Abstract
This study aimed to cross-calibrate body composition measures from the GE Lunar Prodigy and GE Lunar iDXA in a cohort of young children. 28 children (mean age 3.4 years) were measured on the iDXA followed by the Prodigy. Prodigy scans were subsequently reanalysed using enCORE v17 enhanced analysis (“Prodigy enhanced”). Body composition parameters were compared across three evaluation methods (Prodigy, Prodigy enhanced, iDXA), and adjustment equations were developed. There were differences in the three evaluation methods for all body composition parameters. Body fat percentage (%BF) from the iDXA was approximately 1.5-fold greater than the Prodigy, whereas bone mineral density (BMD) was approximately 20% lower. Reanalysis of Prodigy scans with enhanced software attenuated these differences (%BF: − 5.2% [95% CI − 3.5, − 6.8]; and BMD: 1.0% [95% CI 0.0, 1.9]), although significant differences remained for all parameters except total body less head (TBLH) total mass and TBLH BMD, and some regional estimates. There were large differences between the Prodigy and iDXA, with these differences related both to scan resolution and software. Reanalysis of Prodigy scans with enhanced analysis resulted in body composition values much closer to those obtained on the iDXA, although differences remained. As manufacturers update models and software, researchers and clinicians need to be aware of the impact this may have on the longitudinal assessment of body composition, as results may not be comparable across devices and software versions.
Similar content being viewed by others
Introduction
Dual-energy X-ray absorptiometry (DXA) is a tool that allows the estimation of body composition by measuring the attenuation of X-rays1. As each tissue type has a characteristic R value, which is the ratio of X-ray attenuation at high and low energy, lean mass (LM), fat mass (FM), and bone mineral content (BMC) can be estimated1,2. Bone mineral density (BMD) is subsequently calculated as the BMC for a projected area (i.e., bone area)3. In addition to enabling differentiation between fat and fat-free masses, DXA allows regional estimation of body composition. A limitation is that differences exist between device types and software versions, which may be amplified in young children4,5,6,7. For example, Barbour et al.4 demonstrated that among infants measured using a Hologic device, reanalysis using the updated software increased body fat percentage (%BF) by approximately 50%. These differences are of particular importance in longitudinal studies where DXA devices or software may be upgraded over the course of the study or in multi-centre studies where different DXA devices may be available at each site.
GE Lunar is one of two manufacturers of DXA devices, with the iDXA being their most advanced model (introduced in 2005). The iDXA has improved image resolution due to an X-ray source with a higher voltage (100 kV), greater pixel density, and a greater number of detectors8. The enhanced algorithms from the iDXA have been modified to enable old scans from the GE Lunar Prodigy to be reanalysed with GE Lunar’s “enhanced” analysis option, introduced with the version 14 release of their enCORE analysis software in 2012. While differences between the iDXA and Prodigy have previously been reported in adults9,10,11,12,13, this has not been evaluated in young children. Furthermore, it is unclear how much of the difference observed between old and new scans is related to the software versus differences in scan resolution between the models. Therefore, among a cohort of young children, we aimed first to determine if body composition values are the same when obtained with a GE Lunar Prodigy and with a GE Lunar iDXA; and second, to determine if body composition values from a Prodigy, reanalysed with the enhanced analysis software, are comparable to those obtained using an iDXA.
Subjects and methods
A sample of children aged 3.4 years (n = 29) was selected from the Auckland site of the Nutritional Intervention Preconception and During Pregnancy to Maintain Healthy Glucose Metabolism and Offspring Health (NiPPeR) study14. Children were selected based on good compliance with the DXA protocol (i.e., producing a DXA scan without movement artefact). The NiPPeR trial was registered on 16 July 2015 with ClinicalTrials.gov (NCT02509988, Universal Trial Number U1111-1171-8056); ethics approval was granted by the Northern A Health and Disability Ethics Committee (15/NTA/21/AM20). Written informed consent was obtained from the parents/guardians of the study subjects. All procedures in this study were conducted according to the ethical principles and guidelines laid down in the Declaration of Helsinki.
Children were scanned on a GE Lunar iDXA (enCORE v17, paediatric mode) immediately followed by a scan on a GE Lunar Prodigy (enCORE v17, paediatric mode). It has previously been reported that the effective radiation dose of the iDXA scanner for an infant phantom was 8.9 μSv15, and in adults, 4.7 μSv16. In comparison, the global average for daily natural background radiation exposure is 6.6 μSv17. Therefore, the risk associated with repeat DXA scanning is low.
Before measurement with the DXA machines, standing height was measured three times to the nearest 0.1 cm using a calibrated SECA 213 portable stadiometer (SECA, Hamburg, Germany), and weight was measured once to the nearest 100 g using calibrated SECA 899 scales. Median height, weight, and date of birth were input into the DXA machines prior to measurement.
Both DXA machines were calibrated daily with a manufacturer-specific calibration block phantom and with a spine phantom at regular intervals. Children were measured while lightly clothed, in clothing without metal, lying supine on the measurement bed within the scan limit borders. Feet were rotated inwards slightly, and a Velcro strap was used to hold feet in place. If necessary, the child was swaddled lightly with a thin blanket, ensuring arms and legs remained separated. Each scan was graded according to the degree of movement, with significant movement artefact being excluded from the main analyses (n = 1). Images with minor movement were flagged and sensitivity analyses were run excluding these participants (n = 11). The results of the sensitivity analyses were little changed, so results are reported for the main analyses only.
Three sets of body composition values were obtained: iDXA scan analysed with enCORE v17 and Prodigy scan analysed with enCORE v17 basic and with enCORE v17 enhanced analysis. Total body less head (TBLH)18 and regional estimates of body composition are reported for FM, LM, BMC, and bone area, as well as %BF (FM ÷ total mass × 100) and BMD (BMC ÷ bone area).
Statistical analyses
Subject characteristics and body composition values are reported as means ± SD for continuous variables and n (%) for categorical variables. Differences in body composition values between the three evaluation methods (iDXA, Prodigy basic, and Prodigy enhanced) were assessed using within-subjects ANOVA with Bonferroni post-hoc testing. Differences between the Prodigy and iDXA scans are reported as percentage differences and 95% confidence intervals.
To assess differences between the devices and software versions across a range of body sizes, Bland–Altman analyses were conducted to compare the Prodigy (basic and enhanced) to the iDXA (reference), with results reported as biases (i.e., mean differences) and 95% limits of agreement (LOA). Finally, equations were developed using linear regression to allow measurements made on the Prodigy to be adjusted to be comparable to those made on the iDXA. Prediction equations were developed using leave-one-out cross-validation for FM, LM, BMC, and bone area. Adjusted body composition values were then compared to the reference (iDXA) using paired-samples t-tests and Bland–Altman analyses. All tests were two-tailed and were performed within R (R Foundation for Statistical Computing, Vienna, Austria), with p values less than 0.05 being considered statistically significant.
Results
Population characteristics
29 children were measured on the two DXA devices. Following exclusion of scans with movement artefact (n = 1), the sample comprised of 28 children, described in Table 1. The excluded child was similar in height, weight, BMI, and age (all p > 0.05).
Comparison of the prodigy and iDXA
The mean body composition values for each measurement condition are summarised in Table 2 and Supplementary Table S1. Within-subjects ANOVA indicated differences between the three scan conditions (p < 0.001 for all body composition values). Post-hoc testing revealed differences between the iDXA and Prodigy basic for all body composition parameters. Following reanalysis of Prodigy scans using enhanced analysis, there remained differences between the iDXA and the Prodigy, except for TBLH BMD (− 0.004 g/cm2 [95% CI − 0.009, 0.001], p = 0.131), and some regional estimates (Supplementary Table S1).
When expressed as percentage differences, Prodigy basic TBLH values were up to 37% different from those obtained on the iDXA (Table 2). Differences were largest for fat mass (kg and %) and bone parameters (BMC, bone area, and BMD), as well as for regional estimates, which were up to 65% different (Table 2 and Supplementary Table S1). When Prodigy scans were reanalysed using enhanced analysis, the percentage differences reduced to < 6.5% for TBLH values and < 15.5% for regional estimates (Table 2 and Supplementary Table S1).
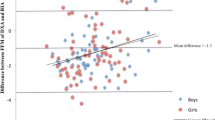
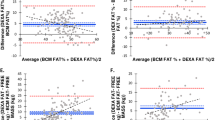
The Bland–Altman analyses are reported in Tables 3 and Table S1 and Supplementary Fig. S1. Compared to the iDXA, Prodigy basic LM was higher by ~ 800 g and FM lower by ~ 1.3 kg, resulting in a difference in total mass of − 550 g and a difference in %BF of − 9.7%. Both bone area and BMC were reduced (− 255 g [95% LOA − 329, − 181] and − 59 [95% LOA − 86, − 32], respectively), although bone area to a greater extent, resulting in greater estimates of BMD (+ 0.11 g/cm2 [95% LOA 0.09, 0.13]). A systematic bias for %BF was observed, with differences being greater among those with low %BF. When the Prodigy scans were reanalysed using enhanced analysis, the bias for TBLH LM reduced to less than 250 g, while the bias for FM reduced to almost a tenth of the original value (+ 167 g [95% LOA − 133, 466]). Meanwhile, the bias for BMD was reduced to 0 g/cm2. Regional analyses paralleled the TBLH results, with the Prodigy basic having higher LM but lower FM and bone area. Reanalysis of Prodigy files with enhanced analysis attenuated these differences.
Adjustment equations
Prediction equations were developed to enable adjustment of Prodigy (basic) measurements (Table 4 and Fig. 1). Prediction equations for enhanced measurements are contained within the supplementary file (Supplementary Table 2 and Supplementary Fig. S2).
When the equations were validated, the adjusted values aligned more closely with iDXA estimates than the reanalysed Prodigy scans (i.e., enhanced Prodigy) did. For example, in comparison to iDXA estimates, Prodigy enhanced LM was 2.7% lower, with a bias of ~ 250 g, whereas adjusted Prodigy LM was almost identical (0.0% [95% CI − 1.8, 1.7]), with a bias of less than 10 g (Table 5).
Discussion
Previous studies have identified differences between DXA models and software versions; however, few have evaluated differences in young children. The International Society for Clinical Densitometry (ISCD) recommend in vitro cross-calibration when comparing devices of the same model but in vivo cross-calibration when comparing devices from different manufacturers19. A study comparing two models by the same manufacturer found that spine phantom cross-calibration can be inaccurate compared to in vivo calibration20. This is further complicated in body composition studies, as there is a lack of a suitable phantom for cross-calibration of fat and lean masses. Therefore, in our study, we cross-calibrated two GE Lunar DXA systems (Prodigy and iDXA) in vivo among 28 young children and found significant differences between the two devices, even after Prodigy scans were reanalysed with enhanced analysis.
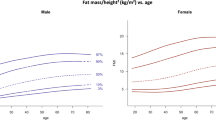
To our knowledge, no previous study has cross-calibrated the Prodigy and iDXA in a cohort of young children (< 5 years). DXA cross-calibration studies in young children are limited; however, a previous study (3–19 years, n = 126) found that FM from the iDXA (v16) was approximately 15% higher in girls and 31% higher in boys in comparison to the GE Lunar DPX-Pro (v9.3). LM was also reduced when measured with the iDXA compared to the DPX-Pro; however, this was only significant in boys21. Other studies have compared single Hologic scans reanalysed with updated software and found differences in FM, FFM, and %BF, but no differences in total mass4,6. In young children, there are clear differences between device types and software versions; however, the contribution of scan versus software has not previously been evaluated.
We observed differences between the two devices in all parameters, with iDXA %BF being approximately 1.5-fold greater than Prodigy measurements, whereas BMD was ~ 20% lower (Table 2). When we reanalysed the Prodigy scans with enhanced analysis, although differences remained in all estimates except for TBLH BMD, as well as some regional estimates, the percentage differences and biases were substantially reduced (Table 2 and Table S1).
In our study, differences between devices were most substantial among children with low %BF. Shypailo et al.6 reanalysed a large number of paediatric scans (n = 1384) obtained with a Hologic QDR-4500 (v11.2) with updated software (v12.1) and observed greater differences in FM and %BF among younger, smaller subjects, and in girls; although, these results may not be relevant to GE Lunar devices given the differences in technology used in the two scanner types22. A pilot study in 13 women (20–46 years) found that differences between the iDXA and Prodigy were most substantial among women who were least adipose (< 20 kg FM and < 30% BF)16. DXA estimates body composition according to the attenuation of X-ray beams at high and low energy. A limitation of the technology is that DXA can only differentiate between two tissue types simultaneously (i.e., bone vs non-bone, fat vs lean)1. In an adult DXA scan, 40 to 45% of pixels will contain bone, fat, and lean tissue, whereas, in children, this percentage is increased4. Therefore, improvements to the estimation of body composition in bone-containing tissue will have a greater impact in younger, smaller children. This may also explain why in some cross-validation studies, only regional estimates were affected9,10.
Although comparison has not been made between the iDXA and the Prodigy in a cohort of young children, previous studies in adults have found only small differences between the Prodigy and the iDXA, which have not been consistent across body composition parameters and regions, nor in the direction of the difference9,10,11,12,13. The variations in software used may partially explain these conflicting results. The studies used Prodigy scanners with enCORE software versions ranging from 6.10 to 16, while the iDXA scanners used enCORE software version 12.3–179,10,11,12,13.
Watson et al.13,23 evaluated differences between the iDXA and Prodigy following reanalysis of Prodigy files with enhanced analysis in both adults (20–65 years, n = 69) and school-aged children (6–16 years, n = 124). Among their cohort of children, differences were apparent in all parameters except whole-body, leg, and trunk BMC. Similar to our findings, differences were most pronounced for total FM and LM, which were 0.71 kg (6%) higher and 1.07 kg (3.5%) lower with the Prodigy than the iDXA23.
Although they did not compare basic and enhanced analysis in their study of children, among adults, Watson et al.13 noted no differences in whole-body FM and LM when Prodigy scans were analysed with basic compared to enhanced analysis. However, the authors observed differences in total BMC and bone area and regional FM and LM (arm FM and leg LM). This contrasts with our study, where substantial differences were noted between Prodigy scans analysed with the two software versions for all parameters. In line with our results, Crabtree et al.22 found differences between basic and enhanced analysis when data was pooled from DXA studies involving children aged 4–20 years.
An inherent limitation of using DXA is that although based on basic principles and hence intrinsically accurate, the software used to analyse the data is proprietary. Animal cadaver studies have shown that both the Prodigy and iDXA have good correlation with chemical analysis results, though many body composition parameters were over- or underestimated24,25, which may in part be due to differences in animal tissue thickness26,27 and FFM hydration24,26. The proprietary nature of the software means that we are unable to fully elucidate where differences between the devices may stem from, though our results suggest a larger role of software than instrumentation. However, it is unclear how the enhanced software option that can be applied to Prodigy scans differs from the default iDXA software, and what adjustments are applied to paediatric scans.
An additional limitation of our study is that we could not compare our results to a suitable reference method to determine which of the two DXA scans was most accurate. In early childhood, there is no gold-standard method for assessing body composition. A four-compartment (4C) model may be used as a reference since it provides additional clarification about the composition of the FFM compartment2; however, this would have been time- and resource-intensive. Furthermore, air displacement plethysmography body volume measurements (as required for computation of body composition using a 4C model) are currently not optimised for use at this age28. Nonetheless, a previous study in adults found that the iDXA aligned more closely with a 4C model than results from the Prodigy, although there was a systematic bias, with FM being overestimated among those with greater FM13. This systematic bias in FM was not observed when iDXA measurements were validated against a 4C model in school-aged children, although mean FM was overestimated by 2 kg23. The authors also found iDXA to underestimate FFM by 1.3 kg, with this increasing as total FFM increased23. Correction of iDXA FFM according to individually measured TBW (i.e., correcting for FFM hydration) resulted in a reduction in limits of agreement and removal of the systematic bias. However, a mean bias of approximately 2 kg remained23. In addition to determining which DXA device is more accurate, we acknowledge the need to replicate the adjustment equations in an independent group of children.
In summary, we have conducted the first cross-calibration study of the GE Lunar Prodigy and iDXA in a cohort of young children. There were substantial differences between the iDXA and the Prodigy, which were attenuated following reanalysis of the Prodigy scans with enhanced software. Thus, the same child scanned by the two devices will yield different results in part due to differences in scan resolution but also due to software differences. However, it is difficult to disentangle these differences and to determine which is a more accurate reflection of true body composition. This highlights a key challenge researchers and clinicians face when collecting longitudinal body composition data in children. As manufacturers upgrade devices and software over the duration of a study or clinical observation, it becomes difficult to determine the true trajectory of body composition. Therefore, researchers and clinicians need to consider the manufacturer, model, and software version when conducting DXA scans as results may not be comparable.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available as the participants did not consent to open access data sharing and this is an ongoing longitudinal study in which there will be further future analyses conducted but are available from the corresponding author on reasonable request.
References
Pietrobelli, A., Formica, C., Wang, Z. & Heymsfield, S. B. Dual-energy X-ray absorptiometry body composition model: Review of physical concepts. Am. J. Physiol. Endocrinol. Metab. 271, E941–E951. https://doi.org/10.1152/ajpendo.1996.271.6.E941 (1996).
Demerath, E. W. & Fields, D. A. Body composition assessment in the infant. Am. J. Hum. Biol. 26, 291–304. https://doi.org/10.1002/ajhb.22500 (2014).
International Atomic Energy Agency. Vol. IAEA Human Health Series No. 15 (International Atomic Energy Agency, 2010).
Barbour, L. A. et al. Striking differences in estimates of infant adiposity by new and old DXA software, PEAPOD and skin-folds at 2 weeks and 1 year of life. Pediatr. Obes. 11, 264–271. https://doi.org/10.1111/ijpo.12055 (2016).
Brunton, J. A., Weiler, H. A. & Atkinson, S. A. Improvement in the accuracy of dual energy X-ray absorptiometry for whole body and regional analysis of body composition: validation using piglets and methodologic considerations in infants. Pediatr. Res. 41, 590–596. https://doi.org/10.1203/00006450-199704000-00022 (1997).
Shypailo, R. J., Butte, N. F. & Ellis, K. J. DXA: Can it be used as a criterion reference for body fat measurements in children?. Obesity (Silver Spring) 16, 457–462. https://doi.org/10.1038/oby.2007.81 (2008).
Koo, W. W., Hockman, E. M. & Hammami, M. Dual energy X-ray absorptiometry measurements in small subjects: Conditions affecting clinical measurements. J. Am. Coll. Nutr. 23, 212–219. https://doi.org/10.1080/07315724.2004.10719363 (2004).
GE Healthcare. Lunar Technology Advantages. https://www.gehealthcare.de/-/jssmedia/feature/gehc/products/lunar-idxa/lunartechnology.pdf?rev=-1. (2017). Accessed on 31 March 2021.
Morrison, S. A., Petri, R. M., Hunter, H. L., Raju, D. & Gower, B. Comparison of the lunar prodigy and iDXA dual-energy X-ray absorptiometers for assessing total and regional body composition. J. Clin. Densitom. 19, 290–297. https://doi.org/10.1016/j.jocd.2015.06.003 (2016).
Oldroyd, B., Treadgold, L. & Hind, K. Cross calibration of the GE prodigy and iDXA for the measurement of total and regional body composition in adults. J. Clin. Densitom. 21, 383–393. https://doi.org/10.1016/j.jocd.2017.05.009 (2018).
Ramirez, E. A., Escalante, G. & Chen, Z. Cross-calibration of GE Lunar iDXA and Prodigy Densitometer for measurement of bone mineral density in young adults. J. Kinesiol. Wellness 9, 38–46 (2020).
Hind, K., Cooper, W., Oldroyd, B., Davies, A. & Rhodes, L. A cross-calibration study of the GE-Lunar iDXA and prodigy for the assessment of lumbar spine and total hip bone parameters via three statistical methods. J. Clin. Densitom. 18, 86–92. https://doi.org/10.1016/j.jocd.2013.09.011 (2015).
Watson, L. P. E., Venables, M. C. & Murgatroyd, P. R. An Investigation into the differences in bone density and body composition measurements between 2 GE lunar densitometers and their comparison to a 4-component model. J. Clin. Densitom. 20, 498–506. https://doi.org/10.1016/j.jocd.2017.06.029 (2017).
Godfrey, K. M. et al. Nutritional intervention preconception and during pregnancy to maintain healthy glucose metabolism and offspring health (“NiPPeR”): Study protocol for a randomised controlled trial. Trials 18, 131. https://doi.org/10.1186/s13063-017-1875-x (2017).
Redman, L., Hsia, D. & Carmichael, O. Measurement of Body Fat in Infants: "Baby Fat Pilot". https://clinicaltrials.gov/ProvidedDocs/27/NCT03490227/Prot_SAP_000.pdf (2018). Accessed on 5 July 2022.
Toombs, R. J., Ducher, G., Shepherd, J. A. & De Souza, M. J. The impact of recent technological advances on the trueness and precision of DXA to assess body composition. Obesity (Silver Spring) 20, 30–39. https://doi.org/10.1038/oby.2011.211 (2012).
United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). Sources and Effects of Ionizing Radiation. http://www.unscear.org/docs/reports/2008/09-86753_Report_2008_GA_Report.pdf (2008). Accessed on 5 July 2022.
Moon, R. J. et al. Is the skull responsive to bone mineralisation stimuli in children?. Bone 160, 116415. https://doi.org/10.1016/j.bone.2022.116415 (2022).
Shuhart, C. R. et al. Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J. Clin. Densitom. 22, 453–471. https://doi.org/10.1016/j.jocd.2019.07.001 (2019).
Blake, G. M. Replacing DXA scanners: Cross-calibration with phantoms may be misleading. Calcif. Tissue Int. 59, 1–5. https://doi.org/10.1007/s002239900075 (1996).
Khadilkar, A. et al. A cross-calibration study of GE lunar iDXA and GE lunar DPX pro for body composition measurements in children and adults. J. Clin. Densitom. 23, 128–137. https://doi.org/10.1016/j.jocd.2019.03.003 (2020).
Crabtree, N. J. et al. Amalgamated reference data for size-adjusted bone densitometry measurements in 3598 children and young adults—The ALPHABET study. J. Bone Miner. Res. 32, 172–180. https://doi.org/10.1002/jbmr.2935 (2017).
Watson, L. P. E., Carr, K. S., Orford, E. R. & Venables, M. C. The Importance of hydration in body composition assessment in children aged 6–16 years. J. Clin. Densitom. https://doi.org/10.1016/j.jocd.2020.12.004 (2020).
Schallier, S. et al. Dual-energy X-ray absorptiometry is a reliable non-invasive technique for determining whole body composition of chickens. Poult. Sci. 98, 2652–2661. https://doi.org/10.3382/ps/pez013 (2019).
Kasper, C., Schlegel, P., Ruiz-Ascacibar, I., Stoll, P. & Bee, G. Accuracy of predicting chemical body composition of growing pigs using dual-energy X-ray absorptiometry. bioRxiv. https://doi.org/10.1101/2020.09.15.286153 (2020).
Pomar, C., Kipper, M. & Marcoux, M. Use of dual-energy X-ray absorptiometry in non-ruminant nutrition research. Revista Brasileira de Zootecnia 46, 621–629. https://doi.org/10.1590/s1806-92902017000700010 (2017).
Kipper, M., Pomar, C., Marcoux, M. & Radünz Neto, J. Evaluation of DXA technology to study the composition of pig carcasses and primal cuts. Journées de la Recherche Porcine en France 47, 31–36 (2015).
Gallagher, D. et al. Body composition measurements from birth through 5 years: Challenges, gaps, and existing & emerging technologies—A national institutes of health workshop. Obes. Rev. https://doi.org/10.1111/obr.13033 (2020).
Acknowledgements
The authors would like to acknowledge Auckland NiPPeR research staff Christine Creagh, Marysia Depczynski, and Sarah Wilkins for their contribution to this study, staff at the University of Auckland Clinical Research Centre for facilitating the use of their GE Lunar Prodigy, and Paul Markwardt at GE Lunar for his critical review of the final manuscript. Public good funding for the investigator-led NiPPeR study is through the UK Medical Research Council (as part of an MRC award to the MRC Lifecourse Epidemiology Unit (MC_UU_12011/4)); the Singapore National Research Foundation, National Medical Research Council (NMRC, NMRC/TCR/012-NUHS/2014); the National University of Singapore (NUS) and the Agency of Science, Technology and Research (as part of the Growth, Development and Metabolism Programme of the Singapore Institute for Clinical Sciences (SICS) (H17/01/a0/005); and as part of Gravida, a New Zealand Government Centre of Research Excellence. Funding for aspects of the NiPPeR study has been provided by Société Des Produits Nestlé S.A under a Research Agreement with the University of Southampton, Auckland UniServices Ltd, SICS, National University Hospital Singapore PTE Ltd and NUS. JL is supported by a University of Auckland Doctoral Scholarship. KMG is supported by the National Institute for Health Research (NIHR Senior Investigator (NF-SI-0515-10042), NIHR Southampton 1000DaysPlus Global Nutrition Research Group (17/63/154) and NIHR Southampton Biomedical Research Center (IS-BRC-1215-20004)), British Heart Foundation (RG/15/17/3174) and the European Union (Erasmus+ Programme ImpENSA 598488-EPP-1-2018-1-DE-EPPKA2-CBHE-JP). SYC is supported by a Singapore NMRC Clinician Scientist Award (NMRC/CSA-INV/0010/2016; MOH-CSAINV19nov-0002). NH is supported by the UK Medical Research Council (MC_PC_21003; MC_PC_21001). The funders had no role in the data collection and analysis, and the decision to submit for publication. For the purpose of Open Access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
W.S.C., T.K., and B.B.A. supervised all aspects of the research study. K.M.G., S.Y.C., and W.S.C. led the NiPPeR trial conception and design. J.L., W.S.C., and T.K., conceived and designed the DXA cross-calibration sub-study. J.L. compiled the data and carried out the statistical analyses. J.L. wrote the manuscript with critical input from all other authors. All authors have approved the final version of this manuscript and have agreed to be accountable for all aspects of this work.
Corresponding author
Ethics declarations
Competing interests
KMG, SYC, and WSC are part of an academic consortium that has received grants from Société Des Produits Nestlé S.A. outside the submitted work. SYC and KMG have received reimbursement for speaking at conferences sponsored by companies selling nutritional products. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lyons-Reid, J., Kenealy, T., Albert, B.B. et al. Cross-calibration of two dual-energy X-ray absorptiometry devices for the measurement of body composition in young children. Sci Rep 12, 13862 (2022). https://doi.org/10.1038/s41598-022-17711-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17711-0
This article is cited by
-
Prediction of fat-free mass in young children using bioelectrical impedance spectroscopy
European Journal of Clinical Nutrition (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.