Abstract
Cough during therapeutic thoracentesis (TT) is considered an adverse effect. The study was aimed to evaluate the relationship between cough during TT and pleural pressure (Ppl) changes (∆P). Instantaneous Ppl was measured after withdrawal of predetermined volumes of pleural fluid. Fluid withdrawal (FW) and Ppl measurement (PplM) periods were analyzed separately using the two sample Kolmogorov–Smirnov test and the nonparametric skew to assess differences between ∆P distributions in periods with and without cough. The study involved 59 patients, median age 66 years, median withdrawn fluid volume 1800 mL (1330 ÷ 2400 mL). In total, 1265 cough episodes were recorded in 52 patients, in 24% of FW and 19% of PplM periods, respectively. Cough was associated with significant changes in ∆P distribution (p < 0.001), decreasing the left tail of ∆P distribution for FW periods (the skew = − 0.033 vs. − 0.182) and increasing the right tail for PplM periods (the skew = 0.182 vs. 0.088). Although cough was more frequent in 46 patients with normal pleural elastance (p < 0.0001), it was associated with significantly higher ∆P in patients with elevated elastance (median Ppl increase 2.9 vs. 0.2 cmH2O, respectively). Cough during TT is associated with small but beneficial trend in Ppl changes, particularly in patients with elevated pleural elastance, and should not be considered solely as an adverse event.
Similar content being viewed by others
Introduction
Pleural effusion affects approximately 1.5 million patients per year in the United States with the annual number of thoracenteses reported between 127,000 and 173,0001,2,3. Although, in general, therapeutic thoracentesis (TT) is thought to be a safe procedure, the withdrawal of a large pleural fluid volume can be associated with some complications, including chest discomfort, pain, pneumothorax and re-expansion pulmonary edema; some of these side effects are at least partially related to pleural pressure (Ppl) fall caused by fluid withdrawal4,5,6. In patients with normal pleuro-pulmonary mechanics, a gentle slope of the withdrawn pleural fluid volume−Ppl curve reflects the replacement of the fluid by the expanding lung. However, if lung expandability is limited by, for example, visceral pleural thickening, lung scars, fibrosis, or airway collapse, even a small amount of withdrawn pleural fluid may result in significant Ppl decline, which in turn may produce symptoms such as vague chest discomfort or cough7. Although significant chest discomfort is believed to be an indication for TT termination because it may suggest a potentially unsafe decline of Ppl5,6,7,8, the significance of cough seems to be controversial. Jones et al. recorded cough in less than 1% of patients undergoing ultrasound guided TT and it was not related to post procedure pneumothorax9; however these authors referred to other studies showing a significantly higher cough incidence (9–24%) and stated that cough in the late phase of TT should be regarded as an indication to stop the procedure. On the other hand, cough may be associated with lung re-expansion and thus, if not accompanied by other symptoms, it should not be considered as an indication for TT termination5,10.
Pleural manometry is a key tool to study different aspects of pleural pathophysiology in patients with pleural effusion. Access to pleural manometers, whether water or electronic, enables Ppl monitoring during TT and provides new insight into processes occurring during pleural fluid withdrawal, including a better understanding of complications and symptoms reported by the patients11, although its routine use in clinical practice in daily life was recently put into question12. Some previous observations led to the intriguing conclusion that cough during TT may favorably impact Ppl allowing to avoid excessive Ppl decline10. Although that observation was based on three patients only, it suggested that cough during TT need not necessarily be considered as a predictor of forthcoming complications, but may also be viewed as a protective phenomenon during the procedure. In general, we hypothesized that: (a) cough is linked with subsequent Ppl increase or its less significant decrease, (b) cough can be related to increased recruitment rate of atelectatic lung regions. Verification of the first hypothesis was the main purpose of this study.
Results
Data of 63 patients who underwent TT with pleural manometry between January 2015 and January 2019 were reviewed. Records of 3 patients were excluded due to a questionable reliability of Ppl measurements caused by the presence of fibrin membranes and loculations (n = 2) and low quality records (n = 1). One patient was excluded due to unclear and uncertain cough markings in the study documentation. Thus, the records of 59 patients were included in the final analysis. Patients' characteristics are presented in Table 1.
Cough during TT occurred in 52 patients. The total number of cough episodes was 1265 and the median and maximal number of episodes in individual patients were 11 and 104, respectively. Cough was found in 172 of 926 analyzed Ppl measurement periods (PplM; 19%) and in 222 of 927 analyzed fluid withdrawal periods (FW; 24%). Characteristics of the changes in Ppl (∆P) distributions for PplM and FW, with and without cough, are presented in Table 2.
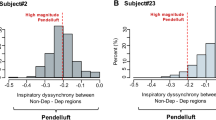
There was a relationship between cough and ∆P both during PplM and FW. Histograms of ∆P during PplM showed that cough was associated with an increase of the right tail of the ∆P distribution (Fig. 1). This is quantitatively illustrated by nonparametric skew values, e.g., the skew for all PplM without cough was equal to 0.088 vs. 0.182 for periods with cough (Table 2). During FW, cough was associated with a decrease of the left tail and an increase of the right tail of the ∆P distribution, resulting in an increase of the skew from − 0.182 for all periods without cough to − 0.033 for all periods with cough. Of note, the changes in the ∆P distribution were statistically significant only in the second phase of TT, i.e. the frequent measurement phase (Table 2).
Influence of cough on the ∆P distribution during Ppl measurement periods (PplM) (a and b) and during fluid withdrawal periods (FW) (c and d). (a) the distribution for PplM without cough, (b) the distribution for PplM with cough episodes, (c) the distribution for FW with no cough, (d) the distribution for FW with cough episodes. The figure was created using graph tool included in Statistica 13.1 software package (StatSoft Inc., Tulsa, USA) for which the required license has been purchased by the authors' institution.
Forty six and thirteen patients were found to have normal and elevated Pel, respectively. There was a statistically significant difference in the number of cough episodes between these groups (p < 0.0001; Mann–Whitney U-test). The median number of coughs in normal and elevated Pel group was 22 and 1, respectively; ΔP was greater in patients with increased Pel, particularly during PplM with cough (Table 3). In both groups, the differences in the ∆P distributions between PplM with and without cough were statistically significant (Table 3).
Discussion
Our study showed the association between cough and the pattern of Ppl changes during pleural fluid withdrawal. This is reflected by a significantly different ΔP distribution for periods with cough episodes compared to those with no cough. Cough was associated with the shift of ΔP towards more positive values during PplM and less negative values during FW (Table 2, Fig. 1). Thus, the occurrence of cough seems to be associated with a beneficial trend in Ppl changes, making Ppl slightly higher or less negative than in periods without cough. An additional important observation is that cough during TT was significantly more common in patients with normal pleural elastance compared to those with elevated Pel. Interestingly, albeit cough was far less common in patients with high Pel, it resulted in significantly more pronounced increase in Ppl than in patients with normal Pel (Table 3). As, to our knowledge, this is the first study that provides reliable statistical data on the relationship between cough and Ppl changes during TT, we believe our paper adds to the existing literature on pleural physiology. In the context of our results, we can hypothesize that cough during TT can be perceived not only as an adverse effect of pleural fluid withdrawal but also as a factor contributing to a mechanism preventing the rapid and excessive decline of Ppl.
Based on our previous observation10, two possible trends of cough-related Ppl changes during PplM had been assumed: (1) an increase of Ppl due to lung re-expansion and (2) no significant changes if cough was not associated with additional lung re-expansion. It can be supposed that the withdrawal of the first several portions of pleural fluid in patients with large volume pleural effusion may not significantly reduce lung compression. Therefore cough in the initial phase of pleural fluid withdrawal may not generate significant Ppl changes until the space for lung re-expansion appears. Then, the increase in Ppl may be observed if cough helps to open the compressed alveoli and fill them with air. The above hypothesis seems to be confirmed by our results. We found that cough-associated increase in Ppl was more pronounced in measurements performed after withdrawal of 1 L of pleural fluid (Table 2). We believe this may be related to a more significant decrease in hydrostatic pressure and smaller lung compression, which may facilitate lung re-expansion. As, in general, cough is associated with significant intrathoracic pressure variations up to 400 cm H2O during the compression phase13, we may anticipate that such a Ppl fluctuation may facilitate lung recruitment. Without these significant Ppl fluctuations the recruitment is hindered due to such factors as the surface tension and viscosity of liquid layer in the collapsed bronchioles, alveolar ducts and alveoli14,15. According to Mead et al., a fast opening of the atelectatic lung regions may require an airway pressure as high as 140 cm H2O16. Considering the above, we postulate a direct influence of cough on lung recruitment.
The above suggestion seems to be supported by a recent study that showed some beneficial influence of continuous positive airway pressure (CPAP) applied during TT17. CPAP primarily results in an increase of airway pressure, with only a secondary increase of Ppl. This implies the transpulmonary pressure increase18 that favors lung re-expansion. The impact of cough is probably much more complex. This is because cough also generates extremely high airway pressure but its rise is invariably associated with rapid contraction of the expiratory muscles and increase in Ppl. Thus, in general, there is no increase in transpulmonary pressure unless the deep inspiration preceding the contraction (Fig. 2) is also considered. However, as cough is a complex mechanical phenomenon and there are sophisticated mechanical interactions between the lung compressed by pleural fluid and the second lung, the distribution of airway pressure might probably be different than in normal lungs. Hence, we can speculate that regional differences of airway pressure distribution and the differences in the dynamics of its changes in relation to Ppl may favor re-expansion of some lung regions and result in the change of natural pattern of Ppl decline. It should be admitted that the opposite relationship cannot be excluded, i.e. that lung re-expansion is responsible for cough generation. In other words, cough does not facilitate lung recruitment and is beneficial per se but it only reflects some factors or phenomena associated with lung re-expansion. In FW, Ppl declines due to fluid evacuation, and, therefore, ∆P has negative values. If, however, effects of atelectatic regions recruitment are comparable to hydrostatic pressure decrease caused by fluid withdrawal, ∆P has less negative or even positive values (Fig. 1c). As, according to our hypothesis, cough episodes facilitate lung expansion, the number of positive ∆P values increases and the number of negative ∆P values decreases for FW with coughs (Fig. 1d), and, in consequence, the value of non-parametric skew is less negative (Table 2).
An example of pleural pressure record during therapeutic thoracentesis. The figure depicts 2 measurement periods (PplM) and 2 fluid withdrawal periods (FW) with red, vertical lines outlined during the procedure indicating cough episodes during PplM and FW. These markings were used to identify cough episodes during off-line analysis. Note that during PplM the cough episode (red line) corresponds with peaks of Ppl; in contrast, as Ppl is not registered during FW, cough can be identified exclusively by the marking drawn during the procedure. As depicted, no cough episodes occurred during the second PplM.
Although, according to the literature9, cough is a symptom presented by 9–24% of patients undergoing TT (while 88% in our study), its mechanism remains unclear. It has been documented that the main receptors responsible for cough are present in the larynx, trachea and main bronchi19. The vagal afferents are also present in small bronchi and lung parenchyma (juxtapulmonary receptors), and the new ERS chronic cough guidelines mention potential existence of cough receptors also in the alveolar septa and parenchyma of the lungs20. However, there is no proof that their irritation results in cough, despite the fact that cough is one of the symptoms in patients with heart failure, pulmonary edema or altitude sickness. It is supposed that cough in those cases appears only when sputum moves to larger bronchi and irritates the cough receptors or when there is bronchial compression21. The presence of cough receptors in the pleura is also considered4. Some authors suggested that negative Ppl caused by fluid withdrawal stimulates cough receptors on the visceral pleura, particularly in patients with nonexpendable lung 4,22. The results of our study do not seem to support these opinions since cough was significantly less common in patients with elevated Pel. Importantly, although less common, cough in patients with high Pel resulted in higher increase in Ppl than in patients with normal Pel (Table 3). Perhaps, lower (more negative) Ppl in those patients together with cough resulted in more effective and rapid recruitment of atelectatic lung regions, what may be supported by higher ∆P values observed also in PplM without cough (Table 3). Thus, considering the above, we suggest that patients with elevated Pel may be further sub-classified into the two following groups: (a) sustainably elevated Pel, and (b) elevated Pel which can be overcome by additional maneuvers e.g. cough or CPAP.
Some authors believe that cough is a criterion for TT termination as it is considered a sign of complete or near-complete drainage23,24,25. The results of our study do not support this opinion. This is because our study showed that in some patients a large fluid volume could have been withdrawn without significant Ppl fall despite episodes of cough which appeared even in the early phase of the procedure (data not published). Therefore, we agree with the opinion of Feller-Kopman et al. that TT should not be terminated solely because of cough5. Moreover, our findings may even support a hypothesis that cough can even be a beneficial factor preventing an excessive Ppl drop during TT in some cases. To confirm this view and to evaluate the clinical application of voluntary cough during thoracentesis, further, well-designed prospective studies are mandatory. It also seems necessary in the future to have a closer look to cough episodes characteristics in terms of Ppl increase; namely to check whether all types and episodes of cough can be construed as beneficial, especially cough attacks or severe excessive cough during the procedure.
Our study has several limitations, with the most important being the retrospective nature of the analysis which can only prove statistical associations and does not allow us to assess other aspects of cough as e.g. the duration of its impact on Ppl changes. However, it should be stressed that the study hypothesis was formulated before the retrospective analysis had been performed and the data were evaluated in a predefined and well-designed manner. As previously mentioned, we could only calculate ΔP using the maximal value of Ppl for each breath as a surrogate of Ppl at FRC, whereas this value depends on the Ppl at FRC and possible intrinsic positive end-expiratory pressure (therefore, ΔP could be slightly negative in some PplM–Fig. 3). Unfortunately, reliable estimation of the Ppl at FRC was impossible without continuous, simultaneous spirometry measurement to detect the expiration end. Also, the majority of the patients had malignant pleural effusion, as we focused on subjects requiring large therapeutic thoracentesis. Therefore, it was impossible to analyze if cough affects Ppl similarly in patients with benign pleural effusion. Finally, as the study was specifically focused on the relationship between cough and Ppl, we have not analyzed other characteristics of cough during TT.
Graphic presentation of the method used to extract specific sections of the pleural pressure (Ppl) curve for the assessment of Pplmax changes. PplM- pleural pressure measurement period, FW–fluid withdrawal period, PplmaxB—maximal values of Ppl at the beginning of Ppl measurement period (the initial 2/5 of the entire PplM), PplmaxE—maximal values of Ppl at the end of Ppl measurement period (the terminal 2/5 of the entire PplM).
Conclusions
Cough during TT is associated with small, beneficial trends in Ppl changes. This effect is particularly pronounced in patients with elevated Pel. Although the true significance of cough-related increase in Ppl is difficult to estimate, the results of our study may suggest that cough during TT should not be considered solely as an adverse event. We believe that the effect of voluntary cough on the pattern of Ppl decline should also be tested in the context of its potential effect on elevation of Ppl and increase in the volume of pleural fluid that can be withdrawn.
Methods
General study design
This was a retrospective analysis of data collected from a cohort of patients who were enrolled in a larger, prospective project evaluating the impact of TT on cardiovascular and pulmonary function. This project was supported by the Polish National Science Centre (grant No 2012/05/B/NZ5/01343) and by the Nalecz Institute of Biocybernetics and Biomedical Engineering, Polish Academy of Sciences (the IBBE PAS own research fund). The study protocol was approved by the Institutional Review Board of Medical University of Warsaw (KB 105/2012) and registered at ClinicalTrials.gov (NCT02192138) on 16/07/2014. The study conformed to the standards set by the Declaration of Helsinki. All medical procedures were performed in patients hospitalized in the Department of Internal Medicine, Pulmonary Diseases and Allergy, Medical University of Warsaw, and all patients signed an informed consent to participate in the study.
Patients
Sixty three patients who underwent TT with pleural manometry between January 2015 and January 2019 were included in the analysis; consecutive subjects were enrolled to avoid selection bias. The inclusion criteria were as follows: (1) age 18–85 years; (2) symptomatic pleural effusion occupying at least 1/3 of the hemithorax (in posteroanterior chest radiograph); (3) symptoms severity (dyspnea) warranting TT; (4) no contraindication for TT; (5) signed informed consent for participation in the study. The exclusion criteria were: (1) poor performance status requiring maximal shortening of the procedure; (2) unstable hemodynamic or respiratory status unrelated to pleural effusion; (3) respiratory failure requiring mechanical ventilation.
Thoracentesis and pleural manometry
TT and pleural manometry were performed in sitting position, as described previously26,27,28,29. Pleural fluid was evacuated through a small-bore pleural catheter (Turkel™ Safety System, Covidien, Whiteley Fareham, UK). Pleural pressure was measured with a digital pleural manometer (IBBE PAS, Warsaw, Poland) and recorded for one minute directly after catheter insertion and then during the procedure. There were interchanging periods of Ppl measurement (PplM) and periods of fluid withdrawal (FW) (Fig. 2). Initially, Ppl was measured after the withdrawal of each 200 mL up to 1L (the phase of rare Ppl measurements), and then after the withdrawal of each 100 mL (frequent Ppl measurement phase). The procedure was terminated when no more fluid could be aspirated, a significant pleural pressure decline was observed or chest pain occurred. Ppl was displayed on a monitor during the procedure and its instantaneous values were recorded on a portable computer for further analysis. Each cough episode, both during PplM and FW, was marked in the computer record at the corresponding place on the time vector and noted in the patient's individual study documentation (Fig. 2).
Data analyses
In each patient, all PplM periods recorded during the procedure were analyzed to assess a possible influence of cough on the respiratory system. As instantaneous Ppl values depend on several variables, including respiratory muscle activity, the end-expiratory Ppl values (at functional residual capacity (FRC)) should ideally be used for analysis. This is because at FRC (i.e. after spontaneous, slow expiration) respiratory muscles are fully relaxed and Ppl depends entirely on the volume of pleural fluid and the relationship between the outward pull of the thoracic cavity and the inward elastic recoil of the lung. Since, however, the exact time points of expiration ends were impossible to determine without airflow measurement, the maximal value of Ppl (Pplmax) in a breathing cycle was assumed to reflect Ppl at FRC. The median values of Pplmax at the beginning (PplmaxB) and the end (PplmaxE) of PplM were used to quantitatively characterize Ppl changes during PplM and FW. Thus, ∆P equal to the difference between PplmaxE and PplmaxB (PplmaxE–PplmaxB) was considered as the index characterizing the Ppl change during the corresponding PplM, whereas ∆P equal to the difference between PplmaxB for the subsequent PplM and PplmaxE for the previous PplM was used to quantify the Ppl change during FW (Fig. 3). The first and last 2/5 of the PplM period were treated as the beginning and as the end of the PplM, respectively. This 2/5 was a compromise between the following requirements: (a) the number of Pplmax values used in determination of the median should be as large as possible to avoid random errors, and thus the interval for analysis should be relatively long; (b) PplmaxB and PplmaxE should reflect the Pplmax values at the actual beginning and end of each PplM, and thus the intervals should be short and limited to extremes of the PplM.
Additionally, to examine whether a possible link between cough and ΔP depends on lung expandability, all patients were classified according to the total pleural elastance (Pel), i.e. the ratio of Ppl fall during the whole procedure to the total volume of withdrawn fluid. The first group included patients with normal Pel (< 14.5cm H2O/L)30, while the second included those with elevated elastance (≥ 14.5cm H2O/L).
Statistical analysis
Statistical analysis was performed using the Statistica 13.1 software package (StatSoft Inc., Tulsa, USA). Data were presented as median and quartiles. Since the majority of analyzed variables had non-normal distributions, non-parametric statistical tests were used. The differences between groups were tested with the Mann–Whitney U-test. To analyze the statistical significance of cough influence on the ΔP distribution shape, the two-sample Kolgomorow-Smirnow test was used. The nonparametric skew was used to determine the nature of this influence. P values < 0.05 were considered statistically significant.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Change history
28 August 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-41308-w
References
Feller-Kopman, D. & Light, R. Pleural disease. N. Engl. J. Med. 378(8), 740–751 (2018).
Owings, M. F. & Kozak, L. J. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat. 13(139), 1–119 (1998).
Duszak, R. Jr., Chatterjee, A. R. & Schneider, D. A. National fluid shifts: fifteen-year trends in paracentesis and thoracentesis procedures. J. Am. Coll. Radiol. 7(11), 859–864 (2010).
Feller-Kopman, D., Parker, M. J. & Schwartzstein, R. M. Assessment of pleural pressure in the evaluation of pleural effusions. Chest 35(1), 201–209 (2009).
Feller-Kopman, D., Walkey, A., Berkowitz, D. & Ernst, A. The relationship of pleural pressure to symptom development during therapeutic thoracentesis. Chest 129, 1556–1560 (2006).
Petersen, W. G. & Zimmerman, R. Limited utility of chest radiograph thoracentesis. Chest 117, 1038–1042 (2000).
Huggins, J. T., Doelken, P. & Sahn, S. A. The unexpandable lung. F1000 Med. Rep. 2, 77 (2010).
Light, R. W., Jenkinson, S. G., Minh, V. D. & George, R. B. Observations on pleural fluid pressures as fluid is withdrawn during thoracentesis. Am. Rev. Respir. Dis. 121, 799–804 (1980).
Jones, P. W. et al. Ultrasound-guided thoracentesis: Is it a safer method?. Chest 123(2), 418–423 (1980).
Zielinska-Krawczyk, M. et al. Cough during therapeutic thoracentesis: Friend or foe?. Respirology 20(1), 166–168 (2015).
Maldonado, F. & Feller-Kopman, D. Should manometry be routinely used during thoracentesis? Yes, but not without some basic physiologic understanding!. Expert Rev. Respir. Med. 10, 1035–1037 (2016).
Lentz, R. J. et al. Routine monitoring with pleural manometry during therapeutic large-volume thoracentesis to prevent pleural-pressure-related complications: a multicentre, single-blind randomised controlled trial. Lancet Respir. Med. 7(5), 447–455 (2019).
McCool, F. D. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest 129(1 Suppl), 48S-53S (2006).
Gaver, D. P., Samsel, R. W. & Solway, J. Effects of surface tension and viscosity on airway reopening. J. Appl. Physiol. 75, 1323–1333 (1990).
Hsu, S. H., Strohl, K. P., Haxhiu, M. A. & Jamieson, A. M. Role of viscoelasticity in tube model of airway reopening. J. Appl. Physiol. 80, 1649–1659 (1994).
Mead, J., Takishima, T. A. & Leith, D. A. Stress distribution in lungs: a model of pulmonary elasticity. J. Appl. Physiol. 28(5), 596–608 (1970).
Abouzgheib, W. et al. The impact of continuous positive airway pressure upon pleural fluid pressures during thoracentesis. Respiration 17, 1–5 (2019).
Loring, S. H., Topulos, G. P. & Hubmayr, R. D. Transpulmonary pressure: the importance of precise definitions and limiting assumptions. Am. J. Respir. Crit Care Med. 194(12), 1452–1457 (2016).
Canning, B. J. et al. Chest expert cough panel: Anatomy and neurophysiology of cough: Chest guideline and expert panel report. Chest 146(6), 1633–1648 (2014).
Morice, A. H. et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur. Respir. J. 55(1), 1901136 (2019).
Widdicombe, J. G. Neurophysiology of the cough reflex. Eur. Respir. J. 8, 1193–1202 (1995).
Bibby, A. C. et al. The prevalence and clinical relevance of nonexpandable lung in malignant pleural mesothelioma: A prospective, single-center cohort study of 229 patients. Ann. Am. Thorac. Soc. 16, 1273–1279 (2019).
Light, R. W., Stansbury, D. W. & Brown, S. E. The relationship between pleural pressures and changes in pulmonary function after therapeutic thoracentesis. Am. Rev. Respir. Dis. 133(4), 658–661 (1986).
Bhuniya, S. et al. Role of therapeutic thoracentesis in tuberculous pleural effusion. Ann. Thorac. Med. 7(4), 215–219 (2012).
Na, M. J. Diagnostic tools of pleural effusion. Tuberc. Respir. Dis. 76(5), 199–210 (2014).
Krenke, R. et al. Development of an electronic manometer for intrapleural pressure monitoring. Respiration 82, 377–385 (2011).
Zielinska-Krawczyk, M. et al. Patterns of pleural pressure amplitude and respiratory rate changes during therapeutic thoracentesis. BMC Pulm. Med. 18, 36 (2018).
Gólczewski, T. et al. The use of a virtual patient to follow pleural pressure changes associated with therapeutic thoracentesis. Int. J. Artif. Organs. 40, 690–695 (2017).
Stecka, A. M. et al. The use of a virtual patient to follow changes in arterial blood gases associated with therapeutic thoracentesis. Int. J. Artif. Organs. 41, 690–697 (2018).
Heidecker, J., Huggins, J. T., Sahn, S. A. & Doelken, P. Pathophysiology of pneumothorax following ultrasound-guided thoracentesis. Chest 130, 1173–1184 (2006).
Acknowledgements
The authors thank Piotr Korczyński, PhD MD, Krzysztof Zieliński, PhD Eng. and Krzysztof J Pałko, PhD Eng., for their assistance during the clinical phase of the study. We would like to thank Marta Maskey-Warzęchowska for her editorial assistance. The study was partially supported by funds from the National Science Centre, Poland (grant No 2019/35/B/NZ5/02531).
Author information
Authors and Affiliations
Contributions
T.G. and R.K. conceived the study. T.G., R.K., A.M.S., E.M.G. designed the study. A.M.S., E.M.G., M.M., M.Z.K., and R.K. collected the data. A.M.S., E.M.G., M.M., R.K., T.G. contributed substantially to the data analysis and interpretation and are responsible for the accuracy and integrity of the results. All authors contributed to drafting, critical review, and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors declare that they had no competing interests, except personal fees from the grant from National Science Centre, Poland (Grant No 2012/05/B/NZ5/01343).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The Acknowledgements section in the original version of this Article was incomplete. It now reads: “The authors thank Piotr Korczyński, PhD MD, Krzysztof Zieliński, PhD Eng. and Krzysztof J Pałko, PhD Eng., for their assistance during the clinical phase of the study. We would like to thank Marta Maskey-Warzęchowska for her editorial assistance. The study was partially supported by funds from the National Science Centre, Poland (grant No 2019/35/B/NZ5/02531).”
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stecka, A.M., Grabczak, E.M., Michnikowski, M. et al. The impact of spontaneous cough on pleural pressure changes during therapeutic thoracentesis. Sci Rep 12, 11502 (2022). https://doi.org/10.1038/s41598-022-15480-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15480-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.