Abstract
We attempted to assess the performance of an ethnic-specific polygenic risk score (PRS) designed from a Korean population to predict aggressive prostate cancer (PCa) and early-onset (age < 60). A PRS score comprised of 22 SNPs was computed in 3695 patients gathered from one of 4 tertiary centers in Korea. Males with biopsy or radical prostatectomy-proven PCa were included for analysis, collecting additional clinical parameters such as age, BMI, PSA, Gleason Group (GG), and staging. Patients were divided into 4 groups of PRS quartiles. Intergroup differences were assessed, as well as risk ratio and predictive performance based on GG using logistic regression analysis and AUC. No significant intergroup differences were observed for BMI, PSA, and rate of ≥ T3a tumors on pathology. Rate of GG ≥ 2, GG ≥ 3, and GG ≥ 4 showed a significant pattern of increase by PRS quartile (p < 0.001, < 0.001, and 0.039, respectively). With the lowest PRS quartile as reference, higher PRS groups showed sequentially escalating risk for GG ≥ 2 and GG ≥ 3 pathology, with a 4.6-fold rise in GG ≥ 2 (p < 0.001) and 2.0-fold rise in GG ≥ 3 (p < 0.001) for the highest PRS quartiles. Combining PRS with PSA improved prediction of early onset csPCa (AUC 0.759) compared to PRS (AUC 0.627) and PSA alone (AUC 0.736). To conclude, an ethnic-specific PRS was found to predict susceptibility of aggressive PCa in addition to improving detection of csPCa when combined with PSA in early onset populations. PRS may have a role as a risk-stratification model in actual practice. Large scale, multi-ethnic trials are required to validate our results.
Similar content being viewed by others
Introduction
Incidence of prostate cancer (PCa) is constantly on the rise, especially with introduction of nationwide early PSA screening, westernized diets with high dietary fat, and increase in average life expectancy1. Such increase is more marked in East Asian countries, where PCa is known to take on a more aggressive form2, which can be explained by both genetic predisposition and environmental effects3. However, conventional screening with PSA alone is vastly limited, due to ambiguities affecting PSA levels such as prostatitis or benign hyperplasia. This has fueled the need for additional biomarkers more specific to PCa, in order to tailor screening and intervention methods and aid clinical decision making process.
Interest in genetic association of PCa has rapidly grown with the finding of nominal mutations eligible for therapy, such as BRCA 1/2 that have been recently indicated for treatment with PARP (Poly-ADP ribose polymerase) inhibitors through major clinical trials4. However, as not all genetic background of PCa can be explained with the inheritance of high penetrance genes alone, research on the combinatory effect of small genetic variants or SNPs (single nucleotide polymorphisms) has gained popularity, with numerous positive results on different models utilizing the technique5,6,7. A recent multi-ethnic study found more than a fivefold increase in risk for any PCa and PCa-related deaths8.
While a handful of models with moderate predictive performance have been introduced using polygenetic risk in PCa, there is a disproportion in the level of evidence available for models to be used in Asian populations. Most models use datasets that consists of largely European heritage, leading to an overwhelming under-representation of Asian genetics, while many studies have underlined the difference in variants by ethnicity9,10. Also, while previous results have found significant findings for SNP-based prediction of any PCa5, whether such models can predict aggressiveness or early onset still requires further research. In this study, we aimed to test a polygenic risk score (PRS) model for prediction of high-risk, aggressive PCa and examine performance in patients with early age at diagnosis.
Materials and methods
Study population and genotyping
Data for this multicenter study was gathered from 4 tertiary medical centers (Seoul National University of Bundang Hospital, Seoul National University of Hospital, Chungbuk National University Hospital and the Catholic University St. Vincent hospital Seoul) and was Institutional Review Board approved at SNUBH (B-1607/355-302). Informed consent for study and genotyping was obtained for all subjects. Patients who had biopsy or pathology proven PCa through transrectal ultrasound prostate biopsy and/or radical prostatectomy (RP) were included for analysis. Healthy controls with genotyped data were also included. All patients were of Asian (Korean) ethnicity. Routine clinical parameters including age, BMI, PSA, Gleason Scores (grade groups), and clinicopathological staging were obtained. Genotyping was performed using the Korea Biobank array (K-CHIP) per manufacturer instructions with 200 ng of DNA from blood or saliva11. Clinically significant PCa (csPCa) was defined as Grade group (GG) ≥ 2. All methods included in this study was carried out in accordance with relevant guidelines and regulations.
PRS model development
The PRS model described in a previous study12 were implemented for calculating genetic risk in the study participants. PRS is an aggregate sum of the effect size estimate or Cox proportional hazard ratio multiplied by the number of risk alleles found in the patient’s genotype13. Our PRS was developed using 10,187 genetic samples with 2702 PCa cases and 7485 controls, later validated with in an independent cohort with 311 cases and 822 controls, achieving a performance of AUC 0.700 (95% CI 0.667–0.734) with 29 top SNPs included. In this study, a 22 SNP model with reported AUC of 0.689 (95% CI 0.655–0.723) in csPCa were included after filtering excess SNPs with inadequately low allele frequencies or call rates (Supplementary Table 1). A single SNP (rs72725879) was replaced with the next highest performing variant (rs1456315) in the same LD block (Locus PRNCR1) due to replication inconsistencies when constructed as a custom array. All candidate SNPs during initial development were chosen only if proven on association studies in previous literature. Details on model development can be found in a previous article12.
Statistical analysis
Patients were divided into 4 groups based on calculated PRS by quartile (0–24.9, 25–49.9, 50–74.9, 75–100th percentile). Subsets were further assessed for intergroup differences in GG distribution as well as pathologic grade, using student t-tests, Pearson Chi, and ANOVA statistics for continuous, categorical, and multi-categorical variables. Overall model predictive performance was evaluated using Area Under Receiver Operating Characteristic (AUROC, AUC). Logistic regression analysis was performed for PCa risk. All statistical analyses were performed using IBM SPSS software package version 25.0 (Statistical Package for Social Sciences™, Chicago, IL, USA).
Results
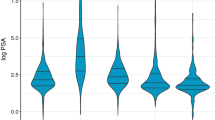
Total 3695 patients were included in final analysis, of whom 3203 were PCa patients and 483 controls. Mean age for the overall sample population was 67.3, with mean PSA of 29.8 ± 192.2 ng/ml (Table 1). 132 patients (4.1%) harbored GG1 tumors overall, and others comprised of 26.8% GG2, 41.1% GG3, and 28.0% > GG4. 2170 patients (58.7%) underwent RP for csPCa, with 823 patients harboring high stage tumors (≥ pT3a) at final pathology. When divided by PRS quartiles, no significant intergroup differences were observed for BMI, PSA, and rate of high stage tumors at RP pathology. Only age between the 25–49.9th percentile and 75–100th percentile was found to be significant (p = 0.036), with no other notable intergroup outcome distinctions.
However, rate of csPCa showed a sequential increase, from 70.0% patients harboring GG ≥ 2 in the first quartile, to 83.1%, 87.5%, and 91.6% in the 2nd, 3rd, and 4th quartiles, respectively (p < 0.001) (Fig. 1). Rate of intermediate to high-risk pathology showed a similar pattern, with GG ≥ 3 increasing from 50.3% in the bottom quartile to 58.5%, 63.4%, and 67.2% in the 2nd, 3rd, and 4th quartiles, respectively (< 0.001). Rate of GG ≥ 4 resembled a comparable increase in the first 3 quartiles from 21.1%, 23.9%, to 26.5%, but was slightly decreased in the highest quartile with 25.4% (p = 0.039).
When using the lowest PRS quartile as reference (< 25 percentile), all sequential higher PRS risk groups showed an increase in risk for GG ≥ 2 and ≥ 3 tumor pathology (Table 2). Patients with the highest genetic risk based on PRS (≥ 75 centile) had a 4.6-fold increased risk for clinically significant disease (95% CI 3.544–6.098, p < 0.001), as well as a 2.0-fold increased risk for more aggressive GG ≥ 3 tumors.
PRS alone showed a moderate predictive performance of AUC 0.627 (95% CI 0.550–0.703, p = 0.002) for men with early-onset csPCa before the age of 60 (Fig. 2), with PSA outperforming PRS alone with AUC 0.736 (95% CI 0.666–0.805, p < 0.001). However, when combined with PSA, the clinicogenetic model of PRS + PSA outperformed either model with a AUC of 0.759 (95% CI 0.694–0.823, p < 0.001), suggesting the clinical utility of PRS for detection of early-onset disease requiring active intervention.
Discussion
In this multicenter analysis of polygenetic risk for PCa, a PRS model constructed in a predominantly Asian population resulted in an increasing rate of high grade tumors detected at RP or biopsy in males with higher PRS. Patients with the highest genetic risk in the top quartile showed a 4.6-fold and 2.0-fold increase in GG ≥ 2 and GG ≥ 3 pathology, respectively. For men with early-onset disease (GG ≥ 2 prior to age 60), combination of PRS to the conventional PSA model improved predictive performance of AUC 0.759, from AUC 0.736 and 0.627 in PRS and PSA alone, respectively. These findings further support the feasibility and usefulness of genetic models for prediction and stratification of high risk patients based on germline mutation, especially via ethnic-specific models.
Previous studies on genomic risk from GWAS summary statistics laid strong foundations for any PCa risk but show mixed results on the ability to predict aggressive, intermediate-high risk disease14. A meta-analysis comprised of over 100,000 cases and 120,000 controls showed that a genetic score aggregate of total 269 risk variants was significantly associated with three to fivefold increase in absolute risk for PCa across ancestry, but was not able to differentiate aggressive disease defined as ≥ T3, regional N1/M1+, GG ≥ 4, or PSA ≥ 20 ng/ml9. The large model developed and validated in a Japanese-specific cohort found no difference in aggressive PC despite moderate performance of AUC 0.679 for any PCa15. A multiethnic dataset of approximately 50,000 cases and 30,000 controls8 described positive predictive performance of PRS to detect aggressive PCa, where HR for ≥ T3, regional N1/M1+, GG ≥ 2, or PSA ≥ 10 ng/ml was significantly higher in the top 20th percentile, with near 4.5-fold increase in the Asian subset. A more recent study in European men found a strong association for overall-risk increase for PCa based on PRS stratification, but not for high-grade tumors16. Other studies have produced similar results, with no strong association with tumor grade and aggressiveness5,17. As such, the results from our finding establishes potential for possible stratification for high-grade disease based on PRS, with sequential increase in GG ≥ 4 tumors being identified even within a case–control cohort largely composed of PCa patients. However, limitations of relatively few controls and overall small sample size, as well as lack of family history information must be addressed to fully explain the differences in tumor grade distribution in our study.
While patients diagnosed with PCa at a young age are evidently at risk for high penetrance pathogenic germline mutations such as BRCA1/218 or HOXB1319, predicting earlier age of onset based on multiple variants with small effect size potential have produced ambiguous results, with a previous study20 finding a PRS of 24 SNPs to be discriminatory for any and high grade GG ≥ 2 PCa only between age 60–70 years, losing predictive value in younger patients, most likely due to low prevalence and high likelihood of low-grade disease in this age group. Recent results from a Japanese cohort of 4893 PCa cases6 found patients with high PRS to have a younger mean age at diagnosis by 2.7 years (68.7 vs. 71.4 years in the top and bottom 5%, respectively), but weakened statistical association between PRS and early onset PCa when discarding variants without significant association with Japanese PCa. On the other hand, Seibert et al. designed a PRS utilizing data from the PRACTICAL consortium and UK ProtecT study, and found that a score of 54 SNPs were significantly predictive of early age at diagnosis of aggressive PCa5. A meta-analysis in males of European ancestry identified a novel locus rs138004030 for age of onset ≤ 5521, adding to the list of risk alleles significant for diagnosis ≤ 50 years in predominantly Caucasian dataset22.
Discrepancies in PRS performance by ethnic groups is not new, due to obvious variations in genetics as well as sociocultural environments. As such, accurate estimation of genetic contribution to PCa development inevitably requires development of ethnic-specific optimization9. However, Asian populations are vastly under-represented in most GWAS summary statistics, limiting direct implementation and generalizability in different patient populations and few PRS currently developed23. In this study, a KoreanChip customized for optimal evaluation including rare and novel variants found in Korean patients were utilized11, improving coverage and better representing genomic variations in East Asians. In order avoid overfitting by inclusion of non-PCa associated SNPs with high statistical significance, only variants with literature evidence for PCa risk in East Asians were included for PRS development. Also, as sample size is critical to accurate estimation of variant risk in a population, this study has strengths by using one of the largest patient cohorts in an East Asian population to our knowledge.
To note, the mean age of patients included this study were not vastly different by PRS quartiles, with the only significant difference found between the top quartile and patients in the 25–50th percentile (Table 1). PSA was also not significant for intergroup difference when stratified by PRS, suggesting the potential clinical utility of PRS when used as a reflex test when PSA alone is limiting. In fact, the clinicogenetic model of PSA augmented with PRS showed best performance, suggesting the additive value in real-life scenarios when other PCa parameters such as DRE positivity, MRI findings, or other biomarkers (e.g. 4 K Score, prostate health index) are used in clinical decision making.
Our study is not without limitations. First, family history of PCa was not including for analysis. Familial PCa is undeniably important in PCa risk analysis, with a person with 2 first-degree relatives inflicted with PCa to be 5 times more likely to develop the disease during his lifetime24. However, in previous literature5, the predictive performance of a PRS did not improve nor was undermined by the inclusion and exclusion of family history, and may not have had a detrimental effect on our model. Second, only Korean populations ethnicities were included during analysis, and while this does reinforce tailoring to East Asian populations, further assessment for generalizability of the model is essential. In addition, while the effect size estimates for variants were calculated from a previous cohort including over 7000 healthy controls, fewer healthy controls were included in this study, as the intent was to evaluate its ability to discriminate high-risk subgroups within PCa populations. While enrolled patients have considerable overlap to our previous study and may have caused an overfitting bias, these results indicate that PRS has the potential to discriminate and stratify high-grade, aggressive tumors among csPCa. Also, routine clinical parameters such as prostate volume or MRI findings were not available for analysis, the inclusion of which could have enhanced model performance. Inquiry for role in treatment selection in specific subgroups such as patients eligible for active surveillance requires further research, especially in Asian populations where the criteria for enrollment is still unclear25 due to different tumor characteristics.
Despite these limitations, this study shows that a PRS can be readily exploited in practice for predicting aggressive tumors that may occur early on in males with high genetic risk based on SNP mutations. While PRS may be inadequate as a diagnostic tool, it holds strong potential for diversifying screening and intervention strategies depending on germline risk in the era of precision medicine.
Conclusion
A PRS specific to Asian males was found to increase detection of aggressive tumors, with men in the top 25 percentile harboring more than fourfold risk for GG ≥ 2 and twofold risk for GG ≥ 3 pathology. PRS combined with PSA was able to better predict early onset, outperforming PSA alone. These results bolster the role of genetic testing in risk stratification in PCa patients and provide evidence for active implementation in early stages of patient screening and diagnosis. Future validation in multi-ethnic cohorts are required to broaden potential applications.
References
Han, H. H. et al. Epidemiology of prostate cancer in South Korea. Prostate Int. 3, 99–102. https://doi.org/10.1016/j.prnil.2015.06.003 (2015).
Jeong, I. G. et al. Differences in the aggressiveness of prostate cancer among Korean, Caucasian, and African American men: A retrospective cohort study of radical prostatectomy. Urol. Oncol. 34(3), e9–e14. https://doi.org/10.1016/j.urolonc.2015.08.004 (2016).
HaChung, B., Horie, S. & Chiong, E. The incidence, mortality, and risk factors of prostate cancer in Asian men. Prostate Int. 7, 1–8. https://doi.org/10.1016/j.prnil.2018.11.001 (2019).
de Bono, J. et al. Olaparib for metastatic castration-resistant prostate cancer. N. Engl. J. Med. 382, 2091–2102. https://doi.org/10.1056/NEJMoa1911440 (2020).
Seibert, T. M. et al. Polygenic hazard score to guide screening for aggressive prostate cancer: Development and validation in large scale cohorts. BMJ 360, j5757. https://doi.org/10.1136/bmj.j5757 (2018).
Takata, R. et al. 12 new susceptibility loci for prostate cancer identified by genome-wide association study in Japanese population. Nat. Commun. 10, 4422. https://doi.org/10.1038/s41467-019-12267-6 (2019).
Gronberg, H. et al. Prostate cancer screening in men aged 50–69 years (STHLM3): A prospective population-based diagnostic study. Lancet Oncol. 16, 1667–1676. https://doi.org/10.1016/S1470-2045(15)00361-7 (2015).
Huynh-Le, M. P. et al. Polygenic hazard score is associated with prostate cancer in multi-ethnic populations. Nat. Commun. 12, 1236. https://doi.org/10.1038/s41467-021-21287-0 (2021).
Conti, D. V. et al. Trans-ancestry genome-wide association meta-analysis of prostate cancer identifies new susceptibility loci and informs genetic risk prediction. Nat. Genet. 53, 65–75. https://doi.org/10.1038/s41588-020-00748-0 (2021).
Hoffmann, T. J. et al. A large multiethnic genome-wide association study of prostate cancer identifies novel risk variants and substantial ethnic differences. Cancer Discov. 5, 878–891. https://doi.org/10.1158/2159-8290.CD-15-0315 (2015).
Moon, S. et al. The Korea Biobank array: Design and identification of coding variants associated with blood biochemical traits. Sci. Rep. 9, 1382. https://doi.org/10.1038/s41598-018-37832-9 (2019).
Song, S. H. et al. Prediction of clinically significant prostate cancer using polygenic risk models in Asians. Investig. Clin. Urol. 63, 42 (2022).
Choi, S. W., Mak, T. S. & O’Reilly, P. F. Tutorial: A guide to performing polygenic risk score analyses. Nat. Protoc. 15, 2759–2772. https://doi.org/10.1038/s41596-020-0353-1 (2020).
Catalona, W. J. et al. National Cancer Institute Prostate Cancer Genetics Workshop. Cancer Res. 71, 3442–3446. https://doi.org/10.1158/0008-5472.CAN-11-0314 (2011).
Akamatsu, S. et al. Reproducibility, performance, and clinical utility of a genetic risk prediction model for prostate cancer in Japanese. PLoS ONE 7, e46454. https://doi.org/10.1371/journal.pone.0046454 (2012).
Plym, A. et al. Evaluation of a multiethnic polygenic risk score model for prostate cancer. J. Natl. Cancer Inst. 114, 771–774. https://doi.org/10.1093/jnci/djab058 (2022).
Black, M. H. et al. Validation of a prostate cancer polygenic risk score. Prostate 80, 1314–1321. https://doi.org/10.1002/pros.24058 (2020).
Nyberg, T., Tischkowitz, M. & Antoniou, A. C. BRCA1 and BRCA2 pathogenic variants and prostate cancer risk: Systematic review and meta-analysis. Br. J. Cancer. https://doi.org/10.1038/s41416-021-01675-5 (2021).
Ewing, C. M. et al. Germline mutations in HOXB13 and prostate-cancer risk. N. Engl. J. Med. 366, 141–149. https://doi.org/10.1056/NEJMoa1110000 (2012).
Zhu, Y. et al. Influence of age on predictiveness of genetic risk score for prostate cancer in a Chinese hospital-based biopsy cohort. Oncotarget 6, 22978–22984. https://doi.org/10.18632/oncotarget.3938 (2015).
Schumacher, F. R. et al. Association analyses of more than 140,000 men identify 63 new prostate cancer susceptibility loci. Nat. Genet. 50, 928–936. https://doi.org/10.1038/s41588-018-0142-8 (2018).
Lange, E. M. et al. Early onset prostate cancer has a significant genetic component. Prostate 72, 147–156. https://doi.org/10.1002/pros.21414 (2012).
Song, S. H. & Byun, S. S. Polygenic risk score for genetic evaluation of prostate cancer risk in Asian populations: A narrative review. Investig. Clin. Urol. 62, 256–266. https://doi.org/10.4111/icu.20210124 (2021).
Steinberg, G. D., Carter, B. S., Beaty, T. H., Childs, B. & Walsh, P. C. Family history and the risk of prostate cancer. Prostate 17, 337–347. https://doi.org/10.1002/pros.2990170409 (1990).
Song, S. H. et al. A single-center long-term experience of active surveillance for prostate cancer: 15 years of follow-up. Investig. Clin. Urol. 62, 32–38. https://doi.org/10.4111/icu.20200206 (2021).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea government (MSIT) (No. NRF-2020R1F1A1070203) and by Grant No. 18-2018-003 from the Seoul National University Bundang Hospital (SNUBH) Research Fund.
Author information
Authors and Affiliations
Contributions
S.H.S.: investigation, writing original draft, review & editing. E.K.: conceptualization, investigation, analyses. Y.J.J.: conceptualization, investigation, analyses. H.K.: investigation, analyses, project administration. J.K.K: investigation, supervision. H.L.: supervision. J.J.O.: analyses, supervision. S.L.: investigation, supervision. S.K.H.: investigation, supervision. S.S.B.: conceptualization, investigation, review & editing, funding acquisition. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Eunae Kim, Yu Jin Jung, Hamin Kim are employees, Seok-Soo Byun is the chief executive officer, and Jong Jin Oh is the inside director of Procagen. Sang Hun Song, Eunae Kim, Hakmin Kim, Moon Soo Park, Jung Kwon Kim, Hakmin Lee, Jong Jin Oh, Sangchul Lee and Seok-Soo Byun have an equity interest in Procagen. All other authors report no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, S.H., Kim, E., Jung, Y.J. et al. Polygenic risk score for tumor aggressiveness and early-onset prostate cancer in Asians. Sci Rep 13, 798 (2023). https://doi.org/10.1038/s41598-022-17515-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17515-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.