRx 0.45 [0.26–0.59]) in more than half of the samples (55.4%). For longer artifacts lasting 15 s and more, the PRx reached the set threshold in all cases—very often the correlation coefficient was close to 1.0 (for 15 s long artifact: PRx 0.88 [0.81–0.93]) (Fig. 2). This behavior was even more pronounced in the presence of the saw tooth artifact, in which the rise of the amplitude of 30% caused a surge of the PRx index to 1.0 in all cases, regardless of how long the artifact was (30, 45, or 60 s). Compared to the previous two artifacts, the isoline drift caused a significant change in the PRx index only when the drift lasted at least 1 min and the baseline ascended by nearly a third; in these cases, more than one-fifth of the PRx coefficients (21.6%) reached a value above 0.3. The most common artifact—the fast impulse—did not show a statistically significant change in the PRx index for all simulated amplitudes when inserted only into ABP or into both signals.
The effect of the rectangular artifact on PRx value. Even the shortest artifact of this shape present in both signals causes a significant change in the PRx index; when the artifact is prolonged to 15 s, the PRx index approaches 1.0. Box-and-whisker plots representing the median value, with 50% of all data falling within the box (interquartile range). The "whiskers'' extend to the minimum and maximum. Cross inside the box represents the mean value. (a) Box plots depicting the effect of rectangular artifacts lasting 4 s with an amplitude rise of 25% in the arterial blood pressure waveform and in both waveforms. (b) Box plots depicting the effect of rectangular artifacts lasting 15 s with an amplitude rise of 25% in the arterial blood pressure waveform and in both waveforms.
The artifacts inserted only into one of the signals showed an unalike behavior. The rectangular artifact in ABP revealed a set threshold value of PRx in maximum at 4.3% (30 s duration with amplitude rise 75–100%); even in the longest and tallest artifact (60 s long with 100% amplitude rise), the occurrence of the critical PRx value was in 2.9%. A similar behavior was observed for saw tooth artifacts, with the highest increase to critical PRx value in just 4.3% of the cases. These results are different compared to the presence of artifacts in both signals, where the surge of a PRx index over 0.3 occurs in all cases (see Supplementary Table S1, S2).
The only artifact simulated solely in the intracranial pressure was a constant value of ICP for 4 s, where the change in the PRx index did not reach the critical value and the change in the PRx index was not statistically significant (p = 0.16).
Discussion
The main finding of this study is that the effect of artifacts on PRx is variable depending on their shape, duration, and presence in one or both signals. The most common artifact—the fast impulse—does not have a significant effect on the calculated PRx value, even when present in both signals—ABP and ICP. Although this artifact is generally easily detectable by manual inspection or by automatic artifact detection systems, the negligible effect on the PRx calculation suggests that removal of this artifact is not critical for signal analysis.
On the other hand, even a 4 s-long rectangular artifact with a 25% rise in amplitude present in both signals significantly affects the PRx value. With increasing duration of the artifact, reaching 15 s or more, the PRx in all studied cases reached nearly 1.0. Moreover, due to the length of the moving calculation window (300 s), even this 4-s-long artifact in both signals affects the PRx calculation for 5 min (see Fig. 3).
The presented results show that despite the 10-s averaging window, an artifact in both signals is prone to change the PRx towards values over 0.3, suggesting disturbed cerebral autoregulation, which can have significant consequences for treatment strategy. For an alteration of the PRx index, not only the amplitude but also the duration of the artifact in the source biosignals is important.
When artifacts occur in both signals, they can alter the PRx even if the artifacts last only a couple of seconds with an amplitude increase of tens of percent. The authors hypothesized that the larger the area under the curve (AUC) of the artifact, the larger the impact on the correlation coefficient calculation. However, in the presence of the artifact in both signals, the importance of the area of the artifact is less pronounced. Importantly, except for the fast impulse, an artifact in both signals routinely changes the PRx towards 1.0 (Supplementary Fig. 4, S1), which is clinically consequential. Thus, these artifacts are worth removing.
Some of the artifacts can be removed using an automatic or a manual tool embedded, for instance, in the ICM+ software. However, even the artifacts discovered by the automatic removal tools are usually reviewed by a researcher or a clinician which is a laborious work and suitable mainly for a post hoc offline analysis only.
Differentiation of the artifact from a physiological signal is challenging. Pasma et al.13 compared the algorithmic and manual annotation of artifacts in arterial blood pressure signals during anesthesia. There was a significant discrepancy among the direct observation of the artifacts and the retrospective analysis or the detection using machine learning algorithms. Although the data presented in this study were analyzed only retrospectively and without any clinical information about potential sources of artifacts, several artifacts necessitated two experienced physicians to decide about their artificial or physiological origin.
The results support the proposed concept of automatic online artifact detection systems15. Such a system allows not only the detection but also the bridging of these segments, so the final reliable results of advanced calculations are presented to the clinician at the bedside.
Lee et al.15 suggested that all segments with artifacts, regardless of whether they occur in ABP, ICP, or both signals, should be simultaneously removed due to their potential effect on the reliability of the composite parameters, such as cerebral perfusion pressure (CPP) and PRx. However, our results propose that some of the simple artifacts do not affect the PRx values significantly; thus, their removal is not crucial. Moreover, a global removal of signals can cause loss of important clinical information.
The 'clarity' of the signals and the calculated parameters used in the management of patients with intracranial hypertension can significantly increase the prognostic potential and future clinical value of these parameters. Lee et al. also hypothesized that some clinical events, such as intracranial hypertension and cerebral hypoperfusion, might be in reality less frequent, as seen in biosignals following artifact removal. Thus, the effect of the artifacts might be greater than previously expected15.
For this study we have classified artifacts as “stereotyped” or “complex”. Stereotyped artifacts could have been described in terms of their shape, duration and amplitude and thus modeled in MATLAB software for a subsequent analysis. Unlike this, complex artifacts lacked the above-mentioned properties and could not be described and characterized for analysis method used in this study.
The complex artifacts are likely of multifaceted origin and detailed investigation without well clinically annotated signal records is deemed impossible by the study team. We hypothesize, that they—at least in part—origin from the nursing care (patient suctioning, positioning or overall care) or from physiological phenomena like coughing. Additionally, the goal was not to categorize the artifact types according to their cause but to find some common waveform patterns among them. Studies with a systematic recording and assessment of the potentially disturbing situations which may lead to artifact generation should help us better understand the causes of these artifacts. The authors propose that finding the cause of an artifact is less important than properly identifying it and treating it in data management.
Moreover, this study suggests that certain types of artifacts can have a significant effect on PRx calculation, thus possibly affecting its value as a research or clinical tool. Various strategies to deal with artifacts have been proposed, from retrospective manual removal, simple logic filtering to machine learning or artificial intelligence approach12,13,14,15. Based on available evidence, no universal strategy can be proposed. Artifact treatment remains a significant challenge for future research in this field.
The current study has several limitations. First, only raw data were analyzed, and detailed information about the patients (e.g., their age, sex, diagnosis, outcome, etc.) was not available. This makes the correlation between the effect of the artifacts and the outcome impossible. However, this study was focused solely on the effects of artifacts on PRx itself, which does not require any further patient data.
Second, the modeled artifacts were applied on undisturbed segments where cerebrovascular pressure autoregulation (CAR) was still preserved to some extent, as documented by the PRx values below 0.3. The effect on signals with ICP over 15 mmHg was not assessed. On the other hand, patients with intracranial pathology, yet with preserved CAR, are also vulnerable to incorrect treatment potentially based on artifact-affected parameters. However, further research of artifact effect on ICP signals in case of elevated intracranial pressure or pathological morphology of ICP waveform is needed.
Conclusions
Our study shows that the effect of artifacts on PRx calculation is variable. While the most frequent artifacts—fast impulses—are easily detectable and can be automatically removed, they do not significantly alter the value of PRx. Other artifacts that significantly affect PRx are mainly the artifacts present in both signals—ABP and ICP—except for fast impulse. Even four-second-long rectangular artifacts that occur in both signals with a small amplitude rise cause substantial changes in PRx above the threshold value of 0.3.
Most of the artifacts analyzed in this study affect the PRx value. This study underlines the need for careful artifact treatment prior PRx calculation, as certain types artifacts can have significant impact on PRx value, possibly leading to faulty data interpretation. However, the present results suggest that not all artifacts have the same effect on the PRx calculation, and potentially, not all of them have to be removed via laborious work.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Sorrentino, E. et al. Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit. Care 16, 258–266 (2002).
Beqiri, E. et al. Feasibility of individualised severe traumatic brain injury management using an automated assessment of optimal cerebral perfusion pressure: The COGiTATE phase II study protocol. BMJ Open 9, e030727 (2019).
Tas, J. et al. An update on the COGiTATE phase II study: Feasibility and safety of targeting an optimal cerebral perfusion pressure as a patient-tailored therapy in severe traumatic brain injury. Acta. Neurochir. Suppl. 131, 143–147 (2021).
Czosnyka, M., Czosnyka, Z. & Smielewski, P. Pressure reactivity index: Journey through the past 20 years. Acta Neurochir. 159(11), 2063–2065 (2017).
Dias, C. et al. Optimal cerebral perfusion pressure management at bedside: A single-center pilot study. Neurocrit. Care 23(1), 92–102 (2015).
Smielewski, P. et al. ICM+: Software for on-line analysis of bedside monitoring data after severe head trauma. In Intracranial Pressure and Brain Monitoring XII, 43–49 (2005).
Smielewski, P. et al. ICM+, a flexible platform for investigations of cerebrospinal dynamics in clinical practice. Acta Neurochir. Suppl. 102, 145–151 (2008).
Li, Q., Mark, R. & Clifford, G. Artificial arterial blood pressure artifact models and an evaluation of a robust blood pressure and heart rate estimator. Biomed. Eng. Online 8, 13 (2009).
Son, Y. et al. Automated artifact elimination of physiological signals using a deep belief network: An application for continuously measured arterial blood pressure waveforms. Inf. Sci. 456, 145–158 (2018).
Zong, W., Moody, G. B. & Mark, R. G. Reduction of false arterial blood pressure alarms using signal quality assessment and relationships between the electrocardiogram and arterial blood pressure. Med. Biol. Eng. Comput. 42(5), 698–706 (2004).
Sun, J. X., Reisner, A. T. & Mark, R. G. A signal abnormality index for arterial blood pressure waveforms. Comput. Cardiol. 33, 13–16 (2006).
Zhang, P., Liu, J., Wu, X., Liu, X. & Gao, Q. A novel feature extraction method for signal quality assessment of arterial blood pressure for monitoring cerebral autoregulation. In 4th International Conference on Bioinformatics and Biomedical Engineering, 1–4 (2010).
Pasma, W., Wesselink, E. M., van Buuren, S., de Graaff, J. C. & van Klei, W. A. Artifacts annotations in anesthesia blood pressure data by man and machine. J. Clin. Monit. Comput. 35(2), 259–267 (2021).
Cao, H., Norris, P., Ozdas, A., Jenkons, J. & Morris, J. A. A simple non-physiological artifact filter for invasive arterial blood pressure monitoring: A study of 1852 trauma ICU patients. In International Conference of the IEEE Engineering in Medicine and Biology Society, 1417–1420 (2006).
Lee, S. B. et al. Artifact removal from neurophysiological signals: Impact on intracranial and arterial pressure monitoring in traumatic brain injury. J. Neurosurg. 132(6), 1952–1960 (2019).
Thomas, E., Czosnyka, M. & Hutchinson, P. Calculation of cerebral perfusion pressure in the management of traumatic brain injury: Joint position statement by the councils of the Neuroanaesthesia and Critical Care Society of Great Britain and Ireland (NACCS) and the Society of British Neurological Surgeons (SBNS). Brit. J. Anaesth. 115, 487–488 (2015).
Steiner, L. A. et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit. Care Med. 30(4), 733–738 (2002).
Zweifel, C. et al. Continuous monitoring of cerebrovascular pressure reactivity in patients with head injury. Neurosurg. Focus 25, 10 (2008).
Acknowledgements
The authors would like to thank Eva Wittenbergova, Julie Stelmach, and Stanislav Polansky from the Department of Anesthesia, Perioperative Medicine and Intensive Care, Masaryk Hospital in Usti nad Labem for their help with data acquisition and David Slajfercik from the Faculty of Biomedical Engineering, Czech Technical University in Prague for his contribution to data processing.
Funding
This work was supported by the Grant Agency of the Czech Technical University in Prague, Grants Nos. SGS22/202/OHK4/3T/17 and SGS20/202/OHK4/3T/17.
Author information
Authors and Affiliations
Contributions
M.R., J.S., L.H., V.T. contributed to study design. J.S. and L.H. provided data acquisition. M.R., L.H., V.T. performed the statistical analysis. M.R., J.S., L.H., V.T. oversaw the interpretation of results. L.H., V.T. did the literature review and wrote the manuscript. All authors critically reviewed the final draft of the manuscript and have given approval for the version submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rozanek, M., Skola, J., Horakova, L. et al. Effect of artifacts upon the pressure reactivity index. Sci Rep 12, 15131 (2022). https://doi.org/10.1038/s41598-022-19101-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19101-y
This article is cited by
-
CPPopt on Medical Devices: The Imitation Game
Neurocritical Care (2024)
-
Continuous monitoring of the lower limit of reactivity in traumatic brain injury patients: understanding what is feasible
Critical Care (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.