Abstract
New SARS-CoV-2 may pose problems in controlling the COVID-19 pandemic for public health. We aimed to assess and compare the symptoms and severity of cases due to the Alpha and Delta variant dominance periods, taking into account the effect of COVID-19 vaccination. A prospective epidemiological study of SARS-CoV-2 in Lleida was made to determine differences between Alpha and Delta variants periods. We assessed symptoms, specific comorbidities, sociodemographic information and vaccination status. Bivariate and logistic regression analyses were used to estimate the adjusted odds ratio (aOR) and 95% confidence intervals (CI) to investigate the relationship between symptoms and severity and the variants. Alpha variant period compared to the Delta showed an increased risk of ICU admission (aOR 2.0; 95% CI 1.2–2.3) and death (aOR 2.6; 95% CI 1.8–3.9) and cases were associated with people aged > 85 years (aOR 2.1; 95% CI 1.7–2.6) and partially vaccinated (aOR 5.6; 95% CI 3.2–9.9) and unvaccinated people (aOR 27.8; 95% CI 19.7–40.5). Fever, cough and vomiting were significantly associated with the Alpha variant compared to the Delta (aOR 1.6 (95% CI 1.5–1.7), 2.0 (95% CI 1.9–2.2) and 2.5 (95% CI 2.2–2.9, respectively). Our results show that the severity and profile of clinical symptoms varied according to the variant. The risk of ICU admission and death was higher in the Alpha period compared to the Delta as it affected the elderly and cases were less vaccinated.
Similar content being viewed by others
Introduction
The emergence of new variants of SARS-CoV-2 has supposed a problem in controlling the COVID-19 pandemic. The COVID-19 variant of concern, B.1.1.7, colloquially known as Alpha, was first identified in the United Kingdom1. Then a new variant was discovered in India. The variant of concern B.1.617.2 was called Delta2.
Studies have analyzed the main symptoms of the Alpha variant by patient characteristics and the role of vaccination3. Some studies4,5 found an association between the Alpha variant and an increase in hospitalization, ICU admission and mortality. However, Veneti et al.6 found no differences in the risk of hospitalization between reported cases of the SARS-CoV-2 Delta and Alpha variants in Norway. Burki7 concluded that the Delta variant was almost twice as likely to lead to hospitalization as infection with the Alpha variant. Therefore, some studies have come to different conclusions.
Vaccination has had an important impact on virus transmission. Studies8,9 have shown the effectiveness of the COVID-19 vaccine in preventing severe cases due to SARS-CoV-2 and concluded that effectiveness may decrease after 6 months of follow-up even though the vaccine remains highly efficacious in preventing serious cases of COVID-1910. Harder et al.11 compared the effectiveness of the vaccine between the Alpha and Delta variants and found that the strength of the vaccine was reduced by 10–20%, but maintained full effectiveness against severe COVID-19. In Spain, the first doses of the vaccines were administrated at the beginning of January 2021. The ≥ 85 and 75–84 years age groups were the first to receive the vaccines12.
Studies of the Alpha and Delta variants have found differing outcomes. However, they mostly concluded that the Alpha variant increased the risk of severe cases, although some studies resulted in different conclusions. Our study added and analyzed all symptoms seen in recorded patients during the dominance of each variant and their vaccination status.
The aim of this study was to assess and compare the symptoms and severity of COVID-19 cases in the months when the Alpha variant predominated, taking into account the effect of COVID-19 vaccination. We also compared the differing patient profiles and comorbidities between the Alpha and Delta periods.
Methods
We made a prospective epidemiological study of SARS-CoV-2 in the province of Lleida (Spain) to determine differences between the periods of predominance of the Alpha and Delta variants. We analyzed symptoms, specific comorbidities, sociodemographic information and the COVID-19 vaccination status. The main sources of information were recorded cases from the Lleida and Alt Pirineu-Aran epidemiological service, which is part of the Catalan Department of Health. SARS-CoV-2 cases were detected by PCR (polymerase chain reaction) and antigen tests. Cases were validated, studied and controlled by epidemiological professionals in order to monitor the disease and observe the evolution of the pandemic in the two outbreaks.
Data
The data collected correspond to new cases from two consecutive waves of the pandemic with circulation of the Alpha and Delta variants. As we did not know the genome sequence for all confirmed cases, each wave was characterized, at baseline, by a prevalence of 50% of the sequenced genome for the respective variant (Alpha or Delta) and, subsequently by a prevalence of > 90% during peak hospital admissions. Data were collected by Department of Health public health officials by telephone interview with each patient and checking and/or reviewing clinical records, as is normal for data collection by the public epidemiological surveillance system. The first period comprises records from January 1, 2021 to March 31, 2021, with circulation of the Alpha variant in the Lleida region. The second period, with circulation of the Delta variant, comprises records from April 1, 2021 to July 31, 202111. In the second period, the government permitted mobility, social contacts and the opening of night clubs. The study variables were variant dominance period (Alpha, Delta); age group (0–14, 15–34, 35–44, 45–54, 55–64, 65–74, 75–84, ≥ 85 years); sex (male, female); asymptomatic; hospitalized; ICU; death; fever; cough; pneumonia; sore throat; shivers; dyspnea; vomiting; diarrhea; respiratory distress syndrome; acute renal failure; cardiovascular disease; neurological disease; vaccinated (fully, half, non). Patients were considered fully vaccinated only if two vaccine doses were received and the time between the second vaccination and the onset of COVID-19 was > 14 days. Patients were considered partially vaccinated if only one effective vaccine dose was received. Patients were considered unvaccinated if no vaccine had been received or the first vaccination was given < 14 days before the onset of COVID-19.
Statistics
We compared SARS-CoV-2 cases during the predominance of the Alpha variant with the predominance of the Delta variant. We compared sociodemographic information, symptoms, risk factors of the patients and the effect of vaccination. In the first analysis, crude odds ratios (OR) were used to compare the differences in positive cases between the variants.
A bivariate analysis was made to investigate relationships between the dependent variable (the Alpha or Delta variants), and independent variables (UCI, death, sociodemographic data, symptoms, risk factors and vaccination status).
The patient profile of the Alpha variant compared with the Delta variant as a reference category was analyzed using logistic regression to estimate probabilities, OR and their corresponding 95% confidence intervals (CI).
The logistic regression analysis was based on forward selection. This involves starting with no variables in the model, adding the variable (if any) whose inclusion gives the most significant improvement to the fit, and repeating this process until none improve the model.
Ethics statement
All data were anonymized to protect patient privacy and confidentiality. This study was part of the public health response to coronavirus outbreaks. This project was approved by the reference ethics committee (Committee of Ethics and Clinical Research of Lleida—CEIC). The patients were interviewed by telephone to obtain the COVID-19 symptoms and vaccine information. They were informed about this study in this interview, and they provided informed consent during enrolment. All methods were carried out in accordance with relevant guidelines and regulations.
Results
The overall data set consisted of 27,011 SARS-CoV-2 cases confirmed by PCR and antigen tests. When the Alpha variant was predominant, 13,037 cases were detected, and when the Delta variant predominated 13,974 cases were detected (Fig. 1).
Bivariate analysis
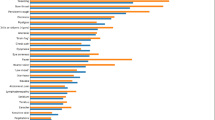
Patient profiles, symptoms, comorbidities and the vaccination effect between the Delta and Alpha variants were analyzed and compared (Table 1). During the Alpha period, 6645 (51%) women were recorded compared with 6727 (48.1%) in the Delta period (P < 0.001). There were differences between age groups: during the Alpha period there were 2948 (23%) cases in the 15–34 age group compared with 5308 (38%) during the Delta period. However, in the 55–64 years and older age groups, the number of cases of the Delta variant decreased compared with the Alpha variant (P < 0.001).
Hospitalized cases were higher during the Alpha period (n = 491; 3.8%) than in the Delta period (n = 245; 1.8%) and 56 (0.4%) cases required ICU admission during the Alpha period and 25 (0.2%) during the Delta period (P < 0.001). Death was also significant with 161 (1.2%) cases related to the Alpha variant and 36 (0.3%) to the Delta variant (P < 0.001).
Regarding symptoms, the P-value was significant for all symptoms (P < 0.001). Major differences between variants were observed in the number of patients with fever and cough. There were also significant differences related to comorbidities. Vaccination also was significant (P < 0.001) in all categories. The number of fully-vaccinated positive cases increased notably in the Delta period.
Logistic regression model
Sociodemographic information, symptoms and comorbidities differed widely (Table 2). Male sex was significant during the Alpha period (aOR 0.9; 95% CI 0.9–1.0). The 15–34 years age group showed the greatest significance [15–34] (aOR 0.5; 95% CI 0.4–0.5). The 35–44 years age group was also significant (aOR 0.7; 95% CI 0.7–0.8). There were significant differences in the elderly (aOR 2.7; 95% CI 2.2–3.2). Differences in hospitalization were not significant, but the risk of ICU admission was higher during the Alpha variant period (aOR 1.7; 95% CI 1.1–2.7) and the aOR for death was also significant (P = 2.7, 95% CI 1.9–4.0).
Fever and cough showed significant results with aORs of 3.7 (95% CI 3.4–4.0) and 4.3 (95% CI 4.0–4.6). Sore throat was also significant with a higher risk with the Alpha variant (aOR 1.2, 95% CI 1.1–1.2). Digestive symptoms were also. The OR for vomiting was 2.7 (95% CI 2.4–3.2) and for diarrhea it was 0.6 (95% CI: 0.5–0.7). Acute renal failure was also significant (aOR 2.9, 95% CI 1.4–7.3).
Respiratory and cardiovascular diseases were significant (aOR 3.0; 95% CI 1.7–6.3 and aOR 1.3; 95% CI 1.1–1.5, respectively). Finally, vaccination also produced significant results. The aOR for partially-vaccinated cases was 5.6 (95% CI 3.2–9.2) and for non-vaccinated cases it was 35.7 (95% CI 25.7–51.3).
Discussion
The risk of ICU admission and death was higher during the Alpha period compared to the Delta period after adjustment in the regression model for the importance effect of age and partial vaccination or lack of vaccination. In addition, in cases in Alpha period with respect to the Delta, there were some clinical differences, such as a higher percentage of fever, cough and vomiting.
This study was based on a previous one13, which described reported cases and identified disease severity risk factors in the first wave in Spain but did not compare this with waves caused by other variants. A later study in Navarra found that the emergence of the Delta variant in Spain was associated with an increased proportion of cases in young people at a time when increased vaccination coverage led to increases in mobility and social interaction, and the relaxation of some preventive measures14. Another early study analyzed the transmissibility and global spread of COVID-19 variants and their differences in terms of effects. Twohig et al.15 analyzed the risk of hospital admission risk from the Delta and Alpha variants and found higher hospital admission and emergency care risks in unvaccinated patients during the Delta period. mRNA vaccines were shown to significantly reduce the risk of hospitalization and death. Bernal et al.16 analyzed the effectiveness of COVID-19 vaccines against the Delta variant and suggested a lower degree of protection than against the Alpha variant, even though they still guaranteed a high level of effectiveness.
Studies have analyzed and compared the symptoms and effectiveness of the vaccine against the COVID-19 variants, with differing results. Some studies found that the Alpha variant may increase the risk of ICU admission and mortality4,5, while others concluded there were no significant differences6. However, after reviewing earlier literature about the effectiveness of vaccines and the new variants, most studies have suggested that vaccine protection was higher against the Alpha variant but that their effectiveness in preventing severe cases caused by the Delta variant remained high.
One of the most significant results was in the 15–34 years age group17, in which the risk from the Delta variant was higher. Similar results were seen in the 35–44 and 65–74-years age groups. The latter group started to receive the first vaccine doses just when the Delta variant started to become predominant18. Therefore, they were still exposed to the virus. However, older people, specifically the ≥ 85 years age group, had a higher risk from the Alpha variant than from the Delta variant because, in the earlier period they had not received two doses of the vaccine19. During the wave caused by the Delta variant, these groups were fully vaccinated.
The number of cases requiring ICU admission, and mortality, during the Alpha period was higher. The logistic regression analysis confirmed the higher risk from the Alpha variant. The risk of ICU admission due to the Alpha variant was double the risk in the Delta period20,21. Mortality was also higher in the Alpha period, perhaps because the Alpha variant was more aggressive4,5.
The most significant symptoms observed during the Alpha period were fever and cough, which may indicate a higher degree of severity22. The incidence of vomiting was also higher with the Alpha variant, but this may not be related to the risk of hospitalization, ICU admission or death23. These differences suggest that symptoms could vary depending on the variant given that the genetic composition of the COVID-19 variants differs24.
Outcomes in partially and unvaccinated patients were also significant compared with those fully-vaccinated. Partial vaccination signified a higher risk compared with full vaccination during the Alpha period, as did non-vaccination. The risk in unvaccinated patients was significantly higher than for the fully-vaccinated. These outcomes suggest a high effectiveness of current vaccines against severity and death25.
This study has some limitations. The transition between the predominance of the Alpha and Delta variants may mean some cases are included in the wrong period. Some asymptomatic patients may have developed symptoms after the interview and not been registered. Some symptoms could also have appeared after the interview and not been recorded. Likewise, the COVID history could not be taken into account due to difficulties in accessing this information. The logistic regression model took into account the main variables involved, such as vaccination and morbidity, but there could still be a residual confounding effect in the results.
In conclusion, our results suggest that more severe cases appeared during the predominance of the Alpha variant. This may show that the Alpha variant is more aggressive than the Delta, depending on the case. The risk of ICU admission, and deaths, were higher in the Alpha period, as were fever, cough, and vomiting. The lack of vaccination was the main risk factor in people infected by the Alpha variant, suggesting vaccines are effective in avoiding UCI admission and death.
These results show further study of vaccine effectiveness against new variants are necessary and the importance of vaccines in maintaining high levels of protection.
Data availability
The dataset is available from the corresponding author upon reasonable request.
References
Xie, X., Lewis, T.-J., Green, N. & Wang, Z. Phylogenetic network analysis revealed the recombinant origin of the SARS-CoV-2 VOC202012/01 (B.1.1.7) variant first discovered in UK. BioRxiv. https://doi.org/10.1101/2021.06.24.449840v2 (2021).
Moona, A. A., Daria, S., Asaduzzaman, M. & Islam, M. R. Bangladesh reported delta variant of coronavirus among its citizen: Actionable items to tackle the potential massive third wave. Infect. Prev. Pract. 3(3), 100159 (2021).
Eyre, D. W. et al. Effect of covid-19 vaccination on transmission of alpha and delta variants. N. Engl. J. Med. 386(8), 744–756. https://doi.org/10.1056/NEJMoa2116597 (2022).
Grint, D. J. et al. Severity of severe acute respiratory system coronavirus 2 (SARS-CoV-2) alpha variant (B.1.1.7) in England. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciab754 (2021).
Pascall, D. J. et al. The SARS-CoV-2 Alpha variant causes increased clinical severity of disease. MedRxiv. https://doi.org/10.1101/2021.08.17.21260128v1 (2021).
Veneti, L. et al. No difference in risk of hospitalisation between reported cases of the SARS-CoV-2 Delta variant and Alpha variant in Norway. MedRxiv https://doi.org/10.1101/2021.09.02.21263014v1 (2021).
Burki, T. K. Lifting of COVID-19 restrictions in the UK and the Delta variant. Lancet Respir. Med. 9(8), e85 (2021).
Zanettini, C. et al. Influenza vaccination and COVID19 mortality in the USA. MedRxiv. 7, 001656 (2020).
Kaplan, R. M. & Milstein, A. Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. Proc. Natl. Acad. Sci. USA. 118(10), 2021726118 (2021).
Thomas, S. J. et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine through 6 months. N. Engl. J. Med. 385(19), 1761–1773 (2021).
Harder, T. et al. Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection with the Delta (B.1.617.2) variant: Second interim results of a living systematic review and meta-analysis. Eurosurveillance. 26(41), 2100920 (2021).
Martínez-Baz, I. et al. Effectiveness of COVID-19 vaccines in preventing SARS-CoV-2 infection and hospitalisation, Navarre, Spain. Eurosurveillance. 26(21), 2100438 (2021).
Redondo-Bravo, L. et al. The first wave of the COVID-19 pandemic in Spain: Characterisation of cases and risk factors for severe outcomes. Eurosurveillance. 25(50), 2001431 (2020).
Trobajo-Sanmartín, C. et al. Differences in transmission between SARS-CoV-2 Alpha (B.1.1.7) and Delta (B.1.617.2) variants. Microbiol. Spectr. 10(2), 22 (2022).
Twohig, K. A. et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: A cohort study. Lancet Infect. Dis. 22(1), 35–42 (2021).
Lopez Bernal, J. et al. Effectiveness of covid-19 vaccines against the B.1.617.2 (Delta) variant. N. Engl. J. Med. 385(7), 585–594 (2021).
Jantzen, R. et al. Epidemiological characteristics of the COVID-19 spring outbreak in Quebec, Canada: A population-based study. BMC Infect. Dis. 21(1), 435 (2021).
Shiehzadegan, S., Alaghemand, N., Fox, M. & Venketaraman, V. Analysis of the Delta variant B.1.617.2 COVID-19. Clin. Pract. 11(4), 778–784 (2021).
Teo, S. P. Review of COVID-19 vaccines and their evidence in older adults. Ann. Geriatr. Med. Res. 25(1), 4 (2021).
Veneti, L. et al. Increased risk of hospitalisation and intensive care admission associated with reported cases of SARS-CoV-2 variants B.1.1.7 and B.1.35.1 in Norway, December 2020–May 2021. PLoS ONE 16(10), e0258513 (2021).
Str, K. et al. Impact of the Alpha VOC on disease severity in SARS-CoV-2-positive adults in Sweden. J. Infect. 84(1), e3–e5 (2021).
Tsai, S.-C., Chang, W.-W. & Lee, W.-S. Analysis of an outbreak of COVID-19(alpha-variant) with rapid progression to mortality in Taipei, Taiwan. J Infect. 84(1), e33–e34 (2021).
Redd, W. D. et al. Prevalence and characteristics of gastrointestinal symptoms in patients with severe acute respiratory syndrome coronavirus 2 infection in the United States: A multicenter cohort study. Gastroenterology 159(2), 765–767 (2020).
Jewell, B. L. Monitoring differences between the SARS-CoV-2 B117 variant and other lineages. Lancet Public Health. 6(5), e267–e268 (2021).
Puranik, A. et al. Comparison of two highly-effective mRNA vaccines for COVID-19 during periods of Alpha and Delta variant prevalence. MedRxiv 383, 1920 (2021).
Funding
This work was supported by Contract 2019-DI-43 of the Industrial Doctorate Program of the Government of Catalonia, by the Spanish Ministry of Science and Innovation under Contract PID2020-113614RB-C22 and by the Lleida Biomedical Research Institute (IRB Lleida). Some authors are members of the 2014-SGR163 research group, funded by the Generalitat de Catalunya.
Author information
Authors and Affiliations
Contributions
D.F., J.M., F.S. and P.G. designed the study. D.F. and R.S. analyzed the data. D.F. wrote the manuscript. J.M., F.S. and P.G. supervised the study and helped interpret the data. C.M. and S.G. collected data and helped analyze them. All authors revised the manuscript and approved it for submission. The authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Florensa, D., Mateo, J., Spaimoc, R. et al. Severity of COVID-19 cases in the months of predominance of the Alpha and Delta variants. Sci Rep 12, 15456 (2022). https://doi.org/10.1038/s41598-022-19125-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19125-4
This article is cited by
-
Mechanical ventilation as a major driver of COVID-19 hospitalization costs: a costing study in a German setting
Health Economics Review (2024)
-
COVID-19 in the Netherlands: lessons from a nationwide query of dutch autopsy, histology, and cytology pathological reports
Virchows Archiv (2024)
-
Epidemiological drivers of transmissibility and severity of SARS-CoV-2 in England
Nature Communications (2023)
-
COVID-19 activity risk calculator as a gamified public health intervention tool
Scientific Reports (2023)
-
Impact of COVID infection on lung function test and quality of life
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.