Abstract
This study aimed to establish a nomogram for the prediction of cancer-specific survival (CSS) of CRC patients with synchronous LM. The final prognostic nomogram based on prognostic factors was evaluated by concordance index (C-index), time-dependent receiver operating characteristic curves, and calibration curves. In the training and validation groups, the C-index for the nomogram was 0.648 and 0.638, and the AUC was 0.793 and 0.785, respectively. The high quality of the calibration curves in the nomogram models for CSS at 1-, 3-, and 5-year was observed. The nomogram model provided a conventional and useful tool to evaluate the 1-, 3-, and 5-year CSS of CRC patients with synchronous LM.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the second leading cause of cancer-related deaths worldwide1. In China, CRC is the third most common malignancy in both men and women2. Approximately 25% of CRC patients were reported to have metastases at the time of diagnosis3. Actually, metastasis was one of the leading causes of the poor prognosis of CRC patients, the survival was approximately 29 to 30 months with the current treatment modality4. Therefore, increasing recognization for CRC with metastasis was of crucial importance for improving patients’ survival. Regretfully, the large-scale prospective study about clinicopathological characteristics and prognostic factors for metastatic CRC were still deficient5.
Currently, the liver and lung are the most common sites of CRC metastases6,7. The lungs are second only to the liver as the site of metastasis, a recent study demonstrated that the rate of lung metastasis (LM) was present in approximately 29% of metastatic cases8. The incidence of LM in patients with CRC was relatively low but was frequently associated with a poor prognosis9. Due to the widespread use of chest CT scans in recent years, the rate of diagnosis of LM for patients with CRC increased when patients were diagnosed with CRC10. Therefore, it is necessary to evaluate the prognosis of CRC with synchronous LM. However, the prognosis of patients with CRC with synchronous LM has rarely been investigated. Furthermore, due to the relatively low incidence, no independent prognostic factors associated with survival in CRC patients with synchronous LM have been identified. Currently, the survival of patients with CRC is usually predicted using the TNM staging system11, which has limitations. A study12 has reported that there are differences involving the metastatic pattern between different metastasis lesions; therefore, the TNM staging system as a general evaluation tool cannot accurately predict the prognosis of CRC patients with synchronous LM, and a more individual prediction model for the survival of CRC with synchronous LM is urgently needed. The nomogram, a simple and useful tool that has been shown to provide more precise survival prediction compared to traditional TNM staging systems, and is built using independent prognostic factors13, has been widely used in medical research and clinical practice14,15,16.
In this study, our objective was to investigate predictive and prognostic factors of CRC with synchronous LM based on the Surveillance, Epidemiology, and End Results (SEER) database, which contains a large number of patients and their detailed clinical information, and then a nomogram was developed based on independent prognostic factors to predict 1-,3-,5-year cancer-specific survival (CSS) for CRC with synchronous LM. The nomogram was then used to stratify patients into high- and low-risk groups.
Materials and methods
Data sources
Patients with CRC diagnosed with synchronous LM were extracted from the SEER database between January 2010 and December 2015. The SEER is an openly accessed database, which collects cancer information on patients from 18 separate cancer registries across the United States and covers about one-quarter of the population of the whole country17. A patient consent form was not required for data from the SEER database as all data were de-identified prior to release and did not contain personally identifiable information from patients. This study was approved by the Ethics Committee of the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences.
Diagnostic and exclusion criteria
The main diagnostic criteria for this study were as follows: (a) patients with CRC; (b) stage IV patients with synchronous LM; and (c) patient’s death attributable to CRC. The exclusion criteria were patients with incomplete clinical data or pathological information. All enrolled patients were staged according to the 6th AJCC TNM staging system.
Patient population
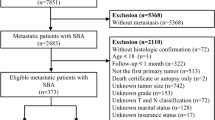
The patient data entered in the database were considered to be representative of the overall population. SEER*Stat version 8.3.9 was used to generate a case list. Data from SEER was used to identify patients with CRC diagnosed between 2010 and 2015, and 2875 stage IV CRC patients with synchronous lung metastasis were extracted according to related indications in SEER (“SEER Combined Mets at DX-lung (2010 +): YES”, “SEER other cause of death classification: Alive or dead due to cancer”, “ICD-O-3: 8140, 8210, 8220, 8261, 8263, 8480, 8481 and 8490”). Then, we excluded the unknown CEA level(n = 845), unknown primary tumor site(n = 115), unknown regional nodes examined(n = 17), unknown race(n = 234), unknown pathologic type(n = 8), unknown AJCC N stage(n = 206). Finally, a total of 1450 patients were enrolled in this study, which was divided into the training cohort and the validation cohort in a 7: 3 ratio by EXCEL using the Rand function. A general description of our study design is presented in Fig. 1. All CRC patients included in this study were definitively diagnosed by pathological examination and LM was diagnosed by imaging examination or pathological examination. Several clinical and tumor-related variables were collected to analyze prognosis, including age, AJCC N stage, CEA level, extra-LM (defined as involving bone, brain, and liver), primary tumor site, primary tumor size, and regional nodes examined, sex, year of diagnosis, race, pathological type, and primary tumor resection (primary CRC surgery combined with lung metastasectomy) in the SEER database.
The construction of the CSS nomogram
The CSS was the endpoint in the present study, it was calculated from diagnosis to death of the patient or the date still alive at the last censored follow-up. CSS was assessed using the Kaplan–Meier method, with the log-rank tests used in univariate analysis. The final independent prognostic factors were identified by multivariate analysis using the Cox regression model. The nomogram was developed based on these prognostic factors (P < 0.05) to predict the CSS of CRC patients with synchronous LM.
Evaluation of nomogram performance
The discrimination ability of the nomogram was evaluated using the concordance index (C-index) and AUC value18. AUC-index of 0.5 indicated a random chance and 1.0 indicated a perfect ability to correctly discriminate the outcome with the model. AUC values of 0.5–0.7, 0.7–0.85, and 0.85–0.95 were defined as low, middle, and high credibility, respectively18. The calibration ability of the nomogram was evaluated with calibration curves for 1-, 3-, and 5-year CSS comparing the predicted survival with the observed survival. The 1-, 3-, and 5-year ROC curves were used to evaluate the predictive accuracy of the nomogram for different periods. Internal validation of the nomogram was achieved with the bootstrap resampling strategy (1000 resamples). External validation was conducted in the validation cohort. Briefly, the validation cohort was individually given a risk score calculated with the nomogram equation.
Statistical analysis
The Rand function of EXCEL was used for the randomization of patients.The Chi-square test was used to compare the differences between the training and validation cohorts for the categorical variables. The R statistical packages “rms”, “survival”, “Hmisc”, “lattice”, “Formula”, “ggplot2”, “foreign”, “nomogramFormula”, “survivalROC”, “pROC” and “timeROC” were used to calculate the C-index, plot the calibration and ROC curves, build a nomogram, and draw the Kaplan–Meier curves. SPSS23.0 (SPSS Inc., Chicago, IL) and R (R version 4.1.1, http://www.r-project.org) were used for statistical analysis, and a P-value < 0.05 was considered statistically significant. This study has been reported in line with the TRIPOD statement19.
Ethics approval
The studies involving human participants were reviewed and approved by the Ethics Committee of the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences. The written consent form was not required for data from the SEER database as all data were de-identified prior to release and did not contain personally identifiable information from patients.
Methods statement
The authors confirm that all methods were carried out in accordance with relevant guidelines and regulations as publicly available data is used.
Results
Patient characteristics
From 2010 to 2015, 74,926 CRC patients were registered in the SEER database, a total of 1450 CRC patients with synchronous LM were included in our study, and patients were assigned in a nearly7:3 ratio to the training cohort and the validation cohort randomly. A total of 1021 patients with complete information were included in the final analysis for the training cohort. For the validation cohort, a total of 429 patients were included in the final analysis after the application of the same inclusion and exclusion criteria. The clinicopathological characteristics and demographics of the entire cohort (n = 1450), including the training (n = 1021), and validation (n = 429) subsets are described in (Table 1). In the training and the validation cohort, the majority of patients were ≥ 60 years old at diagnosis (62.1 and 64.3%, respectively). Most patients had an adenocarcinoma histological type (86.2 and 86.9%, respectively), and most patients’ tumors were located in the descending colon (45.9 and 45.7%, respectively). Extra-LM were identified in 73.8% and 76.2% of the patients in the training and validation cohorts, respectively, and the CEA levels were positive in 84.6% and 88.1% of the patients. Whites accounted for 81.9% and 80.4% of all cases, respectively. Most people were AJCC N0 (39.3 and 41.7%, respectively) and N1 (40.5 and 40.1%, respectively). Across the study population of the two cohorts, only 0.8% and 0.7% of the patients underwent primary surgery, and 62.6% and 65.7% of the patients had no regional nodes examined. The primary tumor size of most patients was < 3 cm (59.6% and 62.0%, respectively). The range of CSS ranged from 0–106 months and 0–107 months in both cohorts, respectively. The mean CSS was 20.35 and 19.84 months. with a median CSS of 14 months and 15 months, respectively. Most of the variables including median survival month (P = 0.739), number of events (P = 0.102), age (P = 0.421), year of diagnosis (P = 0.182), race (P = 0.514), primary tumor site (P = 0.938), pathological type (P = 0.742), primary tumor resection (P = 1.000), Extra-lung metastasis (P = 0.343), CEA(P = 0.084), regional nodes examined (P = 0.723), AJCC N stage (P = 0.582), primary tumor size (P = 0.683) showed no significant differences between the training and the validation cohort, which indicated that patients in the training and validation cohorts had a balanced survival distribution and baseline clinical characteristics.
Survival analysis and independent prognostic factors in CRC patients with synchronous LM
The survival curves for different variables were generated using the Kaplan–Meier method and were compared using the log-rank test. Seven variables, including age, AJCC N stage, CEA level, extra-lung metastasis, primary tumor site, primary tumor size, and regional nodes examined, were associated with CSS (P < 0.05) (Table 2). The Kaplan–Meier curves for these factors are shown in Fig. 2. Next, we performed multivariate Cox regression analysis among the seven variables above, and found age (hazard ratio [HR ] = 1.39; 95% confidence interval [CI] = 1.211–1.595; P < 0.001); CEA level (HR = 1.426; 95% CI = 1.170–1.738; P < 0.001); extra-LM (HR = 1.752; 95% CI = 1.478–2.076; P < 0.001); primary tumor site (transverse colon: reference; ascending colon :HR = 0.899; 95% CI = 0.656–1.233; descending colon :HR = 0.824; 95% CI = 0.614–1.106; rectum: HR = 0.681; 95% CI = 0.500–0.928, P = 0.014), primary tumor size (< 33 cm: reference; ≤ 3 to < 5 cm: HR = 0.955; 95% CI = 0.660–1.382; ≥ 5 cm: HR = 0.613; 95% CI = 0.424–0.888, P = 0.002), and examined reginal nodes examined (< 12: reference; 1–12: HR = 0.739; 95% CI = 0.497–1.098; 13–25: HR = 0.582; 95% CI = 0.398–0.851; 26–76: HR = 0.502; 95% CI = 0.319–0.790, P = 0.010) were significantly corelated with CSS and were also defined as independent prognostic factors of CRC patients with synchronous LM (Table 3).
Kaplan–Meier CSS curves stratifying patients by different prognostic variables with P < 0.05. (A) Kaplan–Meier CSS curve according to age, (B) AJCC N stage. and (C) CEA level. (D) Kaplan–Meier CSS curve according to extra-lung metastasis and (E) primary tumor site. (F) Kaplan–Meier CSS curve according to primary tumor size and (G) the regional nodes examined.
Development and assessment of predictive nomogram
We developed a predictive nomogram containing variables including age,primary site, extra-lung metastasis, CEA, primary tumor size and regional nodes examined, which were demonstrated to be statistically significant in multivariate analysis (Fig. 3). To confirm that the nomogram prediction model had higher efficacy in predicting the prognosis of patients with CRC with synchronous LM, time-dependent ROC analyzes were performed at 1, 3, and 5 years. The AUC of CSS at 1, 3, and 5 years was 0.68 (95% CI = 0.65–0.71), 0.79 (95% CI = 0.75–0.83), and 0.80 (95% CI = 0.75–0.86), respectively in the training cohort (Fig. 4A); whereas 0.68 (95% CI = 0.63–0.73), and 0.74 (95% CI = 0.68–0.80) and 0.78 (95% CI = 0.66–0.90) in the validation cohort (Fig. 4B). The results demonstrated that the 1-, 3-, and 5-year CSS predictions were good.
Nomogram for predicting the 1-, 3-, and 5-year CSS. The total score was obtained according to the value of each indicator (age, primary site, extra-lung metastasis, CEA, primary tumor size and regional nodes examined), and the 1-, 3-, and 5-year CSS corresponding to the total score was the predicted rate by nomogram.
ROC curves based on nomogram and Kaplan–Meier curve of CSS in the training cohort and validation cohort. (A) ROC curve and AUC of the nomogram to predict 1-, 3- and 5-year CSS in the training cohort and (B) in the validation cohort. (C) ROC curve and AUC of nomogram in the training cohort and (D) in the validation cohort. (E) Kaplan–Meier curve of CSS in the training cohort and (F) in the validation cohort. Low- and high-risk groups were divided based on the median total points.
Internal and external validation of the nomogram
The C-index and ROC curves were used to evaluate the discrimination power of the nomogram. For internal validation, the bootstrap-corrected C-index for the nomogram was 0.648. For the predictive survival ability of the nomogram in the external validation cohort, the score for the individual case in the validation cohort was calculated according to the established nomogram and then used in the Cox regression model. C-index for the validation cohort was 0.638. To further clarify the discrimination power of the nomogram. The model had an AUC of 0.793 (95% CI, 0.747–0.839), which showed good discrimination (Fig. 4C). The AUC of the validation cohort was 0.785 (95% CI, 0.708–0.862) which demonstrated the nomogram was well fitted (Fig. 4D).
Risk stratification based on nomogram scores
To further explore the predictive capacity of the nomogram, the total point of each patient was determined based on the nomogram in both the training and validation cohorts. The median point was 33.56 and 28.52 in the training and validation cohort, respectively. Then, we divided the patients into low- and high-risk groups according to the median points and performed a survival analysis using the Kaplan–Meier method. The mean CSS of the training cohort were 13.97 (95% CI = 12.59–15.36) months and 33.07(95% CI = 30.06–36.08) months in the high- and low-risk groups (P < 0.001) (Fig. 4E), and in the validation cohort, the mean CSS of the high- and low-risk groups were 14.36 (95% CI = 12.27–16.45) months and 29.32 (95% CI = 25.36–33.28) months respectively (P < 0.001) (Fig. 4F). The above results illustrated that patients in the high-risk group tended to have poorer outcomes than those in the low-risk group, and the nomogram had good distinguishing ability and generalizability.
Calibration curve analysis of the nomogram
The bootstrapping method (1000 repetitions) was used and a calibration curve was illustrated in Fig. 5. There were no obvious deviations between the model predicted risk and the actually observed risk curves (Fig. 5A–C), meaning good agreement between observed and predicted 1-, 3-, and 5-year CSS predicted by the nomogram in the training cohort. We further validated the model in the validation cohort using the same method (Fig. 5D–F) and good calibration was observed.
Discussion
This study focused on the prediction of the 1-, 3-, and 5-year CSS of CRC patients with synchronous LM. From the perspective of predicting indicators, age, CEA levels, extra-LM, primary tumor site, primary tumor size, and regional nodes examined were defined as independent prognostic factors of stage IV CRC patients with synchronous LM. A nomogram based on the aforementioned variables was constructed to forecast the 1-, 3-, and 5-year CSS, and the discrimination ability was estimated by calibration and discrimination in both training and validation cohorts. The calibration curve of 1-, 3-, and 5-year CSS in the training cohort showed favorable agreement between the predicted and actual observed probabilities, similarly, the validation cohort also showed optimal calibration in the 1-, 3-, and 5-year CSS, which supported the repeatability as well as reliability of the constructed model. Then, we stratified CRC patients with LM into high-risk and low-risk groups according to median individual points. This stratification indicated that patients in the high-risk group had poorer CSS, therefore, more intensive follow-up and more comprehensive treatment should be considered. Both the C-index and AUC values revealed the good discriminatory capacity of the nomogram: the C-index of the training and validation groups were 0.648 and 0.638, respectively, and the AUC values were 0.793 and 0.785, respectively. Furthermore, the clinical parameters to be input into the nomogram are easy to obtain from the patient’s clinical records, making it a simple tool to use. Overall, our nomogram had a good ability to predict CSS and could be applied as a convenient tool to predict 1-, 3-, and 5-year CSS of CRC with synchronous LM.
The present study revealed that the prognosis of CRC patients with synchronous LM was better among individuals < 60 years of age, which was consistent with previous studies20,21 reporting that age was an independent prognostic factor for CRC patients with synchronous LM and suggested that in an increasingly aging population, the functional status of patients should be taken into account. Furthermore, many studies have reported that the primary tumor site could be a prognostic factor for metastasis CRC22,23,24. A proposed explanation is that the colon and rectum present differences in the microbiome composition, chromosomal, and molecular characteristics25. Therefore, colorectal tumors with different sites have different capacities for metastasis. This study shows that the primary tumor site could be prognostic in CRC with LM. We showed that different CSS could be predicted for patients with tumors at the right colon, transverse colon, descending colon, and rectum. The primary tumor in the transverse colon for CRC with LM had worse CSS. A high level of CEA was associated with CRC. Preoperative CEA levels were important in determining diagnosis and prognosis and were widely used in clinical practice20,26,27, and during the post-resection follow-up period, the CEA level was an important indicator to detect local recurrence and distant metastases after surgery in CRC patients. However, it remains unknown whether CEA was an independent factor in CRC survival with LM. A study evaluating synchronous CRC reported26 that patients with multiple colorectal tumors were more likely to express high levels of CEA, Unfortunately, it did not explore the relationship between CEA and the prognosis of synchronous colorectal carcinoma. Although, our study demonstrated that elevation of the CEA level could predict the prognosis of patients with CRC with synchronous LM.In this study, tumor size < 3 cm was shown to be associated with poor CSS. This result was inconsistent with previous research28,29, which showed that tumor size ≥ 5 cm was an independent risk factor for a worse prognosis. However, in the clinic, there may be cases of locally advanced CRC with small primary tumors and small colorectal tumors do not always correlate with early-stage disease. Furthermore, CRC patients with synchronous LM were not the main target investigated in previous studies. Our research indicated that for CRC patients with synchronous LM, smaller tumors tended to have stronger invasiveness and metastatic capacity. Patients with a tumor size < 3 cm may have a poorer prognosis, but further studies are needed. In our study, extra-LM lesions were also identified as a prognostic factor. The presence of extra-LM is associated with a more aggressive primary tumor, on the other hand, extra-LM could influence a patient’s organ function, aggravating symptoms, therefore, the extra-LM may represent a negative factor in the CSS of the patients. Cancer cells in regional lymph nodes30 are often associated with reduced survival. Radical surgery including lymphadenectomy of CRC is a decisive factor for prognosis and is necessary for the therapeutic staging of the patient, the minimum number of 12 examined lymph nodes has been accepted in clinics since 199031. We found that the identification of fewer than 12 regional nodes was associated with a worse CSS, which was consistent with many studies20,32. In particular, the role of primary tumor resection in CRC patients with distant metastases remains controversial. A previous study33 reported better outcomes in patients with CRC LM undergoing lung metastasectomy, and also achieved remarkable improvement in prognosis. But several studies34,35 have also suggested that surgical resection should not be performed if all known tumors could not be completely removed (R0 resection), because it could not provide survival benefits for CRC patients with metastatic diseases. A recent study36 also found that prognosis was similar for those who underwent lung metastasectomy and those who did not. Our study showed that primary surgery cannot comprehensively improve CSS for patients with CRC with synchronous LM. The explanation may be due to the advancement of palliative treatment including chemotherapy and molecular targeting treatment (i.e. FOLFOX or FOLFIRI combined with molecularly targeted drugs), which has improved the prognosis of CRC patients with LM and will continue to improve. However, this needs to be further studied as only 0.8% of the patients in the study had completed primary surgery, which means that a selection bias cannot be avoided, furthermore, detailed treatment information including chemotherapy was not recorded in the SEER database; thus, further studies should include more cases with lung metastasectomy and treatment information.
This large-scale study revealed the clinical characteristics, risk, and prognostic factors for CRC patients with synchronous LM. However, this study still has some limitations. First, this was a retrospective study that included patients from the United States. A future external validation involving patients from other countries is needed to evaluate the generalizability of this nomogram. Moreover, as lung metastasis was the aim of this study, extra-lung metastasis including bone, brain, and liver metastases was not discussed individually while they could influence the evaluation for the CSS. Therefore, Cox regression model might not be the best method to analysis the CSS and a more suitable competing risk model would be applied in the next study, however, the result of this study was still helpful in our future study to further research the CSS influence of other coexisted metastasis for CRC patients with lung metastasis. Also, the 1-year AUC value of the nomogram based on both the training and validation group was 0.68, which suggests the reliability of the 1-year CSS prediction needs to be enhanced. In addition, some patients who received surgery solely targeting their colorectal tumors were not further extracted from this study. Further studies were needed to clarify the necessity of palliative surgery without lung metastasectomy. Finally, this study did not investigate specific treatment options, because detailed treatment information, including radiation therapy, was not recorded in the SEER cohort. In summary, this nomogram was based on the SEER database and made full use of its indicators. The incorporation of other factors, such as additional biomarkers, will improve this model. Despite these limitations, this nomogram remains a good risk model and could be applied to predict the prognosis of stage IV CRC patients with synchronous LM.
In summary, currently, patients with stage I to III tumors who undergo primary surgery are predicted to have a good prognosis; whereas, the prognosis for stage IV CRC patients with LM remains poor. Although these patients only account for a small proportion of CRC patients, greater attention should be placed on their prognosis. In this study, we constructed and validated a predictive nomogram for the CSS of CRC patients with synchronous LM, which could be used to accurately evaluate the 1-, 3-, and 5-year CSS of stage IV CRC patients with synchronous LM and help distinguish high-risk patients who may require more aggressive treatment and follow-up strategies.
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: https://seer.cancer.gov/.
Abbreviations
- CRC:
-
Colorectal cancer
- LM:
-
Lung metastases
- CSS:
-
Cancer-specific survival
- SEER:
-
Surveillance, epidemiology, and end results database
- C-index:
-
Concordance index
- ROC:
-
Receiver operating characteristic curves
- CEA:
-
Carcinoembryonic antigen
- AJCC:
-
American Joint Commission on Cancer
- TNM:
-
Tumor-node-metastasis
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68(6), 394–424. https://doi.org/10.3322/caac.21492 (2018).
Feng, R. M., Zong, Y. N., Cao, S. M. & Xu, R. H. Current cancer situation in China: Good or bad news from the 2018 global cancer statistics?. Cancer Commun. (Lond) 39(1), 22. https://doi.org/10.1186/s40880-019-0368-6 (2019).
Riihimäki, M., Hemminki, A., Sundquist, J. & Hemminki, K. Patterns of metastasis in colon and rectal cancer. Sci. Rep. 6, 29765. https://doi.org/10.1038/srep29765 (2016).
Margalit, O. et al. Lung metastasis predicts better prognosis in metastatic colorectal cancer with mutated KRAS. Clin. Colorectal Cancer 18(3), e300–e307. https://doi.org/10.1016/j.clcc.2019.06.001 (2019).
Venook, A. P. et al. Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients With KRAS wild-type advanced or metastatic colorectal cancer: A randomized clinical trial. JAMA 317(23), 2392–2401. https://doi.org/10.1001/jama.2017.7105 (2017).
Wang, C. C. & Li, J. An update on chemotherapy of colorectal liver metastases. World J. Gastroenterol. 18(1), 25–33. https://doi.org/10.3748/wjg.v18.i1.25 (2012).
Zampino, M. G. et al. Lung metastases from colorectal cancer: Analysis of prognostic factors in a single institution study. Ann. Thorac. Surg. 98(4), 1238–1245. https://doi.org/10.1016/j.athoracsur.2014.05.048 (2014).
Zhang, G. Q. et al. Aggressive multimodal treatment and metastatic colorectal cancer survival. J. Am. Coll. Surg. 230(4), 689–698. https://doi.org/10.1016/j.jamcollsurg.2019.12.024 (2020).
Zellweger, M. et al. Surgical treatment of pulmonary metastasis in colorectal cancer patients: Current practice and results. Crit. Rev. Oncol. Hematol. 127, 105–116. https://doi.org/10.1016/j.critrevonc.2018.05.001 (2018).
Hu, T. et al. CT morphological features integrated with whole-lesion histogram parameters to predict lung metastasis for colorectal cancer patients with pulmonary nodules. Front. Oncol. 9, 1241. https://doi.org/10.3389/fonc.2019.01241 (2019).
Obrocea, F. L., Sajin, M., Marinescu, E. C. & Stoica, D. Colorectal cancer and the 7th revision of the TNM staging system: Review of changes and suggestions for uniform pathologic reporting. Rom. J. Morphol. Embryol. 52(2), 537–544 (2011) (PMID: 21655640).
Robinson, J. R., Newcomb, P. A., Hardikar, S., Cohen, S. A. & Phipps, A. I. Stage IV colorectal cancer primary site and patterns of distant metastasis. Cancer Epidemiol. 48, 92–95. https://doi.org/10.1016/j.canep.2017.04.003 (2017).
Wang, Y., Du, L., Yang, X., Li, J., Li, P., Zhao, Y., Duan, W., Chen, Y., Wang, Y., Mao, H. et al. A nomogram combining long non-coding RNA expression profiles and clinical factors predicts survival in patients with bladder cancer. Aging (Albany NY) 2020, 12(3):2857–2879.https://doi.org/10.18632/aging.102782.
Wang, S. et al. Development and validation of a nomogram prognostic model for SCLC patients. J. Thorac. Oncol. 13(9), 1338–1348. https://doi.org/10.1016/j.jtho.2018.05.037 (2018).
Yu, C. & Zhang, Y. Development and validation of prognostic nomogram for young patients with gastric cancer. Ann. Transl. Med. 7(22), 641. https://doi.org/10.21037/atm.2019.10.77 (2019).
Jiang, S. et al. Prognosis and nomogram for predicting postoperative survival of duodenal adenocarcinoma: A retrospective study in China and the SEER database. Sci. Rep. 8(1), 7940. https://doi.org/10.1038/s41598-018-26145-6 (2018).
Surveillance, Epidemiology, and End Results (SEER) Program: SEER 9, 13, and18GeographicAreas. https://seer.cancer.gov/archive/csr/1975_2011/browse_csr.php?sectionSEL=1&pageSEL=sect_01_zfig.01.html. Accessed July 21, 2019.
Alba, A. C. et al. Discrimination and calibration of clinical prediction models: Users’ guides to the medical literature. JAMA 318(14), 1377–1384. https://doi.org/10.1001/jama.2017.12126 (2017).
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. Br. J. Surg. 102(3), 148–158. https://doi.org/10.1002/bjs.9736 (2015).
Mo, S. et al. Establishment and validation of a novel nomogram incorporating clinicopathological parameters into the TNM staging system to predict prognosis for stage II colorectal cancer. Cancer Cell Int. 20, 285. https://doi.org/10.1186/s12935-020-01382-w (2020).
Abasse Kassim, S. et al. Clinicopathologic and epidemiological characteristics of prognostic factors in post-surgical survival of colorectal cancer patients in Jiangsu Province, China. Cancer Epidemiol. 62, 101565. https://doi.org/10.1016/j.canep.2019.07.004 (2019).
Loupakis, F. et al. Primary tumor location as a prognostic factor in metastatic colorectal cancer. J. Natl. Cancer Inst. https://doi.org/10.1093/jnci/dju427 (2015).
Nitsche, U. et al. Right sided colon cancer as a distinct histopathological subtype with reduced prognosis. Dig. Surg. 33(2), 157–163. https://doi.org/10.1159/000443644 (2016).
Wong, H. L. et al. Impact of primary tumor site on bevacizumab efficacy in metastatic colorectal cancer. Clin. Colorectal Cancer 15(2), e9–e15. https://doi.org/10.1016/j.clcc.2016.02.007 (2016).
Stintzing, S., Tejpar, S., Gibbs, P., Thiebach, L. & Lenz, H. J. Understanding the role of primary tumour localisation in colorectal cancer treatment and outcomes. Eur. J. Cancer 84, 69–80. https://doi.org/10.1016/j.ejca.2017.07.016 (2017).
Chin, C. C., Kuo, Y. H. & Chiang, J. M. Synchronous colorectal carcinoma: predisposing factors and characteristics. Colorectal Dis. 21(4), 432–440. https://doi.org/10.1111/codi.14539 (2019).
Shibutani, M. et al. Significance of CEA and CA19-9 combination as a prognostic indicator and for recurrence monitoring in patients with stage II colorectal cancer. Anticancer Res 34(7), 3753–3758 (2014) (PMID:24982398).
Yan, Q. et al. Value of tumor size as a prognostic factor in metastatic colorectal cancer patients after chemotherapy: A population-based study. Future Oncol. 15, 1745–1758. https://doi.org/10.2217/fon-2018-0785 (2019).
Wu, J. et al. Prognostic nomogram to predict the overall survival of patients with early-onset colorectal cancer: a population-based analysis. Int. J. Colorectal Dis. 36, 1981–1993. https://doi.org/10.1007/s00384-021-03992-w (2021).
Naxerova, K. et al. Origins of lymphatic and distant metastases in human colorectal cancer. Science 357, 55–60. https://doi.org/10.1126/science.aai8515 (2017).
Li Destri, G., Di Carlo, I., Scilletta, R., Scilletta, B. & Puleo, S. Colorectal cancer and lymph nodes: The obsession with the number 12. World J. Gastroenterol. 20, 1951–1960. https://doi.org/10.3748/wjg.v20.i8.1951 (2014).
Li, Y. et al. Predictive and prognostic factors of synchronous colorectal lung-limited metastasis. Gastroenterol. Res. Pract. 2020, 6131485. https://doi.org/10.1155/2020/6131485 (2020).
Hirosawa, T. et al. Prognostic factors in patients undergoing complete resection of pulmonary metastases of colorectal cancer: A multi-institutional cumulative follow-up study. Surg. Today 43, 494–499. https://doi.org/10.1007/s00595-012-0373-8 (2013).
Yoo, P. S., Lopez-Soler, R. I., Longo, W. E. & Cha, C. H. Liver resection for metastatic colorectal cancer in the age of neoadjuvant chemotherapy and bevacizumab. Clin. Colorectal. Cancer 6, 202–207. https://doi.org/10.3816/ccc.2006.n.036 (2006).
Altendorf-Hofmann, A. & Scheele, J. A critical review of the major indicators of prognosis after resection of hepatic metastases from colorectal carcinoma. Surg. Oncol. Clin. N Am. 12(165–92), xi. https://doi.org/10.1016/s1055-3207(02)00091-1 (2003).
Milosevic, M. et al. Pulmonary metastasectomy in colorectal cancer: Updated analysis of 93 randomized patients-control survival is much better than previously assumed. Colorectal Dis 22, 1314–1324. https://doi.org/10.1111/codi.15113 (2020).
Acknowledgements
The first author, Pu Cheng, gratefully acknowledges support from Liying Ren in learning R software.
Funding
This work was supported by National Key R&D Program of China (2017YFC0908203), CAMS Initiative for Innovative Medicine (2017-I2M-2–003), Science and Technology Project of Chaoyang District, Beijing (CYSF-1931), and Beijing Gold-Bridge Funds (ZZ19055).
Author information
Authors and Affiliations
Contributions
P.C.: performing formal analysis and writing-original draft. H.P.: giving significant revision advice and assisting analysis. F.H., J.Y. and H.C.: investigation and project administration. Z.X. and Z.L.: supervised the study and assisted in revision. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheng, P., Chen, H., Huang, F. et al. Nomograms predicting cancer-specific survival for stage IV colorectal cancer with synchronous lung metastases. Sci Rep 12, 13952 (2022). https://doi.org/10.1038/s41598-022-18258-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18258-w
This article is cited by
-
Construction and validation of a nomogram of risk factors and cancer-specific survival prognosis for combined lymphatic metastases in patients with early-onset colorectal cancer
International Journal of Colorectal Disease (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.