Abstract
This study aimed to examine the association between lifestyle factors and metabolic syndrome risk in South Korean adults. Korea National Health and Nutrition Examination Survey 2016–2018 data were used. The study included 6,995 subjects (2835 male; 4,160 female). Multiple logistic regression was used to estimate the relationship between the lifestyle factors, including sedentary time, sleep duration, alcohol consumption, smoking status, and dietary intake. Metabolic syndrome prevalence in healthy adults was 25.6% and 12.4% in men and women, respectively. Male with over four lifestyle risk factors had a higher OR for metabolic syndrome risk (over four lifestyle factors: OR 1.97, CI 1.18–3.27). Female with more than one lifestyle risk factor had a higher OR for metabolic syndrome risk (one lifestyle factor: OR 1.58, CI 1.10–2.28; two lifestyle factors: OR 2.08, CI 1.39–3.11; three lifestyle factors: OR 1.94, CI 1.20–3.13). In particular, female with more lifestyle factors had increased likelihood of abdominal obesity, hypertension, and high triglycerides. Male with more lifestyle factors had increased likelihood of high triglycerides. Sedentary time was significantly associated with increased metabolic syndrome in male and female. This study found a significant association between the number of lifestyle risk factors and the risk of metabolic syndrome in Korean adults. The greater the number of lifestyle risk factors, the higher the risk of metabolic syndrome in both sexes. People with a greater number of poor lifestyle behaviors tended to exhibit increased likelihood of especially elevated triglyceride levels.
Similar content being viewed by others
Introduction
Due to the association between cardiovascular disease and metabolic syndrome as well as their common occurrence, researchers have exhibited keen interest in these conditions1. People with metabolic syndrome have high risks of morbidity and mortality because of cardiovascular disease and type 2 diabetes2. The prevalence of metabolic syndrome in Korean adults increased from 24.9% in 1998 to 31.3% in 2007. In other words, approximately one in three adults in Korea has metabolic syndrome3. Further, cardiovascular disease incidence has continuously increased over the past 10 years and has become the second most common cause of mortality in Korea4. Due to increasing disease duration and accompanying disabilities, the socioeconomic burden posed by these diseases is predicted to increase5. Therefore, it is important to prevent and reduce the prevalence of metabolic syndrome.
The World Health Organization (WHO) defined metabolic syndrome as a pathologic condition comprising abdominal obesity, insulin resistance, hypertension, and hyperlipidemia. Metabolic syndrome is not a single disease but a group of risk factors for cardiovascular disease6.
The main strategy for metabolic syndrome prevention and treatment are the change of poor lifestyle through various approach based on physical exercise, a healthy diet and education. It means that risk factors for metabolic syndrome can be mitigated by modifiable lifestyle factors7. To support this opinion, there are various studies related to risk factor of metabolic syndrome and lifestyle intervention for metabolic syndrome8,9. For instance, prior studies suggests that lifestyle risk factors, such as poor diet, alcohol consumption, physical inactivity, smoking, and sedentary time increase the risk of metabolic syndrome9,10,11,12.
According to recent studies, sleep duration is also a lifestyle factor that potentially acts as an important health status indicator13. To reduce the prevalence of metabolic syndrome, lifestyle and pharmacological method modifications are of paramount importance.
Whereas many studies are focused on the prevalence of single- or double-risk factors and their association with metabolic syndrome, including that in people with comorbid disease14,15, we investigated the association of overalllifestyle factors with metabolic syndrome and its affected components of metabolic syndrome, excluding that in patients with comorbid disease. Such a design potentially demonstrates the prevalence, trends, and determinants of metabolic syndrome. Accordingly, in the present study, we used cross-sectional data to examine the association of lifestyle risk factors with the risk of metabolic syndrome and its components. An enhanced understanding of the association between lifestyle behavior and metabolic syndrome potentially improves the planning of new effective health programs and result in improved health outcomes.
Methods
This cross-sectional study used data from the 2016–2018 Korea National Health and Nutrition Examination Survey (KNHANES) conducted by the Korea Centers for Disease Control and Prevention. The KNHANES is a cross-sectional, nationally representative survey that has been conducted regularly since 1998 to examine the general health and nutritional status of Korean citizens. Our study did not require Institutional Review Board approval because the KNHANES provides a secondary dataset, which is available in the public domain and does not contain private information. And respondents consented the survey for collecting data before participating in the survey16.
Participants
The total survey population from 2016 to 2018 included 24,269 individuals. Individuals younger than 19 years of age (n = 4880) were excluded. Moreover, we excluded individuals undergoing treatment for previously diagnosed hypertension (n = 4223), diabetes mellitus (n = 1697), and hyperlipidemia (n = 2358) as well as those with diagnoses of angina (n = 362), myocardial infarction (n = 209), and stroke (n = 421). Finally, 6995 participants were selected for participation in this study after excluding missing data (n = 7,347).
Variables
The main variables in this study were the number of abnormal lifestyle among the following five lifestyle factors: sleep duration, sedentary time, alcohol use disorders, smoking status, and dietary intake, the data of which were self-reported. Sleep duration was assessed using the following question: “How long do you usually sleep on a weekday and weekend?” Sleep duration was calculated as the total five-weekday plus total two-day-weekend sleep durations divided by 7 days. Subjects were categorized into two groups: (1) short sleep (< 6 h) and long sleep (≥ 9 h) duration and (2) normal sleep duration (6 h ≤ and < 9 h). Sedentary time was assessed using the following question: “How much time do you usually spend sitting?” The sedentary time was then calculated by dividing the sitting time by the time spent awake. Thereafter, we set the median as the cutoff, resulting in one category being Q1–Q2 and the other Q3–Q4: (1) normal sedentary time (Q1–Q2) (2) long sedentary time (Q3–Q4). In a previous study, shorter sleep duration was found to be related to a longer sedentary time17. We used the Alcohol Use Disorders Identification Test (AUDIT-C) score to assess the pattern of alcohol use disorders as follows:
-
1.
“How often have you had a drink containing alcohol in the last year?”
-
2.
“How many drinks containing alcohol did you have on a typical drinking day in the last year?”
-
3.
“How often in the last year have you had six or more drinks on one occasion?”
A high-risk alcohol level was assigned an AUDIT-C score ≥ 8 for both sexes. Subjects were categorized into two groups: (1) never-mild drinking (AUDIT-C < 8), (2) heavy drinking (AUDIT-C ≥ 8). Smoking status was divided into the following two categories: (1) ex- or never-smoker and (2) current smoker. Dietary intake was assessed using the 24-h dietary recall method. We categorized carbohydrate and fat consumption reflected current dietary by cutoff which was recommended by the Korea Ministry of Health and Welfare and the Korean Nutrition Society18,19: poor dietary pattern was defined as having one or two of the following two components: (1) high fat intake corresponded to exceeding 30% of dietary energy intake and (2) high carbohydrate intake corresponded to exceeding 65% of dietary energy intake. If either component is applicable, it was assigned to the abnormal group.
The dependent variable was metabolic syndrome. The definition provided by the modified Third National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults as well as the specific waist circumference values provided by the WHO and Korean Society for the Study of Obesity were used to determine metabolic syndrome and its components20, which were as follows: (1) abdominal obesity (waist circumference ≥ 90 cm in men and ≥ 85 cm in women), (2) high blood pressure (systolic ≥ 130 mmHg or diastolic ≥ 85 mmHg), (3) low high-density lipoprotein cholesterol level (< 40 mmHg/dL in men and < 50 mm/dL in women), (4) high triglyceride level (≥ 150 mg/dL), and (5) high glucose level (≥ 100 mg/dL).
We controlled for participant’s covariates, such as sociodemographic and socioeconomic factors, health behaviors, and health conditions, in this study. The sociodemographic factors were age (19–29, 30–39, 40–49, 50–59, and ≥ 60 years) and sex (male and female). The socioeconomic factors were education level (middle school or lower, high school, or university or higher), region (metropolitan or rural area), marital status (married or not married), occupation (white collar, pink collar, blue collar, or unemployed), and household income (high, middle-high, middle-low, or low). Health conditions included subjective health condition (good, normal, or bad); stress (yes or no); and family history of hypertension, diabetes mellitus, and/or hyperlipidemia (yes or no).
Statistical analysis
To confirm the association between lifestyle risk factors and the risk of metabolic syndrome, the covariates were compared using the chi-squared test. Multiple logistic regression analysis was performed to evaluate the relationship between lifestyle risk factors and metabolic syndrome. The results were reported using odds ratios (ORs) and confidence intervals (CIs). Model fitting was performed using the PROC SURVEYLOGISTIC procedure and application of weight procedures, cluster, and strata. The data were analyzed and further stratified by sex by using SAS 9.4 (SAS Institute Inc; Cary, North Carolina). Statistical significance was set at P < 0.05.
Ethics statement
The KCDA Institutional Review Board (2018-01-03-P-A) approved the protocols of the research, and data release for the seventh KNHANES (2016–2018). All participants provided written informed consent for collecting data before participating in the survey. This study was conducted in accordance to the guidelines of the Declaration of Helsinki-ethnical principles for medical research involving human subjects.
Results
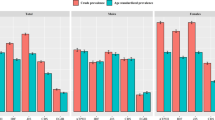
Table 1 shows the general characteristics of the study subjects. There were 2835 male and 4160 female in this study. People at risk of metabolic syndrome comprised 726 (25.6%) male and 517 (12.4%) female. Participants were also grouped into five categories based on the number of lifestyle factors. In the male group, 189 (6.7%) did not have lifestyle risk factors, 786 (27.7%) had one lifestyle risk factor, 1076 (38.0%) had two lifestyle risk factors, 576 (20.3%) had three lifestyle risk factors, and 208 (7.3%) had four or more lifestyle risk factors. In the female group, 522 (12.5%) did not have lifestyle risk factors, 1733 (41.7%) had one lifestyle risk factor, 1465 (35.2%) had two lifestyle risk factors, 393 (9.4%) had three lifestyle risk factors, and 47 (1.1%) had four or more lifestyle risk factors.
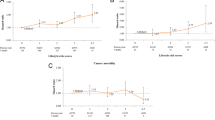
Table 2 displays the findings of the multiple logistic regression analysis stratified by sex of the association between the number of lifestyle risk factors and the risk of metabolic syndrome. Male with over four lifestyle risk factors had a higher OR for metabolic syndrome risk (over four lifestyle factors: OR 1.97, CI 1.18–3.27).Female with more than one lifestyle risk factor had a higher OR for metabolic syndrome risk (one lifestyle factor: OR 1.58, CI 1.10–2.28; two lifestyle factors: OR 2.08, CI 1.39–3.11; three lifestyle factors: OR 1.94, CI 1.20–3.13).
Table 3 shows subgroup analysis findings stratified by dependent variables. Apparently, a higher frequency of poor lifestyle factors was considerably associated with an increased risk of abdominal obesity, hypertension, and elevated triglyceride levels. Especially, triglyceride levels were more likelihood of metabolic syndrome among both male and female. (men: 2 lifestyle factor: OR 1.77, CI 1.18–2.66; 3 lifestyle factors: OR 2.30, CI 1.50–3.52; 4 or more lifestyle factors: OR 3.29, CI 1.99–5.45; women: 2 lifestyle factor: OR 1.98, CI 1.37–2.87; 3 lifestyle factors: OR 2.31, CI 1.50–3.54; 4 or more lifestyle factors: OR 3.62, CI 1.62–8.09).
Table 4 displays logistic regression analysis results stratified by variables of poor lifestyle. People who sat longer is more likelihood of metabolic syndrome among both male and female. (male: Q4 sedentary time: OR 1.63, CI 1.21–2.19; female: Q4 sedentary time: OR 1.85, CI 1.31–2.62).
Discussion
In this study, we found that people who have more poor lifestyle behaviors tended to have an increased risk of metabolic syndrome in the Korean adult population. And the association with metabolic syndrome was more shown in female group than male group. In prior studies, sex difference in lifestyle factor were shown the relationship with metabolic syndrome21,22,23. This sex difference was derived from energy metabolism and difference of physical characteristic. Women have higher proportion of body fat than men and have different effects on hormones24.
In our study, women who had four poor lifestyle factors did not show any significant association because of poor data regarding smoking status. Our study was based on self-reported data. According to some previous studies, validity assessments of self-reported smoking status data among women have revealed discrepancies in self-reported, non-smoker data25. So we think that the value with over four lifestyle risk factors in female is affected to the defect.
The prevalence and trend of metabolic syndrome in Korea vary widely, that is, 5.2–35.3% in the male population and 9.0–39.2% in the female population26. In our study, the prevalence of metabolic syndrome was 25.6% and 12.4% in the male and female groups, respectively. We excluded patients with diagnoses of angina, myocardial infarction, and stroke because baseline cardiovascular diseases and stroke have a strong relationship with the risk of metabolic syndrome and the diagnoses of disease is a great trigger to change people’s lifestyle. Further, people undergoing treatment for hypertension, diabetes mellitus, and hyperlipidemia have been linked to lifestyle behaviors in previous studies, and if we were to include that subgroup in our study, the association between lifestyle and metabolic syndrome would have been underestimated.
People with a greater number of poor lifestyle factors tended to be increased likelihood of abdominal obesity, hypertension and TG. level. Some studies have investigated the combination of metabolic syndrome components23,27,28. For abdominally obese Korean females and males, the most prevalent metabolic syndrome combination is “triglyceride + HDL-cholesterol” and “triglyceride + blood pressure”, respectively27. In the other studies, the combination of abdominal obesity, low HDL and hypertriglyceridemia is significantly different between socioeconomic status and sex in Korea23. The combination is more prevalence in lower SES group and female. In other country, the relationship between abdominal obesity, high TG and reverse HDL-C is observed28. Therefore, components of metabolic syndrome may have different prevalence with regard to external effect.
Several studies have demonstrated that long sedentary time has a negative effect on health outcomes29. Sedentary behavior, generally characterized by a mere lack of physical activity, has also been associated with worse health outcomes, such as obesity, diabetes, insulin resistance, metabolic syndrome, and cardiovascular disease30,31. Some studies have also found alcohol consumption to have a positive relationship with metabolic syndrome. Alcohol intake has been positively associated with body weight, high-density lipoprotein cholesterol levels, and hypertension32. Current smoking was found to affect all components of metabolic syndrome in the male group only. In this study, the proportion of current smokers was 38.6% and 7% in the male and female groups, respectively. Smoking is known to increase insulin resistance and affect lipid metabolism in the body33. Smoking has also been considered to influence adverse abdominal obesity34, and those who quit smoking may exhibit high levels of hyperglycemia and triglycerides35. But in our study, it was not significant, which is that smoking surveyed by self- report is unreliable as mentioned above.
For more effective lifestyle interventions targeting metabolic syndrome, the current study proposes the following recommendations. The initial management of metabolic syndrome entails lifestyle modifications recommended by The National Cholesterol Education Panel Adult Treatment Panel36. First, when formulating a preventive program against metabolic syndrome in adults, we should consider that the effectiveness of the program potentially varies by sex. Second, according to sex, programs should target specific lifestyle risk factors for intervention. When evaluating people’s risks of metabolic syndrome, the number of poor lifestyle behaviors should be taken into account. Third, further research is required to establish reasons underlying sex differences in lifestyle behaviors that affect the risk of metabolic syndrome. Further, an investigation of the associations between the various components of metabolic syndrome and each lifestyle behavior is imperative.
The current study has certain limitations. First, this study was based on data from a cross-sectional study. Therefore, whereas associations could be confirmed, causality could not be evaluated. Second, our study relied on self-reported data. Hence, the measurement of lifestyle risk factors might not have been accurate. Future studies will need to perform precise measurements of lifestyle risk factors. Third, as the cutoff points for lifestyle risk factors were adopted from the KNHANES, it may be difficult to generalize our findings to different settings or populations12. Despite these limitations, this study has several strengths. We used the most recent, nationally representative database to determine the association between lifestyle risk factors and the risk of metabolic syndrome. Therefore, the results obtained are highly representative of healthy South Korean adults. In addition, we utilized American Heart Association/National Heart, Lung, and Blood Institutes Scientific Statement criteria for defining metabolic syndrome in Asians and diagnosing patients with metabolic syndrome.
Conclusion
This study found a significant association between the number of lifestyle risk factors and the risk of metabolic syndrome in Korean adults. The greater the number of lifestyle risk factors, the higher the risk of metabolic syndrome in both sexes. People with a greater number of poor lifestyle behaviors tended to exhibit increased likelihood of abdominal obesity, hypertension, and especially elevated triglyceride levels. Sedentary time was also strongly associated with the risk of metabolic syndrome.
Data availability
The datasets analyzed during the current study are available the KNHANES official website (https://knhanes.kdca.go.kr/knhanes/main.do).
References
Nangaku, M. et al. In a type 2 diabetic nephropathy rat model, the improvement of obesity by a low calorie diet reduces oxidative/carbonyl stress and prevents diabetic nephropathy. Nephrol. Dial. Transplant. 20, 2661–2669 (2005).
Hu, G. et al. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic european men and women. Arch. Intern. Med. 164, 1066–1076 (2004).
Yim, E., Lee, K., Park, I. & Lee, S. The prevalence of metabolic syndrome and health-related behavior changes: The Korea National Health Examination Survey. Healthcare 8, 134 (2020).
Shin, J. I., Oh, J., Kim, H. C., Choi, D. & Yoon, Y.-S. Current State of Cardiovascular Research in Korea. Am. Heart Assoc. 1, 1 (2019).
Lee, S. W., Kim, H. C., Lee, H. S. & Suh, I. Thirty-year trends in mortality from cerebrovascular diseases in Korea. Kor. Circ. J. 46, 507–514 (2016).
Saklayen, M. G. The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 20, 12 (2018).
Takahara, M. & Shimomura, I. Metabolic syndrome and lifestyle modification. Rev. Endocr. Metab. Disord. 15, 317–327 (2014).
Stone, N. J. & Saxon, D. Approach to treatment of the patient with metabolic syndrome: lifestyle therapy. Am. J. Cardiol. 96, 15–21 (2005).
Mokdad, A. H., Marks, J. S., Stroup, D. F. & Gerberding, J. L. Actual causes of death in the United States, 2000. JAMA 291, 1238–1245 (2004).
Kim, J., Chu, S.-K., Kim, K. & Moon, J.-R. Alcohol use behaviors and risk of metabolic syndrome in South Korean middle-aged men. BMC Public Health 11, 1–8 (2011).
Oh, S. W. Obesity and metabolic syndrome in Korea. Diabetes Metab. J. 35, 561 (2011).
Poortinga, W. The prevalence and clustering of four major lifestyle risk factors in an English adult population. Prev. Med. 44, 124–128 (2007).
Hall, M. H. et al. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep 31, 635–643 (2008).
Villegas, R., Creagh, D., Hinchion, R., O’Halloran, D. & Perry, I. J. Prevalence and lifestyle determinants of the metabolic syndrome. Ir. Med. J. 97, 300–303 (2004).
Kwaśniewska, M., Kaleta, D., Dziankowska-Zaborszczyk, E. & Drygas, W. Healthy behaviours, lifestyle patterns and sociodemographic determinants of the metabolic syndrome. Cent. Eur. J. Public Health 17, 14–19 (2009).
Kweon, S. et al. Data Resource Profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 43, 69–77 (2014).
Lakerveld J. The relation between sleep duration and sedentary behaviours in European adults. Obesity reviews 2016;v. 17 Suppl S1:pp. 62–7–2016 v.17 Suppl S1.
rhan Go. 2020 Diatary reference intakes for Koreans: Energy and Macronutrients. Sejong: Ministy of Health and Welfare, the Korean Nutrition Society (2020).
Zhu, S., St-Onge, M.-P., Heshka, S. & Heymsfield, S. B. Lifestyle behaviors associated with lower risk of having the metabolic syndrome. Metabolism 53, 1503–1511 (2004).
Grundy Scott, M. et al. Diagnosis and management of the metabolic syndrome. Circulation 112, 2735–2752 (2005).
Monterrosa, A. E., Haffner, S. M., Stern, M. P. & Hazuda, H. P. Sex difference in lifestyle factors predictive of diabetes in Mexican-Americans. Diabetes Care 18, 448–456 (1995).
Chang, S. H., Chang, Y. Y. & Wu, L. Y. Gender differences in lifestyle and risk factors of metabolic syndrome: Do women have better health habits than men?. J. Clin. Nurs. 28, 2225–2234 (2019).
Lim, H., Nguyen, T., Choue, R. & Wang, Y. Sociodemographic disparities in the composition of metabolic syndrome components among adults in South Korea. Diabetes Care 35, 2028–2035 (2012).
Wu, B. N. & O’Sullivan, A. J. Sex differences in energy metabolism need to be considered with lifestyle modifications in humans. J. Nutr. Metab. 2011, 391809 (2011).
Kang, H. G. et al. Biochemically-verified smoking rate trends and factors associated with inaccurate self-reporting of smoking habits in Korean women. Asian Pac. J. Cancer Prev. 14, 6807–6812 (2013).
Kim, H. C. & Kim, D. J. Causes of different estimates of the prevalence of metabolic syndrome in Korea. Korean J. Intern. Med. 26, 440–448 (2011).
Lee, C. M. Y. et al. The metabolic syndrome identifies a heterogeneous group of metabolic component combinations in the Asia-Pacific region. Diabetes Res. Clin. Pract. 81, 377–380 (2008).
Azimi-Nezhad, M. et al. High prevalence of metabolic syndrome in Iran in comparison with France: What are the components that explain this?. Metab. Syndr. Relat. Disord. 10, 181–188 (2012).
Edwardson, C. L. et al. Association of sedentary behaviour with metabolic syndrome: A meta-analysis. PLoS ONE 7, e34916 (2012).
Biswas, A. et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Intern. Med. 162, 123–132 (2015).
Kim, K. S. et al. Association of self-reported sedentary time with insulin resistance among Korean adults without diabetes mellitus: A cross-sectional study. BMC Public Health 18, 1335 (2018).
Athyros, V. G. et al. Association of drinking pattern and alcohol beverage type with the prevalence of metabolic syndrome, diabetes, coronary heart disease, stroke, and peripheral arterial disease in a mediterranean cohort. Angiology 58, 689–697 (2007).
Balhara, Y. P. S. Tobacco and metabolic syndrome. Indian J. Endocrinol. Metab. 16, 81–87 (2012).
Canoy, D. et al. Cigarette smoking and fat distribution in 21,828 British men and women: A population-based study. Obes. Res. 13, 1466–1475 (2005).
Youn, J. A., Lee, Y. H. & Noh, M. S. Relationship between smoking duration and metabolic syndrome in Korean Former Smokers. J. Kor. Soc. Res. Nicotine Tobacco 9, 18–25 (2018).
Grundy, S. M. et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112, 2735–2752 (2005).
Author information
Authors and Affiliations
Contributions
P.Y.S. and K.S.H. designed the study conducted the statistical analyses. P.Y.S. wrote the main manuscript text. All authors prepared the tables and reviewed the manuscript. The text was reviewed by J.S.I. and P.E.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, Y.S., Kang, S.H., Jang, SI. et al. Association between lifestyle factors and the risk of metabolic syndrome in the South Korea. Sci Rep 12, 13356 (2022). https://doi.org/10.1038/s41598-022-17361-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17361-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.