Abstract
This study aimed to examine the association between meeting 24-h movement guidelines and cardiometabolic health in Chilean adults. We used cross-sectional data of 2618 adults from the Chilean National Health Survey 2016–2017. Meeting the 24-h movement guidelines was defined as ≥ 600 MET-min/week of physical activity; ≤ 8 h/day of sitting time; and 7 to 9 h/day of sleep duration. Cardiometabolic health indicators were body mass index, waist circumference, high triglycerides, high blood pressure, type 2 diabetes, metabolic syndrome, and risk of cardiovascular disease in a 10-year period. Meeting none out of three 24-h movement guidelines (vs all three) was associated with higher odds of overweight/obesity (OR 1.67; 95%CI 1.45 to 1.89), high waist circumference (1.65; 1.40 to 1.90), hypertension (2.88; 2.23 to 3.53), type 2 diabetes (1.60; 1.26 to 1.94), metabolic syndrome (1.97; 1.54 to 2.40) and risk of cardiovascular disease (1.50; 1.20, 1.80). Meeting one guideline (vs three) was associated with higher odds of five of out seven cardiometabolic indicators. Our study found that the composition of movement behaviors within a 24-h period may have important implications for cardiometabolic health.
Similar content being viewed by others
Introduction
From a movement perspective, the 24-h period is distributed among physical activity of various intensities (light, moderate and vigorous), sedentary behaviors and sleep duration. Engaging in sufficient levels of physical activity, limiting sitting time, and adequate sleep duration throughout the day have been associated with several health benefits across the lifespan1,2,3,4. Traditionally, studies have focused on investigating independent associations of physical activity, sitting time, and sleep duration with different health outcomes, or with only partial adjustment for time spent in other movement behaviors5. However, because recent studies revealed that these movement behaviors may interact with each other5, there is growing interest in an integrated approach to movement behavior studies. Previous studies have showed the independent and joint association of physical activity, sitting time, and sleep duration with poor cardiometabolic health indicators (i.e., adiposity level, HDL-cholesterol, and triglycerides)6,7,8.
The world’s first 24-h movement guidelines that integrate physical activity, sitting time, and sleep duration was published by Canada7,9, and soon after by Finland, New Zealand, Australia, and in some other countries10,11,12,13. As part of such efforts, the World Health Organization (WHO)14 and the National Sleep Foundation15 offer recommendations for physical activity and sleep duration for different age groups. Although no specific benchmark is available for sitting time, it is generally recommended to minimize time spent in sedentary behaviors, mainly sitting time16,17. To date, no evidence is available to understand the levels of movement behaviors in Latin American countries inhabitants based on internationally recognized benchmarks such as global physical activity guidelines or international sleep duration recommendations14,15. The guidelines represent a new approach to health promotion by including several general recommendations over a that include time spent in physical activity, sitting time, and sleep duration7.
Chile, a high-income Latin American country, has experienced a rapid epidemiological and nutritional transition18. Of note, the prevalence of overweight and metabolic syndrome (defined as a cluster of risk factors that include abdominal obesity, hypertension, hyperglycemia, and dyslipidemia) reached 78% and 13%, respectively19,20. Furthermore, the prevalence of type 2 diabetes mellitus increased from 4.2% in 2003 to 12.3% in 201619. These transitions might be partially explained by insufficient levels of physical activity, high sitting time, and inadequate sleep duration throughout the day. However, to our knowledge, no studies in Chile and Latin American region have examined the association of meeting 24-h movement guidelines with cardiometabolic health indicators.
In this study, we estimated the prevalence of meeting the general and specific combinations of 24-h movement guidelines by sociodemographic characteristics in Chilean adults. We also examined the associations of meeting general and specific-combinations of 24-h movement guidelines with cardiometabolic health indicators.
Material and methods
Study design and sample
We obtained data from the National Health Survey of Chile (NHS) 2016–201719. The NHS 2016–2017 was a cross-sectional, household survey that enrolled 6233 participants aged 15 years and older, who habitually reside in private homes located in urban and rural areas of the fifteen regions of Chile19. A complex, multistage sampling strategy was performed, considering counties as the primary sampling unit, households as the secondary sampling unit, and one participant from selected households as the tertiary sampling unit. Sampling weights from the survey accounted for differences in selection probability and non-response rates19. The post-stratification adjustment allowed to expand the sample to the estimated population in Chile. Data collection was carried out between August 2016 and March 2017. One participant per household was randomly selected using a Kish computational algorithm, and the response rate was 67%. Details on NHS 2016–2017 are available elsewhere19.
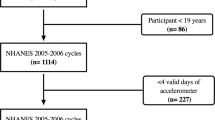
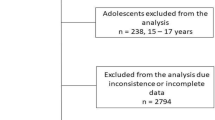
We excluded from our study adolescents aged 15–17 years (n = 238) and participants with missing or incomplete data of physical activity, sitting, sleep duration, or cardiometabolic health (n = 3377). Thus, our final analitical sample included 2618 adults (Fig. 1).
Assessing the 24-h movement guidelines
The Global Physical Activity Questionnaire (GPAQ) was used to assess physical activity and sitting time21,22. Developed by the WHO to measure population-level physical activity behaviors, the GPAQ uses standardized protocols and have shown to be a valid and reliable instrument to incorporate cultural and other differences21,22. Participants provided information on the duration, frequency, and intensity of physical activities performed in three domains (occupational, active commuting, and recreational). For each domain, metabolic-equivalent tasks (MET; where 1 MET = ~ 3.5 ml O2 kg−1 Min−1) were assigned according to the GPAQ protocol (4-METs was used for moderate and transport-related activities and 8-METs for vigorous activities). Total self-reported physical activity was calculated as the sum of MET-min/week−1 across all three domains. Participants were subsequently categorized as physically inactive (< 600 MET-min/week−1) or active (≥ 600 MET-min/week−1)23. Prevalences were based on 600 MET-min/week, which is approximately 150 min/week of moderate to vigorous physical activity24.
A single question from the GPAQ was used to measure sitting time25,26. The question was (i) “How much time do you usually spend sitting or reclining at work, at home, getting to and from places, or with friends including time spent sitting at a desk, sitting with friends, travelling in car, bus, or train, reading, playing cards or watching television, but do not include time spent sleeping on a typical day?” The participant responded in hours and minutes per day. This question has shown fair validity as was similarly reported in other countries (r = 0.23 to 0.26)25,26. We adopted the cutpoint of spend ≤ 8 h/day as guideline for sitting time7,9.
Self-reported sleep duration was assessed using two items, which asked participants to report their time spent sleeping on a typical day19. The sleep questionnaire consisted of two questions examining the sleep duration (hours/day): “How much time did you usually sleep on weekdays and weekends?” These questions were asked separately for weekdays and weekend days. The average sleep duration per day was calculated as follows = [(weekday time*5) + (weekend day time*2)]/719. Sleep duration values were dichotomized into meeting (≥ 7 and ≤ 9 h/day) or not meeting (< 7 or > 9 h/day) the sleep duration guidelines7,9.
Cardiometabolic health indicators
All measurements of cardiometabolic health were taken by previously trained professionals, using standard protocols19. The collected variables were body height and weight, waist circumference, triglycerides, blood pressure, and indicators for type 2 diabetes. In addition, based on the abovementioned cardiometabolic indicators, metabolic syndrome status and risk of cardiovascular disease were determined19.
Height was measured with a portable stadiometer with accuracy to the nearest 0.1 cm)19. Weight was measured with a digital scale (Tanita HD713) with an accuracy of 0.1 kg19. Weight measurements were taken barefoot, and the participants wearing light clothing. Body mass index (kg/m2) was calculated (weight [kg]/height [m2]) and participants were categorized as underweight/eutrophic (≤ 24.9 kg/m2) or overweight/obesity (≥ 25.0 kg/m2)19,27.
Waist circumference (cm) was measured midpoint between the lower coastal ridge and the upper margin of the superior iliac crest, using a flexible plastic tape19. Central obesity was defined as > 88 cm for women and > 102 cm for men19,28.
Venous blood samples were obtained after at least 8 h of fasting according standardized methods that have been described previously19. Participants with circulating triglycerides ≥ 150 mg/dL; HDL-C < 40 mg/dL for men, or < 50 mg/dL for women, or under drug treatment for cholesterol control were considered as high triglycerides19.
Blood pressure was measured with an Omron HEM-7200 Monitor and participants being seated19,29. Hypertension was defined by a measured systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg or self- reported antihypertensive treatment19.
Type 2 diabetes was determined by the presence of any of the following three criteria: (a) self-reported medical diagnosis of type 2 diabetes, (b) being under medical prescription for type 2 diabetes, (c) having fasting baseline glycaemic values > 126 mg/dL19.
Metabolic syndrome was defined according to the Chilean National Guidelines as having at least three of the following five components: high waist circumference (> 90 cm for men and > 80 cm for women), low HDL, hypertension (HDL-C 130/85 mmHG or under BP-lowering treatment) and impaired fasting glucose (IFG, glucose > 5.6 mmol/L or under treatment with antidiabetic drugs)19.
The risk of cardiovascular disease was evaluated by the Framingham Risk Score30, which was adapted for a Chilean population19,31,32. The Framingham Risk Score estimates the possibility of suffering a cardiovascular event or stroke in a 10-year period for people without a history of a previous cardiovascular event31. Participants were classified as low (< 5%) and middle/high (≥ 5%) risk of cardiovascular disease in a 10-year period19,31,32.
Sociodemographic correlates
Sociodemographic characteristics included sex (women/men), age (adults [18–64 years], and older adults [≥ 65 years])7, education level (up to primary [< 8 years of studies], secondary [between 8 and 12 years of studies] and beyond secondary [> 12 years of study]), monthly household income (stratified into tertiles: lowest [< US $310.00], medium [US $310.00–705.00], and highest [> US 705.00]), health insurance (private [Isapres], public [Fonasa] or other/none), and indigenous ethnicity (yes/no)19. In Chile, there are two main ethnicities; the first relates to Indigenous, and the second relates to those with other roots33. We also considered urban–rural geographic areas based on the Chilean population census19. Lifestyle risk factors included low consumption of fruits and vegetables (≤ 4 days per week)20, tobacco smoking (never/former or smoker)20, any alcohol consumption (using the short version of Alcohol Use Disorder Identifcation Test (AUDIT-C)34, adapted and validated for Chile residents35.
Statistical analysis
Descriptive data were presented as means, standard deviation (SD), frequency, and proportions according to sociodemographic correlates and cardiometabolic health. Each participant was categorized as either “meeting” or “not meeting” the 24-h movement guidelines as follows: (1) engage in ≥ 600 MET-min/week of physical activity; (2) spend ≤ 8 h/day in sitting time; and (3) obtain between 7 and 9 h/day of sleep duration7,9. The number of 24-h movement guidelines (0–3) met was created. For instance, the participants who met all three recommendations for physical activity, sitting time and sleep duration were categorized as meeting the integrated all three movement guidelines. In the specific-combination of 24-h movement guidelines, the proportion of participants meeting the physical activity, sitting time, and sleep duration and combinations of the guidelines (“none”, “only physical activity guideline met”, “only sitting time guideline met”, “only sleep duration guideline met”, “both the physical activity and sitting time guidelines met”, “both the physical activity and sleep duration guidelines met”, “both the sitting time and sleep duration guidelines met”, and “all three guidelines met”) were also calculated.
Multivariable logistic regression models were performed to estimate odds ratios (OR) and 95% confidence interval for the association between 24-h movement guidelines and cardiometabolic health indicators (dependent variable). Models were adjusted for the following potential confounders: region, sex, age, education level, monthly household income, health insurance, ethnicity, geographic area, fruits and vegetables consumption, tobacco consumption, and alcohol consumption. All analyses considered the NHS 2016–2017 complext sampling design19,20. Weights took into account the complex sampling design and the four levels of multistage sampling. All statistical analyses were conducted using SPSS V28 software (SPSS Inc., IBM Corp., Armonk, New York, NY, USA). A significance level of p < 0.05 was adopted.
Ethics approval and consent to participate
The NHS was funded by the Chilean Ministry of Health and approved by the Research Ethics Committee of the Faculty of Medicine of the Pontificia Universidad Católica de Chile (project number 16-019). Informed consent was obtained from all subjects and/or their legal guardian(s). All aspects of the study were in accordance with the Declaration of Helsinki and were performed in accordance with relevant guidelines and regulations.
Results
Participants sociodemograhic characteristics, lifestyle risk factors and cardiometabolic health indicators by 24-h movement guideline groups are presented in Table 1. The total number of participants included in the study was 2618 (1661; 63.4% women) with a mean age of 49.4 years (SD: 18.9). Overall, 25.1% were older adults (≥ 65 years), 54.8% had 8 to 12 years of education, 49.7% were in the lowest of household income group, 88.2% had access to health insurance, 88.3% were not of indigenous heritage, 82.7% lived in urban areas, 50.9% ate ≤ 4 days/week of fruit and vegetables, 73.2% were never/former tobacco smokers and 73.9% consumed alcohol. Most participants (76.4%) were classified as living with overweight/obesity. Almost half (46.1%) had high waist circumference, 33.7% had high triglycerides, 36.6% had hypertension, 15.5% had type 2 diabetes, 45.1% had metabolic syndrome, and 30.9% had a high risk of cardiovascular disease (Table 1). We did not observed differences (p > 0.05) between the participants who had complete data and those who were excluded from the analytical sample in terms of sex, age group and educational level (data not shown).
Participants meeting all three 24-guideline recommendations were more likely older, women, had lower household income and higher acces to public health insurance, indigenous, and living in rural area compared to those meeting none of the guidelines. Participants meeting all three 24-guideline were also more likely never smokers and had higher consumption of fruits and vegetable and alcohol compared to those meeting none of the guidelines (Table 1).
The prevalences of meeting general and specific combinations of the 24 h movement guidelines are presented in Table 2. Overall, 18.1% (95% CI 15.5, 20.7) of the sample met all three recommendations, 44.7% (95% CI 41.5, 47.9) met two, 33.1% (95% CI 29.8, 36.4) one, and 4.1% (95% CI 2.5, 5.7) met none of the three recommendations. We also found the following prevalences of meeting the specific guidelines: 22.0% (95% CI 18.1, 25.9) for physical activity, 15.2% (95% CI 11.7, 18.7) for sitting time, 6.5% (95% CI 4.1, 8.9) for sleep duration. In addition, 12.6% (95% CI 9.9, 15.3) of participants met physical activity and sitting time, 9.5% (95% CI 8.9, 10.1) met sleep duration and sitting time, while 12.0% (95% CI 8.1, 15.9) of participants met physical activity and sleep duration guidelines (Table 2).
Figures 2 and 3 show the proportion of participants meeting the general and specific combinations according sociodemographic characteristics. A total of 16.6% of men and 20.9% of women met all three recommendations, whereas 4.2% and 3.9% met none of the three recommendations, respectively. Older adults, women, those with up to primary education level, indigenous ethnicitiy and living in rural areas were more likely to meet all three 24-h movement guidelines.
Not meeting any 24-h movement guidelines was associated with higher odds of body mass index (OR 1.67; 95% CI 1.45 to 1.89), waist circumference (OR 1.65; 95% CI 1.40 to 1.90), hypertension (OR 2.88; 95% CI 2.23 to 3.53), type 2 diabetes (OR 1.60; 95% CI 1.26 to 1.94), metabolic syndrome (OR 1.97; 95% CI 1.54 to 2.40) and risk of cardiovascular disease (OR 1.50; 95% CI 1.20 to 1.80) compared to participants meeting all three 24-h movement guidelines. Compared to participants meeting all three 24-h movement guidelines, those meeting only one out of three guidelines had higher odds of triglycerides (OR 1.75; 95% CI 1.40 to 2.10), hypertension (OR 1.44; 95% CI 1.11 to 1.77), type 2 diabetes (OR 2.61; 95% CI 2.10 to 3.12), metabolic syndrome (OR 1.54; 95% CI 1.11 to 1.97), and risk of cardiovascular disease (OR 1.12; 95% CI 1.05 to 1.19). These associations were not statistically significant when compared participants meeting two vs all three guidelines (Table 3).
In the specific combinations of movement behaviors, meeting both physical activity and sleep duration was associated with higher odds of triglycerides (OR 1.15; 95% CI 1.06 to 1.24), hypertension (OR 1.75; 95% CI 1.40 to 2.10), type 2 diabetes (OR 1.50; 95% CI 1.23 to 1.77), and metabolic syndrome (OR 1.70; 95% CI 1.26 to 2.14) compared to met all three meeting 24-h movement guidelines. Furthermore, sleep duration and sitting time was associated with higher odds of five (waist circumference, triglycerides, hypertension, type 2 diabetes, and metabolic syndrome) of out seven cardiometabolic indicators compared to meeting all three recommendations. Meeting a combination of physical activity and sitting time vs meeting all three guidelines was not associated with a higher odds of all cardiometabolic health indicators (Table 3).
Meeting only the physical activity or only sitting time guidelines were associated with higher odds of six (except triglycecerides for physical activity, and waist circumference for sitting time) out of seven cardiometabolic indicators compared to meeting all three 24-h movement guidelines. Meeting only sleep duration guidelines vs meeting all three guidelines was not associated with a higher odds of all cardiometabolic health indicators (Table 3).
Discussion
Using a representative sample of adults from Chile, our study examined the associations between different combinations of meeting 24-h movement guidelines and cardiometabolic health in Chilean adults. We found that 18% of participants met all three 24-h movement guidelines. Participants meeting none out of three 24-h movement guidelines had higher odds of overweight/obesity, above threshold waist circumference, hypertension, type 2 diabetes, metabolic syndrome and risk of cardiovascular disease compared to meeting all three guidelines. The results also showed that meeting only one of the three 24-h movement guidelines was associated with higher odds of having several cardiometabolic risk factors compared to meeting all three guidelines.
This study is the first to examine the prevalence of 24-h movement guidelines in Chilean adults. Our study may also contribute to the scientific evidence regarding the association of movement behavior with health outcomes. In line with the findings of our analyses, two recent systematic reviews with compositional data analysis studies suggested that the composition of movement behaviors across the 24-h day (including physical activity, sitting time, and sleep duration) was associated with cardiometabolic health indicators (i.e., body mass index, waist circumference, triglycerides, hypertension)6,36.
To properly analyze movement behaviours constrained to, but filling, the 24-h period compositional analyses are recommended9,17. As none of the 24-h movement behaviors are independent of each other, and each of these behaviors has reciprocal effects on the others37, it has been recommended that it is unsuitable for studying their associations with important health implications separetely. Compositional data analysis methods allow for general 24-h time use among dissimilar movement behaviors to be assessed. Compositional approaches address multicollinearity issues between movement variables, ensure that estimates are fully adjusted for all-time habit, and allow for the inspection of mutual and synergistic associations of the 24-h movement behaviors with health indicators38. Our findings support the importance the association between the daily composition of movement behaviors and cardiometabolic health.
This study found that meeting none and one out of three recommendations was associated with a increased odds of cardiometabolic risk compared to meeting all three guidelines. Even specific combinations of meeting 2 out of 3 movement guidelines may not suffice to ensure optimal cardiometabolic health. Rao et al. also found a dose–response relationship between the number of movement guidelines met and physical, mental, and social health outcomes, such as physical activity, screen time, prosocial behaviours, and life satisfaction39. Similar results were also reported in children with a dose–response relationship between meeting movement guidelines and reduced risk of obesity40. Our study, however, showed that the combination of sufficient physical activity and lower sitting time may provide beneficial effects on maintaining cardiometabolic health. Meeting sleep duration and sitting time, on the other hand, was associated with higher odds of five (waist circumference, triglycerides, hypertension, type 2 diabetes, and metabolic syndrome) out of seven cardiometabolic indicators compared to meeting all three recommendations. Only meeting sleep duration guidelines, however, was not associated with cardiometablic health indicators compared to meeting all three guidelines.
In a recent study that examined the temporal and bidirectional relationship between objectively-measured sleep duration, sitting time, and physical activity, results indicated that higher levels of physical activity were related with adequade sleep duration, whereas increased sitting time was concomitant with poor sleep duration41, and these interactions may influence cardiometabolic health indicators. The complex temporal and reciprocal relationships between the 24-h movement behaviors remains poorly understood. Clarifying these interactions, and their relationship with other outcomes is essential for notifying targeted intervention approaches to increase the amount of people meeting all movement guidelines in order to reduce the burden of non-communicable diseases. The quantity of studies using compositional analyses and/or assessing compliance with the 24-h movement guidelines to analyse interactions with well-being is rapidly increasing. These findings are essential for understanding 24-h movement behaviors in Latin American adults and establishing evidence-based interventions for preventing cardiometabolic diseases.
The evidence presented in our study suggests that 18.1% of Chilean adults met the integrated 24-h movement behavior recommendations (i.e., a combination of physical activity, sitting time, and sleep duration recommendations). A recent systematic review also highlights the lack of data on compliance of movement guidelines in aduts and older adults6. Future studies are necessary to gain a more thorough understanding of the proportion of individuals who simultaneously achieve all of the movement behavior recommendations and the associations with cardiometabolic health indicators.
This study has several limitations. One limitation of the study is the cross-sectional design which cannot reveal the temporal relationship between 24-h movement behaviors and cardiometabolic health indicators. Further, the NHS and other publicly available national health surveillance data rely on self-reported measures, which are subject to measurement error. The limited sample size of “none" group means that caution must be exercised when interpreting our findings on guidelines met none. In addition, 3615 participants, were excluded from the analyses due to incomplete data, which may have led to selection bias. However, participants excluded due to missing data were similar (p > 0.05) to those included in our study in terms of sex, age group and educational level. The physical activity guidelines were only calculated based on moderate-to-vigorous physical activity without considering muscle-strengthening activities and other light activites. We also used sitting time to estimate total sitting time. This measure may not capture time spent lying down, for example42.
There are several strengths of the present study, however, that should be considered. Associations were adjusted for several potential confounders, such as sex, age, education level, monthly household income, health insurance, ethnicity, geographic area and other lifestyle risk factors. We used objective measurements for body mass index, waist circumference, triglycerides, blood samples, and blood pressure. A large sample size also ensured adequate statistical power. Furthermore, currently, there has been limited data on 24-h movement behavior in Latin America; countries need to develop these to allow greater measurement, surveillance and promotion of movement behaviors among adults in this region.
Our findings, illustrate important considerations that must be made about the content of new guidelines released in Chile. Longitudinal and intervention studies are needed to examine a wide range of cardiometabolic health that are potentially associated with the 24-h movement guidelines. Future studies should also apply device-based measures of physical activity (e.g., accelerometers) or combine them with subjective ones (e.g., diaries and questionnaires) to assess movement behaviors in more detail.
Conclusions
In summary, around one out of five adults met the 24-h movement behavior guidelines in Chile. Meeting none or one out of three 24-h movement behavior guidelines was associated with higher odds of having poor cardiometabolic indicators in Chilean adults. National public health efforts are needed to promote more physical activity, less sitting time, and adequate sleep duration among Chilean residents to increase the proportion of individuals meeting at least 2, and preferably all three, existing 24-h movement recommendations. Future efforts should, therefore, consider novel strategies to simultaneously improve physical activity, sitting time and sleep duration in adults.
Data availability
The datasets generated and/or analysed during the current study are available in the database repository of the Epidemiology Department of the Chilean Ministry of Health: http://epi.minsal.cl/bases-de-datos/.
References
Rezende, L. F. M., Lee, D. H., Ferrari, G. & Giovannucci, E. Confounding due to pre-existing diseases in epidemiologic studies on sedentary behavior and all-cause mortality: A meta-epidemiologic study. Ann. Epidemiol. 52, 7–14. https://doi.org/10.1016/j.annepidem.2020.09.009 (2020).
Ortega, F. B., Lavie, C. J. & Blair, S. N. Obesity and cardiovascular disease. Circ. Res. 118, 1752–1770. https://doi.org/10.1161/CIRCRESAHA.115.306883 (2016).
Lauby-Secretan, B. et al. Body fatness and cancer-viewpoint of the IARC working group. N. Engl. J. Med. 375, 794–798. https://doi.org/10.1056/NEJMsr1606602 (2016).
Williams, E. P., Mesidor, M., Winters, K., Dubbert, P. M. & Wyatt, S. B. Overweight and obesity: Prevalence, consequences, and causes of a growing public health problem. Curr. Obes. Rep. 4, 363–370. https://doi.org/10.1007/s13679-015-0169-4 (2015).
Oftedal, S. et al. Associations of health-behavior patterns, mental health and self-rated health. Prev Med. 118, 295–303. https://doi.org/10.1016/j.ypmed.2018.11.017 (2019).
Rollo, S., Antsygina, O. & Tremblay, M. S. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J. Sport Health Sci. 9, 493–510. https://doi.org/10.1016/j.jshs.2020.07.004 (2020).
Ross, R. et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 45, S57–S102. https://doi.org/10.1139/apnm-2020-0467 (2020).
Ferrari, G. et al. Prevalence and sociodemographic correlates of meeting the Canadian 24-hour movement guidelines among latin american adults: A multi-national cross-sectional study. BMC Public Health 22, 217. https://doi.org/10.1186/s12889-022-12613-2 (2022).
Tremblay, M. S. et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 41, S311-327. https://doi.org/10.1139/apnm-2016-0151 (2016).
New Zealand Ministry of Health. Sit Less, Move More, Sleep Well: Physical Activity Guidelines for Children and Young People (Ministry of Health, 2017).
Okely, A. D. et al. A collaborative approach to adopting/adapting guidelines: The Australian 24-Hour Movement Guidelines for the early years (Birth to 5 years): An integration of physical activity, sedentary behavior, and sleep. BMC Public Health 17, 869. https://doi.org/10.1186/s12889-017-4867-6 (2017).
Khamput, T. et al. Thailand Recommendations on Physical Activity, Non-sedentary Lifestyles, and Sleeping 1st edn. (Division of Physical Activity and Health, Ministry of Public Health, 2017).
Draper, C. E. et al. The South African 24-hour movement guidelines for birth to 5 years: An integration of physical activity, sitting behavior, screen time, and sleep. J. Phys. Act. Health 17, 109–119. https://doi.org/10.1123/jpah.2019-0187 (2020).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462. https://doi.org/10.1136/bjsports-2020-102955 (2020).
Hirshkowitz, M. et al. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 1, 40–43. https://doi.org/10.1016/j.sleh.2014.12.010 (2015).
Tremblay, M. S. et al. Sedentary behavior research network (SBRN): Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act 14, 75. https://doi.org/10.1186/s12966-017-0525-8 (2017).
Tremblay, M. S., Carson, V. & Chaput, J. P. Introduction to the Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 41, iii–iv. https://doi.org/10.1139/apnm-2016-0203 (2016).
Vio, F., Albala, C. & Kain, J. Nutrition transition in Chile revisited: Mid-term evaluation of obesity goals for the period 2000–2010. Public Health Nutr. 11, 405–412. https://doi.org/10.1017/S136898000700050X (2008).
MINSAL. Encuesta Nacional de Salud 2016–2017-Ministerio de Salud (MINSAL, 2017).
Aburto, M. J. et al. Prevalence and co-occurrence of lifestyle risk factors for non-communicable diseases according to sociodemographic characteristics among adults Chilean residents. Sci. Rep. 11, 21702. https://doi.org/10.1038/s41598-021-01167-9 (2021).
Hoos, T., Espinoza, N., Marshall, S. & Arredondo, E. M. Validity of the global physical activity questionnaire (GPAQ) in adult Latinas. J. Phys. Act Health 9, 698–705. https://doi.org/10.1123/jpah.9.5.698 (2012).
Bull, F. C., Maslin, T. S. & Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act Health 6, 790–804. https://doi.org/10.1123/jpah.6.6.790 (2009).
Armstrong, T. & Bull, F. Development of the world health organization global physical activity questionnaire (GPAQ). J. Public Health 14, 66–70 (2006).
Mealing, N. M., Bowles, H. R., Merom, D. & Bauman, A. Impact of scoring algorithm on physical activity prevalence estimates in Australian adults. J. Sci. Med. Sport 14, 27–32. https://doi.org/10.1016/j.jsams.2010.05.003 (2011).
Aguilar-Farias, N. & LeppeZamora, J. Is a single question of the global physical activity questionnaire (GPAQ) valid for measuring sedentary behaviour in the Chilean population?. J. Sports Sci. 35, 1652–1657. https://doi.org/10.1080/02640414.2016.1229010 (2017).
Cleland, C. L. et al. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health 14, 1255. https://doi.org/10.1186/1471-2458-14-1255 (2014).
World Health Organization. Obesity: Preventing and Managing the Global Epidemic 1–253 (World Health Organization, 2000).
Ross, R. et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 16, 177–189. https://doi.org/10.1038/s41574-019-0310-7 (2020).
The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med 157, 2413–2446, https://doi.org/10.1001/archinte.157.21.2413 (1997).
Yousefzadeh, G., Shokoohi, M., Najafipour, H. & Shadkamfarokhi, M. Applying the Framingham risk score for prediction of metabolic syndrome: The Kerman Coronary Artery Disease Risk Study, Iran. ARYA Atheroscler. 11, 179–185 (2015).
Icaza, G. et al. Estimation of coronary heart disease risk in Chilean subjects based on adapted Framingham equations. Rev. Med. Chil. 137, 1273–1282 (2009).
Lanas, F., Seron, P., Munoz, S., Margozzini, P. & Puig, T. Latin American Clinical Epidemiology Network Series-Paper 7: Central obesity measurements better identified risk factors for coronary heart disease risk in the Chilean National Health Survey (2009–2010). J. Clin. Epidemiol. 86, 111–116. https://doi.org/10.1016/j.jclinepi.2016.04.018 (2017).
Subramanian, S. V., Delgado, I., Jadue, L., Vega, J. & Kawachi, I. Income inequality and health: Multilevel analysis of Chilean communities. J. Epidemiol. Community Health 57, 844–848. https://doi.org/10.1136/jech.57.11.844 (2003).
Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R. & Grant, M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 88, 791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x (1993).
Alvarado, M. E., Garmendia, M. L., Acuna, G., Santis, R. & Arteaga, O. Assessment of the alcohol use disorders identification test (AUDIT) to detect problem drinkers. Rev. Med. Chil. 137, 1463–1468 (2009).
Janssen, I. et al. A systematic review of compositional data analysis studies examining associations between sleep, sedentary behaviour, and physical activity with health outcomes in adults. Appl. Physiol. Nutr. Metab. 45, S248–S257. https://doi.org/10.1139/apnm-2020-0160 (2020).
McGregor, D. E. et al. Compositional analysis of the associations between 24-h movement behaviours and health indicators among adults and older adults from the Canadian health measure survey. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph15081779 (2018).
Chastin, S. F., Palarea-Albaladejo, J., Dontje, M. L. & Skelton, D. A. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: A novel compositional data analysis approach. PLoS ONE 10, e0139984. https://doi.org/10.1371/journal.pone.0139984 (2015).
Rao, D. P., Orpana, H. & Krewski, D. Physical activity and non-movement behaviours: Their independent and combined associations with metabolic syndrome. Int. J. Behav. Nutr. Phys. Act. 13, 26. https://doi.org/10.1186/s12966-016-0350-5 (2016).
Roman-Vinas, B. et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int. J. Behav. Nutr. Phys. Act. 13, 123. https://doi.org/10.1186/s12966-016-0449-8 (2016).
Master, L. et al. Bidirectional, daily temporal associations between sleep and physical activity in adolescents. Sci. Rep. 9, 7732. https://doi.org/10.1038/s41598-019-44059-9 (2019).
Weatherson, K. A. et al. Post-secondary students’ adherence to the Canadian 24-hour movement guidelines for adults: Results from the first deployment of the Canadian Campus Wellbeing Survey (CCWS). Health Promot. Chronic Dis. Prev. Can. 41, 173–181. https://doi.org/10.24095/hpcdp.41.6.01 (2021).
Author information
Authors and Affiliations
Contributions
G.F., conceived, designed, and helped to write and revise the manuscript; R.R., and G.F., were responsible for coordinating the study, contributed to the intellectual content, and revise the manuscript, R.R., L.F.M.R., A.M., C.D., and G.F., interpreted the data, helped to write and revise the manuscript. All authors contributed to the study design, critically reviewed the manuscript, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Riquelme, R., Rezende, L.F.M., Marques, A. et al. Association between 24-h movement guidelines and cardiometabolic health in Chilean adults. Sci Rep 12, 5805 (2022). https://doi.org/10.1038/s41598-022-09729-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09729-1
This article is cited by
-
Prevalence and association of compliance with the Canadian 24-hour movement guidelines with sociodemographic aspects in Brazilian adults: a cross-sectional epidemiological study
BMC Public Health (2024)
-
Combined association of physical activity and sitting time with cardiometabolic risk factors in Chilean adults
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.