Abstract
The association between Lipocalin-2 (LCN2) and cognition in patients with metabolic syndrome (MetS) has not been thoroughly investigated. We aimed to evaluate whether serum LCN2 levels are associated with the alteration of cognitive function in patients with MetS. The total of 191 non-demented participants with MetS were enrolled onto the study in 2015, and a cohort study was conducted in a subpopulation in 2020. After adjustment for sex, age, waist circumference, creatinine levels, and HbA1C, an association between the higher serum LCN2 levels and the lower Montreal cognitive assessment (MoCA) scores was observed (B = − 0.045; 95%CI − 0.087, − 0.004; p 0.030). A total of 30 participants were followed-up in 2020. Serum LCN2 levels were decreased in correlation with age (23.31 ± 12.32 ng/ml in 2015 and 15.98 ± 11.28 ng/ml in 2020, p 0.024), while other metabolic parameters were unchanged. Magnetic resonance imaging studies were conducted on a subsample of patients in 2020 (n = 15). Associations between high serum LCN2 levels from 2015 and 2020 and changes in brain volume of hippocampus and prefrontal cortex from 2020 have been observed. These findings suggest a relationship between changes of the level of circulating LCN2, cognitive impairment, and changes in brain volume in patients with MetS. However, further investigation is still needed to explore the direct effect of circulating LCN2 on the cognition of MetS patients.
Similar content being viewed by others
Introduction
Metabolic syndrome (MetS) refers to a cluster of several pathological conditions that can increase the incidence of type 2 diabetes, cardiovascular conditions, stroke, and neurodegeneration. The features of MetS include obesity, as indicated by excess body fat around the waist, dyslipidemia, hyperglycemia, and hypertension. In addition, much evidence from in vivo and clinical studies has demonstrated a relationship between MetS and cognitive decline1,2. However, the underlying mechanisms of links between MetS and cognitive decline are elusive.
The prodromal stage of cognitive decline in humans is called mild cognitive impairment (MCI). Individuals with MCI develop cognitive abnormalities in normal daily function3,4. Approximately twenty percent of the people with MCI progress to dementia a few years later5,6,7. Although physical examination can be used to make a diagnosis of cognitive impairment, the clinical signs of MCI have been mainly identified at later stages of cognitive decline or in the early phase of dementia8. Therefore, a tool to distinguish the earliest stage of MCI could be of the greatest benefit to patients with dementia in order to intervene in the development of cognitive impairment in MCI patients or to promptly protect patients from the development of dementia. Several underlying mechanisms of MCI and dementia have been proposed including neuroinflammation, oxidative stress, insulin resistance and microvascular abnormalities in the brain9,10,11,12.
Lipocalin-2 (LCN2), known as neutrophil gelatinase-associated lipocalin, 24p3, or siderocalin, is a small glycoprotein in the lipocalin family13. LCN2 acts as an acute phase protein and it is an inducible factor synthesized and secreted by reactive astrocytes, activated microglia, neurons, choroid plexus and endothelial cells in response to inflammatory or injurious insults to the brain14. It has been demonstrated that LCN2 acts as a modulatory factor for diverse cellular functions in the brain, including cell death and survival15,16, morphology16, migration16,17, and amplification of inflammatory responses18,19,20. LCN2 also play roles in the regulation of brain iron21,22, the innate immune response, and the regulation of neuroinflammation and neurodegeneration14. Apart from its molecular properties, LCN2 has been shown to be responsible for several biobehavioral activities, including pain hypersensitivity, cognitive functions, emotion, depression, and anxiety14. It has been proposed that circulating LCN2 could be used a biomarker for many conditions, for example, acute kidney injury23, cardiovascular diseases24, obesity and metabolic syndrome25, and various brain disorders, including dementia26.
Clinical studies into LCN2 and its relationship with cognitive impairment have mainly been conducted in AD populations, findings indicating potential predictive properties of the protein26,27,28,29. A recent study demonstrated that the circulating LCN2 level is involved early in AD pathogenesis at preclinical stages and may be an early blood biomarker of amyloid-beta pathology30. However, the knowledge of its role in MCI in the MetS condition is still unclear. Therefore, this study aims to evaluate whether circulating LCN2 level is associated with cognitive status in patients with MetS. Furthermore, a 5-year follow up in a random subpopulation was conducted to assess the predictive property of circulating LCN2 level on mild cognitive impairment by assessing cognitive performance and the anatomical structure of the brain and its volume.
Results
From the total of 191 patients with MetS in 2015, 107 (56.02%) were female, and the average age was 64.53 (SD 8.45). Mean serum LCN2 levels and MoCA score were 29.70 ng/mL (SD 16.75) and 19.42 (SD 4.72), respectively. Demographic data of the participants is described in Table 1.
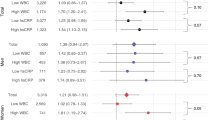
Table 2 shows the association between serum LCN2 levels and MoCA score in 2015. Serum LCN2 levels were negatively associated with the MoCA scores in crude analysis (B = − 0.043; 95%CI − 0.082, − 0.003; p 0.004). After adjustment for sex, age, waist circumference, creatinine levels, and HbA1C, a significant association between the higher serum LCN2 levels and the lower MoCA scores was still observed (B = − 0.045; 95%CI − 0.087, − 0.004; p 0.030).
Out of the 30 participants in the subpopulation that had been followed up in 2020, fifty percent were female and the mean age in 2015 was 60.1 years (SD 4.63). No significant changes in clinical and biological parameters from 2015 to 2020 was observed, except for serum LCN2 levels which were significantly decreased in 2020, as shown in Table 3. Serum LCN2 levels in 2015 were negatively associated with the volume of the left hippocampus in 2020. In 2020, the levels of LCN2 were significantly related to the lower volume of left and right prefrontal cortices and higher left hippocampal volume. These data are presented in Table 4. Figure 1 shows the representation of the prefrontal cortex and hippocampus from MRI brain of patients with MetS. No association between white matter hyperintensity and LCN2 levels in 2015 and 2020 were observed (p 0.536 and 0.095, respectively). There was also no association between specific brain volume and MoCA scores in 2015 and 2020.
Representation of MRI brain images of participants, the prefrontal cortex identified in green and the hippocampus in red (scale bar, 1 cm × 10 scale); (A) the brain of a 59-year-old man with a MoCA score = 25, total prefrontal cortex percentage = 26.9 and circulating lipocalin level in 2020 = 8.59 ng/ml; (B) the brain of a 65-year-old man with a MoCA score = 27, total hippocampus percentage = 0.6 and circulating lipocalin level in 2020 = 21.15 ng/ml; (C) the brain of a 60-year-old man with a MoCA score = 24, total prefrontal cortex percentage = 23.4 and circulating lipocalin level in 2020 = 21.98 ng/ml; (D) the brain of a 60-year-old man with a MoCA score = 25, total hippocampus percentage = 0.49, and circulating lipocalin level in 2020 = 13.07 ng/ml.
Discussion
Several clinical studies have reported controversial results about LCN2 levels and cognitive status37, however, the present study showed a positive association between circulating LCN2 and cognitive decline in non-demented MetS population. We found that circulating LCN2 levels declined over time. Even though there was no association between the change in LCN2 levels and cognitive performance in 2020, the volume of the prefrontal cortex in 2020 recorded using MRI was negatively associated with LCN2 levels at the same timepoint. Interestingly, the volume of the hippocampus in 2020 was negatively associated with serum LCN2 levels in 2015.
It has been shown that MetS can contribute to cognitive impairment38, but the role of LCN2 in cognitive decline in patients with MetS was unknown. The positive finding of an association between circulating LCN2 levels and cognitive decline in our study highlights the possible role of LCN2 as a possibly predictor of MCI in patients with MetS. There are reports that LCN2 is associated with metabolic dysfunction and insulin resistance39,40. Interestingly the circulating LCN2 levels among patients with MetS was higher than those without MetS41. Thus, there is a possibility that LCN2 could be one of factors involved in the MetS condition, and may contribute to cognitive impairment. However, whether LCN2 has a detrimental or beneficial role in metabolic syndrome is still unclear. In the case of cognitive function, an increase in circulating LCN2 levels tended to be harmful as demonstrated with in vitro and in vivo studies as described in a recent review37. Therefore, the higher levels of LCN2 in patients with MetS are not likely to be of benefit to the cognitive status of the patients.
Our results are consistent with a previous study that reported that the circulating LCN2 levels in a cognitive impaired population were higher than a control group with normal cognition37. In addition, several clinical studies have been conducted in many cognitive impaired populations to explore the relationship between LCN2 and cognitive status. A positive correlation between circulating LCN2 level and cognitive decline was reported in vascular dementia19, late-life depression42, and MCI populations29. We found that the higher circulating LCN2 levels were associated with lower cognitive testing scores in a non-demented MetS population. A previous study also reported an association between plasma LCN2 levels and another global-score cognitive test, the Mini-Mental State Examination score (MMSE)29. However, our findings are contradictory to those from another recent study in preclinical AD which reported no association between LCN2 levels and MMSE30 adjusted for age and sex.
Interestingly, the circulating LCN2 levels in our study were significantly decreased in 2020 compared to 2015 without any changes in kidney function, and metabolic status. This finding implies that circulating LCN2 level may decrease with age. This result is in contrast with prior cross-sectional studies, which reported that circulating LCN2 concentrations are increased with age43,44. Aging is associated with increased levels of many circulating cytokines and proinflammatory markers45. For example: elevated levels of interleukin (IL)-1, IL-6, and tumor necrosis factor-α are associated with an older population. However, we found that LCN 2 levels significantly decreased when people got older. Our study may not represent the general aging population as the population in our study involved MetS.
A negative association between circulating LCN2 levels in 2015 and the volume of left, but not right, hippocampus in 2020 might imply the predicting role of LCN2 for brain changes in patients with MetS. Left and right hippocampus are associated with different functions, the left hippocampus being related to verbal memory, and the right hippocampus to spatial memory46. These differing functions could explain why the association was found only with one, not two sides of hippocampus. However, a limitation to this study is that we did not have the brain imaging in 2015 to compare therefore we could not prove this predictive property. Nonetheless, in 2020, circulating LCN2 levels were negatively associated with the prefrontal cortex in the same year. This brain region found to be associated with LCN2 levels were congruent with the finding from a prior study in preclinical AD30. That study demonstrated a possible link between circulating LCN2 levels and the ability to carry out executive functions which are controlled by the prefrontal cortex. There was a significant positive association between LCN2 in 2020 and the left hippocampus in the same year. This might imply that LCN2 could play different roles in different brain regions and it might act differently over time as the overall levels of LCN2 were lower in 2020. Our findings suggest that LCN2 could have a predictive role as an early biomarker for cognitive impairment and changes in the prefrontal cortex related to executive function and in the left hippocampus related to verbal memory.
A strength of this study is its relatively large sample size compared to prior studies. In addition, the five-year time span of this cohort study provides more information about the direction of changes of LCN2 levels and its possible direction of association with cognitive decline. However, some limitations of the study need to be taken into account. First, as mentioned earlier, we had no MRI records to establish brain volume in 2015 to compare with the present time (2020), so we cannot tell whether the brain volume had changed. Secondly, we did not have levels of inflammatory cytokines in the present study, so the underlying mechanism cannot be explained. Lastly, no association between MoCA score and brain volume was observed in our study which may be due to the limitation of the sample size in 2020, the overall low levels of MoCA score in the population, or the limitation of the tool that is not a domain specific assessment tool. Further studies with a larger sample size or using a more in-depth neuropsychological test for each specific domain of cognition could provide more information.
In conclusion, our findings suggest that circulating LCN2 levels are positively associated with the reduction in the volume of the prefrontal cortex in this MetS population and changes in volume of the left hippocampus. Further investigation is still needed to explore the direct effect of circulating LCN2 on the cognitive function of patients with metabolic syndrome as well as the mechanisms underlying these changes.
Methods
Participants
The study protocol was approved by the ethics committee of the Faculty of Medicine, Chiang Mai University (Nos: 253/2020, 154/2020, and 427/2020). Written informed consent from each participant was also gathered in this study. All methods were performed in accordance with the relevant guidelines and regulations.
The present study is a sub-study of The Cohort Of patients at a high Risk for Cardiovascular Events (CORE) Thailand registry, which is an ongoing cohort study of patients with a high cardiovascular risk31. One hundred and ninety one patients in 2015 were recruited in this study if they met at least three of the following five criteria for MetS (19): (1) elevated waist circumference (WC, ≥ 90 cm in men and ≥ 80 cm in women); (2) elevated triglycerides (TG, ≥ 150 mg/dL) or being treated; (3) reduced high density lipoprotein cholesterol (HDL-C, < 40 mg/dL in men and < 50 mg/dL in women); (4) elevated blood pressure (BP, ≥ 130/85 mmHg) or being treated; (5) elevated fasting plasma glucose (FPG ≥ 100 mg/dL) or being treated. Exclusion criteria of the study included dementia, depression, or had undergone surgery within 3 months. Then, 30 patients with MetS from 2015 were randomly followed up in 2020. The experimental protocol is summarized in Fig. 2.
Data and specimen collection
All data collection was performed on the same day. These data include history taking, physical examination, and blood collection. History taking was used to collect personal information including age, sex, education, comorbid diseases, history of alcohol drinking and smoking. Data collected from physical examination included WC, blood pressure, body weight and height. Measurements of FPG, HDL-C, LDL-C, TG, insulin, creatinine, and LCN2 levels were performed on fasting venous blood samples collected from each participant. A human LCN2 (RAB0332, Sigma-Aldrich, Darmstadt, Germany) ELISA kit was used to measure serum LCN2 level, in accordance with protocols provided by the test manufacturer.
Cognitive function assessment
Cognitive function was assessed by using The Montreal Cognitive Assessment (MoCA). The Thai version of the MoCA was used to assess cognitive function as it has high sensitivity and specificity for detecting mild cognitive impairment32. The 30 items of the test are to assess multiple cognitive domains including: executive function (adapted trail making test); visuospatial ability (a cube copy task and clock drawing test); language abilities (naming of animals, fluency, and repetition of sentences); abstract thinking (telling similarity between objects); short-term memory (delayed recall); concentration, attention and working memory (digit span task and serial subtraction); and orientation to time and place. The maximum score is 30. The higher scores refer to the better cognitive performance. As the score can be influenced by education, for the Thai version, one point is added to the scores of participants with 6 years of education or less.
MRI data acquisition and post-processing for hippocampal, prefrontal, and white matter lesion measurements
A magnetic resonance imaging (MRI) study was conducted on a subsample of patients in 2020 (N = 15). All participants underwent a 1.5 T MRI (GE Medical Systems, Waukesha, WI). Imaging protocol consists of the following sequences: a sagittal three-dimensional (3D) IR-SPGR T1-weighted sequence (170 slices, voxel size: 1.00 × 1.00 × 1.00 mm3), and an axial 2D T2-FLAIR sequence (27 slices, voxel size: 1.00 × 1.00 × 5.00 mm3).
In accordance with the evidence about changes in brain structure from structural imaging of MCI and dementia, apart from volumetric study of each lobe of the brain (frontal lobe, parietal lobe, temporal lobe, occipital lobe, and insula lobe), specific brain regions were chosen for further analysis in this study. These regions included the hippocampus33, entorhinal cortex34, prefrontal cortex35, and precuneus36.
All Digital Imaging and Communications in Medicine (DICOM) images from the scanner were converted to the Neuroimaging Informatics Technology Initiative (NIfTI) format using MRIcroGL software (NeuroImaging Tool & Resources Collaboratory, https://www.nitrc.org). T1 IR-SPGR images were used to measure cortical and subcortical structures using Freesurfer6.0 software (https://surfer.nmr.mgh.harvard.edu). For cortical volumes, each individual volume of frontal, parietal, occipital, temporal, and prefrontal regions was normalized by the total cortical volume of cerebrum. The prefrontal volume includes caudalanteriocingulate, lateralorbitofrontal, medialorbitofrontal, parsopercularis, parsorbitalis, parstriangularis, rostralanteriorcingulate, rostralmiddlefrontal, and superiorfrontal regions. For subcortical volume, only the hippocampus was used for investigation, which was normalized against the intracranial cavity. White matter lesion measurement was performed using lesion Brain1.0 software (http://volbrain.upv.es.), in which T1 IR-SPGR and T2-FLAIR images are required.
Statistical analysis
Statistical analysis was performed using Stata version 16 (StataCorp LLC, College Station, TX, USA). Categorical and Continuous variables were expressed as frequencies and percentages, and mean ± SD, respectively. Multivariable analysis was used to assess the association between LCN2 levels and MoCA score in 2015. Age, gender, WC, and creatinine were all included in the analysis model as potential confounders. Other variables which were significantly associated with MoCA score from univariable analysis were included in the multivariable regression analysis model. The reduced model is shown in Model 2. The associations between each parameter and LCN2 from 2015 and 2020 were determined by using paired t-tests. The association between LCN2 levels and the brain volume in each brain region was determined using Spearman’s rank correlation analysis. A P value of less than 0.05 was considered statistically significant.
Data availability
The datasets used and/or analyzed in this study are available from the corresponding author on reasonable request.
References
de Bem, A. F. et al. Animal models of metabolic disorders in the study of neurodegenerative diseases: an overview. Front. Neurosci. https://doi.org/10.3389/fnins.2020.604150 (2021).
Alcorn, T. et al. Cross-sectional associations between metabolic syndrome and performance across cognitive domains: a systematic review. Appl. Neuropsychol. Adult 26, 186–199. https://doi.org/10.1080/23279095.2017.1363039 (2019).
Smith, G. E. & Bondi, M. W. Mild Cognitive Impairment and Dementia: Definitions, Diagnosis, and Treatment. (Oxford University Press, 2013).
Petersen, R. C. et al. Mild cognitive impairment: ten years later. Arch. Neurol. 66, 1447–1455. https://doi.org/10.1001/archneurol.2009.266 (2009).
Loewenstein, D. A. et al. Stability of different subtypes of mild cognitive impairment among the elderly over a 2- to 3-year follow-up period. Dement. Geriatr. Cogn. Disord. 27, 418–423. https://doi.org/10.1159/000211803 (2009).
Roberts, R. & Knopman, D. S. Classification and epidemiology of MCI. Clin. Geriatr. Med. 29, 753–772. https://doi.org/10.1016/j.cger.2013.07.003 (2013).
Koepsell, T. D. & Monsell, S. E. Reversion from mild cognitive impairment to normal or near-normal cognition: risk factors and prognosis. Neurology 79, 1591–1598. https://doi.org/10.1212/WNL.0b013e31826e26b7 (2012).
Liss, J. L. et al. Practical recommendations for timely, accurate diagnosis of symptomatic Alzheimer’s disease (MCI and dementia) in primary care: a review and synthesis. J. Int. Med. https://doi.org/10.1111/joim.13244 (2021).
Saedi, E., Gheini, M. R., Faiz, F. & Arami, M. A. Diabetes mellitus and cognitive impairments. World J. Diabetes 7, 412–422. https://doi.org/10.4239/wjd.v7.i17.412 (2016).
Muriach, M., Flores-Bellver, M., Romero, F. J. & Barcia, J. M. Diabetes and the brain: oxidative stress, inflammation, and autophagy. Oxid. Med. Cell. Longev. 2014, 102158. https://doi.org/10.1155/2014/102158 (2014).
Biessels, G. J. in Diabetic Neuropathy: Clinical Management (eds Aristidis Veves & Rayaz A. Malik) 187–205 (Humana Press, 2007).
van den Berg, E., Reijmer, Y. D. & Biessels, G. J. in Diabetes and the Brain (eds Geert Jan Biessels & Jose A. Luchsinger) 295–322 (Humana Press, 2010).
Chakraborty, S., Kaur, S., Guha, S. & Batra, S. K. The multifaceted roles of neutrophil gelatinase associated lipocalin (NGAL) in inflammation and cancer. Biochem. Biophys. Acta. 129–169, 2012. https://doi.org/10.1016/j.bbcan.2012.03.008 (1826).
Jha, M. K. et al. Diverse functional roles of lipocalin-2 in the central nervous system. Neurosci. Biobehav. Rev. 49, 135–156. https://doi.org/10.1016/j.neubiorev.2014.12.006 (2015).
Lee, S. et al. A dual role of Lipocalin 2 in the apoptosis and deramification of activated microglia. J. Immunol. 179, 3231–3241. https://doi.org/10.4049/jimmunol.179.5.3231 (2007).
Lee, S., Lee, W. H., Lee, M. S., Mori, K. & Suk, K. Regulation by lipocalin-2 of neuronal cell death, migration, and morphology. J. Neurosci. Res. 90, 540–550. https://doi.org/10.1002/jnr.22779 (2012).
Lee, S. et al. Lipocalin-2 Is a chemokine inducer in the central nervous system: role of chemokine ligand 10 (CXCL10) in lipocalin-2-induced cell migration. J. Biol. Chem. 286, 43855–43870. https://doi.org/10.1074/jbc.M111.299248 (2011).
Bhusal, A., Rahman, M. H., Lee, I. K. & Suk, K. Role of Hippocampal Lipocalin-2 in Experimental Diabetic Encephalopathy. Front. Endocrinol. 10, 25. https://doi.org/10.3389/fendo.2019.00025 (2019).
Kim, J. H. et al. Astrocyte-derived lipocalin-2 mediates hippocampal damage and cognitive deficits in experimental models of vascular dementia. Glia 65, 1471–1490. https://doi.org/10.1002/glia.23174 (2017).
Almeida-Suhett, C. P., Li, Z., Marini, A. M., Braga, M. F. & Eiden, L. E. Temporal course of changes in gene expression suggests a cytokine-related mechanism for long-term hippocampal alteration after controlled cortical impact. J. Neurotrauma 31, 683–690. https://doi.org/10.1089/neu.2013.3029 (2014).
Dong, M., Xi, G., Keep, R. F. & Hua, Y. Role of iron in brain lipocalin 2 upregulation after intracerebral hemorrhage in rats. Brain Res. 1505, 86–92. https://doi.org/10.1016/j.brainres.2013.02.008 (2013).
Dekens, D. W. et al. Lipocalin 2 contributes to brain iron dysregulation but does not affect cognition, plaque load, and glial activation in the J20 Alzheimer mouse model. J. Neuroinflammation 15, 330. https://doi.org/10.1186/s12974-018-1372-5 (2018).
Pozzoli, S., Simonini, M. & Manunta, P. Predicting acute kidney injury: current status and future challenges. J. Nephrol. 31, 209–223. https://doi.org/10.1007/s40620-017-0416-8 (2018).
Cruz, D. N., Gaiao, S., Maisel, A., Ronco, C. & Devarajan, P. Neutrophil gelatinase-associated lipocalin as a biomarker of cardiovascular disease: a systematic review. Clin. Chem. Lab. Med. 50, 1533–1545. https://doi.org/10.1515/cclm-2012-0307 (2012).
Wang, Y. et al. Lipocalin-2 is an inflammatory marker closely associated with obesity, insulin resistance, and hyperglycemia in humans. Clin. Chem. 53, 34–41. https://doi.org/10.1373/clinchem.2006.075614 (2007).
Song, J. & Kim, O. Y. Perspectives in Lipocalin-2: emerging biomarker for medical diagnosis and prognosis for Alzheimer’s disease. Clin. Nutr. Res. 7, 1–10. https://doi.org/10.7762/cnr.2018.7.1.1 (2018).
Naude, P. J. et al. Lipocalin 2: novel component of proinflammatory signaling in Alzheimer’s disease. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 26, 2811–2823. https://doi.org/10.1096/fj.11-202457 (2012).
Dekens, D. W. et al. Neutrophil gelatinase-associated lipocalin and its receptors in Alzheimer’s disease (AD) brain regions: differential findings in AD with and without depression. J. Alzheimer’s Disease JAD 55, 763–776. https://doi.org/10.3233/jad-160330 (2017).
Choi, J., Lee, H. W. & Suk, K. Increased plasma levels of lipocalin 2 in mild cognitive impairment. J. Neurol. Sci. 305, 28–33. https://doi.org/10.1016/j.jns.2011.03.023 (2011).
Eruysal, E., Ravdin, L., Kamel, H., Iadecola, C. & Ishii, M. Plasma lipocalin-2 levels in the preclinical stage of Alzheimer’s disease. Alzheimers Dement (Amst) 11, 646–653. https://doi.org/10.1016/j.dadm.2019.07.004 (2019).
Phrommintikul, A. et al. Factors associated with cognitive impairment in elderly versus nonelderly patients with metabolic syndrome: the different roles of FGF21. Sci. Rep. 8, 5174–5174. https://doi.org/10.1038/s41598-018-23550-9 (2018).
Nasreddine, Z. S. et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x (2005).
Apostolova, L. G. et al. Hippocampal atrophy and ventricular enlargement in normal aging, mild cognitive impairment (MCI), and Alzheimer Disease. Alzheimer Dis Assoc Disord 26, 17–27. https://doi.org/10.1097/WAD.0b013e3182163b62 (2012).
Du, A. T. et al. Magnetic resonance imaging of the entorhinal cortex and hippocampus in mild cognitive impairment and Alzheimer’s disease. J Neurol Neurosurg Psychiatry 71, 441–447. https://doi.org/10.1136/jnnp.71.4.441 (2001).
Burgmans, S. et al. Prefrontal cortex atrophy predicts dementia over a six-year period. Neurobiol. Aging 30, 1413–1419. https://doi.org/10.1016/j.neurobiolaging.2007.11.028 (2009).
Karas, G. et al. Precuneus atrophy in early-onset Alzheimer’s disease: a morphometric structural MRI study. Neuroradiology 49, 967–976. https://doi.org/10.1007/s00234-007-0269-2 (2007).
Pinyopornpanish, K., Chattipakorn, N. & Chattipakorn, S. C. Lipocalin-2: Its perspectives in brain pathology and possible roles in cognition. J. Neuroendocrinol. 31, e12779. https://doi.org/10.1111/jne.12779 (2019).
Guicciardi, M., Crisafulli, A., Doneddu, A., Fadda, D. & Lecis, R. Effects of metabolic syndrome on cognitive performance of adults during exercise. Front. Psychol. https://doi.org/10.3389/fpsyg.2019.01845 (2019).
Law, I. K. et al. Lipocalin-2 deficiency attenuates insulin resistance associated with aging and obesity. Diabetes 59, 872–882. https://doi.org/10.2337/db09-1541 (2010).
Huang, Y. et al. Lipocalin-2, glucose metabolism and chronic low-grade systemic inflammation in Chinese people. Cardiovasc. Diabetol. 11, 11. https://doi.org/10.1186/1475-2840-11-11 (2012).
Bhusal, A. et al. Paradoxical role of lipocalin-2 in metabolic disorders and neurological complications. Biochem. Pharmacol. 169, 113626. https://doi.org/10.1016/j.bcp.2019.113626 (2019).
Naude, P. J. et al. Sex-specific associations between Neutrophil Gelatinase-Associated Lipocalin (NGAL) and cognitive domains in late-life depression. Psychoneuroendocrinology 48, 169–177. https://doi.org/10.1016/j.psyneuen.2014.06.016 (2014).
Bennett, M. R., Ma, Q., Ying, J., Devarajan, P. & Brunner, H. Effects of age and gender on reference levels of biomarkers comprising the pediatric Renal Activity Index for Lupus Nephritis (p-RAIL). Pediatr. Rheumatol. Online J. 15, 74–74. https://doi.org/10.1186/s12969-017-0202-0 (2017).
Elneihoum, A. M., Falke, P., Hedblad, B., Lindgärde, F. & Ohlsson, K. Leukocyte activation in atherosclerosis: correlation with risk factors. Atherosclerosis 131, 79–84. https://doi.org/10.1016/s0021-9150(96)06077-7 (1997).
Michaud, M. et al. Proinflammatory cytokines, aging, and age-related diseases. J. Am. Med. Dir. Assoc. 14, 877–882. https://doi.org/10.1016/j.jamda.2013.05.009 (2013).
Ezzati, A. et al. Differential association of left and right hippocampal volumes with verbal episodic and spatial memory in older adults. Neuropsychologia 93, 380–385. https://doi.org/10.1016/j.neuropsychologia.2016.08.016 (2016).
Acknowledgements
Not applicable.
Funding
This study was supported by the Research Medical Fund, Grant Number 118/2563, Faculty of Medicine, Chiang Mai University; a Senior Research Scholar grant from the National Research Council of Thailand (S.C.C); an NSTDA Research Chair Grant from the National Science and Technology Development Agency Thailand (N.C.) and a Chiang Mai University Excellence Center Award (N.C.).
Author information
Authors and Affiliations
Contributions
K.P., A.P., C.A., N.C., and S.C. participated in the concept and design of the study. K.P., N.B., S.K., S.A., U.Y., and A.P. contributed to data acquisition. K.P., C.A., and S.C. performed the statistical analyses and interpretation. K.P. and S.C. drafted the manuscript. K.P., A.P., C.A., S.K., S.A., U.Y., N.B., N.C., and S.C. critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pinyopornpanish, K., Phrommintikul, A., Angkurawaranon, C. et al. Circulating Lipocalin-2 level is positively associated with cognitive impairment in patients with metabolic syndrome. Sci Rep 12, 4635 (2022). https://doi.org/10.1038/s41598-022-08286-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-08286-x
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.