Abstract
Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy and are now the preferred treatment for several tumor types. Though ICIs have shown remarkable efficacy in several cancer histologies, in many cases providing long-term disease control, not all patients will derive clinical benefit from such approaches. Given the lack of a reliable predictive biomarker for therapeutic responses to ICIs, we conducted a retrospective analysis of publicly available genomic data from a large pan-cancer cohort of patients receiving ICI-based immunotherapy. Consistent with previous results, patients in the combined cohort deriving a long-term survival benefit from ICIs were more likely to have a higher tumor mutational burden (TMB). However, this was not uniform across tumor-types, failing to predict for long-term survivorship in most non-melanoma cancers. Interestingly, long-term survivors in most cancers had conserved patterns of mutations affecting several genes. In melanoma, this included mutations affecting TET1 or PTPRD. In patients with colorectal cancer, mutations affecting TET1, RNF43, NCOA3, LATS1, NOTCH3, or CREBBP were also associated with improved prognosis, as were mutations affecting PTPRD, EPHA7, NTRK3, or ZFHX3 in non-small cell lung cancer, RNF43, LATS1, or CREBBP mutations in bladder cancer, and VHL mutations in renal cell carcinoma patients. Thus, this study identified several genes that may have utility as predictive biomarkers for therapeutic responses in patients receiving ICIs. As many have no known relationship to immunotherapy or ICIs, these genes warrant continued exploration, particularly for cancers in which established biomarkers such as PD-L1 expression or TMB have little predictive value.
Similar content being viewed by others
Introduction
Immune checkpoint inhibitors (ICIs) are a cornerstone of cancer therapy and have largely replaced broad-spectrum chemotherapy in several tumor types1. These strategies consist of antibodies directed against negative immune checkpoints including programmed cell death protein 1 (PD-1), PD-1 ligand 1 (PD-L1), and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4). By disrupting the interaction between these molecules and their target proteins, these medications aim to de-restrain the cytotoxic immune program, thereby promoting immune-mediated destruction of tumor cells2. This approach has shown substantial anti-tumor activity in most cancer types, including melanoma, lung, and renal cancers3,4,5,6,7,8,9. Despite these successes, there remain many patients in ICI-sensitive tumors that fail to derive long-term clinical benefit from ICI-based immunotherapy10. As clinical responses can be highly varied even within the same tumor type, there is an increasing interest in identifying new, clinically useful biomarkers to predict for drug responses in patients receiving ICI-based immunotherapy10.
Several potential predictive biomarkers have been suggested, with PD-L1 expression earning FDA approval across several tumor types11. Despite this, PD-L1 status has shown only modest predictive value for ICI responsiveness, and many patients with PD-L1 non-expressing tumors will still show durable clinical benefit in response to ICI-based immunotherapy11,12,13. The FDA has also granted tissue agnostic approval for the PD-1 inhibitor Pembrolizumab for any solid tumor with high microsatellite instability (MSI-H) due to the presumed increase in DNA mismatches and larger tumor antigen pool, though recent estimates suggest that this applies to fewer than 4% of cancer patients14,15,16,17,18,19. Consistent with these observations, total mutational burden (TMB) has also been suggested as a potential means of predicting therapeutic responses across several tumor types20,21. Though TMB has shown promise in this application, TMB is still emerging as a predictive biomarker, and may be insufficient to predict for responses to ICIs alone22,23.
Given the lack of a reliable predictive biomarker, in this study we conducted a retrospective analysis of publicly available genomic data from a large pan-cancer cohort of patients receiving ICI-based immunotherapy. Consistent with previous observations in this cohort, patients with a high TMB demonstrated improved survival across the combined group20. However, we also demonstrate that mutations to select genes with no known relationship to cancer immunotherapy are also strongly associated with a long-term survival benefit, in some cohorts showing a more significant relationship than that between survival and TMB. Hence, several candidate genes identified in this study may have utility as an unrecognized predictive biomarker for drug responses and warrant continued exploration, particularly for cancers in which PD-L1 expression and TMB status demonstrate little predictive value.
Methods
Genomic database analysis
For the discovery cohort, the Sametein et al. patient dataset20 was downloaded and visualized using cBioPortal for Cancer Genomics as described in the original references24,25. Detailed information regarding the dataset, DNA sequencing analyses and protocols can be found in the original reference20. TMB was determined using the MSK-IMPACT assay also as described in the original reference20. Only patients receiving ICI-based immunotherapy were included, and all subsequent genetic analyses were restricted to fully sequenced tumors and gene sequences compared to a reference population as described in our previous studies26,27,28,29. For the melanoma validation cohort, the Van Allen et al., Snyder et al., and the Hugo et al. patient datasets were aggregated and analyzed as described. The non-small cell lung cancer (NSCLC) validation cohort consisted of the Riavi et al. and Hellmann et al. patient datasets, and the renal cell carcinoma (RCC) validation cohort the Miao et al. patient dataset. Additional information regarding these patients as well as26,27,28,29,30 DNA sequencing analyses and protocols can be found in the original references31,32,33,34,35,36. For the non-treated ICI cohort, the Zehir et al. patient dataset was downloaded and evaluated as described above. Additional information regarding this patient cohort, DNA sequencing analyses, and protocols can be found in the original reference37.
Inclusion/exclusion criteria
All genomic analyses were restricted to fully sequenced tumors, and individualized cancer type analysis restricted to cohorts with an N ≥ 30. Analysis was restricted to patients receiving ICI-based immunotherapy in the form of an anti-PD-1, anti-PD-L1, and/or anti-CTLA-4 antibody unless otherwise stated.
Statistical analysis
Patients were separated into groups based on final vital status, and differentially expressed genes were evaluated by an unpaired, non-parametric Mann–Whitney U-test and considered significant at an FDR-adjusted P value of < 0.05. Categorical data were evaluated using the Pearson’s chi-squared test. For time-to-endpoint/survival analyses, data were analyzed using the Kaplan Meier method/log rank test with hazard ratios and considered significant at a P value of < 0.05 as described previously26,27,28,29,30.
Patient and public involvement statement
Neither our patients nor the public were involved in this study.
Guide statement
All methods were carried out in accordance with relevant guidelines and regulations.
Results
Clinical characteristics of patients receiving immune checkpoint inhibitors
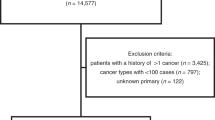
To identify additional prognostic biomarkers in patients receiving ICI-based immunotherapy, we evaluated the publicly available genomic data from the MSKCC pan-cancer cohort of 1661 patients, restricting analysis to patients receiving PD-1, PD-L1, and/or CTLA-4 inhibitors20. Of these 1661 patients, 11 cancer types were represented, including NSCLC (N = 350), melanoma (N = 320), bladder cancer (215), RCC (N = 151), head and neck cancer (N = 139), esophagogastric cancer (N = 126), glioma (N = 117), colorectal cancer (N = 110), cancer of unknown primary (N = 88), breast cancer (N = 44), and non-melanoma skin cancer (N = 1).
We subsequently arranged patients by overall vital status (alive or dead) and compared the clinical characteristics in each group using the Pearson's chi-squared test. In alive and dead groups, there was no statistically significant difference in natal sex or age group (Table S1). Additionally, in both alive and dead groups, all tumor types were similarly represented (Fig. 1A), and there was no significant difference between groups with respect to the immunotherapy regimen used (Fig. 1B). The immunotherapy approach used was closely related to tumor type, with the majority of patients receiving anti-CTLA-4 antibodies being treated for melanoma, with similar results observed in the combination (anti-PD-L1/PD-1 and anti-CTLA-4) group. Patients receiving anti-PD-L1/PD-1 were more diverse with all tumor types represented, though this group contained the majority of lung cancer patients (Fig. 1C). When arranged by the Kaplan Meier method, patients with melanoma and RCC had longer median overall survival when compared to all other cancers (Fig. 1D), and patients receiving anti-PD-L1 or anti-PD-1 had shorter overall survival when compared to those receiving anti-CTLA-4 or a combination regimen (Fig. 1E), likely attributed to the different cancer types represented within these groups.
Clinical characteristics of patients receiving immune checkpoint inhibitors. (A) The Samstein et al. MSKCC pan-cancer cohort of 1661 patients receiving PD-1, PD-L1, and/or CTLA-4 inhibiting antibodies were arranged by vital status, and the tumor types represented in each group displayed by percent. (B) The percent of patients in each group receiving anti-PD-1/PD-L1 antibodies (N = 1307), anti-CTLA-4 antibodies (N = 99), or a combination of both (N = 255). (C) The percent of each tumor type arranged by treatment group. (D, E) Kaplan Meier plot showing overall survival for patients arranged by either cancer type or treatment group.
Mutations to genes associated with improved overall survival in the pan-cancer cohort
Using the described genomic data, we next evaluated the mutational profiles of patients in this study as arranged by vital status (alive or dead) using an unpaired, non-parametric Mann–Whitney U-test. This approach revealed several differentially mutated genes that were overrepresented in the alive group (Fig. 2A, B), with the 13 most significant (by FDR-adjusted P value) being TET1, RNF43, PTPRD, NCOA3, EPHA7, NTRK3, ZFHX3, LATS1, NOTCH3, CREBBP, KMT2A, RET, and VHL (Fig. 2C). The presence of a mutation to one of more of these genes was slightly more common in males compared to females, and these patients also had a marginal but statistically significant increase in median age (Table S2). The most frequent type of mutation in all genes was a missense mutation, many with presumed loss of function, though several other mutations were observed (Table S3). Patients with a mutation to one or more of these genes had a highly significant improvement in overall survival when compared to the non-mutated group (Fig. 2D), as well as an increase in the number of total mutations (Fig. 2E). Despite these differences, all 10 cancer types were represented in each group, though the non-mutated group had an increased frequency of RCC and NSCLC (Fig. 2F). Additionally, in the MSKCC pan-cancer cohort of 10,336 patients, the overwhelming majority of whom have not received ICI-based immunotherapy, there was no significant association between mutation to any of these genes and time-to-endpoint survival outcomes, with the exception of VHL which was associated with improved overall survival (Table S4). This was presumably because VHL mutations were observed almost exclusively in RCC tumors, which carry a better prognosis than other cancers included in this cohort. However, when restricting analysis to the 187 RCC patients in this cohort with clinical outcomes, there was no significant association between VHL mutation and clinical outcome (P = 0.258, 73 VHL-mutated and 114 VHL-non-mutated patients).
Mutations to genes associated with improved overall survival in the pan-cancer cohort. (A, B) Patients from the MSKCC pan-cancer cohort (N = 1661) were arranged by final vital status, and differentially mutated genes were arranged by volcano and scatter plot with those significantly different between the two groups shown in blue. (C) The 13 most differentially mutated genes are presented by percent mutated in each group, and shown with the corresponding false discovery rate (FDR)-adjusted P value. (D) Kaplan Meier plot showing overall survival for patients with or without a mutation in one or more of these 13 genes. (N = 1661 consisting of 610 patients with one or more mutation and 1051 non-mutated patients). (E, F) The total number of mutations and tumor types represented in patients with or without a mutation in one or more of these genes.
TET1 mutations are associated with improved outcomes in colorectal cancer and melanoma patients receiving immune checkpoint inhibitors
To better explore the prognostic relevance of mutations to these genes, we first evaluated the survival for all patients arranged by TMB, to date the best prognostic factor established in this cohort20. Consistent with prior observations20, patients with a high (above the median) TMB had a significant survival benefit when compared to those with a low (below the median) TMB (Fig. 3A). TET1 mutation was also strongly associated with improved survival across all patients, and TET1-mutated patients displayed a relative increase in TMB compared to TET1-non-mutated patients (Fig. 3B). As TET1 mutations were most common in colorectal cancer, bladder cancer, and melanoma patients (Fig. 3C), we subsequently evaluated the relationship between TET1 mutation and overall survival in these cancers specifically. Interestingly, TET1 was a highly significant predictor of improved survival in colorectal cancer and melanoma patients (Fig. 3D, E), though there was no relationship between TET1 mutation and survival in bladder cancer (P = 0.209). While TET1 mutation was associated with an increase in total mutational burden in colon cancer and melanoma patients (Fig. 3F,G), the relationship between total mutational burden and survival did not reach statistical significance in this cohort of colorectal cancer patients (Fig. 3H), though it remained a significant prognostic factor in the melanoma cohort (Fig. 3I).
TET1 mutations are associated with improved outcomes in colorectal cancer and melanoma patients receiving immune checkpoint inhibitors. (A) Kaplan Meier plot showing overall survival for the pan-cancer cohort (N = 1661) for patients with either a high (above median) or low (below median) tumor mutational burden (TMB). (B) Overall survival and the total number of mutations for all patients arranged by TET1 mutation status (58 TET1-mutated and 1603 TET1-non-mutated patients) (C) The percent of TET1-mutated patients arranged by tumor type. (D–G) Overall survival and the total number of mutations for patients from the colorectal cancer (N = 110, 7 TET1-mutated and 103 TET1-non-mutated patients) or melanoma (N = 320, 18 TET1-mutated and 302 TET1-non-mutated patients) cohorts arranged by TET1 mutation status. (H, I) Overall survival for the colorectal cancer and melanoma cohorts arranged by TMB.
RNF43 mutations are associated with improved survival in colorectal and bladder cancer cohorts
Given the relationship between TET1 and clinical outcome, we next conducted a similar analysis using RNF43, the gene with the second strongest association with vital status in the pan-cancer cohort. Consistent with these observations, RNF43 mutation was associated with improved survival across all patients using the Kaplan Meier method (Fig. 4A). RNF43 mutation was most common in colorectal cancers, followed by esophagogastric and bladder cancers (Fig. 4B). RNF43 mutations were strongly associated with improved overall survival in the colorectal and bladder cancer cohorts (Fig. 4C, D), surpassing the relationship between survival and total mutational burden in these patients (Fig. S1A). However, there was no significant relationship between RNF43 mutation and overall survival in esophagogastric cancer patients (P = 0.504).
RNF43 mutations are associated with improved survival in colorectal and bladder cancer patients receiving immune checkpoint inhibitors. (A) Kaplan Meier plot showing overall survival for the pan-cancer cohort (N = 1661) arranged by RNF43 mutation status (61 RNF43-mutated and 1600 RNF43-non-mutated patients). (B) The percent of RNF43-mutated patients arranged by tumor type. (C, D) Overall survival for the colorectal (N = 110, 22 RNF43-mutated and 88 RNF43-non-mutated patients) and bladder cancer (N = 215, 9 RNF43-mutated and 206 RNF43-non-mutated patients) cohorts arranged by RNF43 mutation status.
PTPRD mutations are associated with improved survival in melanoma and lung cancer cohorts
Continuing our analysis, PTPRD mutation status was also associated with improved overall survival in the pan-cancer cohort using the Kaplan Meier method (Fig. 5A). PTPRD mutations were most common in melanoma and NSCLC patients, followed distantly by colorectal cancer, cancers of unknown primary origin, esophagogastric cancer, bladder cancer, and HNSCC (Fig. 5B). PTPRD mutation was modestly associated with overall survival in melanoma and NSCLC cohorts (Fig. 5C, D), though this relationship was more significant than that between total mutational burden and overall survival (Fig. S1B). As TET1 and PTPRD mutations were the only significant predictors of outcomes in the melanoma discovery cohort, we next explored their prognostic utility in a valuation cohort consisting of melanoma patients from three independent immunogenomic studies all receiving ICIs (N = 212). In this group, 23% of patients had a mutation in either gene, and as previously, TET1- or PTPRD-mutated patients had a highly significant improvement in overall survival compared to non-mutated patients, as well as a modest increase in TMB (Fig. S2).
PTPRD mutations are associated with improved survival in melanoma and lung cancer patients receiving immune checkpoint inhibitors. (A) Kaplan Meier plot showing overall survival for the pan-cancer cohort (N = 1661) arranged by PTPRD mutation status (148 PTPRD-mutated and 1513 PTPRD-non-mutated patients). (B) The percent of PTPRD-mutated patients arranged by tumor type. (C, D) Overall survival for the melanoma (N = 320, 63 PTPRD-mutated and 257 PTPRD-non-mutated patients) and non-small cell lung cancer (NSCLC) (N = 350, 43 PTPRD-mutated and 307 PTPRD-non-mutated patients) cohorts arranged by PTPRD mutation status.
NCOA3 and NOTCH3 mutations are associated with improved survival in colorectal cancer patients
As previously, we next evaluated the prognostic relevance of NCOA3 in the combined cohort using the Kaplan Meier method. Though NCOA3 mutations were a favorable prognostic factor in the combined cohort (Fig. 6A), NCOA3 mutations were predominant in colorectal cancer patients, followed by melanoma and bladder cancer patients (Fig. 6B). We subsequently evaluated the relationship between NCOA3 mutation and survival in these cohorts and found that NCOA3 mutation was associated with improved survival only in colorectal cancer, though this bordered on the threshold for statistical significance (Fig. 6C). We conducted a similar analysis using NOTCH3, which also was associated with improved survival in the pan-cancer cohort (Fig. 6D). NOTCH3 mutation was also most frequent in colorectal cancers, followed by melanoma (Fig. 6E). However, NOTCH3 mutation was only associated with improved survival in the colorectal cancer group, though unlike NCOA3, this relationship was highly significant (Fig. 6F).
NCOA3 and NOTCH3 mutations are associated with improved survival in colorectal cancer patients receiving immune checkpoint inhibitors. (A) Kaplan Meier plot showing overall survival for the pan-cancer cohort (N = 1661) arranged by NCOA3 mutation status (33 NCOA3-mutated and 1369 NCOA3-non-mutated patients. An additional 259 NCOA3-unprofiled patients were excluded from analysis). (B) The percent of NCOA3-mutated patients arranged by tumor type. (C) Overall survival for the colorectal cancer cohort arranged by NCOA3 mutation status (N = 110, 8 NCOA3-mutated, 102 NCOA3-non-mutated patients). (D) Kaplan Meier plot showing overall survival for the combined pan-cancer cohort arranged by NOTCH3 mutation status (96 NOTCH3-mutated and 1565 NOTCH3-non-mutated patients). (E) The percent of NOTCH3-mutated patients arranged by tumor type. (F) Overall survival for the colorectal cancer cohort arranged by NOTCH3 mutation status (16 NOTCH3-mutated and 94 NOTCH3-non-mutated patients).
EPHA7, NTRK3, and ZFHX3 mutations are associated with improved survival in lung cancer patients
We next evaluated the relationship between overall survival and mutations to the next three genes identified, specifically EPHA7, NTRK3, and ZFHX3. Though EPHA7 mutation was associated with improved survival in the combined cohort (Fig. 7A), EPHA7 mutations were by far most frequent in melanoma patients, followed distantly by NSCLC and colorectal cancer patients (Fig. 7B). However, despite these observations, only EPHA7 mutations had a statistically significant relationship with overall survival in NSCLC patients (Fig. 7C), failing to achieve statistical significance in any other cancer type. We observed similar results with respect to NTRK3, as NTRK3 mutation was also associated with improved overall survival in the combined cohort (Fig. 7D), and was most frequent in melanoma patients, followed by cancers of unknown primary and NSCLC (Fig. 7E). However, NTRK3 mutations only had a significant relationship with survival in NSCLC (Fig. 7F).
EPHA7, NTRK3, and ZFHX3 mutations are associated with improved survival in lung cancer patients receiving immune checkpoint inhibitors. (A) Kaplan Meier plot showing overall survival for the pan-cancer cohort (N = 1661) arranged by EPHA7 mutation status (86 EPHA7-mutated and 1316 EPHA7-non-mutated patients. An additional 259 EPHA7-unprofiled patients were excluded from analysis). (B) The percent of EPHA7-mutated patients arranged by tumor type. (C) Overall survival for the non-small cell lung cancer (NSCLC) cohort arranged by EPHA7 mutation status (N = 350, 18 EPHA7-mutated and 265 EPHA7-non-mutated patients. An additional 67 EPHA7-unprofiled patients were excluded from analysis). (D) Kaplan Meier plot showing overall survival for the combined pan-cancer cohort arranged by NTRK3 mutation status (76 NTRK3-mutated and 1585 NTRK3-non-mutated patients). (E) The percent of NTRK3-mutated patients arranged by tumor type. (F) Kaplan Meier plot showing overall survival for the NSCLC cohort arranged by NTRK3 mutation status (20 NTRK3-mutated and 330 NTRK3-non-mutated patients). (G) Kaplan Meier plot showing overall survival for the pan-cancer cohort arranged by ZFHX3 mutation status (118 ZFHX3-mutated and 1284 ZFHX3-non-mutated patients. An additional 259 ZFHX3-unprofiled patients were excluded from analysis). (H) The percent of ZFHX3-mutated patients arranged by tumor type. (I) Overall survival for the NSCLC cohort arranged by ZFHX3 mutation status (27 ZFHX3-mutated and 256 ZFHX3-non-mutated patients. An additional 67 ZFHX3-unprofiled patients were excluded from analysis).
ZFHX3 mutations were also associated with a significant survival benefit across all patients (Fig. 7G), and were most common in colorectal cancer patients, followed by bladder cancer, melanoma, and NSCLC patients (Fig. 7H). However, as previously, ZFHX3 mutation was only a significant prognostic factor in NSCLC patients (Fig. 7I). As EPHA7, NTRK3, ZFHX3, and PTPRD mutations were all associated with improved outcomes in NSCLC patients in the discovery cohort, we next explored whether this relationship was also observed in a validation cohort consisting of 91 NSCLC patients also receiving ICIs. As observed in the discovery cohort, patients with a mutation in one or more of these genes had significantly longer progression-free survival compared to non-mutated patients (Fig. S3). Though overall survival data was not available, mutated patients also had a modest increase in TMB, consistent with observations from the discovery cohort (Fig. S3).
LATS1, CREBBP, and VHL mutations are associated with improved survival in urologic malignancies
Finally, we explored the prognostic relevance of the remaining genes identified in our analysis. While KMT2A and RET mutations were associated with favorable overall survival in the combined cohort, there was no relationship between either KMT2A or RET mutation and survival in any individual cancer type (Fig. S4A–D). LATS1 mutations were also strongly associated with improved survival in all patients (Fig. 8A) and were observed with similar frequency in several cancers including bladder cancer, colorectal cancer, cancers of unknown primary, esophagogastric cancer, melanoma, and others (Fig. 8B), though LATS1 mutations were only associated with improved survival in bladder cancer and colorectal cancer patients (Figs. 8C and S5A). Similarly, CREBBP mutations were a positive prognostic factor in the combined cohort (Fig. 8D), and were most common in colorectal and bladder cancer patients (Fig. 8E). Accordingly, CREBBP mutations were strongly associated with improved survival in both bladder and colorectal cohorts (Figs. 8F and S5B). Though VHL mutations were also associated with improved overall survival in the combined cohort (Fig. 8G), VHL mutations were almost exclusive to RCC patients (Fig. 8H). Accordingly, in the RCC cohort, patients with a VHL mutation demonstrated a significant survival benefit compared to non-VHL-mutated patients (Fig. 8I), exceeding the predictive value of tumor mutational burden (Fig. S6).
LATS1, CREBBP, and VHL mutations are associated with improved survival in urologic malignancies. (A) Kaplan Meier plot showing overall survival for the pan-cancer cohort (N = 1661) arranged by LATS1 mutation status (48 LATS1-mutated and 1613 LATS1-non-mutated patients). (B) The percent of LATS1-mutated patients arranged by tumor type. (C) Kaplan Meier plot showing overall survival for the bladder cancer cohort arranged by LATS1 mutation status (N = 215, 11 LATS1-mutated and 204 LATS1-non-mutated patients). (D) Kaplan Meier plot showing overall survival for the combined pan-cancer cohort method arranged by CREBBP mutation status (108 CREBBP-mutated and 1553 CREBBP-non-mutated patients). (E) The percent of CREBBP-mutated patients arranged by tumor type. (F) Kaplan Meier plot showing overall survival for the bladder cancer cohort arranged by CREBBP mutation status (31 CREBBP-mutated and 184 CREBBP-non-mutated patients). (G) Kaplan Meier plot showing overall survival for the pan-cancer cohort arranged by VHL mutation status (111 VHL-mutated and 1550 VHL-non-mutated patients). (H) The percent of VHL-mutated patients arranged by tumor type. (I) Kaplan Meier plot showing overall survival for the renal cell carcinoma cohort arranged by VHL mutation status (N = 151, 106 VHL-mutated and 45 VHL-non-mutated patients).
We subsequently explored the relationship between VHL mutation and clinical outcomes in an independent validation cohort consisting of 35 clear cell RCC (ccRCC) patients also receiving ICIs. Though survival data was not available, VHL-mutated patients were more likely to derive clinical benefit from ICIs. In addition to being the only group with complete responses, 72% of VHL-mutated patients had at least an intermediate benefit from treatment compared to only 40% of non-mutated patients (Fig. S7).
Discussion
ICIs have revolutionized cancer therapy in the past decade, and are now the preferred first-line treatment for several tumor types1. Though select patients will derive long-term clinical benefit from immune checkpoint inhibitors either as a monotherapy or in combination with other treatments, others will fail to show therapeutic responses or demonstrate only a transient response38. Hence, there is a clear need for novel, predictive biomarkers to identify the patients most likely to benefit from ICI-based immunotherapy, particularly given their often severe immune-mediated adverse effects39. As mentioned, patients with MSI-H tumors often show favorable response to ICIs, yet this is only relevant to a small fraction of cancer patients14,15,16,17,18,19. Additionally, while PD-L1 expression can be informative when predicting for responses to select ICIs such as Pembrolizumab, recent evidence suggests that PD-L1 status alone is not sufficient as a predictive biomarker and should be complemented by other clinical findings11. TMB is emerging as an important consideration in cancer immunotherapy, predicting for responses in a wide range of cancer types20,21. However, this is rather controversial, with other recent studies suggesting that, like PD-L1 status, TMB may have limited utility alone22,23.
In this study, we evaluated genomic data from a large pan-cancer cohort initially used to support the predictive value of TMB in patients receiving ICI-based immunotherapy. Consistent with the authors’ initial findings20, patients with a high TMB demonstrated a long-term survival benefit compared to those with a lower TMB. However, when retrospectively comparing mutation data from patients arranged by vital status at the study endpoint, we identified several genes that were differentially mutated in patients who derived a long-term clinical benefit from ICIs. Additionally, when restricting our analysis to patients with the same tumor types, though TMB failed to predict for long-term survivorship in many cohorts including colorectal cancer, several of these newly identified genes were strongly associated with improved outcomes.
For example, TET1 is a DNA demethylase belonging to the ten-eleven translocation family40. In the present study, we identified TET1 mutation as a significant, positive predictor of outcomes in the combined cohort. Though TET1 mutations were observed across a wide range of different cancers, TET1 mutations were most strongly associated with improved responses to ICI-based immunotherapy in colorectal and melanoma patients, and in the case of colorectal cancer, exceeded the predictive value of TMB. This appears consistent with prior observations suggesting that TET1 mutation may have utility as a predictive biomarker for ICIs. Recently, another study exploring predictors of therapeutic responses to ICIs in the Cancer Genome Atlas (TCGA) dataset also identified TET1 mutation as a positive prognostic biomarker across the combined group. In the combined TCGA cohort, the authors reported that patients with a TET1 mutation had a higher TMB, as observed in our study, as well as an increased neoantigen pool and an inflamed pattern of tumor-infiltrating immune signatures41. As our study also supports TET1 mutation as a potential predictive biomarker, particularly for colorectal and melanoma patients, this warrants continued clinical investigation.
In addition to TET1, our study also identified mutations affecting the E3 ubiquitin-protein ligase RNF43 as a potential predictor of therapeutic responses, notably for colorectal and bladder cancer patients. Classically, RNF43 functions as a negative regulator of oncogenic WNT/β-Catenin signaling and is considered a tumor suppressor gene42. However, several studies now also support an important immunomodulatory role for RNF43. For example, in a transgenic mouse model of early pancreatic ductal adenocarcinoma (PDAC), the loss of RNF43 accelerated the formation of high-grade cystic lesions and led to extensive immune remodeling in the form of decreased macrophage infiltration, increased T- and B-cell infiltration, and enhanced expression of immune checkpoints. Further, these mice also appeared to derive benefit from CTLA-4 inhibition, with 2/6 showing a radiographic response and 4/6 showing stable disease43. Similar to our observations, RNF43 mutations were associated with improved survival in colorectal cancer patients receiving ICIs in the TCGA cohort44. This is consistent with prior observations, also in colon cancer, where RNF43 was identified as a tumor-associated antigen that can elicit tumor-reactive cytotoxic T-cell responses45. Accordingly, RNF43 peptide-based therapeutic vaccines are now under investigation in combination with chemo- or immunotherapy in a variety of solid tumors46,47,48, and RNF43 mutation status may also warrant exploration as a predictive biomarker.
In addition to TET1 and RNF43, our study also identified an association between NCOA3, CREBBP, and NOTCH3 mutations and improved survival in colorectal cancer patients. This is consistent with studies reporting a positive predictive role for NCOA3 mutations in a multi-cancer cohort49, as well as CREBBP and NOTCH3 mutations in the TCGA colorectal cohort44. Our study has also identified several additional candidate biomarkers in other tumor types, including PTPRD for melanoma and NSCLC patients. PTPRD is a tumor suppressor gene with important roles in regulating JAK/STAT signaling50,51. Though little is known regarding PTPRD mutation and drug responses in melanoma, previous observations support PTPRD mutations (or those to the functionally related gene PTPRT) as a positive predictor of outcomes in NSCLC patients receiving ICIs in a pooled cohort from three publicly available datasets as well as the TCGA cohort of NSCLC patients52. Our study additionally identified a similar role for EPHA7 and ZFHX3 mutations in NSCLC, consistent with prior observations from a large pan-cancer cohort49,53.
Though there is limited data supporting mutations to the genes described above as potentially useful biomarkers, our study identified several other candidate genes that have yet to be suggested in this application. While NTRK3 mutations have yet to be linked to response to ICIs, there is early evidence that NTRK3-mutated bladder cancers are more immunogenic, with increased TMB and enhanced immune infiltration compared to non-mutated tumors54. Similarly, while our study determined that LATS1 mutations were also associated with a survival benefit in the combined, bladder, and colorectal cancer cohorts, very little is known regarding LATS1 mutations and ICI responses. However, Lats1/2 deletion led to regression of three murine syngeneic tumor models. Further, this required the adaptive immune system, and Lats1/2 deficiency enhanced the efficacy of tumor vaccines in vivo55. Similarly, though RET is not a known biomarker in immune oncology, RET does appear to have central roles in directing the tumor microenvironment, promoting cancer-associated inflammation, and suppressing anti-tumor immune responses56. Hence, loss of function mutations to genes such as LATS1 or RET may lead to considerable immune reprogramming, explaining the improved outcomes in patients receiving ICIs in this study.
Finally, our study identified a highly significant association between VHL mutation and improved survival in RCC patients. VHL is a tumor suppressor gene often mutated in ccRCC patients57. At the present time, VHL mutations are not known to confer increased sensitivity to ICIs in RCC patients. However, VHL mutations confer increased sensitivity to natural killer cell-mediated killing of RCC cells in vitro58, with similar observations in RCC patients59. Hence, as ICIs are a cornerstone in the treatment of RCC60, this observation warrants investigation. This can be said for the several candidate genes identified in this study, many of which may have utility as unrecognized biomarkers for drug responses in patients receiving ICIs. However, it is important to recognize the inherent limitation of public database analyses. For example, though these data are compelling, these patient datasets do not fully account for additional factors including demographic data, cancer stage, line of treatment, comorbidity profile, performance status, and others. Hence, these should be included in future prospective analyses before any of these candidate biomarkers are used to guide clinical decision making. Similarly, though several mutations identified presumably confer loss of function, others are of unknown significance. Hence, this too warrants exploration in a laboratory setting. However, given the highly varied responses in patients receiving these medications, these and other biomarkers warrant continued exploration, particularly for cancers in which better-established methods such as PD-L1 expression and TMB fail to reliably predict for patients most likely to derive clinical benefit from ICI-based immunotherapy.
Data availability
The datasets analyzed in the current study are publicly available and can be found at www.cBioPortal.org.
References
Robert, C. A decade of immune-checkpoint inhibitors in cancer therapy. Nat. Commun. 11, 3801. https://doi.org/10.1038/s41467-020-17670-y (2020).
Wei, S. C., Duffy, C. R. & Allison, J. P. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 8, 1069–1086. https://doi.org/10.1158/2159-8290.CD-18-0367 (2018).
Hodi, F. S. et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 363, 711–723. https://doi.org/10.1056/NEJMoa1003466 (2010).
Robert, C. et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N. Engl. J. Med. 364, 2517–2526. https://doi.org/10.1056/NEJMoa1104621 (2011).
Borghaei, H. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N. Engl. J. Med. 373, 1627–1639. https://doi.org/10.1056/NEJMoa1507643 (2015).
Garon, E. B. et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N. Engl. J. Med. 372, 2018–2028. https://doi.org/10.1056/NEJMoa1501824 (2015).
Larkin, J. et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med. 373, 23–34. https://doi.org/10.1056/NEJMoa1504030 (2015).
Gibney, G. T., Weiner, L. M. & Atkins, M. B. Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol. 17, e542–e551. https://doi.org/10.1016/S1470-2045(16)30406-5 (2016).
Darvin, P., Toor, S. M., Sasidharan Nair, V. & Elkord, E. Immune checkpoint inhibitors: recent progress and potential biomarkers. Exp. Mol. Med. 50, 1–11. https://doi.org/10.1038/s12276-018-0191-1 (2018).
Fares, C. M., Allen, E. M. V., Drake, C. G., Allison, J. P. & Hu-Lieskovan, S. Mechanisms of resistance to immune checkpoint blockade: Why does checkpoint inhibitor immunotherapy not work for all patients?. Am. Soc. Clin. Oncol. Educ. Book https://doi.org/10.1200/edbk_240837 (2019).
Davis, A. A. & Patel, V. G. The role of PD-L1 expression as a predictive biomarker: an analysis of all US Food and Drug Administration (FDA) approvals of immune checkpoint inhibitors. J. Immunother. Cancer 7, 278. https://doi.org/10.1186/s40425-019-0768-9 (2019).
Doroshow, D. B. et al. PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat. Rev. Clin. Oncol. 18, 345–362. https://doi.org/10.1038/s41571-021-00473-5 (2021).
Wallis, C. J. D. et al. Association between PD-L1 status and immune checkpoint inhibitor response in advanced malignancies: A systematic review and meta-analysis of overall survival data. Jpn. J. Clin. Oncol. 50, 800–809. https://doi.org/10.1093/jjco/hyaa021 (2020).
Marcus, L., Lemery, S. J., Keegan, P. & Pazdur, R. FDA approval summary: Pembrolizumab for the treatment of microsatellite instability-high solid tumors. Clin. Cancer Res. 25, 3753–3758. https://doi.org/10.1158/1078-0432.CCR-18-4070 (2019).
Marabelle, A. et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient cancer: results from the phase II KEYNOTE-158 study. J. Clin. Oncol. 38, 1–10. https://doi.org/10.1200/JCO.19.02105 (2020).
Le, D. T. et al. Phase II open-label study of pembrolizumab in treatment-refractory, microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: KEYNOTE-164. J. Clin. Oncol. 38, 11–19. https://doi.org/10.1200/JCO.19.02107 (2020).
Andre, T. et al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N. Engl. J. Med. 383, 2207–2218. https://doi.org/10.1056/NEJMoa2017699 (2020).
Boyiadzis, M. M. et al. Significance and implications of FDA approval of pembrolizumab for biomarker-defined disease. J. Immunother. Cancer 6, 35. https://doi.org/10.1186/s40425-018-0342-x (2018).
Bonneville, R. et al. Landscape of microsatellite instability across 39 cancer types. JCO Precis. Oncol. https://doi.org/10.1200/PO.17.00073 (2017).
Samstein, R. M. et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat. Genet. 51, 202–206. https://doi.org/10.1038/s41588-018-0312-8 (2019).
Marabelle, A. et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 21, 1353–1365. https://doi.org/10.1016/S1470-2045(20)30445-9 (2020).
Maleki Vareki, S. High and low mutational burden tumors versus immunologically hot and cold tumors and response to immune checkpoint inhibitors. J. Immunother. Cancer 6, 157. https://doi.org/10.1186/s40425-018-0479-7 (2018).
Strickler, J. H., Hanks, B. A. & Khasraw, M. Tumor mutational burden as a predictor of immunotherapy response: Is more always better?. Clin. Cancer Res. 27, 1236–1241. https://doi.org/10.1158/1078-0432.CCR-20-3054 (2021).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. https://doi.org/10.1126/scisignal.2004088 (2013).
Cerami, E. et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404. https://doi.org/10.1158/2159-8290.CD-12-0095 (2012).
Principe, D. R., Narbutis, M., Koch, R. & Rana, A. Frequency and prognostic value of mutations associated with the homologous recombination DNA repair pathway in a large pan cancer cohort. Sci. Rep. 10, 20223. https://doi.org/10.1038/s41598-020-76975-6 (2020).
Principe, D. R. et al. Long-term gemcitabine treatment reshapes the pancreatic tumor microenvironment and sensitizes murine carcinoma to combination immunotherapy. Cancer Res. 80, 3101–3115. https://doi.org/10.1158/0008-5472.CAN-19-2959 (2020).
Principe, D. R. et al. Loss of SMAD4 is associated with poor tumor immunogenicity and reduced PD-L1 expression in pancreatic cancer. Front. Oncol. 12, 806963. https://doi.org/10.3389/fonc.2022.806963 (2022).
Principe, D. R. et al. XP-524 is a dual-BET/EP300 inhibitor that represses oncogenic KRAS and potentiates immune checkpoint inhibition in pancreatic cancer. Proc. Natl. Acad. Sci. U. S. A. https://doi.org/10.1073/pnas.2116764119 (2022).
Principe, D. R. et al. Calcium channel blockers potentiate gemcitabine chemotherapy in pancreatic cancer. Proc. Natl. Acad. Sci. U. S. A. 119, e2200143119. https://doi.org/10.1073/pnas.2200143119 (2022).
Snyder, A. et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N. Engl. J. Med. 371, 2189–2199. https://doi.org/10.1056/NEJMoa1406498 (2014).
Van Allen, E. M. et al. Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science 350, 207–211. https://doi.org/10.1126/science.aad0095 (2015).
Hugo, W. et al. Genomic and transcriptomic features of response to anti-PD-1 therapy in metastatic melanoma. Cell 165, 35–44. https://doi.org/10.1016/j.cell.2016.02.065 (2016).
Hellmann, M. D. et al. Genomic features of response to combination immunotherapy in patients with advanced non-small-cell lung cancer. Cancer Cell 33, 843–852. https://doi.org/10.1016/j.ccell.2018.03.018 (2018).
Rizvi, N. A. et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 348, 124–128. https://doi.org/10.1126/science.aaa1348 (2015).
Miao, D. et al. Genomic correlates of response to immune checkpoint therapies in clear cell renal cell carcinoma. Science 359, 801–806. https://doi.org/10.1126/science.aan5951 (2018).
Zehir, A. et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat. Med. 23, 703–713. https://doi.org/10.1038/nm.4333 (2017).
Jenkins, R. W., Barbie, D. A. & Flaherty, K. T. Mechanisms of resistance to immune checkpoint inhibitors. Br. J. Cancer 118, 9–16. https://doi.org/10.1038/bjc.2017.434 (2018).
Martins, F. et al. Adverse effects of immune-checkpoint inhibitors: Epidemiology, management and surveillance. Nat. Rev. Clin. Oncol. 16, 563–580. https://doi.org/10.1038/s41571-019-0218-0 (2019).
Tahiliani, M. et al. Conversion of 5-methylcytosine to 5-hydroxymethylcytosine in mammalian DNA by MLL partner TET1. Science 324, 930–935. https://doi.org/10.1126/science.1170116 (2009).
Wu, H. X. et al. Alteration in TET1 as potential biomarker for immune checkpoint blockade in multiple cancers. J. Immunother. Cancer 7, 264. https://doi.org/10.1186/s40425-019-0737-3 (2019).
Jiang, X. et al. Inactivating mutations of RNF43 confer Wnt dependency in pancreatic ductal adenocarcinoma. Proc. Natl. Acad. Sci. U. S. A. 110, 12649–12654. https://doi.org/10.1073/pnas.1307218110 (2013).
Hosein, A. N. et al. Loss of Rnf43 accelerates Kras-mediated neoplasia and remodels the tumor immune microenvironment in pancreatic adenocarcinoma. Gastroenterology https://doi.org/10.1053/j.gastro.2021.12.273 (2021).
Lin, A. et al. Age, sex, and specific gene mutations affect the effects of immune checkpoint inhibitors in colorectal cancer. Pharmacol. Res. 159, 105028. https://doi.org/10.1016/j.phrs.2020.105028 (2020).
Uchida, N. et al. Ring finger protein 43 as a new target for cancer immunotherapy. Clin. Cancer Res. 10, 8577–8586. https://doi.org/10.1158/1078-0432.CCR-04-0104 (2004).
Cotton, A. D., Nguyen, D. P., Gramespacher, J. A., Seiple, I. B. & Wells, J. A. Development of antibody-based PROTACs for the degradation of the cell-surface immune checkpoint protein PD-L1. J. Am. Chem. Soc. 143, 593–598. https://doi.org/10.1021/jacs.0c10008 (2021).
Kawamura, J. et al. Cytotoxic T lymphocyte response to peptide vaccination predicts survival in stage III colorectal cancer. Cancer Sci. 109, 1545–1551. https://doi.org/10.1111/cas.13547 (2018).
Hijikata, Y. et al. A phase I clinical trial of RNF43 peptide-related immune cell therapy combined with low-dose cyclophosphamide in patients with advanced solid tumors. PLoS ONE 13, e0187878. https://doi.org/10.1371/journal.pone.0187878 (2018).
Zhang, Z. et al. EPHA7 mutation as a predictive biomarker for immune checkpoint inhibitors in multiple cancers. BMC Med. 19, 26. https://doi.org/10.1186/s12916-020-01899-x (2021).
Veeriah, S. et al. The tyrosine phosphatase PTPRD is a tumor suppressor that is frequently inactivated and mutated in glioblastoma and other human cancers. Proc. Natl. Acad. Sci. U. S. A. 106, 9435–9440. https://doi.org/10.1073/pnas.0900571106 (2009).
Ortiz, B. et al. Loss of the tyrosine phosphatase PTPRD leads to aberrant STAT3 activation and promotes gliomagenesis. Proc. Natl. Acad. Sci. U. S. A. 111, 8149–8154. https://doi.org/10.1073/pnas.1401952111 (2014).
Wang, X. et al. Association of PTPRD/PTPRT mutation with better clinical outcomes in NSCLC patients treated with immune checkpoint blockades. Front. Oncol. 11, 650122. https://doi.org/10.3389/fonc.2021.650122 (2021).
Zhang, J. et al. ZFHX3 mutation as a protective biomarker for immune checkpoint blockade in non-small cell lung cancer. Cancer Immunol. Immunother. 70, 137–151. https://doi.org/10.1007/s00262-020-02668-8 (2021).
Zhang, Z. et al. Identification of NTRK3 as a potential prognostic biomarker associated with tumor mutation burden and immune infiltration in bladder cancer. BMC Cancer 21, 458. https://doi.org/10.1186/s12885-021-08229-1 (2021).
Moroishi, T. et al. The hippo pathway kinases LATS1/2 suppress cancer immunity. Cell 167, 1525–1539. https://doi.org/10.1016/j.cell.2016.11.005 (2016).
Castellone, M. D. & Melillo, R. M. RET-mediated modulation of tumor microenvironment and immune response in multiple endocrine neoplasia type 2 (MEN2). Endocr. Relat. Cancer 25, T105–T119. https://doi.org/10.1530/ERC-17-0303 (2018).
Kaelin, W. G. Jr. The von Hippel-Lindau tumor suppressor protein and clear cell renal carcinoma. Clin. Cancer Res. 13, 680s–684s. https://doi.org/10.1158/1078-0432.CCR-06-1865 (2007).
Perier, A. et al. Mutations of the von Hippel-Lindau gene confer increased susceptibility to natural killer cells of clear-cell renal cell carcinoma. Oncogene 30, 2622–2632. https://doi.org/10.1038/onc.2010.638 (2011).
Trotta, A. M. et al. Mutated Von Hippel-Lindau-renal cell carcinoma (RCC) promotes patients specific natural killer (NK) cytotoxicity. J. Exp. Clin. Cancer Res. 37, 297. https://doi.org/10.1186/s13046-018-0952-7 (2018).
Atkins, M. B., Clark, J. I. & Quinn, D. I. Immune checkpoint inhibitors in advanced renal cell carcinoma: Experience to date and future directions. Ann. Oncol. 28, 1484–1494. https://doi.org/10.1093/annonc/mdx151 (2017).
Acknowledgements
The author would like to thank Dr. Patricia Finn (University of Illinois at Chicago) for her administrative support. This work was supported by NIH F30CA236031 to D.R. Principe.
Author information
Authors and Affiliations
Contributions
D.P. designed the study, analyzed data, assembled figures, and drafted the manuscript.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Principe, D.R. Patients deriving long-term benefit from immune checkpoint inhibitors demonstrate conserved patterns of site-specific mutations. Sci Rep 12, 11490 (2022). https://doi.org/10.1038/s41598-022-15714-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15714-5
This article is cited by
-
Uncovering the role of transient receptor potential channels in pterygium: a machine learning approach
Inflammation Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.