Abstract
To evaluate the prognostic role of the preoperative plasma lipid profile, including triglycerides (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) in patients with lung squamous cell carcinoma (LUSC) who underwent complete resection. Clinical data, including preoperative plasma profile levels, were retrospectively collected and reviewed in 300 patients with LUSC who underwent radical lung resection between 2016 and 2017. The overall survival (OS) and disease-free survival (DFS) were assessed by the Kaplan–Meier method and the Cox proportional hazards regression model. TG ≤ 1.35, HDL-C ≤ 1.17, and LDL-C ≤ 2.32 were deemed as independent preoperative risk factors for OS, and HDL-C ≤ 1.17 was an independent preoperative risk factor for DFS. In the multivariate analyses involving OS and DFS, a decreased HDL-C level was significantly associated with worse OS (HR, 0.546; 95% CI, 0.380–0.784, P = 0.001) and DFS (HR, 0.644; 95% CI, 0.422–0.981, P = 0.041). Additionally, an increased TG (HR, 0.546; 95% CI, 0.366–0.814, P = 0.003) or LDL-C (HR, 0.652; 95% CI, 0.456–0.933, P = 0.019) level was significantly associated with better OS. In patients with LUSC, decreased levels of HDL-C may predict worse outcomes for both DFS and OS, while increased TG or LDL-C levels may predict better OS.
Similar content being viewed by others
Introduction
Non-small cell lung cancer (NSCLC), which accounts for a majority of cases of lung cancer, is a primary subtype responsible for a predominant proportion of cancer-related deaths worldwide with an increasing incidence rate1. As a histology of NSCLC, lung squamous cell carcinoma (LUSC) accounts for 20–30% of all lung cancers2. While a high rate of recurrence after complete resection is a significant prognostic factor, the risk of metastasis and recurrence after surgery for patients with LUSC is high. To date, a variety of biomarkers have been shown to predict clinical outcomes in patients with LUSC3,4. For example, Masuda et al. found that laminin-5γ2 chain expression is associated with tumor cell invasiveness and patient prognosis of LUSC5 and Okabe et al. suggested that family with sequence similarity 83, member A (FAM83B) is a novel biomarker for the diagnosis and prognosis in LUSC6. Due to complicated detection equipment and expensive costs, the development of accurate, fast, and convenient predictive biomarkers for the identification of patients with a high risk of metastasis and recurrence is emerging as a significant area of investigation and may present an opportunity for improving clinical prognosis and postoperative quality of life.
Patients with cancer often present with an altered serum lipid profile. Findings from previous studies have demonstrated that a high level of serum triglycerides (TG) increases the risk of lung cancer7,8. Chen et al. reported a possible association between serum total cholesterol (TC) and increased risk of pancreatic carcinoma9, and Kitahara et al. showed a lower risk of lung cancer in males with higher serum TC than in the general population10. Additionally, studies have associated low high-density lipoprotein cholesterol (HDL-C) levels with an increased risk of postmenopausal breast cancer11,12, and the similar result has been described in patients with lung cancer13. A prospective cohort study of Chinese men showed that low levels of low-density lipoprotein cholesterol (LDL-C) is implicated in an increased risk of lung cancer8. Moreover, several recent studies have confirmed that dyslipidemia is associated with an increased risk of tumor recurrence and reduced survival for several types of cancer9,14. Such expositions are unsatisfactory because they do not fully explain the role of lipid metabolism in cancer development, with little evidence about the impact of lipid profiles on clinical outcomes in patients with LUSC.
Our study attempted to show the predictive role of the lipid profile on overall survival (OS) and disease-free survival (DFS) in patients with LUSC who underwent complete lung resections.
Methods
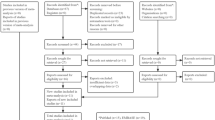
Patient selection
We collected and reviewed clinical data including the preoperative plasma profile levels of 300 patients with LUSC who underwent complete lung resections at Shaoxing People’s Hospital from 2016 through 2017. The study protocol was approved by the Ethics Committee of Human Experimentation in China, and all methods were performed in accordance with the relevant guidelines and regulations. All patients provided written informed consent before participation. All patients met the following eligibility criteria: (1) diagnosis of pathologically confirmed LUSC; (2) no history of cancer; (3) no treatment (including anti-cancer treatment or any other treatment that may affect blood lipids) before the serum had been obtained; and (4) collection of serum samples completed before surgery. All pathological diagnoses were independently confirmed by experienced pathologists at Shaoxing People’s Hospital.
Patient follow-up
All patients were followed up in the clinic, and 10 patients were lost to follow up before the study was discontinued. Physical examination and laboratory blood draws were conducted every 3–6 months in the first 2 years and every 6–12 months from the third to the fifth year. The main outcome of this study was OS, defined as the time from curative resection to death. The secondary outcome was DFS, calculated from the date of radical surgery to the date of disease recurrence or diagnosis of distant metastasis14.
Statistical analysis
Continuous variables are shown as means ± standard deviation (SD). The optimal cut-off values for the lipid profile determined by statistical analysis of the receiver operating characteristic (ROC) curve were used to dichotomize lipids for chi-square test and cox proportional analyses14. The Kaplan–Meier method and log-rank test were used to calculate the survival curve. The risk factors for survival were identified using the Cox proportional hazards model. The association between serum lipid levels and clinicopathological parameters (age, gender, smoking State, drinking state, T stage, lymph node metastasis, TNM stage, recurrence, and death) was tested with the chi-square test. In all statistical methods, P < 0.05 was considered significant. Data analyses were performed on SPSS 20.
Patient study
The study has been approved by the academic ethics committee of Shaoxing People's Hospital and patients gave their informed consent before material was obtained for use in the study.
Results
Patient characteristics
After the eligibility review, 300 patients with LUSC who had undergone radical surgical resection were enrolled in the analysis, with their characteristics being presented in Table 1. The median follow-up time was 39 months (range: 1–70 months). The median age at resection was 60 years (range: 40–81 years), and 284 (94.7%) of the patients were male and 16 (5.3%) were female. Cancer staging was conducted according to the tumor-node-metastasis (TNM) classification for LUSC. A total of 212 patients (70.7%) were diagnosed with stage I–II disease and 88 (29.3%) were diagnosed with stage III–IV disease. A total of 138 patients (46%) died during follow-up and 109 patients (36.3%) had disease recurrence or distant metastasis.
Preoperative plasma profile levels in 300 patients with LUSC
The relationship between preoperative plasma lipid profile levels and clinical parameters was analyzed (Table 2). TG level was identified to be up-regulated in patients with a higher T stage (P = 0.001) or TNM stage (P = 0.015) compared to those with a lower T stage or TNM stage. A higher HDL-C level was closely correlated with females (P = 0.008) and no smoking stage (P = 0.002). In addition, TG (P = 0.004) and TC (P = 0.047) levels were lower in patients with death status. Other clinical parameters were not significantly associated with preoperative plasma lipid profile levels, such as drinking state, lymph node metastasis, and recurrence (p > 0.05).
The Survival Rate of Patients with Increased TG or TC Levels Is Significantly Higher Than That of Patients with Decreased Levels of TG or TC.
The Kaplan–Meier analysis results are depicted in Fig. 1. The patients with TG, TC, HDL-C, or LDL-C higher than the median were assigned to the high expression group; the other patients were assigned to the lower expression group. The OS rate was significantly higher in the TG (p = 0.006, cut-off value = 1.14) or TC (p = 0.008, cut-off value = 4.01) high expression group. In addition, the OS rate was also higher in the HDL-C or LDL-C high expression group although the difference was not significant (p > 0.05).
We then defined patients with LUSC with TG higher than 1.7 mmol/l, TC higher than 5.2 mmol/l, HDL-C higher than 1.04 mmol/l or LDL-C higher than 3.12 mmol/l as lipid disorder group, and others as normal group. The Kaplan–Meier analysis results are plotted in Fig. 2. The OS rate was significantly higher in the TG (p = 0.011, cut-off value = 1.7) or TC (p = 0.037, cut-off value = 5.2) disorder group. In addition, the OS rate was also higher in the HDL-C or LDL-C disorder group although the difference was not significant (p > 0.05).
To investigate the potential of preoperative blood lipid level as a prognostic marker, survival Receiver operating curve (ROC) method was introduced to determine the optimal cutoff value.
Optimal cut-off determination of lipid metabolism
ROC analysis presented that the optimal cutoff value for TG was 1.35 mmol/L (AUC 0.588, 95% CI 0.530–0.644), 3.93 mmol/L for TC (AUC 0.578, 95% CI 0.520–0.634), 1.17 mmol/L for HDL (AUC 0.551, 95% CI 0.493–0.609), and 2.32 mmol/L for LDL (AUC 0.547, 95% CI 0.489–0.605).
The association of TG, HDL-C, and LDL-C levels with clinical characteristics
The relationships between the clinicopathological features of LUSC and TG, HDL-C, and LDL-C levels are summarized in Tables 3, 4 and 5. The Chi-square test showed the TG level was significantly related to the tumor (T) stage (P = 0.003), TNM stage (P = 0.008), and death (P = 0.002) (Table 3). However, no significant associations were reported between TG levels with other clinicopathological parameters, including smoking status, lymph node metastasis, and tumor recurrence (all P > 0.05; Table 3). The HDL-C level was significantly associated with sex (P = 0.020), smoking status (P = 0.002), tumor recurrence (P = 0.031), and death (P = 0.013) (Table 4). The LDL-C level was significantly associated with death (P = 0.014; Table 5).
The prognostic significance of clinical characteristics in LUSC
In the univariate analyses, a significant correlation between T stage, lymph node metastasis, TNM stage, levels of TG, TC, HDL-C, and LDL-C, and OS were detected. Additionally, we found a correlation between T stage, TNM stage, HDL-C levels, and DFS. In multivariate analysis, we observed significant associations of T stage, LNM, and levels of TG, HDL-C, and LDL-C with OS (Table 6). In addition, associations between T stage and HDL-C levels with DFS were observed (Table 7). The multivariate analysis was conducted based on age at resection, sex, smoking status, drinking status, T stage, lymph node metastasis, TNM stage, and levels of TG, TC, HDL-C, and LDL-C.
The prognostic significance of the serum lipid profile in LUSC
Among the 300 patients, 102 of 194 (52.6%) patients had a TG level ≤ 1.35 mmol/L, and 36 of 106 (34.0%) patients had a TG level > 1.35 mmol/L (P = 0.002); 74 of 135 (54.8%) patients had a TC level ≤ 3.93 mmol/L, and 64 of 165 (38.8%) patients had a TC level > 3.93 mmol/L (P = 0.006); 92 of 177 (52.0%) patients had an HDL-C level ≤ 1.17 mmol/L, and 46 of 123 (37.4%) patients had an HDL-C level > 1.17 mmol/L (P = 0.013); 56 of 100 (56.0%) patients had an LDL-C level ≤ 2.32 mmol/L, and 82 of 200 (41.0%) patients had an LDL-C level > 2.32 mmol/L (P = 0.014) who died. In the univariate Cox proportional analysis, a decreased TG (HR, 0.497; 95% CI, (0.340–0.728), P = 0.000), HDL-C (HR, 0.639; 95% CI, (0.449–0.911), P = 0.013), or LDL-C (HR, 0.642; 95% CI, (0.457–0.903), P = 0.011) level was significantly associated with decreased OS (Table 6; Fig. 3) and this finding remained significant in the multivariate analysis (HR, 0.546; 95% CI, 0.380—0.784, P = 0.001) that included T stage and lymph node metastasis. In addition, an increased TC level (HR, 0.621; 95% CI, (0.444–0.868), P = 0.005; Table 6; Fig. 3) and III-IV TNM stage (HR, 0.404; 95% CI, (0.288–0.566), P = 0.000) were statistically linked with increased OS in the univariate Cox proportional analysis. However, in the multivariate analysis, TC levels were not statistically significant including TNM stage (P > 0.05; Table 6). Other clinical parameters showed no significant difference in the results from either the univariate or multivariate analysis, such as gender and smoking state (P > 0.05; Table 6).
Regarding DFS, local recurrence or distant metastasis after radical surgical resection was diagnosed in 76 of 187 (40.6%) patients with a TG level ≤ 1.35 mmol/L and in 33 of 103 (32.0%) patients with a TG level > 1.35 mmol/L (P > 0.05); in 55 of 129 (42.6%) patients with a TC level ≤ 3.93 mmol/L and in 54 of 161 (33.5%) patients with a TC level > 3.93 mmol/L (P > 0.05); in 73 of 171 (42.7%) patients with an HDL-C level ≤ 1.17 mmol/L and in 36 of 119 (30.3%) patients with an HDL-C level > 1.17 mmol/L (P = 0.031); in 38 of 96 (39.6%) patients with an LDL-C level ≤ 2.32 mmol/L and in 71 of 194 (36.6%) patients with an LDL-C level > 2.32 mmol/L (P > 0.05). In the univariate Cox proportional analysis, A decreased HDL-C (HR, 0.650; 95% CI, (0.426–0.990), P = 0.045; Table 7; Fig. 4) level was significantly correlated with decreased DFS and the significance of this finding remained in the multivariate analysis (HR, 0.546; 95% CI, 0.380–0.784, P = 0.001) including the T stage. In addition, III-IV TNM stage was statistically linked with increased DFS (HR, 0.518; 95% CI, (0.344–0.779), P = 0.002), although there was no statistical significance of TNM stage in the multivariate analysis (P > 0.05; Table 7). TG, TC, and HDL-C showed no significant difference in the results from either the univariate or multivariate analysis (Table 7; Fig. 4) including age, gender, smoking state, and drinking State (P > 0.05; Table 7).
Discussion
In view of the poor prognosis of patients with LUSC and the high tumor recurrence rate after resection, investigations on risk factors for tumor prognosis and recurrence are warranted, so as to support early intervention, improve monitoring, reduce tumor recurrence rate, and prolong patient survival time15,16. On account of the close relationship between blood lipids and tumorigenesis or tumor recurrence, we were interested to see if a relationship existed between lipid profile and the prognosis of Chinese patients with LUSC.
In our present study, the result that a lower TG level indicated a poorer prognosis in patients with LUSC and was associated with advanced cancer stages may be elucidated by the poor nutritional status and high-energy consumption of patients with advanced tumors17,18. The present study suggests, for the first time, an association of a low TG level with reduced survival of lung cancer.
Additionally, we manifested that lower TC levels indicated a poor OS in patients with LUSC. Cholesterol is essential for maintaining the integrity, fluidity, and function of the cell membrane, including signal transduction19,20. Low cholesterol has been proposed to be associated with suppressed immunity, upregulated activity or responsiveness of the mevalonate pathway and increased activity of nuclear transcription factor NF-κB, promoting the initiation and progression of cancer8. High cholesterol levels reduce the risk of death in patients with advanced NSCLC who have the epidermal growth factor receptor (EGFR) gene mutation21, which is line with our results. But the question of whether TC is an independent risk factor for the prognosis of patients with LUSC warrants further study.
There is emerging evidence that HDL-C may be linked to the tumorigenesis and progression of cancers14,22. The initial observations prompted us to investigate the relation between HDL-C and LUSC. We revealed that increased pre-operative plasma HDL-C levels were associated with increased DFS and OS after radical surgery. Lower HDL-C levels were related to sex and smoking status but not cancer stages. Additional support for the role of HDL-C comes from recent publications, which demonstrated that HDL-C may affect the occurrence of cancer by participating in the reverse transport of cholesterol23, affecting the entry into the cell cycle24, and regulating apoptosis and inflammatory response25,26. From previous studies, two possible molecular mechanisms have been suggested for the relation between HDL-C and the relapse of LUSC and poor survival. Serum HDL-cholesterol levels are negatively associated with cholesterol levels in the tumor tissues of patients, revealing the possibility that lower HDL levels are resulted from the increased cholesterol metabolism in the tissue of proliferating tumors27. The other is that the increase in HDL level is related to the decrease of pro-inflammatory cytokines that can promote cell proliferation and inhibit apoptosis, and also related to the increase of anti-inflammatory cytokines28,29.
LDL-C is another major indicator for monitoring lipoprotein cholesterol in addition to HDL-C. Our study found that low expression of LDL-C in patients with LUSC was substantially associated with poor OS. Although there are limited reports on the relationship between LDL-C and the prognosis of tumor patients, Zhou et al. observed that higher LDL level is an important independent prognostic factor for poor OS in patients with small-cell lung cancer30. The inconsistency of the role of LDL level may be due in part to the different pathological basis of LUSC and small cell lung cancer. Furthermore, the treatment of LUSC is mainly surgery in our study, while either radiotherapy or chemotherapy is used for treating small cell lung cancer in the study of Zhou et al.30.
Previous studies have demonstrated that most patients with non-small cell lung cancer suffer from malnutrition19. In addition, even patients with normal nutrition may suffer from malnutrition in the early postoperative period, which may lead to poor wound healing and reduced immunity after surgery, resulting in an increased risk of postoperative complications including bronchial leakage, postoperative infection, respiratory asthenia, and ultimately poor OS and progression-free survival31,32. Lipids, as an essential nutrient of human body, the absence of which can slow down or even stop all functions of human body. This will lead to the increased incidence rate and mortality.
Being limited to this retrospective study, blood lipids were not measured again after surgery. Another deficiency existed that some patients with hyperlipidemia received lipid-lowering treatment after surgery. At present, a much debated issue is that whether taking statins after surgery can improve the prognosis of lung cancer patients. Whilst some studies have proven that taking statins before diagnosis can reduce the specific mortality of lung cancer patients and prolong the survival time of patients33,34, some other scholars believe no superiority of taking statins over no-statins in lowering risk of lung cancer35.
Conclusions
In summary, our research indicated that blood lipid levels were substantially correlated with LUSC generation and development and may be helpful in the identification of, and follow-up in, high-risk patients with LUSC. Therefore, TG, HDL-C, and LDL-C levels at diagnosis can be considered prognostic factors for LUSC.
Data availability
The data used to support the findings of this study is included in the article and supplementary file.
References
Herbst, R. S. et al. The biology and management of non-small cell lung cancer. Nature 553, 446 (2018).
Li, R. et al. Identification of a prognostic model based on immune-related genes of lung squamous cell carcinoma. Front. Oncol. 10, 1588 (2020).
Yan, Y. et al. Identification of an immune gene expression signature for predicting lung squamous cell carcinoma prognosis. Biomed. Res. Int. 2020, 1–12 (2020).
Martínez-Terroba, E. et al. 5 protein-based signature for resectable lung squamous cell carcinoma improves the prognostic performance of the TNM staging. Thorax 74, 371 (2018).
Masuda, R. et al. Laminin-5γ2 chain expression is associated with tumor cell invasiveness and prognosis of lung squamous cell carcinoma. Biomed. Res. 33, 309 (2012).
Okabe, N. et al. FAM83B is a novel biomarker for diagnosis and prognosis of lung squamous cell carcinoma. Int. J. Oncol. 46, 999–1006 (2015).
Lin, X. et al. Blood lipids profile and lung cancer risk in a meta analysis of prospective cohort studies. J. Clin. Lipidol. 11, 1073 (2017).
Lyu, Z. et al. Independent and joint associations of blood lipids and lipoproteins with lung cancer risk in Chinese males: A prospective cohort study. Int. J. Cancer 144, 2972 (2018).
Chen, X., Zhou, T. & Chen, M. Meta analysis of the association of cholesterol with pancreatic carcinoma risk. J. Buonoff. J. Balkan Union Oncol. 20, 109–113 (2015).
Kitahara, C. M. et al. Total cholesterol and cancer risk in a large prospective study in Korea. J. Clin. Oncol. 29, 1592 (2011).
Moorman, P. G. et al. Association between high-density lipoprotein cholesterol and breast cancer varies by menopausal status. Cancer Epidemiol. Biomark. Prevent. 7, 483–488 (1998).
Alexopoulos, C. G., Blatsios, B. & Avgerinos, A. Serum lipids and lipoprotein disorders in cancer patients. Cancer 60, 3065–3070 (1987).
Siemianowicz, K. et al. Serum HDL cholesterol concentration in patients with squamous cell and small cell lung cancer. Int. J. Mol. Med. 6, 307–311 (2000).
Shan-Shan, J. et al. The clinical significance of preoperative serum cholesterol and high-density lipoprotein-cholesterol levels in hepatocellular carcinoma. J. Cancer 7, 626–632 (2016).
Wang, Y. et al. Human sperm-associated antigen 4 as a potential prognostic biomarker of lung squamous cell carcinoma. J. Int. Med. Res. 49, 030006052110328 (2021).
Long, J. et al. Combination of body mass index and oxidized low density lipoprotein receptor 1 in prognosis prediction of patients with squamous non-small cell lung cancer. Oncotarget 6, 22072–22080 (2015).
Wang, Z. et al. Pretreatment prognostic nutritional index as a prognostic factor in lung cancer: Review and meta-analysis. Clin. Chim. Acta 486, 303 (2018).
Nakayama, T. et al. Prognostic impact of preoperative psoas muscle index as nutritional status on patients with esophageal cancer receiving neoadjuvant therapy. Nutrition 90, 111232 (2021).
Trestini, I. et al. Nutritional derangements in non-small cell lung cancer patients: Prevalence and impact on treatment outcome. Nutrition 75–76, 110908 (2020).
Ihara, A. et al. Cholesterol regulates DAF-16 nuclear localization and fasting-induced longevity in C. elegans. Exp. Gerontol. 87, 40–47 (2016).
Zhang, Y. et al. Pretreatment direct bilirubin and total cholesterol are significant predictors of overall survival in advanced non-small-cell lung cancer patients with EGFR mutations. Int. J. Cancer 140, 1645–1652 (2017).
Zhao, W. et al. HDL cholesterol and cancer risk among patients with type 2 diabetes. Diabetes Care 37, 3196–3203 (2014).
Pommier, A. et al. Liver X receptor activation downregulates AKT survival signaling in lipid rafts and induces apoptosis of prostate cancer cells. Oncogene 29, 2712–2723 (2010).
Nofer, J. R. et al. High density lipoproteins induce cell cycle entry in vascular smooth muscle cells via mitogen activated protein kinase-dependent pathway. Thromb. Haemost. 85, 730–735 (2001).
Eckardstein, A. V., Hersberger, M. & Rohrer, L. Current understanding of the metabolism and biological actions of HDL. Curr. Opin. Clin. Nutr. Metab. Care 8, 147–152 (2005).
Nofer, J. R. et al. Suppression of endothelial cell apoptosis by high density lipoproteins (HDL) and HDL-associated lysosphingolipids. J. Biol. Chem. 276, 34480 (2001).
Dessì, S. et al. Cholesterol content in tumor tissues is inversely associated with high-density lipoprotein cholesterol in serum in patients with gastrointestinal cancer. Cancer 73, 253–258 (2015).
Esteve, E., Ricart, W. & Fernández-Real, J. Dyslipidemia and inflammation: An evolutionary conserved mechanism. Clin. Nutr. 24, 16–31 (2005).
Yvan-Charvet, L., Wang, N. & Tall, A. R. Role of HDL, ABCA1, and ABCG1 transporters in cholesterol efflux and immune responses. Arterioscler. Thromb. Vasc. Biol. 30, 139–143 (2009).
Zhou, T. et al. Serum low-density lipoprotein and low-density lipoprotein expression level at diagnosis are favorable prognostic factors in patients with small-cell lung cancer (SCLC). BMC Cancer 17, 269 (2017).
Kaya, S. O. et al. Is preoperative protein-rich nutrition effective on postoperative outcome in non-small cell lung cancer surgery? A prospective randomized study. J. Cardiothorac. Surg. 11, 1–8 (2016).
Pascal, A. T. et al. National perioperative outcomes of pulmonary lobectomy for cancer: The influence of nutritional status. Eur. J. Cardiothorac. Surg. 4, 652–659 (2014).
Cardwell, C. R. et al. Statin use and survival from lung cancer: A population-based cohort study. Cancer Epidemiol. Biomark. Prevent. 24(5), 833–841 (2015).
Lin, J. J. et al. The effect of statins on survival in patients with stage IV lung cancer. Lung Cancer 99, 137–142 (2016).
Hamelin, B. A. & Turgeon, J. Hydrophilicity/lipophilicity: Relevance for the pharmacology and clinical effects of HMG-CoA reductase inhibitors. Trends Pharmacol. Sci. 19(1), 26–37 (1998).
Acknowledgements
We thank LetPub (https://www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Funding
This study was funded by Zhejiang medical and health science and technology projects (grant number 2020KY321 and 2020KY331).
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Z.L., Jianfeng Xu, Weizhong Feng (II) Administrative support: J.Z., G.Y. (III) Provision of study materials or patients: Z.L., J.X., W.F. (IV) Collection and assembly of data: P.X., L.D., J.Yi D. (V) Data analysis and interpretation: Z.L., Jianfeng Xu (VI) Manuscript writing: All authors (VII) Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Z., Xu, J., Feng, W. et al. The clinical significance of preoperative serum triglyceride, high-density lipoprotein, and low-density lipoprotein levels in lung squamous cell carcinoma. Sci Rep 12, 16828 (2022). https://doi.org/10.1038/s41598-022-18589-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18589-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.