Abstract
The Delta (B.1.617.2) variant was the predominant UK circulating SARS-CoV-2 strain between May and December 2021. How Delta infection compares with previous variants is unknown. This prospective observational cohort study assessed symptomatic adults participating in the app-based COVID Symptom Study who tested positive for SARS-CoV-2 from May 26 to July 1, 2021 (Delta overwhelmingly the predominant circulating UK variant), compared (1:1, age- and sex-matched) with individuals presenting from December 28, 2020 to May 6, 2021 (Alpha (B.1.1.7) the predominant variant). We assessed illness (symptoms, duration, presentation to hospital) during Alpha- and Delta-predominant timeframes; and transmission, reinfection, and vaccine effectiveness during the Delta-predominant period. 3581 individuals (aged 18 to 100 years) from each timeframe were assessed. The seven most frequent symptoms were common to both variants. Within the first 28 days of illness, some symptoms were more common with Delta versus Alpha infection (including fever, sore throat, and headache) and some vice versa (dyspnoea). Symptom burden in the first week was higher with Delta versus Alpha infection; however, the odds of any given symptom lasting ≥ 7 days was either lower or unchanged. Illness duration ≥ 28 days was lower with Delta versus Alpha infection, though unchanged in unvaccinated individuals. Hospitalisation for COVID-19 was unchanged. The Delta variant appeared more (1.49) transmissible than Alpha. Re-infections were low in all UK regions. Vaccination markedly reduced the risk of Delta infection (by 69-84%). We conclude that COVID-19 from Delta or Alpha infections is similar. The Delta variant is more transmissible than Alpha; however, current vaccines showed good efficacy against disease. This research framework can be useful for future comparisons with new emerging variants.
Similar content being viewed by others
Introduction
Viruses mutate over time1, affecting transmissibility2, disease presentation3, and natural or vaccine-induced protective immunity.4 The Delta variant of SARS-CoV-2 (B.1.617.2) was identified in India in late 2020 and declared a ‘Variant of Concern’ in May 2021 by the UK5, the World Health Organization6, and the European Centre for Disease Control7, mainly due to evidence of increased transmissibility,8,9 possibly larger risk of hospitalisation,10,11 and conceivably less effectiveness of vaccination compared with previous variants4,12,13.
In the UK, the Delta variant rapidly became the dominant circulating form of SARS-CoV-2, (from 0.09% at the beginning of April 2021 to > 98% at the end of June 2021) displacing the Alpha (B.1.1.7) variant which concomitantly decreased from 98% to 1.67% (Supplementary Table S1, Supplementary Figure S1)14. On November 27, 2021, a new variant (Omicron B.1.1.529) emerged and spread rapidly, and became the predominant SARS-CoV-2 variant in UK after December 20, 2021. However, on 15 January 2022, Delta variant was still accounting for up to 40% new cases of SARS-CoV-2 infection in many European countries, and 20% cases in UK (https://www.gisaid.org/hcov19-variants/). Many other factors also changed contemporaneously, including SARS-CoV-2 prevalence, relaxation of lockdown restrictions, test access criteria, and the delivery of a mass vaccination campaign stratified by age, clinical vulnerability, and healthcare worker status.
We previously described COVID-19 profile, transmissibility, re-infection risk15, and vaccine effectiveness16 when the Alpha (B.1.1.7) variant was predominant. Here, we present these data after the Delta variant became predominant, and compare illness from Delta versus Alpha infection, in a large UK community cohort.
Results
Cohort description
44,718 adults testing positive for SARS-CoV-2 between December 28, 2020 and July 1, 2021, 22,699 had symptoms within requisite timeframes and logged sufficiently regularly for calculation of illness duration: 19,118 individuals when Alpha was predominant and 3581 when Delta was predominant. Demographic characteristics (after age, gender, and 1:1 matching) are presented in Table 1.
Illness profile
Symptoms within the first 28 days of illness are presented in Fig. 1 and Supplementary Table S3 (descriptive data). All symptoms evidenced until day 28 had presented by day 21, in all individuals with both variants. The seven most reported symptoms were the same for Delta as for Alpha infection, though varied in prevalence: headache (75% vs. 67%), fatigue (73% in both), rhinorrhea (71% vs. 54%), anosmia/dysosmia (64% vs. 54%), sneezing (59% vs. 44%), sore throat (56% vs. 42%) and persistent cough (51% vs. 41%).
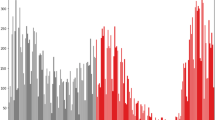
Correcting for age, sex, and vaccination status at time of positive test, and for false discovery rate, several symptoms were more common during the first 28 days of illness with Delta versus Alpha infection, including fever (OR 2.82 [95% CI 2.44–3.26]), hoarse voice (OR 1.82 [95% CI 1.56; 2.11]), sore throat (OR 1.73, [95% CI 1.5; 2]), and persistent cough (OR 1.64 [95% CI 1.43; 1.88]); conversely, the risk of shortness of breath was lower (OR 0.82 [95% CI 0.69; 0.96]) (Fig. 2, Supplementary Table S4). The odds of five or more symptoms in the first week of illness were higher with Delta versus Alpha infection, whether for the 14 symptoms analysed in Sudre et al.17 (OR 1.70 [95% CI 1.47; 1.95], p < 0.00005) or all symptoms (Supplementary Table S2) (OR 1.78 [95% CI 1.50; 2.11], p < 0.00005). However, the risk for any given symptom to last ≥ 7 days was either lower (chills, headache, rhinorrhea, fatigue) or unchanged (Fig. 3; Supplementary Table S4).
Odds ratios for any symptom presenting within the first 28 days of illness in individuals with COVID-19 during periods of SARS-CoV-2 Delta versus Alpha variant predominance. Age, gender, and vaccination.status are included as covariates in this analysis. Red markers encode statistical significance with α-value < 0.05, whereas grey markers encode non-significant differences, after correction for false discovery rate.
Odds ratios for risk of symptom duration ≥ 7 days for individuals with COVID-19 during periods of SARS-CoV-2 Delta versus Alpha variant predominance. Age, gender, and vaccination.status are included as covariates in this analysis. Red markers encode statistical significance with α-value < 0.05 (after FDR correction), whereas grey markers encode non-significant differences.
Long illness duration
The risk of LC28 was moderately lower with Delta versus Alpha infection (8.7% [311/5581] vs. 10.6% [380/5581] of individuals, OR 0.69 [0.50; 0.94], p = 0.018 (considering the cohort overall, with age, sex and vaccination status included as covariates). In a sensitivity analysis considering only unvaccinated individuals (Table 1), there was a trend towards lowered risk of LC28 with Delta versus Alpha infection (OR 0.75 [0.54; 1.04], p = 0.087).
Hospital presentation
Hospital care for COVID-19 was needed for 120 (3.4%) of 3581 individuals during the Delta period and 207 (5.8%) of 3581 during the Alpha period. Noting here that the UK vaccination campaign was stratified by age, clinical vulnerability, and health-care worker status, the risk of hospital presentation was moderately but not significantly lower for Delta versus Alpha infection, considered overall (OR 0.76 [95% CI 0.53; 1.11] p = 0.156, with age, sex and vaccination status included as covariates) or for unvaccinated individuals alone considered as a sensitivity analysis (OR 0.82 [95% CI 0.56; 1.20], p = 0.299).
Transmissibility
Consistent with other studies, the Delta variant was more transmissible than Alpha, by 1.47 (95%CI 1.45–1.49) according to a population-weighted average (Table 2), noting wide confidence intervals and variation over time. Estimates per region agreed broadly with some regional variation (Fig. 4, Table 2).
Incidence and R(t) for Delta and non-Delta variants. Left column shows total incidence, and incidence for each variant. Middle column shows R(t) for each variant. Rightmost column shows the ratio R_Delta/R_non-Delta, noting that in the timeframe considered non-Delta was predominantly Alpha. Vertical line indicates lifting of some lockdown restrictions on May 17, 2021.
Effect of the Delta variant on re-infection
Figure 5 shows the (small) absolute numbers of re-infections across regions, with: a) the number of positive tests reported by app users; and b) the Delta variant as a proportion of circulating SARS-CoV-2, over time. Spearman correlations between reinfection and positive test incidence ranged from 0.46 in the South East to 0.83 in the Midlands. Correlations between reinfection and Delta variant proportions in each region were lower, ranging from 0.41 in the North East and Yorkshire to 0.69 in the North West. In most regions, the correlation of reinfections with the number of reported tests was higher than the correlation of reinfections with the proportion of Delta variant. Supplementary Table S5 presents characteristics of the bootstrapped distribution (100 samples) of correlations for each region over time. Thus, the rise of SARS-CoV-2 infection during the time of Delta predominance correlates more closely with the rise of incidence of new cases per se, rather than the rise in proportion of cases due to the Delta variant specifically.
Regional graphs presenting evolution of numbers of reported natural reinfection with SARS-CoV-2. Reported natural reinfection is charted over time in weeks (starting from March 1, 2021) (x-axis). The blue bars graph the absolute number of cases with re-infection. The red line graphs the proportion of the Delta variant among circulating SARS-CoV-2 (COG UK—Supplementary Table S1). The green line graphs the total numbers of positive tests reported by ZOE COVID Symptom Study app users. Data are combined for East and West Midlands, and for Yorkshire and the North East.
Post-vaccination infection during the Delta period
402,191 app users aged 20–65 years were vaccinated with BNT162b2 (1st dose only: 33,171, 2nd dose: 117,091) or ChAdOx1 nCoV-19 (1st dose only: 59,663, 2nd dose: 192,266) and reported at least one PCR or LFAT test after vaccination between May 26 and July 1, 2021. A positive result was reported by 1723 of 92,834 (1.86%) who had received one dose, and 1722 of 309,357 (0.56%) who had received two doses. Data were compared to 25,395 unvaccinated time-matched participants, in whom 1361 (5.36%) individuals reported a positive test.
After adjustment for population differences in the vaccinated groups using Poisson regressions as described in Methods, the risk reduction of post-vaccination infection after first dose (considered 14–60 days after first dose) was − 71.5% (95% CI − 74.4 to − 68.3) with BNT162b2 and − 58.3% (95% CI − 63.7 to − 52.1) with ChAdOx1 nCoV-19, compared with unvaccinated individuals. The risk reduction was even larger in fully vaccinated individuals (considered 14–60 days after second dose): − 84.1% [95% CI − 86.9 to − 80.6] with BNT162b2, and -69.6% [95% CI − 72.9 to − 65.9] with ChAdOx1 nCoV-19, compared with unvaccinated controls (Fig. 6).
Discussion
Our large-scale community-based UK study has shown that COVID-19 is clinically similar whether due to Alpha or Delta variants. Ten of 31 symptoms were more common with Delta infection and one with Alpha infection. Although the burden of symptoms in the first week was higher with Delta infection, duration of many individual symptoms was shorter; fewer individuals experienced illness lasting more than 28 days—though saliently this was unchanged in unvaccinated individuals; and there was a trend towards fewer hospital presentations. These observations need to be interpreted in the context of increasing vaccination of the UK population, along with many other environmental and societal changes.
Few studies of COVID-19 due to the Delta variant are available for comparison. One study of 27 infected young individuals reported symptoms in 22 (81%), with the commonest symptoms fever (41%), cough (33%), headache (26%), and sore throat (26%) (duration of illness not reported)18. Other studies report smaller cohorts. The REACT-1 study Round 14 report (UK data during September 2021, with Delta variant the predominant UK variant) showed a weighted prevalence of individuals testing positive varied greatly by age (0.29% in adults aged > 75 years compared to 2.55% in teenagers and 2.32% in children aged 5–12 years), noting high vaccination rates in older individuals and little or no vaccination in younger age groups at the time of this report19. However, data on symptoms (duration and/or prevalence) were not reported.
The risk of LC28 was lower with Delta (8.7%) versus Alpha infection (10.6%), although not statistically different in unvaccinated individuals. These results are similar to our previous paper using similar methodology, for individuals infected during the first UK pandemic wave (13.3%)17. The Post COVID syndrome (Long COVID) is defined as illness duration > 12 weeks after likely SARS-CoV-2 infection (https://www.nice.org.uk/guidance/NG188). Our census dates preclude our ability to compare illness duration beyond 28 days between our two cohorts. Estimates of prevalence of the Post-COVID syndrome are difficult, as many studies lack appropriate control groups. A recent meta-analysis of UK longitudinal cohort studies suggested the post-COVID syndrome was present in 1.2–4.8% of individuals20, similar to recently published figures from the Office for National Statistics (ONS) (1.9% of the UK population self-reporting long COVID (diagnosis otherwise unverified) as of October 2, 2021, although only 71% had (or suspected they had) COVID-19 12 weeks earlier (https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/4november2021).
We showed a marked increase in transmissibility with the Delta versus non-Delta (i.e., Alpha) variant, noting wide confidence intervals. This analysis does not take into account prior natural infection or vaccination rates within the community; and is likely a combination of both the Delta variant’s transmission advantage and its potential ability to evade immunity (whether induced by vaccination or prior natural infection with Alpha or other strains). This estimated increase in transmissibility is greater than we previously estimated for Alpha versus earlier variants using the same methodology [1.35 (95% CI 1.02–1.69)]15 noting again pertinent differences (e.g., viral prevalence, lockdown restrictions) between the current and previous studies. Estimates in both studies assume that incidence estimated from app users can be made representative of the wider population, using stratification by age and vaccination status. However, other factors such as behavior and socio-economic status are not corrected for by this analysis. Other studies have also identified higher Delta transmissibility, resulting in rising incidence particularly in young unvaccinated age groups, higher re-infection rates, and a higher viral load in infected individuals21. Here we note the REACT-1 study report of an exponential increase in infections in children aged 5–17 years in September 2021, coinciding with return-to-school, with most school-age children unvaccinated at this time.
Our study found that for most regions of the UK, the correlation of reinfections with the number of reported positive tests (i.e., incidence of cases) was higher than the correlation of reinfections with the proportion of Delta among the circulating variants (i.e., incidence of variant). In other words, the rise in COVID-19 correlated more closely with increase in prevalence of SARS-CoV-2 overall rather than the increased proportion of circulating SARS-CoV-2 due to the Delta variant. SARS-CoV-2 infection provides substantial and persistent immunologic protection for at least several months for most individuals, with a recent systematic review suggesting a risk reduction of reinfection of > 90%, similar to vaccination, and evident for at least 10 months22. However, this may not be uniform across the population. A study of tested individuals followed prospectively for at least 3 months demonstrated a protective effect after prior infection of 80.3% for younger individuals (aged 20–59 years) but only 67.4% for older individuals (aged ≥ 60 years), with lower levels of protection in individuals associated with a long-term care facility and/or who had milder initial disease23. A study of Danish healthcare workers24 found small absolute numbers of re-infected individuals (5 of 750 seropositive individuals over 5–6 months). However, 5% of previously seropositive individuals reverted to seronegative status, associated with older age and fewer symptoms with initial infection (noting here that the relationship between antibody titre and subsequent infection risk is currently unclear). In July 2021 UK governmental figures estimated an adjusted odds ratio of reinfection risk from the Delta variant versus the Alpha variant as 1.5. However, this varied according to time since initial infection: the odds ratio was not elevated if initial infection was < 180 days earlier (adjusted odds ratio = 0.8), but was higher if initial infection was ≥ 180 days earlier (adjusted odds ratio = 2.4) (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1005517/Technical_Briefing_19.pdf).
Our observational data support effectiveness of both BNT162b2 and ChAdOx1 nCoV-19 vaccines against the Delta variant. Both reduced the risk of testing positive during the Delta period, evident after the first and enhanced after the second dose25. These figures are similar to our previous results when the Alpha variant was predominant15. We have an inherent bias due to the nature of the UK vaccine rollout, whereby health-care workers, elderly people, and clinically vulnerable individuals were prioritised before the younger population, creating unbalanced demographic characteristics between vaccinated and unvaccinated populations. Moreover, we cannot compare vaccination effectiveness against Alpha versus Delta variants, given the many differences between the two timeframes. Although we attempted to adjust for some of these differences using Poisson regression, behavioural factors are difficult to capture. For example, individuals vaccinated earlier may have changed their behaviours over concern of possible waning antibody status and possible reducing immunity26. However, our results concord with vaccination trial data27,28, and provide support for ongoing vaccination campaigns internationally. Previous data have shown that vaccination is associated with significant reduction in risk of hospitalisation and disease progression to death or mechanical ventilation in individuals with COVID-1912,29. Our data similarly showed a trend towards fewer hospital presentations. Later analyses during further waves of the pandemic will be useful here with the methods and approaches described here similarly applied to assess the impact of emerging variants.
We acknowledge the limitations of our observational study. Self-reported data from a mobile phone app may disproportionately represent more affluent populations and can introduce information bias and/or effect bias, although previous work from the CSS has shown that our self-reported data aligns well with surveys designed to be representative of the population30 and smartphone ownership in the UK is extensive with little evidence that this varies greatly across socio-economic groups. Further, 1600 of 7162 individuals were proxy-reported, which may also affect symptom reporting, although the proportion of proxy-reported individuals as a percentage of total individuals was the same for both time-periods (22.4%). Participants could only report a positive test and we cannot confirm the actual variant causing infection, although our assumptions of Delta and Alpha infection are strongly supported by UK-COG surveillance variant testing. During the study, both overall numbers and individual app users fluctuated in their participation in the CSS-app, potentially for many factors including mass-media information, summer vacation, and perception of relevance. Our populations were matched for age and sex but not BMI; and we note higher diabetes prevalence and BMI in the Alpha cohort. Relevantly, vaccination was not only tiered by age but also to those with co-morbidities including diabetes. As mentioned, the timeframes of Alpha and Delta variant predominance differed with respect to guidance on social distancing and behavior in public spaces, highly likely to affect viral diffusion in the population, thus affecting our transmission calculations. Last, vaccine effectiveness could only be determined in tested individuals, noting that we do not have information regarding the reason for testing in these individuals. We were also only able to assess individuals in the age range of 20–65, in order to avoid unbalanced case/control data. Relevantly, early post-vaccination symptoms can mimic COVID-1931 but may not necessarily trigger testing. Here, our previous work showed that vaccinated individuals are more likely to have post-vaccination systemic symptoms after a previously positive test compared to those without known past infection (odds ratios 2.3–4.0), which may bias presentation for SARS-CoV-2 testing post-vaccination.
Conclusions
The clinical presentation of COVID-19 due to the Delta variant is similar to illness caused by the Alpha variant: although symptom burden in the first week is modestly higher, individual symptom duration was either the same or shorter, and the risk of LC28 was lower. The Delta variant was more transmissible than the preceding predominant variant (i.e., Alpha) but did not increase the risk of reinfection per se. The risk of infection in fully vaccinated individuals was reduced by both BNT162b2 and ChAdOx1 nCoV-19, compared with unvaccinated controls, confirming good vaccine efficacy against the Delta variant and supporting the ongoing anti-SARS-CoV-2 vaccination campaign internationally.
Methods
COVID Symptom study
Prospective longitudinal observational data were collected as part of the King’s College London [KCL]/ZOE COVID Symptom Study, using the ZOE COVID Study App32 (Supplementary Information). Briefly, upon enrolment users provide baseline demographic and health information, and subsequently are prompted daily to record symptoms (or their absence) through direct questioning (Supplementary Table S2) and free text, any SARS-CoV-2 testing and corresponding result, vaccination details, and any hospital presentation. Users can also proxy-report for others. The current study was drawn from approximately 1 million UK app users who logged data at least once between December 28, 2020 to July 1, 2021. Data were extracted and curated through ExeTera software33.
Ethics approval was granted by the KCL Ethics Committee (LRS-19/20-18210). To ensure informed consent, at registration with the app, all participants were shown informative documentation, and were offered to provide consent for their data to be used for COVID-19 research. Governance was specifically granted for use of proxy-reported data. Research was performed in accordance with the relevant guidelines and regulations, and particularly in full compliance with the Declaration of Helsinki and further updates.
Data from all UK adult participants aged 18 to 100 years (including proxy-reported individuals) who logged a positive PCR or lateral flow antigen test (LFAT) for SARS-CoV-2 between December 28, 2020 to July 1, 2021 were considered. As previously17, individuals were considered to have COVID-19 if SARS-CoV-2-associated symptoms were reported (or proxy-reported) (Supplementary Table S2) between two weeks before and one week after positive testing. Data were included for individuals who reported at least weekly, from first symptom report until returning to symptom-freedom or until reporting ceased22.
Data were compared between two time periods: December 28, 2020 to May 6, 2021, when the Alpha variant was the predominant circulating SARS-CoV-2 strain (proportion of sequenced strains: > 75% from December 28, 2020, reaching > 95% by February 3 2021, and remaining > 75% until 28 April); and May 26, 2021 to July 1, 2021, when the Delta variant was the predominant strain (> 75% from May 26, reaching > 95% by June 9 and > 99% from June 30 to data census date) (Supplementary Table S1). Individuals logging a positive test did not have variant confirmation by sequencing; thus, illness within these two timeframes was attributed to the predominant circulating variant. Terminology herein reflects this assumption.
Through an Euclidean distance-based algorithm34, individuals with Delta infection were matched 1:1, based on their age and sex, with individuals with Alpha infection. We were unable to match for SARS-CoV-2 prevalence, tiered lockdown restrictions, or vaccination rates, which varied widely across the community and with time during this study.
Symptom data were censored at August 5, 2021, 35 days after last inclusion date for testing positive with Delta infection, allowing at least 28 days’ symptom evaluation for all individuals. Symptoms were considered over the entire illness, which by virtue of illness definition could extend outside SARS-CoV-2 testing date boundaries (a maximum of two weeks before and five weeks after testing, allowing for individuals whose illness started up to a week after positive test). To allow for symptom waxing and waning, individuals who returned a healthy report but subsequently logged as symptomatic within seven days of their last unhealthy report were considered unwell from their initial illness, with per-symptom and illness duration calculated accordingly.
We ascertained odds of a given symptom developing within 28 days of illness; and odds of each symptom lasting ≥ 7 days, corrected for age, sex and vaccination status (unvaccinated, 1 dose, 2 doses), with a given vaccination considered valid after 14 days (allowing for evolving immunity). We used false discovery rate to account for multiple comparisons. We assessed risk of illness duration ≥ 28 days (LC28) and hospital presentation (admission or emergency room attendance), in the cohort overall (similarly adjusted for age, sex and vaccination status) and in unvaccinated individuals alone, as a sensitivity analysis.
Transmissibility
We used data from COVID-19 Genomics UK Consortium (COG-UK) to extract time-series of the percentage of daily positive SARS-CoV-2 testing from the Delta lineage in Scotland, Wales, and each of nine National Health Service (NHS) regions in England. Northern Ireland was excluded due to low sample numbers in the COG-UK dataset. The COG-UK data are produced by sequencing a random sample of positive PCR tests from the general community.
Daily SARS-CoV-2 incidence data for Scotland, Wales, and each NHS region in England were estimated from March 14 to August 8, 2021, using CSS app data and previously described methodology35. The method uses both positive SARS-CoV-2 test results and symptom reports from app users, to estimate incidence. Data are stratified by age and vaccination status to ensure estimates made from the CSS app population are representative of the wider population.
Using COG-UK data to estimate the proportion of Delta in circulation in each region per day, incidence estimates were decomposed into two incidence time-series per region, one for ‘non-Delta’ (in the timeframe considered here, predominantly Alpha [Supplementary Table S1]) and one for Delta, assuming that the two incidence time-series should sum to match total incidence. R(t) was estimated separately for non-Delta and Delta variants, using previously described methodology35. Briefly, we used the relationship It+1 = It exp(μ (R(t) – 1)), where 1/μ is the serial interval and It the incidence on day t. We modelled the system as a Poisson process and assumed the serial interval was drawn from a gamma distribution with α = 6.0 and β = 1.5; and used Markov Chain Monte-Carlo to estimate R(t). We compared both multiplicative and additive differences of the new and old R(t) values for days when the Delta proportion in a region was > 3%.
Reinfection during rise of Delta variant
Reinfection was defined as previously36 (presence of two positive PCR or LFAT tests separated by > 90 days, with an asymptomatic period of ≥ 7 days before the second positive test). To assess risk of reinfection during the Delta variant timeframe we performed ecological studies for each region, examining the Spearman correlation between the proportion of circulating SARS-CoV-2 due to Delta (Supplementary Table S5, Supplementary Figure S1) and number of reinfections per week over time, assessed from 10 weeks prior to Delta prevalence of 25% until 10 weeks after Delta prevalence of 75% (22 weeks); and between the number of positive tests reported through the app and the number of reinfections. We compared the bootstrapped distributions of these two correlations in each region, using the Mann–Whitney U test (Supplementary Table S5).
Post-vaccination infection during Delta period
We analysed 515,138 app users who reported vaccination with BNT162b2 (BioNTech-Pfizer) or ChAdOx1 nCoV-19 (Oxford-Astra Zeneca) and were subsequently tested for SARS-CoV-2 (PCR or LFAT) 14–60 days after either first or second vaccination (assessed separately) after 26 May 202136. Age was restricted to 20–65 years, as most individuals > 65 years were vaccinated and most individuals < 20 years unvaccinated during the time of analysis, biasing the control groups for these ages. Users who had reported SARS-CoV-2 infection previously were excluded. Unvaccinated users reporting SARS-CoV-2 test results in the same or following week as a vaccinated app user served as controls. In the event of multiple tests logged for an individual vaccinated user, either the first positive or the last negative result was selected. For each vaccine and per dose, we modelled rates of positive testing in vaccinated versus unvaccinated individuals, using Poisson regressions adjusting for number of tests, age, co-morbidities, sex, healthcare worker status, obesity, and weekly incidence in the community (by controlling for the date of the test). The adjusted risk reduction was then calculated as RR = riskratioi,n − 1, where i is the vaccine type, and riskratio is the ratio of infection rates in vaccinated individuals compared to unvaccinated individuals, derived from our Poisson model.
Ethics
Ethics approval was granted by KCL Ethics Committee (reference LRS-19/20-18210).
Data availability
Data collected in the COVID Symptom Study smartphone app can be shared with other health researchers through the UK National Health Service-funded Health Data Research UK and Secure Anonymised Information Linkage consortium, housed in the UK Secure Research Platform (Swansea, UK). Anonymised data are available to be shared with researchers according to their protocols in the public interest, and an administrative fee might apply. Link at https://web.www.healthdatagateway.org/dataset/594cfe55-96e3-45ff-874c-2c0006eeb881. Information on anonymized SARS-CoV-2 test results is recorded as positive/negative/invalid, and sequencing data were not captured.
Abbreviations
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- IQR:
-
Inter-quartile range
- LC28:
-
Long COVID-19 with duration of symptoms ≥ 28 days
- LFAT:
-
Lateral flow antigen test
- ONS:
-
Office for National Statistics (UK)
- OR:
-
Odds Ratio
- PCR:
-
Polymerase chain reaction
- SARS-CoV-2:
-
Severe acute respiratory syndrome‐related coronavirus 2
- UK:
-
United Kingdom of Great Britain and Northern Ireland
- WHO:
-
World Health Organisation
References
Forni, D., Cagliani, R., Pontremoli, C., Clerici, M. & Sironi, M. The substitution spectra of coronavirus genomes. Brief. Bioinform. https://doi.org/10.1093/bib/bbab382 (2021).
Forni, D. et al. Antigenic variation of SARS-CoV-2 in response to immune pressure. Mol. Ecol. https://doi.org/10.1111/mec.15730 (2021).
Anastassopoulou, C., Gkizarioti, Z., Patrinos, G. P. & Tsakris, A. Human genetic factors associated with susceptibility to SARS-CoV-2 infection and COVID-19 disease severity. Hum. Genomics https://doi.org/10.1186/s40246-020-00290-4 (2020).
Lopez Bernal, J. et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2108891 (2021).
Public Health England. SARS-CoV-2 variants of concern and variants under investigation in England: technical briefing 15. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/993879/Variants_of_Concern_VOC_Technical_Briefing_15.pdf. (2021).
[ECDC] European Centre for Disease Prevention and Control. Threat assessment brief: emergence of SARS-CoV-2 B.1.617 variants in India and situation in the EU/EEA. https://www.ecdc.europa.eu/en/publications-data/threat-assessment-emergence-sars-cov-2-b1617-variant. (2021).
[ECDC] European Centre for Disease Prevention and Control. Confirmed cases of COVID-19 variants identified in UK. https://www.gov.uk/government/news/confirmed-cases-of-covid-19-variants-identified-in-uk. (2021).
Keeling, M. J. Estimating the Transmission Advantage for B. 1.617. 2. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/993156/S1269_WARWICKTransmission_Advantage.pdf.
Luo, C. H., Morris, C. P., Sachithanandham, J., et al. Infection with the SARS-CoV-2 Delta Variant is Associated with Higher Infectious Virus Loads Compared to the Alpha Variant in both Unvaccinated and Vaccinated Individuals. medRxiv 2021: 2021.08.15.21262077.
Ong, S. W. X. et al. Clinical and virological features of SARS-CoV-2 variants of concern: a retrospective cohort study comparing B.1.1.7 (Alpha), B.1.315 (Beta), and B.1.6.17.2 (Delta). Clin. Infect. Dis. https://doi.org/10.1093/cid/ciab721 (2021).
Twohig, K. A. et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B16172) compared with alpha (B117) variants of concern: A cohort study. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(21)00475-8 (2021).
Puranik, A., Lenehan, P. J., Silvert, E., et al. Comparison of two highly-effective mRNA vaccines for COVID-19 during periods of Alpha and Delta variant prevalence. medRxiv : the preprint server for health sciences. https://doi.org/10.1101/2021.08.06.21261707(2021).
Planas, D. et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature https://doi.org/10.1038/s41586-021-03777-9 (2021).
Our World in Data. SARS-CoV-2 variants in analyzed sequences, United Kingdom. https://ourworldindata.org/grapher/covid-variants-area?country=~GBR.
Graham, M. S. et al. Changes in symptomatology, reinfection, and transmissibility associated with the SARS-CoV-2 variant B.1.1.7: an ecological study. Lancet Public Health https://doi.org/10.1016/S2468-2667(21)00055-4 (2021).
Menni, C. et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: A prospective observational study. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(21)00224-3 (2021).
Sudre, C. H. et al. Author Correction: Attributes and predictors of long COVID. Nat. Med. https://doi.org/10.1038/s41591-021-01361-2 (2021).
Lam-Hine, T. et al. Outbreak Associated with SARS-CoV-2 B.1.617.2 (Delta) Variant in an Elementary School—Marin County, California, May–June 2021. MMWR Morbidity Mortality Weekly Rep. 70, 1. https://doi.org/10.15585/mmwr.mm7035e2 (2021).
Chadeau-Hyam, M., Wang, H., Eales, O., et al. REACT-1 study round 14: High and increasing prevalence of SARS-CoV-2 infection among school-aged children during September 2021 and vaccine effectiveness against infection in England. medRxiv 2021: 2021.10.14.21264965.
Thompson, E. J., Williams, D. M., Walker, A. J., et al. Risk factors for long COVID: analyses of 10 longitudinal studies and electronic health records in the UK. https://doi.org/10.1101/2021.06.24.21259277.
Vöhringer, H. S. et al. Genomic reconstruction of the SARS-CoV-2 epidemic in England. Nature https://doi.org/10.1038/s41586-021-04069-y (2021).
Molteni E, Sudre CH, Canas LS, et al. Illness characteristics of COVID-19 in children infected with the SARS-CoV-2 Delta variant. medRxiv 2021.
Spicer, K. B., Glick, C., Cavanaugh, A. M. & Thoroughman, D. Protective immunity after natural infection with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)—Kentucky, USA, 2020. Int. J. Infect. Dis. https://doi.org/10.1016/j.ijid.2021.10.010 (2021).
Iversen, K. et al. Seroprevalence of SARS-CoV-2 antibodies and reduced risk of reinfection through 6 months: a Danish observational cohort study of 44000 healthcare workers. Clin. Microbiol. Infect. https://doi.org/10.1016/j.cmi.2021.09.005 (2021).
Sheikh, A., McMenamin, J., Taylor, B. & Robertson, C. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet 397, 1. https://doi.org/10.1016/S0140-6736(21)01358-1 (2021).
Goldberg, Y. et al. Waning immunity after the BNT162b2 vaccine in Israel. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2114228 (2021).
Ramasamy, M. N. et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet https://doi.org/10.1016/S0140-6736(20)32466-1 (2020).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N. Engl. J. Med. 383, 1. https://doi.org/10.1056/NEJMoa2034577 (2020).
Tenforde, M. W. et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA https://doi.org/10.1001/jama.2021.19499 (2021).
Menni, C. et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat. Med. https://doi.org/10.1038/s41591-020-0916-2 (2020).
Canas, L. S., Österdahl, M. F., Deng, J., et al. Disentangling post-vaccination symptoms from early COVID-19. medRxiv 2021: 2021.07.21.21260906.
Drew, D. A. et al. Rapid implementation of mobile technology for real-time epidemiology of COVID-19. Science https://doi.org/10.1126/science.abc0473 (2020).
Murray, B. et al. Accessible data curation and analytics for international-scale citizen science datasets. Sci. Data 8, 297 (2021).
Molteni, E. et al. Symptoms and syndromes associated with SARS-CoV-2 infection and severity in pregnant women from two community cohorts. Sci. Rep. https://doi.org/10.1038/s41598-021-86452-3 (2021).
Varsavsky, T. et al. Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study. Lancet Public Health https://doi.org/10.1016/S2468-2667(20)30269-3 (2021).
Antonelli, M. et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(21)00460-6 (2021).
Acknowledgements
This research was funded in part by the Wellcome Trust (WT213038/Z/18/Z). This work is also supported by the Wellcome Engineering and Physical Sciences Research Council Centre for Medical Engineering at King’s College London (WT203148/Z/16/Z) and the UK Department of Health via the National Institute for Health Research (NIHR) comprehensive Biomedical Research Centre award to Guy’s and St Thomas’ NHS Foundation Trust in partnership with King’s College London and King’s College Hospital NHS Foundation Trust, the Medical Research Council (MRC), and British Heart Foundation. SO and MM are supported by the UK Research and Innovation London Medical Imaging and Artificial Intelligence Centre for Value Based Healthcare. SO is supported by the Wellcome Flagship Programme (WT213038/Z/18/Z). EM is funded by an MRC Skills Development Fellowship Scheme at King’s College London. CHS is supported by the National Core Studies, an initiative funded by United Kingdom Research and Innovation, NIHR, and the Health and Safety Executive, and funded by MRC (MC_PC_20030). CHS is also supported by an Alzheimer’s Society Junior Fellowship (ASJF-170–11). ZOE Limited supported all aspects of building and running the application and service to all users worldwide. For the purpose of open access, the authors have applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. COG-UK is supported by funding from the Medical Research Council (MRC) part of UK Research & Innovation (UKRI), the National Institute of Health Research (NIHR) [grant code: MC_PC_19027], and Genome Research Limited, operating as the Wellcome Sanger Institute. The authors are grateful to Michael Absoud and Sunil Bhopal for constructive comments on the paper. For the purpose of open access, the authors have applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Funding
UK Government Department of Health and Social Care, Wellcome Trust, UK Engineering and Physical Sciences Research Council, UK Research and Innovation London Medical Imaging & Artificial Intelligence Centre for Value Based Healthcare, UK National Institute for Health Research, UK Medical Research Council, British Heart Foundation, Alzheimer’s Society, and ZOE Limited.
Author information
Authors and Affiliations
Consortia
Contributions
K.K., C.H.S., M.S.G., S.O., T.D.S., C.J.S., and E.L.D. contributed to study concept and design. C.H.S., A.M., B.M., J.C., The COG-UK Consortium, JW, TDS, CJS, and SO contributed to acquisition of data. K.K., C.H.S., M.S.G., A.M. and E.L.D. contributed to data analysis and verified the underlying data. K.K., E.M., M.S.G., CHS and E.L.D. contributed to initial drafting of the manuscript. All authors contributed to interpretation of data and critical revision of the manuscript. C.J.S., T.D.S., S.O. and E.L.D. contributed to study supervision. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
Tim D Spector is co-founder shareholder and consultant of ZOE Limited. Jonathan Wolf, Anna May, Ben Fox, and Joan Capdevila Pujol are employed at ZOE Limited. All the other authors declare no competing interests. Specifically, SO, MM, EM, and CHS are funded by non-competing trusts (see acknowledgments in the manuscript).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kläser, K., Molteni, E., Graham, M. et al. COVID-19 due to the B.1.617.2 (Delta) variant compared to B.1.1.7 (Alpha) variant of SARS-CoV-2: a prospective observational cohort study. Sci Rep 12, 10904 (2022). https://doi.org/10.1038/s41598-022-14016-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-14016-0
This article is cited by
-
Impact of vitamin D supplementation on the clinical outcomes of COVID-19 pneumonia patients: a single-center randomized controlled trial
BMC Complementary Medicine and Therapies (2024)
-
Dynamic SARS-CoV-2 surveillance model combining seroprevalence and wastewater concentrations for post-vaccine disease burden estimates
Communications Medicine (2024)
-
Reproduction number projection for the COVID-19 pandemic
Advances in Continuous and Discrete Models (2023)
-
Comparing SARS-CoV-2 variants among children and adolescents in Germany: relative risk of COVID-19-related hospitalization, ICU admission and mortality
Infection (2023)
-
Management of Multisystem Inflammatory Syndrome in Children (MIS-C) in resource limited settings: The Kenyan Experience
Pediatric Rheumatology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.