Abstract
We retrospectively investigated in women treated with fulvestrant for HR+/HER2 negative advanced breast cancer clinical, pathological and molecular features associated with long-term benefit from treatment defined as being progression-free at 18 months. Specifically, we analyzed on formalin-fixed paraffin-embedded tumor samples ESR1 and PI3KCA mutations and miRNAs profiles. 59 patients were evaluable (median age of 67 years, range 32–92). 18-month PFS rate was 27%; the lack of visceral metastases significantly predicted the likelihood of being progression-free at 18 months, while PI3KCA mutations, found in 36% of patients, were not associated with 18-month PFS. As of miRNAs, miR-549a, miR-644a, miR-16-5p were negatively while let-7c-5p was positively associated with 18-month PFS. In addition, miR-520d-3p and miR-548g-3p values were significantly lower while miR-603, miR-181a-5p and miR-199a-miR-199b-3p values were significantly higher in patients achieving 18-month PFS. In silico analysis of targets modulated by these two latter groups of miRNAs show that in patients achieving 18-month PFS the Hippo and Wnt signaling pathways were predicted to be upregulated while endocrine resistance was potentially repressed by miR-603, miR-181a-5p and miR-199a-miR-199b-3p. Our results provide additional clues on the molecular mechanisms involved in fulvestrant activity and resistance. Underlying pathways should be further elucidated and confirmed in larger cohorts.
Similar content being viewed by others
Introduction
About two thirds of breast cancers are hormone receptor-positive HER2 negative (HR+/HER2−)1. The combination of endocrine therapy (ET) and CDK4/6 inhibitors (CDK4/6i) has established as standard treatment for HR+/HER2− advanced breast cancer (ABC)2. Four randomized trials including thousands of patients have shown an impressive and consistent advantage of 10–14 months in progression free survival (PFS) for the association of any of the three CDK 4/6i (palbociclib, ribociclib and abemaciclib) investigated with non-steroidal aromatase inhibitors (NSAI) in endocrine sensitive ABC as compared to the endocrine agent alone3.
On the other hand, since multiple mechanisms of resistance underlying CDK4/6i failure have been proposed, no definite treatment indications after progression to CDK4/6i exist and international guidelines indicate that a further endocrine manipulation as well as a switch to chemotherapy may be offered2,4.
The Selective Estrogen Receptor Downregulator (SERD) fulvestrant has established as a valuable option in the treatment of advanced HR+/HER2− ABC. Head-to-head comparison with NSAI in the 1st line treatment has shown the superiority of fulvestrant5 and in the CONFIRM study NSAI-resistant patients achieving a clinical benefit with fulvestrant had a prolonged disease control (> 16 months)6.
Thus it appears crucial to identify clinical and pathological factors which may predict the subset of patients who maintain endocrine sensitiveness and may be spared more aggressive treatments for a clinically relevant span of time and, on the other hand, patients who are likely to derive no or minimal benefit from fulvestrant and who deserve more effective treatments upfront. At the present time no predictors of response or resistance have been established.
MicroRNAs (miRNAs) are a class of small, non-coding RNA that regulate the gene expression of target mRNAs at post-transcriptional level7,8. miRNAs have been implicated in regulating breast cancer cell proliferation, cell death, apoptosis, immune response, cell cycle energetics, senescence, invasion, and metastasis9. Moreover, miRNAs are emerging as novel potential predictive/prognostic biomarkers of disease and response to therapies8,9. Several miRNAs have been found deregulated in breast cancer cell lines (BCCL), on cancer specimens and in serum of breast cancer patients and have been correlated with prognostic features and with response and resistance to endocrine manipulations9.
In the present study we investigated in a series of women with HR+/HER2− ABC treated with fulvestrant whether a panel of miRNAs was associated with long-term benefit from fulvestrant. According to previous literature data long-term benefit was defined as treatment duration without progression lasting at least 18 months10.
In addition, since endocrine resistance has been associated with mutations of ESR1 and PI3KCA the occurrence of these mutations was assessed and correlated with miRNA profiles and with outcome11,12.
Patients and methods
This observational retrospective multicentric study which aimed to describe the clinical outcome of patients with HR+/HER2− ABC who received fulvestrant as part of their routine treatment at 3 Italian Institutions and to correlate it with clinical, pathological and molecular features.
Eligible patients were pre/peri- and postmenopausal women aged ≥ 18 years diagnosed with HR+ (defined as ER and/or PgR ≥ 10%) and HER2− (defined as IHC 0, 1 + or 2 + with FISH negative) inoperable locally advanced and/or metastatic breast cancer for whom a tissue specimen of advanced or metastatic disease obtained for diagnosis was available. Pre/perimenopausal patients received concomitant ovarian suppression with GnRH analogues. Fulvestrant was administered 500 mg i.m. q28 days with loading dose after 14 days as any line of treatment. Patients treated before October 2011 received fulvestrant 250 mg i.m q28 days.
All tumor samples were obtained after diagnosis of advanced and/or metastatic disease and before fulvestrant treatment and were analyzed for routine diagnosis at the same pathologic department by breast dedicated pathologists.
Patient medical charts were reviewed and tumor response was assessed. Since this is a retrospective study response could not be evaluated according to RECIST 1.1 criteria in all patients, but CT scans and other imaging were reviewed in order to comply with RECIST criteria whenever possible. Information on age at diagnosis, menopausal status, previous adjuvant therapies, previous therapies for metastatic disease, pathological features of the metastatic tumor, sites of metastatic disease, best response, and disease progression if occurred and last follow up visit were collected.
All patients signed informed consent for participation to the study.
This study was approved by the institutional ethical committee of the coordinating center (Humanitas Research Hospital) and of the other participating Institutions and was conducted in compliance with 1964 Helsinki Declaration.
Mutation analyses
DNA was extracted from 5 slides (5 μm thickness) paraffin-embedded breast cancer tissue at least 70% tumor enriched using the Maxwell RSC DNA FFPE Kit (Promega) according to the manufacturer’s instructions. Manual microdissection was performed to precisely separate tumor regions from normal tissue. The enrichment in tumor cells reached a level higher than 80% upon microdissection. DNA was quantified by Nanodrop 2000 spectrophotometer (NanoDrop Products, Wilmington, DE, USA). Both PIK3CA (E542K, E542Q, C420R, H1047P, H1047R, H1047L, E545K, E545Q, Q546K, Q546E, E545A, E545G, E545V) and ESR1 (E380Q, S463P, D538G, D538V, L536H, L536R, L536P, Y537C, Y537S, Y537N, P535H) hot spot mutations were analyzed by processing 50 ng DNA using the Sequenom MassARRAY platform (SEQUENOM® Inc). The sequences and molecular weights of extension primers and products were listed in Supplementary Table 1. A cutoff of 5% of allelic frequency was generally guaranteed.
miRNA analyses
Tumor enriched RNA was extracted through manual microdissection of 5 paraffin-embedded breast cancer tissue slides (5um thickness) per patient as previously described for DNA. Total RNA isolation using the using the Maxwell RSC RNA FFPE kit (Promega, Madison, WI, USA) according to the manufacturer’s protocol. Quantification and RNA quality assessment were performed using a Nanodrop 2000 spectrophotometer (NanoDrop Products, Wilmington, DE, USA).
miRNA expression profiling was performed using the nCounter Human v3 miRNA Panel (NanoString Technologies, Seattle, WA, USA), which contains 798 unique miRNA barcodes. RNA was prepared according to the manufacturer’s protocol in a total of 5 runs. The nCounter Flex instrument was used and all counts were gathered by scanning on HIGH mode for 555 fields of view per sample. Raw data were analyzed as described in nCounter Data Analysis Guidelines for miRNA13. Specifically, the background threshold was set at 20; any value below this threshold was converted to zero. After that, miRNA counts were normalized to the geometric mean of the 50 miRNAs with the highest counts. Then, normalized miRNA values were subjected to statistical analyses. Nanostring data processing was carried out using R 3.6.1 software (R Core Team)14.
Predicted miRNA targets were searched using the miRTargetLink2 web tool, selecting only validated targets. Then, miRNAs targets were imported in STRING database and analyzed for significantly enriched Gene Ontology (GO) terms (Biological process and Molecular function) and Kyoto Encyclopaedia of Genes and Genomes (KEGG) Pathways using the human whole genome as statistical background as previously described (https://doi.org/10.3389/fonc.2021.643280).
Statistical analyses
Categorical variables were expressed as number and percentages, while continuous variables as medians with the respective range.
Clinical and demographical data and miRNAs were associated with outcome as continuous value in terms of progression free survival (PFS) by the cox proportional hazard model to calculate hazard ratio and their corresponding 95% confidence intervals. Moreover, the impact of miRNAs with long-term survival was described considering as success patients with a PFS ≥ 18 months and estimating Odds ratios with their corresponding 95% confidence intervals with a logistic regression model. Distribution of miRNAs between patients achieving or not 18-month PFS were estimated by Wilcoxon t test. For patients presenting miRNA assessment both at baseline (miRNAto) and at progression (miRNApd), a normalized variation was calculated as (miRNAto − miRNApd)/miRNAto to explore a possible miRNA profile association with progression.
Considering the small sample size all evaluation were explorative in nature. In the analysis of the 118 miRNAs the adjusted α level should be equal to 0.00042 considering Bonferroni Correction. A statistical p value of 0.05 was arbitrarily set to identify miRNAs of potential interest to be further explored in a larger sample size.
All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Results
From a database of 202 women with HR+/HER2− ABC who received treatment with fulvestrant from 2005 to 2017 at the 3 participating Institutions were retrieved 74 patients who underwent a diagnostic biopsy for advanced or metastatic disease before treatment. Fourteen patients were excluded because there was no residual tissue for further analyses and one additional patient did not have clinical information. Fifty-nine patients were evaluable for the molecular analyses. Tumor tissue was obtained from pleura (16), breast, when biopsy of synchronous metastatic sites was not feasible (15), lymph nodes (9), bone (7), skin (5), liver (4), other sites (3). Seven patients had also a biopsy obtained after progression on fulvestrant.
Baseline patient characteristics are summarized in Table 1. Median age was 67 years (range 32–92).
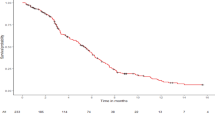
Clinical results
Overall median PFS (mPFS) was 10.7 months (range 2.2–14) and clinical benefit was obtained in 36 patients (61%). No clinical variable (tumor subtype, number of metastatic sites, number of previous lines, disease status at fulvestrant) was statistically significantly associated with mPFS, although a trend towards a shorter mPFS in patients with visceral metastases vs patients with no visceral involvement was observed (7.5 months vs 12.6, respectively p = 0.059). At the same time, patients with both HR positive tumors had a not statistically significant longer PFS as compared with patients with PgR negative tumors (13.8 vs 7.5 months, respectively, p = 0.099).
At 18 months 16 patients were progression free and alive with an 18-month PFS rate of 27%. Analyses of clinical and pathological variables showed that only the lack of visceral metastases significantly predicted the likelihood of being progression-free at 18 months (OR 0.25, 95% CI 0.07–0.9 p = 0.035).
Nonetheless, patients with ≤ 3 metastatic sites (OR: 1.6, CI 95% 0.2;14.9; p value: 0.71), patients with Luminal A tumors (OR 1.4, CI 95% 0.4; 4.8; p = 0.563), and patients treated with < 3 previous lines of therapy (OR 1.7, CI 95% 0.4–5; p = 0.390) had a higher probability to be alive and progression-free at 18 months as compared with patients with > 3 metastatic sites, with luminal B tumors and treated with ≥ 3 lines, respectively, although these results did not reach statistical significance.
Mutation analyses
ESR1 and PI3KCA mutations were assessed in 53 patients. ESR1 mutations were observed in the pretreatment biopsy in 5 patients, all previously treated with NSAI: D538V and Y537S (2 patients) and E380Q (1 patient). In the 7 patients with repeated biopsies ESR1 mutations were observed in both biopsies in 1 patient (Y537S) while they were detected only in the post-progression biopsy in 2 cases (Y537S and D538G). Since ESR1 mutations were found only in 9% of the patients, no correlation with other features was investigated.
PI3KCA mutations were found in pretreatment biopsies in 19 (36%) patients: H1047R (10 patients), E542K (4 patients), E545K and H1047L (2 patients), Q546K (1 patient). Among the 7 patients with repeated biopsies only 2 patients had PI3KCA mutations in both samples while 1 patient lost the PI3KCA mutation and developed an ESR1 mutation in the post-progression biopsy.
PFS in patients with PI3KCA mutated tumors was numerically shorter than in patients not harboring mutations (mPFS 7.6 vs 11 months, respectively, p = 0.28) On the other hand, the probability of being progression-free at 18 months was not different in the 2 groups (OR 1.01, 95% CI 0.28–3.6 p = 0.99).
miRNA analyses
miRNA profiles were assessed in 50 patients since patients with bone biopsies were excluded for this analysis because of poor RNA quality.
45 miRNAs were detected in at least 30 samples, 83 miRNAs were detected in at least 20 samples and 118 miRNAs were detected in at least 10 samples.
We investigated association with outcome only for miRNAs which were detected in at least 20% (n = 10) of samples (detailed in Supplementary Table 2).
miRNAs which were statistically significant associated with PFS are reported in Table 2. Fourteen miRNAs were negatively associated with outcome while 2 miRNAs belonging to the let-7 family were positively associated with improved outcome.
When we considered the likelihood of being progression free at 18 months as endpoint only miR-549a, miR-644a confirmed to be negatively associated with outcome in addition to miR-16-5p, while let-7c-5p was associated also with a greater likelihood of being progression free at 18 months (Table 2).
When we analyzed miRNA distribution comparing patients with or without a PFS ≥ 18 months we found that miR-549a, miR-644a, miR-16-5p values were significantly higher while let-7c-5p value was lower in patients not achieving 18-month PFS, respectively. In addition to these, miR-520d-3p and miR-548g-3p were significantly and negatively associated with 18-month PFS while miR-603, mir-181a-5p and miR-199a-miR-199b-3p values were statistically significantly higher in the long-term benefit cohort; moreover miR-125b-5p showed a not significant trend to be higher in patients being progression free at 18 months. No statistically significant results were found based on adjusted p value (Bonferroni correctioni, p = 0.00042).
In silico analysis of predicted targets (Supplementary Tables 3, 4) showed that cell metabolism was the main biological process involved in fulvestrant treatment. Analysis of predicted pathways suggested that miR-520d-3p and miR-548g-3p decrease might induce Hippo and Wnt signaling (Supplementary Table 5). On the contrary, high levels of miR-603, mir-181a-5p, miR-199a-miR-199b-3p might repress endocrine resistance thus potentially promoting the anti-tumor activity of Fulvestrant (Supplementary Table 6).
Finally, no specific miRNA expression was associated with PI3KCA mutation status (data not shown). Similarly, we did not find any specific baseline miRNA profile or change at disease progression in the 7 patients for whom both a baseline and post progression biopsy were available (data not shown).
Discussion
The identification of clinical, pathological and molecular features predicting the benefit of treatments is a major goal for medical oncologists.
Fulvestrant has been proven a valuable option for treatment of HR+ ABC. First-line fulvestrant was associated with a mPFS of 16.6 months which extended to 22 months in patients with bone-only metastases in a population of mostly treatment-naïve patients (5). In the cohort of patients treated as 1st line in the MonaLEEsa-3 study mPFS in the Fulvestrant/placebo arm was 19 months, while in the control arms of 2nd/3rd line studies with CDK 4/6i and Fulvestrant, mPFS decreased to 9 and 4.6 months, respectively15,16,17. Similar data have been reported in patients treated with Fulvestrant in real-world series18,19,20.
Identification of pathological and molecular features predicting benefit from treatment in tumor samples of patients treated with fulvestrant has been attempted previously21,22. The TransCONFIRM, a translational analysis within the CONFIRM trial aimed to identify clinical-pathological features and molecular signatures in the primary tumors predicting response to fulvestrant, showed in the 112 samples analyzed that only PgR and HER2 expression and a signature of 37 genes were independently associated with PFS21. Of note, no correlation with ESR1 mutations on primary tumors was found21. Christensen et al. investigated in mRNA extracted from 226 tumor samples of patients treated with fulvestrant the predictive value of a mathematical algorithm based on the expression of multiple genes (DRP)22. The DRP was associated although not significantly with outcome in patients treated in earlier lines and unexposed to previous adjuvant endocrine therapies22.
Our clinical data are comparable with those mentioned above, showing a mPFS of 10.6 months in a heavily pretreated cohort, since 46% of our patients were treated in 3rd or later lines. Only the occurrence of visceral metastases was associated with a worse outcome, although we cannot exclude that the correlations between HR and PI3KCA mutation status and outcome were not significant only because of the limited sample size. Similarly, only the absence of visceral metastases was significantly associated with a fourfold higher likelihood of long-term benefit from fulvestrant.
Notably, patients starting Fulvestrant after progressing to other therapies experienced a similar benefit as patients receiving treatment as maintenance after chemotherapy (mPFS = 9.9 months vs 10.8 months, respectively), similarly to what reported in a larger real-world series20.
The role of PI3KCA mutations in the mechanisms of resistance to fulvestrant is not clear. Results of the fulvestrant/placebo arms in studies with PI3K inhibitors conducted in patients harboring or not PI3KCA mutations are inconsistent23. While in the BELLE-2 study mPFS in patients with PI3KCA wild-type tumors doubled that of patients with PI3KCA mutant tumors, no difference was observed in the same comparisons within the BELLE-3 and SOLAR-1 studies23. In a recent analysis on ctDNA of patients included in the PALOMA 3 trial PI3KCA mutations, while being among the most common mutations at baseline, did not increase after progression and did not correlate with PFS24.
In our study PI3KCA mutations were found in about 36% of patients, consistently with what expected in Luminal breast cancers25 and were associated with a numerically shorter PFS, but not with a lower likelihood of being progression-free at 18 months. These findings are only partially consistent with the analysis of long-term benefit in the fulvestrant/placebo arm of the PALOMA 3 trial since in this study only 6% of patients harboring PI3KCA mutations vs 39% of patients with PI3KCA wild type tumors were treated for ≥ 18 months10.
Similarly to what observed in the PALOMA 3 study, the lack of PgR expression was associated with a lower likelihood of long-term benefit from Fulvestrant10.
The rate of ESR1 mutations was lower than expected, despite more than 50% of patients had previously received a NSAI25. Notably ESR1 mutations were observed only in post-progression biopsy in 2 patients, one of whom had lost at the same time PI3KCA mutation, suggesting that a different mechanism of resistance to fulvestrant was developed.
A huge number of miRNAs have been associated with breast cancer with alternative and not always consistent suppressive or oncogenic properties for each miRNA and neither meta-analyses have been able to define an unequivocal expression and role even in case of frequently expressed miRNAs9,26,27,28,29. Discrepancies among studies may be attributed to several factors as differences in patient populations, biological samples (fresh tissues, paraffin-embedded tissues and blood) and methodological procedures (qRT- PCR, NGS, microarray) but may also be related to different functions of each miRNA according to the tumor microenvironment9,26,27,28,29.
In our study we identified 9 miRNAs which were significantly and differently associated with 18-month PFS. Literature data provide evidence about 3 of these miRNAs (let-7c, miR-520d-3p, miR-181a) to be involved in HR+ ABC30,31,32,33,34,35. In particular miR-520d-3p was among miRNAs which were downregulated upon estradiol stimulation in BCCL30. On the other hand, miR-520d-3p has also been proposed to suppress ESR1 expression and to be involved in endocrine resistance31,32.
A larger amount of consistent evidence is available on the let-7 miRNA family which was demonstrated to target ER- alfa and negatively affect its function in ER-positive BCCL33. In particular, let-7c targets ESR1 and is less expressed in metastatic tissue than in primary tumor and normal tissue32. Upon analysis of clinical data from The Cancer Genome Atlas (TCGA), it was suggested that low expression of let-7c in addition to other miRNAs (miR-99a and miR-125b) was associated with worse overall survival compared with patients who had high expression of these miRNAs34.
Our findings showing that let-7c-5p was significantly and positively correlated with a higher likelihood of being progression-free at 18 months and let-7f-5p significantly directly correlated with PFS confirmed the tumor suppressive properties for the members of the let-7 family.
In addition, we found a not significantly higher expression of miR-125b in patients achieving 18-month PFS, supporting the protective role outlined by TCGA for this miRNA34.
Contradictory evidence is available on miR-181a-5p, which belongs to a family of largely expressed miRNAs29. It was found to be upregulated and associated with poor survival in metastatic breast cancer patients particularly in those with TNBC29, but, on the other hand, it is among the most potent miRNAs repressing cell growth and counteracting estradiol-dependent cell proliferation30. In our study a greater expression of miR-181a was positively associated with long-term fulvestrant benefit.
Also on miR-16-5p literature data are somehow inconsistent since preclinical data support tumor suppressive properties but an increased expression in triple negative breast cancer (TNBC) as compared to normal tissues has been found as well as either a down- or upregulation in the serum of breast cancer patients as compared to healthy controls33,35,36,37. In our study miR-16-5p was associated with a decreased probability of being progression-free at 18 months.
In silico analysis of the targets of miRNAs inversely associated with long-term outcome showed that oncogene-induced cell senescence was the most affected biological processes. Analysis of predicted pathways suggested that miR-520d-3p and miR-548g-3p decrease might induce Hippo and Wnt signaling. On the other hand miR-603 and miR-181a-5p and miR-199a-miR-199b-3p were predicted to suppress endocrine resistance.
The miRNAs we found significantly associated with long-term benefit or resistance to fulvestrant were not among miRNAs differently expressed in fulvestrant-resistant cell lines as compared with parental MCF-7 cells38,39. Moreover, in our series miR-221 and mir-222 which had been associated with fulvestrant resistance in BCCL were detected only in 2 and 8 samples, respectively and therefore were not further correlated with outcome; at the same time miR-21, despite being confirmed among the most highly expressed miRNAs, did not show any association with outcome (see Supplementary Table 2)40,41.
We acknowledge that our study has some limitations. First of all, the limited number of patients with available metastatic tissue which resulted in a small sample considering the large number of putative predictive variables examined especially for miRNA analyses; then the retrospective design which resulted in missing clinical information and which may have not allowed to meet with a strict application of RECIST 1.1 criteria for all patients. Moreover, we did not perform in vitro assays in BCCL to better elucidate the correlation between the miRNA profile associated with the in vivo response to fulvestrant and gene expression analyses to identify the related target genes involved. Finally, since the current use of fulvestrant monotherapy is recommended only after CDK 4/6i, we cannot rule out that this treatment can induce molecular patterns different from those observed in our CDK 4/6i naïve population.
In conclusion, altogether our clinical findings are consistent with literature data from randomized trials and real-world series, confirming the poor prognostic role of visceral metastases. Our data do not support an association between PI3KCA mutations and long-term benefit from treatment. Furthermore, we propose a new panel of miRNAs which were associated with long-term benefit of endocrine therapy and which are mainly involved in cell metabolism and endocrine resistance. Our results provide some additional clues on the mechanisms involved in fulvestrant activity and resistance although underlying molecular pathways should be further elucidated and confirmed in larger cohorts of breast cancer patients.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on request.
References
Hammond, M. E. et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J. Clin. Oncol. 2, 2784–2795. https://doi.org/10.1200/JCO.2009.25.6529 (2010).
Cardoso, F. et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann. Oncol. 31, 1623–1649. https://doi.org/10.1016/j.annonc.2020.09.010 (2020).
Murphy, C. G. The role of cd4/6 inhibitors in breast cancer. Curr. Treat. Option Oncol. 20, 52. https://doi.org/10.1007/s11864-019-0651-4 (2019).
NCCN v 1.2021 Guidelines. www.NCCN.org. Accessed 5 July 2021.
Robertson, J. F. R. et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): An international, randomised, double-blind, phase 3 trial. Lancet 388, 2997–3005. https://doi.org/10.1016/S0140-6736(16)32389-3 (2016).
Garnett, S. A. et al. Comparing duration of response and duration of clinical benefit between fulvestrant treatment groups in the CONFIRM trial: Application of new methodology. Breast Cancer Res. Treat. 138, 149–155. https://doi.org/10.1007/s10549-012-2395-8 (2013).
Di Leva, G., Garofalo, M. & Croce, C. M. MicroRNAs in cancer. Annu. Rev. Pathol. 9, 287–314. https://doi.org/10.1146/annurev-pathol-012513-104715 (2014).
Vaira, V. et al. MicroRNA-425-3p predicts response to sorafenib therapy in patients with hepatocellular carcinoma. Liver Int. 35, 1077–1086. https://doi.org/10.1111/liv.12636 (2015).
Campos-Parra, A. D. et al. Micro-RNA as potential predictors of response to breast cancer systemic therapy: Future clinical implications. Int. J. Mol. Sci. 18, 1182. https://doi.org/10.3390/ijms18061182 (2017).
Cristofanilli, M. et al. Predictors of prolonged benefit from palbociclib plus fulvestrant in women with endocrine-resistant hormone receptor- positive/human epidermal growth factor receptor 2. Negative metastatic breast cancer in PALOMA-3. Eur. J. Cancer 104, 21–31. https://doi.org/10.1016/j.ejca.2018.08.011 (2018).
Jeselsohn, R., Buchwalter, G., De Angelis, C., Brown, M. & Schiff, R. ESR1 mutations—A mechanism for acquired endocrine resistance in breast cancer. Nat. Rev. Clin. Oncol. 10, 573–583. https://doi.org/10.1038/nrclinonc.2015.117 (2015).
Miller, T. W., Rexer, B. N., Garrett, J. T. & Arteaga, C. L. Mutations in the phosphatidylinositol 3-kinase pathway: Role in tumor progression and therapeutic implications in breast cancer. Breast Cancer Res. 13, 224. https://doi.org/10.1186/bcr3039 (2011).
Tabano, S. et al. A miRNome analysis of drug-free manic psychotic bipolar patients versus healthy controls. Eur. Arch. Psychiatry Clin. Neurosci. 270, 893–900. https://doi.org/10.1007/s00406-019-01057-2 (2020).
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/ (2014). Accessed 15 Sept 2020.
Slamon, D. J. et al. Overall survival with ribociclib plus fulvestrant in advanced breast cancer. N. Engl. J. Med. 382, 514–524. https://doi.org/10.1056/NEJMoa1911149 (2020).
Sledge, G. W. et al. The effect of abemaciclib plus fulvestrant on overall survival in hormone receptor–positive, ERBB2-negative breast cancer that progressed on endocrine therapy—MONARCH 2 A randomized clinical trial. Jama Oncol. 6, 116–124. https://doi.org/10.1001/jamaoncol.2019.4782 (2020).
Turner, N. C. et al. Overall survival with palbociclib and fulvestrant in advanced breast cancer. N. Engl. J Med. 379, 1926–1936. https://doi.org/10.1056/NEJMoa1810527 (2018).
Kawaguchi, H. et al. Outcomes of fulvestrant therapy among Japanese women with advanced breast cancer: A retrospective multicenter cohort study (JBCRG-C06; Safari). Breast Cancer Res. Treat. 163, 545–554. https://doi.org/10.1007/s10549-017-4212-x (2017).
Blancas, I. et al. Efficacy of fulvestrant in the treatment of postmenopausal women with endocrine-resistant advanced breast cancer in routine clinical practice. Clin. Transl. Oncol. 2, 862–869. https://doi.org/10.1007/s12094-017-1797-9 (2018).
Palumbo, R. et al. Patterns of treatment and outcome with 500-mg fulvestrant in postmenopausal women with hormone receptor-positive/ HER2-negative metastatic breast cancer: A real-life multicenter Italian experience. Ther. Adv. Med. Oncol. 11, 1–13. https://doi.org/10.1177/1758835919833864 (2019).
Jesehlson, R. et al. TransCONFIRM: Identification of a genetic signature of response to fulvestrant in advanced hormone receptor-positive breast cancer. Clin. Cancer Res. 22, 5755–5764. https://doi.org/10.1158/1078-0432.CCR-16-0148 (2016).
Christensen, T. D. et al. Prediction of fulvestrant efficacy in patients with advanced breast cancer: Retrospective-prospective evaluation of the predictive potential of a multigene expression assay. Breast Cancer 27, 266–276. https://doi.org/10.1007/s12282-019-01017-7 (2020).
Mollon, L. E. et al. A systematic literature review of the prognostic and predictive value of PIK3CA mutations in HR+/HER2- metastatic breast cancer. Clin. Breast Cancer 20, e232–e243. https://doi.org/10.1016/j.clbc.2019.08.011 (2020).
O’Leary, B. et al. Circulating tumor DNA markers for early progression on fulvestrant with or without palbociclib in ER+ advanced breast cancer. J. Natl. Cancer Inst. 113, 309–317. https://doi.org/10.1093/jnci/djaa087 (2021).
Razavi, P. et al. The genomic landscape of endocrine-resistant advanced breast cancers. Cancer Cell 34, 427–438. https://doi.org/10.1016/j.ccell.2018.08.008 (2018).
Van Schooneveld, E. et al. Dysregulation of microRNAs in breast cancer and their potential role as prognostic and predictive biomarkers in patient management. Breast Cancer Res. 17, 21. https://doi.org/10.1186/s13058-015-0526-y (2015).
Bertoli, G., Cava, C. & Castiglioni, I. MicroRNAs: New biomarkers for diagnosis, prognosis, therapy prediction and therapeutic tools for breast cancer. Theranostics 5, 1122–1143. https://doi.org/10.7150/thno.11543 (2015).
Howard, E. W. & Yang, X. MicroRNA regulation in estrogen receptor-positive breast cancer and endocrine therapy. Biol. Proced. Online 20, 7. https://doi.org/10.1186/s12575-018-0082-9 (2018).
Zelli, V. et al. Circulating microRNAs as prognostic and therapeutic biomarkers in breast cancer molecular subtypes. J. Pers. Med. 10, 98. https://doi.org/10.3390/jpm10030098 (2020).
Khalife, H., Skafi, N., Fayyad-Kazan, M. & Badran, B. MicroRNAs in breast cancer: New maestros defining the melody. Cancer Genet. 2020, 246–247. https://doi.org/10.1016/j.cancergen.2020.08.005 (2020).
Maillot, G. et al. Widespread estrogen-dependent repression of microRNAs involved in breast tumor cell growth. Cancer Res. 69, 8332–4830. https://doi.org/10.1158/0008-5472.CAN-09-2206 (2009).
Leivonen, S.-K. et al. Protein lysate microarray analysis to identify microRNAs regulating estrogen receptor signaling in breast cancer cell lines. Oncogene 28, 3926–3936 (2009).
Zhao, Y. et al. Let-7 family miRNAs regulate estrogen receptor alpha signaling in estrogen receptor positive breast cancer. Breast Cancer Res. Treat. 127, 69–80. https://doi.org/10.1038/onc.2009.241 (2011).
Bailey, S. T., Westerling, T. & Brown, M. Loss of estrogen-regulated microRNA expression increases HER2 signaling and is prognostic of poor outcome in luminal breast cancer. Cancer Res. 75, 436–445. https://doi.org/10.1158/0008-5472.CAN-14-1041 (2015).
Feliciano, A. et al. Five microRNAs in serum are able to differentiate breast cancer patients from healthy individuals. Front. Oncol. 10, 586268. https://doi.org/10.3389/fonc.2020.586268 (2020).
Haghi, M., Taha, M. F. & Javeri, A. Suppressive effect of exogenous miR-16and miR-34a on tumorigenesis of breast cancer cells. J. Cell. Biochem. 120, 13342–13353. https://doi.org/10.1002/jcb.28608 (2019).
Arabkari, V. et al. Relative and absolute expression analysis of microRNAs associated with luminal A breast cancer—A comparison. Pathol. Oncol. Res. 26, 833–844. https://doi.org/10.1007/s12253-019-00627-y (2020).
Zhou, Q. et al. Differential microRNA profiles between fulvestrant-resistant and tamoxifen-resistant human breast cancer cells. Anticancer Drugs 29, 539–548. https://doi.org/10.1097/CAD.0000000000000623 (2018).
Guo, J. et al. Differential microRNA expression profiles determined by next generation sequencing in three fulvestrant resistant human breast cancer cell lines. Oncol. Lett. 17, 3765–3776. https://doi.org/10.3892/ol.2019.10061 (2019).
Rao, X. et al. MicroRNA-221/222 confers breast cancer fulvestrant resistance by regulating multiple signaling pathways. Oncogene 30, 1082–1097. https://doi.org/10.1038/onc.2010.487 (2011).
Yu, X. et al. Silencing of microRNA-21 confers the sensitivity to tamoxifen and fulvestrant by enhancing autophagic cell death through inhibition of the PI3K-AKT-mTOR pathway in breast cancer cells. Biomed. Pharmacother. 77, 37–44. https://doi.org/10.1016/j.biopha.2015.11.005 (2016).
Acknowledgements
The authors are indebted with prof. Stefano Aldo Pileri for his helpful comments in the processing of miRNA data.
Funding
This study was supported by an unrestricted Grant from Astra Zeneca. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design Conceptualization, R.T., formal analysis V.V., A.D., G.G., N.R., F.B.; investigation R.T., V.B., P.S., G.M.; resources, R.T., V.B., P.S., G.M.; data curation, L.G., S.M.; writing—original draft preparation R.T., V.V., A.D.; writing—review and editing R.T., V.V., L.G., A.D., S.M., N.R., F.B., A.S.; supervision, A.S.; funding acquisition R.T. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Rosalba Torrisi: Astra Zeneca, Eisai, Pfizer, Eli Lilly, Exact Sciences, MSD. Armando Santoro BMS, Servier, Gilead, Pfizer, Eisai, Bayer, MSD, Takeda, Roche, Astra Zeneca, Pfizer, Eli Lilly, Novartis, Aqule, Sandoz, Abb-Vie. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Torrisi, R., Vaira, V., Giordano, L. et al. Predictors of fulvestrant long-term benefit in hormone receptor-positive/HER2 negative advanced breast cancer. Sci Rep 12, 12789 (2022). https://doi.org/10.1038/s41598-022-16409-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16409-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.