Abstract
Breast cancer is the most common cancer among women in Taiwan. The age-standardized incidence rate has doubled in just 20 years, causing considerable concern to health professionals and the general public. This study used an ensemble of age-period-cohort models to estimate breast cancer incidence trends in Taiwan from 1997 to 2016 and project trends up to 2035. The (truncated) world standard population (World Health Organization 2000) proportions (age groups: 25–29, 30–34, …, 80–84, and older than 85 years) were used to calculate age-standardized incidence rates. The age-standardized incidence rate from 1997 (60.33/100,000 population) to 2016 (128.20/100,000 population) increased rapidly. The projection is that the increase in the age-standardized incidence will subsequently slow and exhibit a plateau in 2031 (151.32/100,000 population). From 2026 to 2035, the age-specific incidence rates for women older than 55 years old (postmenopausal breast cancer) are projected to increase with larger percentage increments for older women. A future leveling of female breast cancer incidence trends in Taiwan is anticipated. The majority of the patients with breast cancer in the future will be women aged 55 years and older. Education on lifestyle recommendations and mammography screening is required to reduce the burden of breast cancer. The results should have implications for other countries which are also confronted with the same public health problem of rapidly increasing breast cancer incidences.
Similar content being viewed by others
Introduction
Would Health Organization announce that breast cancer has overtaken lung cancer as the most common cancer in the world1. In Taiwan, it is also the leading cancer among women. The age-standardized incidence rate of breast cancer in Taiwan has increased in recent decades, doubling in just 20 years from 1997 to 2016. Such rapid rises constitute a significant concern to health professionals and the general public. In response to this crisis, the Health Promotion Administration in Taiwan launched a nationwide mammography screening program (every two years for women aged 50 to 69) in 2004. In 2009, the program was further expanded to cover 45 to 69 year old women and 40 to 44 year old women with second-degree relatives ever diagnosed with breast cancer.
Secular trends may provide clues about the etiological factors for breast cancer, generating hypotheses that can be tested. Examination of the patterns and trends of breast cancer incidences enables the etiology of the illness and targets for intervention to be identified to mitigate the disease’s burden. Cancer incidence projections are also essential for the planning of resources and the informing of cancer control programs. In this paper, we fit an ensemble of age-period-cohort (APC) models to breast cancer incidence data in Taiwan from 1997 to 2016 and provide incidence rate projections up to 2035 to establish whether the increasing trend will continue increasing or will level off. The results should be implicative for other countries also confronted with the same public health problem of rapidly growing breast cancer incidences.
Materials and methods
Data source
Breast cancer cases (The International Statistical Classification of Diseases and Related Health Problems 10th Revision: C50) in women and the corresponding populations were abstracted from the Taiwan Cancer Registry. Some quality indicators for this registry are as follows: population coverage = 98.4%; percentage of cases with death certificate only = 0.9%; percentage of morphological verification = 93.0% for all sites combined; data timeliness = 14 months2,3, which rank the registry among the top-tier gold-level cancer registries in the world. Supplementary Table 1 lists the data quality indices of the Taiwan Cancer Registry from 2002 to 2016.
We used 13 groups to categorize the age at diagnosis of patients with breast cancer aged 25 years and older (25–29, 30–34, …, 80–84, and more than 85 years). Data from patients under 25 years at diagnosis were not used because of the scarcity of such cases (Supplementary Table 2). We categorized the calendar years of diagnosis according to each year from 1997 to 2016 by every year (20 groups). The (truncated) world standard population (World Health Organization 2000) proportions (age groups: 25–29, 30–34, …, 80–84, and older than 85 years; Supplementary Table 3) were used to calculate age-standardized incidence rates. The population projection method was the cohort-component method, and the source was National Development Council Population Projections for Taiwan.
This study protocol was approved by the National Taiwan University Research Ethics Committee (202101HM030) and the Data Release Review Board of the Health Promotion Administration, Ministry of Health and Welfare in Taiwan. All methods were performed in accordance with the relevant guidelines and regulations. In addition, the Research Ethics Committee waived the requirement for informed consent due to the lack of personal information and secondary data in the study.
Statistical analysis
We used the APC model to analyze the breast cancer incidence rate and project the trend to 2035. Because of the perfect collinearity between the three temporal factors (cohort = period – age), the APC model suffers from a non-identification problem. In addition, we used data provided in 5-year age groups and 1-year periods in the study, which might cause additional identifiability issues with the unequal intervals in the definition of cohort indices4. However, we considered the APC model with the cohort curvature effect but without the linear cohort effect for making parameters estimable. The incidence projections in this study were impervious to the non-identifiability problem because the fitted values in the nonidentifiable APC model were the same for all possible sets of parameter estimates.
Details of the methods we used in this study were described elsewhere5. An ensemble of 265 APC models was first constructed using the breast cancer incidence data from 1997 to 2006. The 53 model types, consisting of cubic spline APC models (knots were placed at percentiles)6, polynomial APC models (quadratic, cubic, and other polynomial models)7, and Tzeng and Lee’s APC model8, were presented in Supplementary Table 4. The constructed APC models were then used to predict breast cancer incidence rates from 2007 to 2016 with 5 types of link functions (log, power 2, power 3, power 4, and power 5). The prediction was further subjected to a 0%, 5%, 10%, 15%, …, or 100% year-on-year attenuation, respectively, resulting in 5565 (53 model types × 5 link functions × 21 attenuations) sets of projection results.
The symmetric mean absolute percentage error (SMAPE) index was used to quantify the prediction error for each projection. The model and the attenuation factor with the smallest SMAPE were selected. The selected model was then fitted to all available breast cancer incidence data from 1997 to 2016. Based on this refitted model and the previously selected attenuation factor, a projection was made for 2035; the age-specific incidence rates were first projected, and the age-standardized incidence rate was then calculated. For this model selection procedure, the model with the smallest cross-validation error was assumed to be appropriate for future projection9,10. Data management and analyses were performed using SAS statistical software (version 9.4).
Results
The age-standardized breast cancer incidence rate increased from 60.35 to 128.20 per 100,000 population from 1997 to 2016 (the annual percentage change = 5.62%). The mean age of breast cancer diagnosis in Taiwan also increased from 50.5 years in 1997 to 56.0 years in 2016, and the median age at diagnosis was from 48 to 55 years old (Supplementary Table 5).
The best-selected model for the projection (SMAPE = 5.58%) was a polynomial APC model with a log link function and 30% attenuation. Table 1 presents the age-standardized (age range 25 + years) and age-specific incidence rates and case numbers of breast cancer with projected percentage changes from 2016 to 2025 and from 2026 to 2035. Supplementary Table 6 displays the projections of the age-standardized breast cancer incidence rates with different attenuations.
An open interval of 85 + years was used in this paper instead of an equal 5-year age interval. For a sensitivity analysis, we restricted our analysis to the age range 25–84 years and projected the age-standardized and age-specific incidence rates and case numbers in Supplementary Table 7. Because there were very few cases aged over 85 + years, excluding them in the analysis is similar to when including them.
The age-standardized incidence rate of breast cancer was 128.20/100,000 population in 2016. The projected incidence rates are 148.25/100,000 population in 2025 (increased by 15.64% from 2016 to 2025) and 149.45/100,000 population in 2035 (increased by a mere 0.81% from 2026 to 2035). Age-specific incidence rates for all age groups are projected to increase from 2016 to 2025. The three age groups with the greatest increment are 70–74 years (increased by 44.23%), older than 85 years (increased by 43.91%), and 80–84 years (increased by 41.81%). By contrast, the age-specific incidence rate of the 45–49 year age group is projected to increase from 2016 to 2025 by only 0.73%. From 2026 to 2035, the age-specific incidence rate for women older than 55 is projected to increase further with larger percentage increments for older women.
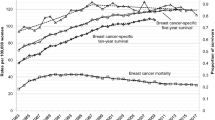
Figure 1 displays the age-standardized breast cancer incidence rate from 1997 to 2016 and the projection from 2017 to 2035. The age-standardized incidence rate from 1997 (60.33/100,000 population) to 2016 (128.20/100,000 population) increased rapidly. The increase in the age-standardized incidence subsequently slows and exhibits a plateau in 2031 (151.32/100,000 population).
Age-standardized breast cancer incidence rate from 1997 to 2016 and projection from 2017 to 2035. The World Health Organization’s 2000 World Standard Populations were used to compute the truncated age-standardized incidence rate (age range 25 + years). Dotted lines indicate 95% confidence intervals for the projections.
Figure 2 demonstrates the age-specific breast cancer incidence rate from 1997 to 2016 and the projections from 2017 to 2035 for each calendar year and birth cohort. From 1997 to 2016, the age-specific incidence rate for each calendar year in all age groups has increased rapidly, particularly in women aged 60–64, 65–69, and older than 85 years. The projected age-specific incidence rates for each calendar year increase until 2035 for women older than 65 years. The projected age-specific incidence rates for each calendar year in the groups of women aged 50–54, 55–59, and 60–64 years exhibit a plateau in 2031 (247.46/100,000 population), 2031 (258.51/100,000 population), and 2033 (273.08/100,000 population), respectively. For women younger than 50 years, the projected age-specific incidence rates for each calendar year reach a plateau around 2017 to 2027. By comparison, the birth-cohort trends are more consistent across different ages. The age-specific incidence rates of the birth cohort born before 1985 increase rapidly, whereas the projected age-specific incidence rates of those born after 1985 reach a plateau.
Discussion
This study observed a rapid increase in breast cancer incidence from 1997 to 2016. Taiwan has been industrialized since the 1960s. After 1960, Taiwanese women adapted to westernized lifestyles, resulting in higher caloric and higher fat diets, earlier menarche11, drastically reduced fertility rates12, later natural menopause ages13, and later childbearing ages. These are all documented risk factors for breast cancer14,15. Breast cancer incidence rapidly increased from 1997 to 2016, but the projected rate is more stable. Our finding shows that the projected age-standardized incidence rate of breast cancer in Taiwan will level off and exhibit a plateau in 2031 (151.32/100,000 population). Supplementary Figure S1 shows that (1) the age-standardized incidence rate for Taiwan in 1997 (60.33/100,000 population) was similar to that for Asian countries (China and India), (2) the rate for Taiwan in 2012 (117.29/100,000 population) was similar to that for Asian-Americans, and (3) the projected plateau rate for Taiwan in 2031 (151.32/100,000 population) is similar to that for Western developed countries or regions. (Supplementary Figure S2 also displayed the global age-standardized breast cancer incidence rates in 1997.) These indicate an epidemiological transition of breast cancer in Taiwan from Eastern countries to one characteristic of Western developed countries. We also projected the age-standardized breast cancer incidence rates separately for urban and rural regions in Taiwan into the future and found the trends leveling off in both regions (Supplementary Figure S3). We projected the age-standardized breast cancer mortality rate in Taiwan into the future (Supplementary Figure S4). However, Taiwan’s breast cancer mortality rate increases less dramatically than the incidence rate.
Age-specific incidence rates for all the age groups are projected to increase from 2016 to 2025. From 2026 to 2035, the age-specific incidence rate is projected to increase further for women older than 55. By contrast, the age-specific incidence rate for women younger than 55 is projected to plateau. In the future, most patients with breast cancer will be women aged 55 years and older (postmenopausal breast cancer). Differential trends among pre and postmenopausal women have been observed in many European countries, where the increases in incidence were more profound in women aged 50 to 69 years16,17. Asian women with breast cancer typically exhibit a younger onset age. The age curve of breast cancer incidence rates reaches a peak before 50 years18. This unimodal bell‐shaped age curve contrasts with the monotonic increase in age-specific breast cancer incidence rate observed in Western countries or regions19. Physicians and the general public in Taiwan believe that patients are diagnosed with breast cancer at increasingly young ages. The impression, however, is not valid. The mean age of breast cancer diagnosis in Taiwan increased from 51 years in 1997 to 56 years old in 2016 (and the median age at diagnosis from 48 to 55 years old). Shifts toward older peak ages of incidence have also occurred in Thailand20 and China21. Another explanation for the rise in premenopausal breast cancer incidence is screening policies17. Most North American and European countries recommend mammography examinations for women older than 50. In Taiwan, however, the recommended age to initiate mammography screening is an earlier age of 40 years old.
Breast cancer encompasses several distinct pathologic entities broadly divided into premenopausal and postmenopausal diseases22. Obesity increases breast cancer risk among postmenopausal women23,24,25. Associations between obesity and postmenopausal breast cancer are mediated mainly by serum estrogen levels25. Obesity is an established risk factor for postmenopausal breast cancer, not premenopausal breast cancer. This could explain some of the differences in age-specific incidence trends. The previous population-based survey from 1993 to 2008 indicated that obesity prevalence has increased among Taiwanese women26. Our projection study, which was based on the assumption that the breast cancer risk factors remain unchanged, suggests that the burden of the disease will continue to increase. This highlights questions concerning future health care infrastructure needs and possible preventive strategies.
Nevertheless, most breast cancer risk factors, including age at first birth, breastfeeding duration, obesity, alcohol use, oral contraceptive use, and hormone replacement therapy, are modifiable. While these are all potentially modifiable, it is unlikely that female reproductive cultures will change to prevent breast cancer, especially when this is balanced with women spending more years in education and entering the job market. Obesity is a more manageable modifiable risk factor. Studies have also indicated that obesity is the most dominant attributable risk factor among Iranian and Korean women27,28. Lifestyle changes also reportedly prevent 25%-30% of breast cancer cases29. Education campaigns regarding lifestyle recommendations are essential for reducing the burden of breast cancer.
Mammography screening may increase in situ breast cancer incidence rate and reduce invasive breast cancer incidence through early detection of breast tumors30,31,32. Mammography screening became widely used during the 1980s, and the coverage rate was estimated to be more than 70% in the United States and Western developed countries or regions33. However, Taiwan had no nationwide mammography screening programs until 200434. The coverage rate was relatively low (only 40.9% of women aged 45–69 years received mammography in 2018)35 compared with the United States and Western developed countries or regions33. The percentage of patients with earlier stages of breast cancer only increased slightly in Taiwan (Supplementary Figure S5). Education campaigns on mammography screening are required to reduce the burden of invasive breast cancer.
A previous study pointed out a substantial birth-cohort effect in breast cancer incidence trend among Taiwanese women36. Similarly, we found a rapid increase from 1997 to 2016 (the birth-cohort born before 1985) and projected that the incidence would reach a plateau in the future (the birth-cohort born after 1985). The APC model is more suitable than other period-based projection models, such as joinpoint regression37, for projecting breast cancer incidence rates in Taiwan. (Supplementary Figure S6 compares the projections of breast cancer age-standardized incidence rate by the APC model and the joinpoint regression model.) Women born after 1985 (with the projected incidence rate reaching a plateau), while they were still young nowadays, will dominate the age-standardized incidence rate of breast cancer in the future (and lead the age-standardized rate to the plateau). The APC model we used in this study takes this into account and can provide advance notice of the age-standardized incidence trend leveling off. Many Asian countries, such as South Korea, Japan, Thailand, India, and China, suffer similar rapid increases in breast cancer incidence due to cohort effects17,38. We recommend these Asian countries (and any other country with an increased breast cancer incidence trend) use our method to make future projections of the incidence rate of breast cancer to see if the trend will continue increasing or level off.
A strength of our study is the use of high-quality population-based data to provide a comprehensive projection of breast cancer incidence rates. However, our study also has limitations. The lack of breast cancer molecular subtypes (estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 status) and cancer stages prevented performing a more refined analysis. The study is ecological, and the inference is susceptible to the ecological fallacy39. Our model assumed that the distribution of risk factors (westernized lifestyles, obesity, reduced fertility, etc.) and public health policy (regarding breast cancer control) do not change over time. We did not consider the scenarios, for example, that the mammography coverage is raised to a level in the future comparable to those of most western countries nowadays. Finally, our APC projection model assumes no interaction between the three temporal factors. For example, if one birth cohort has twice the breast cancer risk as the reference birth cohort, each age group’s risk is twice that of the corresponding age group in the reference birth cohort. The assumption may fail, however.
In conclusion, a rapid increase in breast cancer incidence from 1997 to 2016 is noted. However, the projected age-standardized incidence rate of breast cancer in Taiwan will level off and exhibit a plateau in 2031. In the future, most breast cancer patients will be women aged 55 years and older (postmenopausal breast cancer). Education on lifestyle recommendations and mammography screening is required to reduce the burden of breast cancer incidence.
Data availability
This study uses restricted secondary data and, therefore, we cannot provide the dataset required to recreate our study.
References
WHO. Breast cancer now most common form of cancer: WHO taking action, https://www.who.int/news/item/03-02-2021-breast-cancer-now-most-common-form-of-cancer-who-taking-action (2021).
Chiang, C. J., Wang, Y. W. & Lee, W. C. Taiwan’s Nationwide Cancer Registry System of 40 years: Past, present, and future. J. Formos. Med. Assoc. 118, 856–858. https://doi.org/10.1016/j.jfma.2019.01.012 (2019).
Chiang, C. J. et al. Quality assessment and improvement of nationwide cancer registration system in Taiwan: A review. Jpn. J. Clin. Oncol. 45, 291–296. https://doi.org/10.1093/jjco/hyu211 (2015).
Holford, T. R. Approaches to fitting age-period-cohort models with unequal intervals. Stat. Med. 25, 977–993. https://doi.org/10.1002/sim.2253 (2006).
Su, S. Y., Chiang, C. J., Yang, Y. W. & Lee, W. C. Secular trends in liver cancer incidence from 1997 to 2014 in Taiwan and projection to 2035: An age-period-cohort analysis. J. Formos. Med. Assoc. 118, 444–449. https://doi.org/10.1016/j.jfma.2018.07.001 (2019).
Carstensen, B. Age-period-cohort models for the Lexis diagram. Stat. Med. 26, 3018–3045. https://doi.org/10.1002/sim.2764 (2007).
Møller, B. et al. Prediction of cancer incidence in the Nordic countries: Empirical comparison of different approaches. Stat. Med. 22, 2751–2766. https://doi.org/10.1002/sim.1481 (2003).
Tzeng, I. S. & Lee, W. C. Forecasting hepatocellular carcinoma mortality in Taiwan using an age-period-cohort model. Asia Pac. J. Public Health 27, 65–73. https://doi.org/10.1177/1010539511422941 (2015).
Smittenaar, C. R., Petersen, K. A., Stewart, K. & Moitt, N. Cancer incidence and mortality projections in the UK until 2035. Br. J. Cancer 115, 1147–1155. https://doi.org/10.1038/bjc.2016.304 (2016).
Kontis, V. et al. Future life expectancy in 35 industrialised countries: Projections with a Bayesian model ensemble. Lancet 389, 1323–1335. https://doi.org/10.1016/s0140-6736(16)32381-9 (2017).
Chang, S. R. & Chen, K. H. Age at menarche of three-generation families in Taiwan. Ann. Hum. Biol. 35, 394–405. https://doi.org/10.1080/03014460802154777 (2008).
Interior, M. o. t. Mean age at first birth and fertility rate, https://www.gender.ey.gov.tw/gecdb/Stat_Statistics_DetailData.aspx?sn=lT4902z3YmLGBZadLKLSzQ%3d%3d&d=m9ww9odNZAz2Rc5Ooj%2fwIQ%3d%3d (2020).
Shen, T. Y., Chen, H. J., Pan, W. H. & Yu, T. Secular trends and associated factors of age at natural menopause in Taiwanese women. Menopause 26, 499–505. https://doi.org/10.1097/gme.0000000000001307 (2019).
Bray, F., McCarron, P. & Parkin, D. M. The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res. 6, 229–239. https://doi.org/10.1186/bcr932 (2004).
Rojas, K. & Stuckey, A. Breast cancer epidemiology and risk factors. Clin. Obstet. Gynecol. 59, 651–672. https://doi.org/10.1097/grf.0000000000000239 (2016).
Botha, J. L., Bray, F., Sankila, R. & Parkin, D. M. Breast cancer incidence and mortality trends in 16 European countries. Eur. J. Cancer 39, 1718–1729. https://doi.org/10.1016/s0959-8049(03)00118-7 (2003).
Heer, E. et al. Global burden and trends in premenopausal and postmenopausal breast cancer: A population-based study. Lancet Glob Health 8, e1027–e1037. https://doi.org/10.1016/s2214-109x(20)30215-1 (2020).
Shin, H. R. et al. Recent trends and patterns in breast cancer incidence among Eastern and Southeastern Asian women. Cancer Causes Control 21, 1777–1785. https://doi.org/10.1007/s10552-010-9604-8 (2010).
Anderson, W. F., Chatterjee, N., Ershler, W. B. & Brawley, O. W. Estrogen receptor breast cancer phenotypes in the surveillance, epidemiology, and end results database. Breast Cancer Res. Treat. 76, 27–36. https://doi.org/10.1023/a:1020299707510 (2002).
Vatanasapt, V. et al. Cancer incidence in Thailand, 1988–1991. Cancer Epidemiol. Biomark. Prev. 4, 475–483 (1995).
Fan, L. et al. Breast cancer in a transitional society over 18 years: trends and present status in Shanghai, China. Breast Cancer Res. Treat. 117, 409–416. https://doi.org/10.1007/s10549-008-0303-z (2009).
Velentgas, P. & Daling, J. R. Risk factors for breast cancer in younger women. J. Natl. Cancer Inst. Monogr. 16, 15–24 (1994).
Lahmann, P. H. et al. Body size and breast cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Int. J. Cancer 111, 762–771. https://doi.org/10.1002/ijc.20315 (2004).
Carmichael, A. R. & Bates, T. Obesity and breast cancer: A review of the literature. Breast 13, 85–92. https://doi.org/10.1016/j.breast.2003.03.001 (2004).
Key, T. J. et al. Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. J. Natl. Cancer Inst. 95, 1218–1226. https://doi.org/10.1093/jnci/djg022 (2003).
Yeh, C. J., Chang, H. Y. & Pan, W. H. Time trend of obesity, the metabolic syndrome and related dietary pattern in Taiwan: From NAHSIT 1993–1996 to NAHSIT 2005–2008. Asia Pac. J. Clin. Nutr. 20, 292–300 (2011).
Asadzadeh Vostakolaei, F., Broeders, M. J., Mousavi, S. M., Kiemeney, L. A. & Verbeek, A. L. The effect of demographic and lifestyle changes on the burden of breast cancer in Iranian women: A projection to 2030. Breast 22, 277–281. https://doi.org/10.1016/j.breast.2012.07.002 (2013).
Lee, J. E. et al. Projection of breast cancer burden due to reproductive/lifestyle changes in Korean Women (2013–2030) using an age-period-cohort model. Cancer Res. Treat. 50, 1388–1395. https://doi.org/10.4143/crt.2017.162 (2018).
Dowsett, M. & Folkerd, E. Reduced progesterone levels explain the reduced risk of breast cancer in obese premenopausal women: A new hypothesis. Breast Cancer Res. Treat. 149, 1–4. https://doi.org/10.1007/s10549-014-3211-4 (2015).
Persson, I., Bergström, R., Sparén, P., Thörn, M. & Adami, H. O. Trends in breast cancer incidence in Sweden 1958–1988 by time period and birth cohort. Br. J. Cancer 68, 1247–1253. https://doi.org/10.1038/bjc.1993.513 (1993).
Wun, L. M., Feuer, E. J. & Miller, B. A. Are increases in mammographic screening still a valid explanation for trends in breast cancer incidence in the United States?. Cancer Causes Control 6, 135–144. https://doi.org/10.1007/bf00052774 (1995).
Rostgaard, K., Vaeth, M., Holst, H., Madsen, M. & Lynge, E. Age-period-cohort modelling of breast cancer incidence in the Nordic countries. Stat. Med. 20, 47–61. https://doi.org/10.1002/1097-0258(20010115)20:1%3c47::aid-sim613%3e3.0.co;2-5 (2001).
Li, J. & Shao, Z. Mammography screening in less developed countries. Springerplus 4, 615–615. https://doi.org/10.1186/s40064-015-1394-8 (2015).
Yen, A. M. et al. Population-based breast cancer screening with risk-based and universal mammography screening compared with clinical breast examination: A propensity score analysis of 1 429 890 Taiwanese women. JAMA Oncol. 2, 915–921. https://doi.org/10.1001/jamaoncol.2016.0447 (2016).
Health, Promotion & Administration. https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=591&pid=980 (2020).
Shen, Y. C. et al. Significant difference in the trends of female breast cancer incidence between Taiwanese and Caucasian Americans: Implications from age-period-cohort analysis. Cancer Epidemiol. Biomark. Prev. 14, 1986–1990 (2005).
Kim, H. J., Fay, M. P., Feuer, E. J. & Midthune, D. N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 19, 335–351. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3%3c335::aid-sim336%3e3.0.co;2-z (2000).
Sathishkumar, K. et al. Trends in breast and cervical cancer in India under National Cancer Registry Programme: An age-period-cohort analysis. Cancer Epidemiol. 74, 101982. https://doi.org/10.1016/j.canep.2021.101982 (2021).
Chen, Y. C., Ko, C. I., Lee, W. C. & Lien, W. C. Ecological fallacy in COVID-19 epidemiological inference: Influenza vaccination rate as an example. J. Formos. Med. Assoc. 120, 1655–1656. https://doi.org/10.1016/j.jfma.2021.03.011 (2021).
Acknowledgements
This work is supported by grants from the Health Promotion Administration, the Ministry of Health and Welfare in Taiwan (A1101009; the tobacco control and health care funds), and the Ministry of Science and Technology in Taiwan (MOST 108-2314-B-002-127-MY3; MOST 111-2314-B-002-089-MY3). This study was approved by the Data Release Review Board of the Health Promotion Administration, Ministry of Health and Welfare in Taiwan, which waived the requirement for informed consent. The funders had no role in study design, data collection, and analysis, the decision to publish, or preparation of the manuscript. The content of this research may not represent the opinion of the Health Promotion Administration, Ministry of Health and Welfare.
Author information
Authors and Affiliations
Contributions
In this study, Y.-C.C., J.-R.J., C.-J.C., Y.-W.Y., C.-C.W., L.-J.L., and W.-C.L. collected the data. Y.-C.C., S.-Y.S., and W.-C.L. provided statistical advice on study design and analyzed the data; Y.-C.C. and W.-C.L. drafted the manuscript. All authors contributed substantially to its revision. W.-C.L. takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, YC., Su, SY., Jhuang, JR. et al. Forecast of a future leveling of the incidence trends of female breast cancer in Taiwan: an age-period-cohort analysis. Sci Rep 12, 12481 (2022). https://doi.org/10.1038/s41598-022-16056-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16056-y
This article is cited by
-
Comparing the current short-term cancer incidence prediction models in Brazil with state-of-the-art time-series models
Scientific Reports (2024)
-
Performance measures of 8,169,869 examinations in the National Breast Cancer Screening Program in Taiwan, 2004–2020
BMC Medicine (2023)
-
Incidence trends and spatial distributions of lung adenocarcinoma and squamous cell carcinoma in Taiwan
Scientific Reports (2023)
-
Urban–Rural Disparity in Birth Cohort Effects on Breast Cancer Incidence
Journal of Urban Health (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.