Abstract
Increased physical activity is required in patients with stroke that are hospitalized in the rehabilitation unit. This study investigated the association between the daily number of steps and walking independence in order to determine the cutoff value of daily number of steps that can predict walking independence in hospitalized patients with sub-acute stroke. This cross-sectional observational study included 85 stroke patients admitted to the rehabilitation unit. The average daily number of steps was measured using Fitbit One for 4 days starting at 30 days after stroke onset. 6-min walk test, and Fugl-Meyer assessment of the lower extremities were measured The category of walking independence was classified using the Functional Ambulation Category (FAC). The subjects were divided into two groups according to the FAC score: a walking independence group (FAC ≥ 4) and a walking non-independence group (FAC ≤ 3). Logistic regression analysis was conducted to investigate the association of daily number of steps with walking independence and a receiver operating characteristic curve was used to identify the cutoff value of daily number of steps for predicting walking independence. The daily number of steps (per 1000 steps) was independently associated with walking independence (odds ratio (OR); 2.53, 95% confidence interval (CI); 1.40–5.73, p = 0.009). The cutoff value of daily number of steps for predicting independent walking was 4286 steps (area under the curve = 0.914, sensitivity of 0.731, and specificity of 0.949). The daily number of steps was associated with independent walking in hospitalized patients with sub-acute stroke. The daily number of steps may be a useful target in rehabilitation for patients with sub-acute stroke.
Similar content being viewed by others
Introduction
Physical activity is important for promoting functional recovery and secondary stroke prevention1; however, a previous study found that insufficient physical activity was higher in individuals with stroke than those without stroke2. Moreover, most of the patient’s day was spent inactive (median 48.1%), alone (median 53.7%), and in their bedroom (median 56.5%) in hospitalized stroke patients3. In a rehabilitation unit, hospitalized sub-acute stroke patients took fewer steps than chronic home-living stroke patients4. Light intensity physical activity was associated with improved walking independence5 and physical activity time was associated with activities of daily living (ADL) score6 in rehabilitation unit stroke patients. Hence, increasing the physical activity might be required in patients with stroke hospitalized in the rehabilitation unit.
Improved walking ability is a rehabilitation goal for stroke patients hospitalized in the rehabilitation unit7. Previous studies showed that walking independence was positively associated with the amount of physical activity in patients with stroke hospitalized in the rehabilitation unit, however, they either have a small sample size or did not adjust fully5,8. Additionally, similar physical activity patterns were observed in moderate and severe stroke patients but was different in patients with mild stroke8. As intensity-based physical activity was non-linear due to walking ability in patients with stroke hospitalized in the rehabilitation unit9, there may be a threshold in step count which, if attained, is associated with the greatest increase in walking independence. Knowing these values of physical activity for predicting walking independence may be useful; however, to the best of our knowledge, this has not yet been investigated.
The objective of this study was to investigate the association of daily number of steps with walking independence and to identify the cutoff value of daily number of steps for predicting walking independence in patients with sub-acute stroke admitted to the rehabilitation unit.
Methods
Study design and subjects
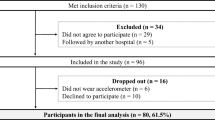
In this cross-sectional study, the part of the data set from the previous study was used10, because the daily number of steps were measured from October 2017. Consecutive stroke patients were admitted to the rehabilitation unit at Itami Kousei Neurosurgical Hospital between October 2017 and September 2019. Eligibility criteria were those who were admitted to the rehabilitation unit within 30 days from stroke onset, could walk alone, or could walk with an intermittent or continuous light touch to assist balance or coordination (Functional Ambulation Category [FAC] ≥ 2). Exclusion criteria were as follows: pre-stroke modified Rankin Scale (mRS) score > 2; patients with subarachnoid hemorrhage; a history of severe diseases such as musculoskeletal disease, cardiopulmonary disease, other brain injuries, Parkinson’s disease, and gastrointestinal disease that the physician considered to have affected the ability to walk; or inability to provide consent due to loss of consciousness, aphasia, dementia, or non-cooperation (Fig. 1). All patients underwent 40–60 min sessions of supervised rehabilitation such as physical therapy, occupational therapy, and speech-language-hearing therapy 2–3 times a day, 7 times a week. This study was approved by the Konan Women’s University Research Committee (acknowledgment number: 2015020) and was in accordance with the Declaration of Helsinki. All participants provided informed consent. All research was performed in accordance with relevant guidelines or regulations.
Patient demographics and clinical characteristics
Age, sex, height, weight, stroke type (cerebral infarction or intracerebral hemorrhage), disease history, and pre-stroke mRS were recorded upon admission and discharge from the rehabilitation unit. Body mass index (BMI) was calculated by dividing the body weight by the height squared (kg/m2). Stroke severity using the National Institutes of Health Stroke Scale (NIHSS) was assessed at 30 days from stroke onset.
Outcome measurement
Physical activity
Physical activity was measured from thirty days after stroke onset. All patients wore the Fitbit One (Fitbit. Inc., San Francisco, CA, USA) on their non-paretic ankle11,12 for six days continuously except when bathing and sleeping. Fitbit One has good test–retest reliability across 3 days of free-living activity in stroke survivors13. Thus, the average daily number of steps taken during the middle 4-day period of the 6 days was used as the value of daily physical activity. Fitbit One is a three-dimensional accelerometer that calculates steps taken, floors climbed, distance traveled, and sleep quality. It has been used for stroke patients with demonstrated accuracy12. Patients were instructed to wear Fitbit One immediately after waking and remove it while bathing and before going to bed. They were instructed to continue with their activities of daily living without the need for excessive exercise, and they did not receive any feedback from the physical therapist. The number of steps was extracted by downloading the data files to Fitbit online dashboard software14. Each patient’s setup parameters, such as age, sex, height, and weight were fed in the device software to ascertain the outcome.
FAC
Patients were classified by category of walking independence using FAC15 at 30 days after stroke onset and discharge from the rehabilitation unit by a physical therapist. The FAC has excellent reliability, good concurrent and predictive validity, and good responsiveness in patients with hemiparesis after stroke16. It has six levels (0 to 5) that are classified according to the walking ability based on the amount of physical support required as follows: nonfunctional ambulatory (FAC 0); ambulatory [level II], continuous manual contact to support the body weight and maintain balance or to assist with coordination (FAC 1); ambulatory [level I], intermittent or continuous light touch to assist with balance or coordination (FAC 2); ambulatory, dependent on supervision (FAC 3); ambulatory, independent, level surface only (FAC 4); and ambulatory, independent (FAC 5).
Fugl-Meyer assessment of the lower extremities
Lower extremity motor impairment following stroke was assessed using the lower limb Fugl-Meyer assessment (FMA)17 at 30 days after stroke onset. The lower limb FMA score ranges from 0 (hemiplegia) to a maximum of 34 points. Seventeen items are included in the lower limb FMA and each item is scored on a 3-point ordinal scale (0 = cannot perform, 1 = performs partially, and 2 = performs fully). The lower limb FMA is best administered by a trained physical therapist.
Six-minute walk test
The 6MWT was used to evaluate the walking endurance at 30 days after stroke onset. A 30-m indoor walkway was used to conduct the test according to the ATS guidelines18. Patients were then instructed to walk from the starting line to the end of the walkway as many times as possible in 6 min. Patients were allowed to use their usual assistive devices and intermittent assistance for fall prevention was provided as necessary. During the test, patients were permitted to slow down, stop, and rest by leaning against the wall as necessary, but they resumed walking as soon as possible. Feedback was given and the distance covered at the end of the 6MWT was recorded.
Statistical analysis
Descriptive statistics are presented as numbers (percentages) and median (interquartile range [IQR]) in all subjects. Shapiro–Wilk test was performed to check for normality. To investigate the difference between the daily number of steps and walking ability measured by FAC, the Kruskal–Wallis test was used when normality was not confirmed for continuous and ordinal variables following previous studies. When a statistically significant effect was found, the Steel–Dwass test was used as a multiple comparison to determine the difference between the daily number of steps and FAC in all subjects and by sex. Then, the subjects were divided into two groups according to the FAC score: a walking independence group (FAC ≥ 4) and a walking non-independence group (FAC ≤ 3). Logistic regression analysis was also performed to investigate the association of the daily number of steps (in increments of 1,000 steps) with walking independence adjusted by age, sex, stroke type (cerebral infarction or intracerebral hemorrhage), NIHSS, lower extremity FMA, and 6MWT following previous studies19,20. Multicollinearity was assessed using the variance inflation factor (VIF) and defined as VIF ≥ 1021. The receiver operating characteristic (ROC) curve analysis was conducted to establish the cutoff value of daily number of steps for predicting walking independence in all subjects. The area under the curve, sensitivity, and specificity were calculated to determine the optimal cutoff point. The optimal cutoff was determined using the Youden index, which was defined as the maximum vertical distance between the ROC curve and the diagonal or chance line, and was calculated as the maximum sum of sensitivity and specificity minus one22. Significance was set at < 0.05; all analyses were performed using JMP version 10.0 software (SAS Institute Japan, Tokyo, Japan).
Results
Patient demographics and clinical characteristics are presented in Table 1. A total of 233 patients with stroke were hospitalized during the study inclusion period. Of these patients, 148 were excluded from the study, and 85 met the inclusion criteria and were enrolled in the study. Normality of the daily number of steps could not be confirmed, the Kruskal–Wallis test and the Steel–Dwass test was used to investigate the differences among FAC. The median daily number of steps was 3,642 steps (IQR, 4,052 steps/day), 3,115.5 (IQR, 3,364.7 steps/day), and 4,286 (IQR, 4,213.5 steps/day) in all subjects, female and male, respectively (Table 2). There were significant interaction effects between the daily number of steps and FAC in all subjects (p < 0.001) (Table 2, Fig. 2).
The logistic regression analysis demonstrated that walking independence was only associated with the daily number of steps (odds ratio, 2.53; 95% confidence interval, 1.40–5.73; p = 0.009) (Table 3).
Based on the ROC curve, the cutoff value of daily number of steps for predicting walking independence was 4286 steps (p < 0.005, area under the curve = 0.914, sensitivity of 0.731, and specificity of 0.949) (Fig. 3).
Discussion
We demonstrated that the daily number of steps was associated with walking independence after adjusting for confounding factors such as age, sex, stroke type, NIHSS, lower extremity FMA, and 6MWT. Previous studies found that increasing day-time physical activity was related to walking independence in patients with sub-acute stroke who could not walk alone5, and gait independence increased the median percentage of time spent standing/walking8 by stroke patients in the rehabilitation unit, which partially support our results. Further studies with longitudinal designs are required to clarify the causal relationship between the daily number of steps and walking independence in stroke patients.
The cutoff value of the daily number of steps for predicting walking independence was 4,286 steps in patients with sub-acute stroke hospitalized in the rehabilitation unit. To our knowledge, the cutoff value of the number of steps for predicting walking independence has not been investigated. In a previous study, the cutoff value of 6MWT for determining walking independence was 304 m10 and the cutoff value of lower extremity FMA for predicting walking independence was 22.5 points23. As improving the walking ability is one of the goals of rehabilitation7, combining the cutoff value of the number of steps in our results with that of other motor performance tests may be useful to facilitate early walking independence. The results of this study suggest that for every 1,000 steps per day increase in the patient’s step count, the odds of becoming an independent ambulator increased between 1.398 and 5.734. Meanwhile, the sensitivity and specificity were 0.731 and 0.949, respectively in the present study; there were non-independent walking patients who achieved 4286 steps. Thus, for non-independent patients who achieved 4286 steps, it may be necessary to consider other factors, such as cognitive function24.
The daily number of steps was 4935 to 5291 in patients with mild stroke (NIHSS score 1 to 2)25 and 1514.3 to 3010.7 in patients with moderate stroke (FAC 3; range 2–5)4. Day-time physical activity differed according to severity measured by NIHSS in patients with acute stroke26. These results are partly consistent with our study findings that the number of steps decreases with increasing disability after stroke.
The number of steps in the walking independence group was 4518.5 steps/day (IQR, 3559.5 steps/day) for FAC 4 and 6763.5 steps/day (IQR, 5082.2 steps/day) for FAC 5. It was previously reported that 6025 steps per day is an initial target for reducing new vascular events after mild ischemic stroke27. The number of steps per day after discharge from the rehabilitation unit increased by 724 steps compared with during hospitalization in stroke patients28. In stroke patients with independent walking, preventing new vascular events is an important therapeutic target27,29. However, FAC 4 stroke patients did not reach the target level for reducing new vascular events. For these patients, improved walking ability for outdoor walking independence and promotion of physical activity may be required during hospitalization. In addition to physical function, environmental factors are involved in physical activity in community-dwelling stroke patients30. Thus, the factors associated with physical activity during hospitalization and after discharge may differ. Even patients with mild stroke who are able to walk outdoors independently may need consider environmental factors after discharge to maintain physical activity.
On the other hand, the number of steps in the walking non-independence group was 1,970 steps/day (IQR, 1770.5 steps/day) for FAC 2 and 2646 steps/day (IQR, 1852 steps/day) for FAC 3. Klassen et al. reported that the number of steps during a physical therapy session was 580 (SD, 440) for usual care physical therapy, 2169 (SD, 1106) for more than double the intensity of the control, and 4747 (SD, 2083) for more than quadruple the intensity of the control, and walking recovery was improved in the higher dose group31. Patients with FAC 2.3 in our study did not reach the values of the previous study; however there is still a possibility of improvement. In addition, daytime and non-therapy time light intensity physical activity were related to functional recovery in patients with sub-acute stroke who could not walk independently5. Thus improvement of the walking ability in patients with poor walking ability and increasing the number of steps during therapy time and light intensity physical activity during non-therapy time are important methods for recovering the walking ability.
Study limitations
There were several limitations in the current study. First, the daily number of steps taken was used as the measure of physical activity; however, the Fitbit One mean error was higher for slower velocities (10.9% for speeds < 0.4 m/s)12. Thus, there may have been measurement errors of physical activity in stroke patients with low walking ability. Second, the daily number of steps was measured at 30 days after stroke onset in patients who were admitted to the rehabilitation unit. Thus, these results may only be applicable to stroke patients in the rehabilitation unit and not to acute stroke or community-dwelling chronic stroke patients. In addition, we could not measure long-term outcomes such as mRS or FAC at 3 or 6 months; thus the relationship between the number of steps at 30 days from stroke onset and long-term outcome was not clarified. Further studies are needed to investigate the step count associated with improvement in function during rehabilitation or beyond. Third, this was a cross-sectional study, and the causal relationship between the daily number of steps and walking independence was unknown. Additionally, the association between walking independence and age and severity also disappeared, which may possibly indicate a high correlation between the daily number of steps and age or stroke severity. Thus, further longitudinal studies with a larger sample size are required to clarify the causal relationship between the daily number of steps and walking independence. Fourth, although pre-stroke physical activity was associated with stroke severity and post-stroke outcome32,33, pre-stroke physical activity or fitness was not measured. Additionally, rehabilitation content affects physical activity; however, the contents of rehabilitation are not standardized because they are determined by each physician. Thus, these factors may affect the result of our study. Fifth, the wearing time of Fitbit One may vary depending on the patient’s lifestyle. Further studies are needed to consider wearing time to measure physical activity. Finally, this study did not use randomization or assignment; thus, there was a possibility of selection bias and lack of internal validity. Further studies with comparative validity designs are required.
Conclusion
This study demonstrated the association between the daily number of steps and walking ability, and calculated the cutoff value for walking independence in patients with sub-acute stroke hospitalized in the rehabilitation unit. A daily number of steps of 4286 steps/day may be useful for determining walking independence in patients with sub-acute stroke.
Change history
23 August 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41598-022-18802-8
References
Lynch, E. A. et al. Activity monitors for increasing physical activity in adult stroke survivors. Cochrane Database Syst. Rev. 7, CD012543 (2018).
Bailey, R. R., Phad, A., McGrath, R. & Haire-Joshu, D. Prevalence of five lifestyle risk factors among US adults with and without stroke. Disabil. Health J. 12, 323–327 (2019).
West, T. & Bernhardt, J. Physical activity in hospitalised stroke patients. Stroke Res. Treat. 2012, 813765 (2012).
Vanroy, C. et al. Physical activity in chronic home-living and sub-acute hospitalized stroke patients using objective and self-reported measures. Top Stroke Rehabil. 23, 98–105 (2016).
Shimizu, N., Hashidate, H., Ota, T. & Yatsunami, M. Daytime physical activity at admission is associated with improvement of gait independence 1 month later in people with subacute stroke: a longitudinal study. Top Stroke Rehabil. 27, 25–32 (2020).
Lacroix, J. et al. Physical activity level among stroke patients hospitalized in a rehabilitation unit. PM R. 8, 97–104 (2016).
Bohannon, R. W., Andrews, A. W. & Smith, M. B. Rehabilitation goals of patients with hemiplegia. Int. J. Rehabil. Res. 11, 181–184 (1988).
Skarin, M. et al. A mapping study on physical activity in stroke rehabilitation: establishing the baseline. J. Rehabil. Med. 45, 997–1003 (2013).
Shimizu, N., Hashidate, H., Ota, T., Suzuki, T. & Yatsunami, M. Characteristics of intensity-based physical activity according to gait ability in people hospitalized with subacute stroke: a cross-sectional study. Phys. Ther. Res. 22, 17–25 (2019).
Kubo, H. et al. Reference value of 6-minute walk distance in patients with sub-acute stroke. Top Stroke Rehabil. 27, 337–343 (2020).
Klassen, T. D. et al. “Stepping up” activity poststroke: ankle-positioned accelerometer can accurately record steps during slow walking. Phys. Ther. 96, 355–360 (2016).
Klassen, T. D. et al. Consumer-based physical activity monitor as a practical way to measure walking intensity during inpatient stroke rehabilitation. Stroke. 48, 2614–2617 (2017).
Hui, J. et al. Validity of the fitbit one for measuring activity in community-dwelling stroke survivors. Physiother. Can. 70, 81–89 (2018).
Fitbit Dashboard, www.fitbit.com/. Accessed 1 October 2019
Holden, M. K., Gill, K. M., Magliozzi, M. R., Nathan, J. & Piehl-Baker, L. Clinical gait assessment in the neurologically impaired. Reliability and meaningfulness. Phys. Ther. 64, 35–40 (1984).
Mehrholz, J., Wagner, K., Rutte, K., Meissner, D. & Pohl, M. Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Arch. Phys. Med. Rehabil. 88, 1314–1319 (2007).
Gladstone, D. J., Danells, C. J. & Black, S. E. The Fugl-Meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil. Neural Repair. 16, 232–40 (2002).
guidelines for the six-minute walk test. ATS committee on proficiency standards for clinical pulmonary function laboratories. ATS statement. Am J Respir Crit Care Med. 166, 111–117 (2002).
Kennedy, C. et al. Factors associated with time to independent walking recovery post-stroke. J. Neurol., Neurosurg. Psychiatr. 92(7), 702–708 (2021).
Cumming, T. B. et al. Very early mobilization after stroke fast-tracks return to walking: Further results from the phase II AVERT randomized controlled trial. Stroke 42, 153–158 (2011).
O’brien, R. M. A caution regarding rules of thumb for variance inflation factors. Qual. Quanti. 41(5), 673–690 (2007).
Akobeng, A. K. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatr. 96, 644–647 (2007).
Rosa, M. C., Marques, A., Demain, S. & Metcalf, C. D. Fast gait speed and self-perceived balance as valid predictors and discriminators of independent community walking at 6 months post-stroke–a preliminary study. Disabil. Rehabil. 37, 129–134 (2015).
Preston, E., Ada, L., Stanton, R., Mahendran, N. & Dean, C. M. Prediction of independent walking in people who are nonambulatory early after stroke: A systematic review. Stroke 52, 3217–3224 (2021).
Mansfield, A. et al. Use of accelerometer-based feedback of walking activity for appraising progress with walking-related goals in inpatient stroke rehabilitation: A randomized controlled trial. Neurorehabil. Neural Repair. 29, 847–857 (2018).
Askim, T., Bernhardt, J., Salvesen, O. & Indredavik, B. Physical activity early after stroke and its association to functional outcome 3 months later. J. Stroke Cerebrovasc. Dis. 23, e305–e312 (2014).
Kono, Y. et al. Predictive impact of daily physical activity on new vascular events in patients with mild ischemic stroke. Int. J. Stroke. 10, 219–223 (2015).
Simpson, D. B. et al. Go home, sit less: The impact of home versus hospital rehabilitation environment on activity levels of stroke survivors. Arch. Phys. Med. Rehabil. 99, 2216-2221.e1 (2018).
Kawajiri, H. et al. Maximum walking speed at discharge could be a prognostic factor for vascular events in patients with mild stroke: A cohort study. Arch. Phys. Med. Rehabil. 100, 230–238 (2019).
Kanai, M. et al. Association of perceived built environment attributes with objectively measured physical activity in community-dwelling ambulatory patients with stroke. Int. J. Environ. Res. Public Health. 16, 3908 (2019).
Klassen, T. D. et al. Higher doses improve walking recovery during stroke inpatient rehabilitation. Stroke 51, 2639–2648 (2020).
Krarup, L. H. et al. Prestroke physical activity is associated with severity and long-term outcome from first-ever stroke. Neurology 71, 1313–1318 (2008).
Ursin, M. H., Ihle-Hansen, H., Fure, B., Tveit, A. & Bergland, A. Effects of premorbid physical activity on stroke severity and post-stroke functioning. J. Rehabil. Med. 47, 612–617 (2015).
Acknowledgements
The authors thank the individuals who participated in this study and the physical therapy staff of the Department of Rehabilitation at Itami Kousei Neurosurgical Hospital for their assistance.
Funding
This work was supported by the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (Grant Number 20K23276).
Author information
Authors and Affiliations
Contributions
H.K. wrote the main manuscript text and prepared Fig. 1-2 and Tables 1–3. H.K., M.K., M.N., K.M. and S.S. designed the study. H.K., A.I. and A.T. corrected the data. H.K., M.K. and M.N. analyzed and interpreted the data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The Supplementary Information file that accompanies the original Article was exchanged. Full information regarding the correction made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kubo, H., Kanai, M., Nozoe, M. et al. Daily steps are associated with walking ability in hospitalized patients with sub-acute stroke. Sci Rep 12, 12217 (2022). https://doi.org/10.1038/s41598-022-16416-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16416-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.