Abstract
Less than half of patients with chronic diseases, including multiple sclerosis (MS), adhere to their prescribed medications. Treatment selection is essential for patient adherence. The aim of this study was to explore the potential factors influencing nonadherence to disease-modifying therapies (DMTs) in MS. This prospective, cross-sectional study was performed at the Multiple Sclerosis Center between 2018 and 2021. In total, 85 patients were eligible for final analysis. Forty-one patient (48.2%) with MS were non-adherent to DMT. Male sex, oral administration of drugs, and longer treatment duration were associated with nonadherence. The mean Expanded Disability Status Scale score did not differ between the adherent and non-adherent patients (p > 0.05). Patients with a higher score on the Symbol Digit Modalities Test, who were receiving self-injection therapy, had shorter treatment duration, and higher disability, were more likely to be adherent to DMT than those without. To minimize nonadherence in patients with MS, the patient’s information processing speed should be considered before DMT initiation, and appropriate treatment options should be discussed.
Similar content being viewed by others
Introduction
Treatment options for multiple sclerosis (MS) have greatly expanded recently1,2. Improving disease stability and quality of life in patients with chronic diseases requires prolonged and often lifelong medication. Less than half of patients with chronic diseases and MS adhere to their prescribed medications, which precludes the full benefit of treatment, worsens disease outcomes, and accelerates disease progression3,4,5. MS is one of the diseases that, despite the coming of new and short treatment options1,2, still requires frequent parenteral or oral administration of disease-modifying therapy (DMT) daily or a few times a week for an undefined extended period.
Poor adherence to treatment in MS reduces the clinical effectiveness of therapy, which can adversely impact disease progression, MS-related hospitalization, and quality of life6,7. Hence, treatment selection is essential for patient adherence. Some factors should be considered when making a treatment decision for patients with MS–not only efficacy and safety issues should be considered, but also the route of administration, dosing frequency, patient lifestyle factors, and willingness should be evaluated before DMT administration8.
Although there is a need to improve the adherence rate in patients with MS, it is equally important to investigate the relationship between adherence and prognostic factors. Nonadherence to DMT is believed to be caused by numerous factors9,10,11, including perceived lack of efficacy, adverse drug effects, and simply forgetting to inject oneself3,9,10,11. Cognitive impairment has also been associated with nonadherence12,13. At least 70% of patients with MS experience mild-to-severe cognitive impairment, most commonly in information processing speed, executive functioning, and visual and verbal memory14,15,16. Despite the cognitive impairment and nonadherence evidence11,12,13, the literature on MS adherence rates lacks recommendations regarding cognitive assessment.
Some studies have shown the relationship between cognitive impairment and nonadherence to DMT for MS12,13; however, all of them have failed to examine which cognitive assessment should be performed and how to select potential non-adherent patients based on cognitive assessment before DMT administration. Identifying patient groups that are more likely to be adherent and determining the explanatory factors are essential to designing targeted management strategies, as poor adherence is associated with increased risk of morbidity and mortality3,4,7. This study aimed to explore the potential factors influencing nonadherence to DMTs for MS.
Results
Patient characteristics
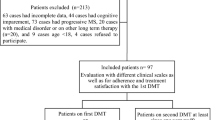
Ninety-eight patients were included in this study. Data regarding adherence to DMT and cognitive assessment were available for 85 patients (Fig. 1). Patients’ demographic and clinical characteristics are shown in Table 1.
Among the injectable DMTs (n = 54), 22.2% of patients were prescribed glatiramer acetate, 14.8% interferon (IFN)-β-1a intramuscularly, 46.3% IFNβ-1a subcutaneously, 13.0% IFNβ-1b, and 3.7% pegylated form of IFNβ-1a. Among the oral DMTs (n = 31), dimethyl fumarate was prescribed in 41.9% of patients, fingolimod in 38.7%, and teriflunomide in 19.4%.
Relationship between demographic, disease characteristics, and adherence to DMT
According to the study data of 85 patients with MS who were taking an injectable or oral DMT, the proportion of days covered (PDC) was < 80 in 41 (48.2%) patients. The adherence range was the same in patients up to 45 and older than 45 years of age (p > 0.05). The nonadherence rate was significantly higher in men than in women (p < 0.05). No differences in adherence rates were detected according to disease duration, education level, and professional activity (all, p > 0.05). Oral administration showed a greater lack of adherence, also longer treatment duration (> 12 months) p < 0.05). Non-adherent patients were associated with an increased frequency of relapse in the post-index 12-month period (p < 0.05) (Table 2).
Neurological disability, cognitive impairment, and adherence to DMT
The mean Expanded Disability Status Scale (EDSS) score did not differ between the adherent and non-adherent patients (p > 0.05). The scores of information processing speed and visuospatial memory were significantly lower in non-adherent patients than in adherent patients (p < 0.05), whereas the scores for verbal learning did not differ between the groups (p > 0.05) (Table 3).
Factors predicting medication adherence in patients with MS
Patient characteristics (sex, age, and education level), disease characteristics (disease duration and treatment duration), form of drug administration (injectable or oral), and scores of the Symbol Digit Modalities Test (SDMT) or Brief Visuospatial Memory Test–Revised (BVMT-R), or California Verbal Learning Test, Second Edition (CVLT-II) were included in the binary logistic regression analysis as independent variables. Dependent binary variables in the models were adherence (PDC ≥ 0.8) or nonadherence (PDC < 0.8). Table 4 shows the results of the binary logistic regression analysis, which identified significant factors that predict nonadherence to DMT in patients with MS.
Patients with a higher SDMT score, self-injection therapy, shorter treatment duration, and higher disability were more likely to be adherent to DMT.
Discussion
In this study, overall adherence to DMT was low, with approximately 48% of patients not meeting the adherence criteria (PDC ≥ 0.8). The rate of adherence (52%) at 12 months was lower than that (60–77%) reported by other authors17,18,19, who applied the PDC criteria to larger samples. The disparate findings may have been due to differences between study populations (in other studies, investigators included patients with disability claims or patients before and after the first DMT claim date) or the DMTs analyzed17,18. Adherence rates vary among studies according to study sample and methods11,13,17,18, and it is apparent that adherence remains suboptimal in patients with MS initiating DMTs, and measures to improve adherence are warranted.
This study found several associations between patient characteristics and DMT adherence. Compliance and adherence levels to DMT were lower in men with MS than in women with MS. Other studies have provided mixed evidence regarding the difference in adherence between sexes5,19,20. Although MS is more prevalent in women than in men, it is important to focus on patient-centered care that can be used by health care practitioners to aid in enhancing adherence to DMT in men.
In the present study, oral DMT administration, a lower EDSS score, and longer treatment duration were associated with a greater lack of adherence. Many studies have compared adherence by type of DMT5,19,21,22. There is no consensus on which DMT patients have a higher compliance with: some studies have shown that patients using self-injected therapy, predominantly IFNβ, are more adherent than those not using such therapy5,19, other studies have indicated that patients using oral therapy, predominantly fingolimod, are more adherent than those not using such therapy21,22. Likewise, a study assessed three oral and five self-injected DMTs and found that the route of administration was not a significant predictor of nonadherence23. Given the equivocal evidence of the studies5,19,21,22,23, the difference in adherence between injectable and oral DMT remains unclear. In many studies, treatment adherence was found to be related to the duration of the treatment and neurological disability24,25. Similarly, in our study, patients with a longer treatment duration and lower EDSS score were also non-adherent to DMT.
Patients adherent to DMT (PDC > 80) in our study had a significantly decreased likelihood of relapse. The observed association between nonadherence and a higher probability of severe relapse (p < 0.05) coincides with the evidence demonstrated in other studies that nonadherence is a significant predictor of relapse7,18,26,27,28. Therefore, clues that promote adherence may improve the overall outcomes for patients with MS receiving DMT by reducing the frequency of relapses and disease progression.
Cognitive impairment in patients with MS as an important indicator of safe medication use should be assessed in patients with MS. The Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS) was selected for cognition assessment in our study, as the BICAMS was recognized as a short, highly sensitive, and easily administered battery for patients with MS29,30. We found an association between a lower score of information processing speed and PDC < 80. There are no published data about adherence and the SDMT score, so this study is the first to examine the relationship between information processing speed and DMT adherence. The SDMT assessment, which is a quick and effective assessment of cognition29,30 can be performed before DMT initiation and can help improve adherence to DMT. The patients with impaired information processing speed on the oral or injectable DMT should be closer monitored during routine visits. Some studies have shown that patient support programs have a positive impact on adherence to DMT independent of the treatment duration on DMT31,32. It is important that the majority of patients also believe in this positive effect31. E-pills or e-injection medication devices (e.g., timers or alarm watches) also can help improve medication compliance in these patients32. After all efforts are taken, if the patient still remains non-adherent, other treatment options should be considered.
The present study has several limitations. First, cognition was only tested with the BICAMS, so other cognitive domains were not assessed. However, most cognitive tests, despite their sensitivity to MS, are time consuming and not routinely used in clinical settings. The aim of this study was to estimate and assess the impact of a cognitive tool that is readily available in most countries. Second, fatigue and depression, which are common comorbid conditions that have a great impact on cognition, were not assessed in the study. However, patients with severe fatigue and depression were excluded from the study.
Conclusions
Patients with a higher SDMT score or who were receiving self-injection therapy, or had a shorter treatment duration, or higher disability were more likely to be adherent to DMT. Improving patients’ adherence level requires not only decision-making between patients and physicians and addressing side-effect profiles of medications, but it also requires cognition assessment before DMT administration. To minimize nonadherence in patients with MS, the patient’s information processing speed should be considered before DMT initiation, and appropriate treatment options should be discussed.
Methods
Study design and population
This prospective, cross-sectional study was performed at the Multiple Sclerosis Center of Vilnius University Hospital Santaros Klinikos, Lithuania. Patients were enrolled and assessed between 2018 and 2021.
A total of 98 patients were enrolled in this study. All patients had relapsing MS and were on DMT (injectable or oral therapy).
Inclusion criteria for all patients were as follows:
-
Male or female patients older than 18 years of age;
-
Patients diagnosed with MS according to the McDonald criteria33,34;
-
Patients with a relapsing disease course;
-
Patients receiving the same DMT at least 6 months before enrollment;
-
Patients who had not used any cognition-influencing medication (e.g., antidepressants, neuroleptics, and anticholinergic drugs) at least 3 months prior to enrollment and during the study;
-
Patients with no MS relapse or relapse treatment at least 3 months before enrollment and cognitive assessment; and
-
Patients with MS who were fluent Lithuanian speakers.
Exclusion criteria for all patients were as follows:
-
Patients with any neurologic or psychiatric disorders that could affect cognitive functions;
-
Patients with a history of clinically significant central nervous system disease (e.g., stroke, traumatic brain, or spinal injury) or neurological disorders that could mimic MS;
-
Patients with moderate or severe fatigue, anxiety, and/or depression; and
-
Patients with neurological signs that could interfere with cognitive performance (e.g., optic neuritis, upper dominant extremity weakness, or severe ataxia).
Neurological and cognitive assessment
The neurological assessment was performed in all participants, and neurological disability was assessed using the EDSS. The BICAMS was used for cognitive assessment29,30, which was performed by the same person in the same sequence:
-
SDMT;
-
BVMT-R, first three recall trials; and
-
CVLT-II, first five trials. The Lithuanian version of the CVLT-II was used for assessment35,36.
DMT and adherence
Eight different DMTs were identified and categorized into two groups: self-injected and oral. Self-injected therapies included IFNβ (Betaferon, Rebif, Avonex and Plegridy) and glatiramer acetate (Copaxone). Oral therapies included fingolimod, teriflunomide, and dimethyl fumarate.
Adherence was measured using pills or injections counts, which were combined into PDC. PDC was calculated for all patients as the sum of days during the follow-up period that were covered by pills or injections, divided by the number of days in the follow-up period (365 days)37. Values for PDC ranged from 0 to 100% with higher values indicating higher adherence and “100%” indicating a patient who had complete DMT adherence. The percentages of patients with adherence levels of < 80% were considered as non-adherent and > 80% as adherent.
Statistical analysis
Descriptive statistics are presented as mean (m) and standard deviation. The Student t-test was used to compare means of the same variables between the two groups when the data distribution was normal. Categorical variables are expressed as absolute number and percentage. Categorical variables were analyzed using the chi-square test. To assess the normality of the distribution of quantitative variables, the Shapiro–Wilk test was used. In the regression analyses, adherence was modeled as a binary variable, with PDC ≥ 0.8 representing adherence and PDC < 0.8 indicating nonadherence. Explanatory variables (covariates) included age, sex, education level, disease duration, treatment duration, self-injectable or oral therapy, disability, SDMT score, or BVMT-R score, or CVLT-II score.
Data were analyzed using the statistical software package SPSS (version 23.0 for Windows, IBM Corp.) The level of statistical significance was set at p < 0.05.
Ethics statements
The Lithuanian Bioethics Committee approved the study (date: January 27, 2011; number [no.]: L-12–01/2), and the Lithuanian Bioethics Committee granted permission to continue the study (date: February 22, 2018; no.: 6B-18–41). All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from all the participants prior to study inclusion.
References
Tintore, M., Vidal-Jordana, A. & Sastre-Garriga, J. Treatment of multiple sclerosis - success from bench to bedside. Nat. Rev. Neurol. 15, 53–58 (2019).
Li, H. et al. Comparative efficacy and acceptability of disease-modifying therapies in patients with relapsing-remitting multiple sclerosis: a systematic review and network meta-analysis. J. Neurol. 267(12), 3489–3498 (2020).
Treadaway, K. et al. Factors that influence adherence with disease-modifying therapy in MS. J. Neurol. 256, 568–576 (2009).
Lafata, J. E. et al. Measuring adherence and persistence to disease-modifying agents among patients with relapsing remitting multiple sclerosis. J. Am. Pharm. Assoc. 48, 752–757 (2008).
Devonshire, V., Lapierre, Y., Macdonell, R., et al.; GAP Study Group. The Global Adherence Project (GAP): a multicenter observational study on adherence to disease-modifying therapies in patients with relapsing-remitting multiple sclerosis. Eur. J. Neurol. 2011;18:69–77.
Osterberg, L. & Blaschke, T. Adherence to medication. N. Engl. J. Med. 353, 487–497 (2005).
Tan, H. et al. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv. Ther. 28, 51–61 (2011).
Happe, L. E. Choosing the best treatment for multiple sclerosis: comparative effectiveness, safety, and other factors involved in disease-modifying therapy choice. Am. J. Manag. Care 19(17 Suppl), S332–S342 (2013).
McKay, K.A., Tremlett, H., Patten, S.B., et al.; for the CIHR Team in the Epidemiology and Impact of Comorbidity on Multiple Sclerosis (ECoMS). Determinants of non-adherence to disease-modifying therapies in multiple sclerosis: a cross-Canada prospective study. Mult. Scler, 2017; 23(4): 588–596.
Tremlett, H. et al. Adherence to the immunomodulatory drugs for multiple sclerosis: Contrasting factors affect stopping drug and missing doses. Pharmacoepidemiol Drug Saf. 17, 565–576 (2008).
Rio, J. et al. Factors related with treatment adherence to interferon beta and glatiramer acetate therapy in multiple sclerosis. Mult. Scler J. 11, 306–309 (2005).
Bruce, J. M., Hancock, L. M. & Arnett, P. Treatment adherence in multiple sclerosis: Association with emotional status, personality, and cognition. J. Behav. Med. 33, 219–227 (2010).
Menzin, J., Caon, C. & Nichols, C. Narrative review of the literature on adherence to disease-modifying therapies among patients with multiple sclerosis. J. Manag. Care Pharm. 19, 24–40 (2013).
Amato, M. P. et al. Cognitive dysfunction in early-onset multiple sclerosis: a reappraisal after 10 years. Arch. Neurol. 58(10), 1602–1606 (2001).
Langdon, D. W. Cognition in multiple sclerosis. Curr. Opin. Neurol. 24(3), 244–249 (2011).
Julian, L. J. et al. Employment in multiple sclerosis. Exiting and re-entering the work force. J. Neurol. 255(9), 1354–1360 (2008).
Yermakov, S. et al. Impact of increasing adherence to disease-modifying therapies on healthcare resource utilization and direct medical and indirect work loss costs for patients with multiple sclerosis. J. Med. Econ. 18(9), 711–720 (2015).
Burks, J., Marshall, T. S. & Ye, X. Adherence to disease-modifying therapies and its impact on relapse, health resource utilization, and costs among patients with multiple sclerosis. Clinicoecon. Outcomes Res. 9, 251–260 (2017).
Halpern, R. et al. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence 5, 73–84 (2011).
Higuera, L., Carlin, C. S. & Anderson, S. Adherence to disease-modifying therapies for multiple sclerosis. J. Manag. Care Spec. Pharm. 22(12), 1394–1401 (2016).
Agashivala, N. et al. Compliance to fingolimod and other disease modifying treatments in multiple sclerosis patients, a retrospective cohort study. BMC Neurol. 13, 138 (2013).
Bergvall, N. et al. Persistence with and adherence to fingolimod compared with other disease-modifying therapies for the treatment of multiple sclerosis: a retrospective US claims database analysis. J. Med. Econ. 17(10), 696–707 (2014).
Munsell, M. et al. An assessment of adherence among multiple sclerosis patients newly initiating treatment with a self-injectable versus oral disease-modifying drug. Neurology 84(14), 3 (2015).
Arroyo, E., Grau, C., Ramo-Tello, C., et al.; GAP Study Group. Adherence to disease-modifying therapies in spanish patients with relapsing multiple sclerosis: two-year interim results of the global adherence project. Eur. Neurol., 2011; 65:59–67.
Koskderelioglu, A. et al. Evaluation of the adherence to immunmodulatory treatment in patients with multiple sclerosis. Noro Psikiyatr Ars 52(4), 376–379 (2015).
Steinberg, S. C. et al. Impact of adherence to interferons in the treatment of multiple sclerosis: a non-experimental, retrospective, cohort study. Clin. Drug Investig. 30(2), 89–100 (2010).
Oleen-Burkey, M. et al. The relationship between alternative medication possession ratio thresholds and outcomes: evidence from the use of glatiramer acetate. J. Med. Econ. 14(6), 739–747 (2011).
Cohen, B. A. et al. Therapy optimization in multiple sclerosis: a cohort study of therapy adherence and risk of relapse. Mult. Scler. Relat. Disord. 4(1), 75–82 (2015).
Langdon, D. W. et al. Recommendations for a brief international cognitive assessment for multiple sclerosis (BICAMS). Mult. Scler. 18(6), 891–898 (2012).
Benedict, R. H. B. et al. Brief international cognitive assessment for MS (BICAMS): international standards for validation. BMC Neurol. 16(12), 55 (2012).
Lenz, F. & Harms, L. The impact of patient support programs on adherence to disease-modifying therapies of patients with relapsing-remitting multiple sclerosis in Germany: a non-interventional, prospective study. Adv. Ther. 37(6), 2999–3009 (2020).
Mason, M. et al. Technologies for medication adherence monitoring and technology assessment criteria: narrative review. JMIR Mhealth Uhealth. 10(3), e35157 (2022).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald criteria”. Ann. Neurol. 58(6), 840–846 (2005).
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17(2), 162–173 (2018).
Giedraitiene, N., Kizlaitiene, R. & Kaubrys, G. The BICAMS battery for assessment of lithuanian-speaking multiple sclerosis patients: relationship with age, education, disease disability, and duration. Med. Sci. Monit. 21, 3853–3859 (2015).
Giedraitiene, N., Kaubrys, G. & Kizlaitiene, R. Cognition during and after multiple sclerosis relapse as assessed with the brief international cognitive assessment for multiple sclerosis. Sci. Rep. 8(1), 8169 (2018).
Raebel, M. A. et al. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med. Care 51(8 Suppl 3), S11-21 (2013).
Author information
Authors and Affiliations
Contributions
N.G. contributed to the conception and design of the study, acquisition of data, analysis and interpretation of the data, and drafting of the manuscript. V.T. contributed to the acquisition of the data, analysis and interpretation of the data, conception and design of the study, and revision of the manuscript. G.K. conceived and designed the study, analyzed and interpreted the data, and drafted the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giedraitiene, N., Taluntiene, V. & Kaubrys, G. Relationship between cognition and treatment adherence to disease-modifying therapy in multiple sclerosis: a prospective, cross-sectional study. Sci Rep 12, 12447 (2022). https://doi.org/10.1038/s41598-022-16790-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16790-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.