Abstract
Patients with cirrhosis may show minimal hepatic encephalopathy (MHE), for which rifaximin is effective. Metabolic syndrome may be associated with cognitive impairment. Our aims were to evaluate the influence of metabolic syndrome features on response to rifaximin for neurological and inflammatory alterations in MHE. A prospective cohort study was conducted in 63 cirrhotic patients and 30 controls from two tertiary centres recruited between 2015 and 2019. Metabolic syndrome was defined according to the Adult Treatment Panel-III. Patients were classified into 31 without and 32 with MHE according to the Psychometric Hepatic Encephalopathy Score (PHES). All participants performed specific psychometric tests, and inflammatory parameters were studied. Patients with MHE received rifaximin (400 mg/8 h). Response was evaluated by PHES at 3 and 6 months. Response according to metabolic syndrome manifestations was compared. The response rate was 66%. Older age (p = 0.012) and all metabolic syndrome diseases (p < 0.05) were associated with non-response, plus an increase in risk as the number of manifestations rose (p < 0.001). Patients with metabolic manifestations exhibited worse processing speed (p = 0.011), working memory (p = 0.005), visual coordination (p = 0.013) and lower proportion of activated CD4+ lymphocytes (p = 0.039) at baseline, as well as worse concentration (p = 0.030), bimanual coordination (p = 0.004) and higher levels of intermediate monocytes (p = 0.026), CX3CL1 (p < 0.05), IL-17 (p = 0.022), AHR (p = 0.010) and IgG (p < 0.05) at 3 and/or 6 months of rifaximin. Patients with clinical signs of metabolic syndrome have poor response to rifaximin for MHE, with a higher proportion of neurological alterations associated with a pro-inflammatory environment.
Similar content being viewed by others
Introduction
Minimal hepatic encephalopathy (MHE) is present in up to 80% of patients with cirrhosis1,2,3,4. Although patients with MHE appear asymptomatic, subtle changes occur in attention, working memory, executive decision making, psychomotor speed and coordination5,6. This condition has a negative impact on quality of life, with an increased risk of falls, home and car accidents, progression to overt hepatic encephalopathy, hospitalization and death7,8,9,10,11,12. Given that this neuropsychiatric disorder can be reversible, therapeutic strategies are of major importance.
Several randomized placebo controlled trials have demonstrated that rifaximin improves psychometric test scores, health-related quality of life and performance in driving simulator test13,14. It is well-tolerated with good adherence rate and no difference in the most common adverse events compared to placebo14.
Several metabolic syndrome clinical manifestations such as non-alcoholic fatty liver disease (NAFLD) and diabetes mellitus (DM) are characterized by a pro-inflammatory environment and may be associated with cognitive impairment15,16,17,18,19. Additionally, metformin treatment for patients with type 2 DM seems to protect against hepatic encephalopathy20. Nevertheless, response to rifaximin for MHE in this high risk group of patients with metabolic syndrome features has not been well established.
We hypothesized that patients with metabolic syndrome manifestations would have a poor response to rifaximin for MHE, associated with higher levels of systemic inflammation.
The main aim of the study was to evaluate the influence of metabolic syndrome manifestations on response to rifaximin in MHE patients. Secondary goals were to analyse: (I) specific cognitive and motor alterations and (II) inflammatory parameters associated with metabolic syndrome features and their response to rifaximin treatment.
Results
Study population and response to rifaximin
A total of 63 patients with cirrhosis (32 of these with MHE) and 30 healthy voluntary controls were included (Table 1). Baseline PHES was 0.7 ± 0.2, − 0.8 ± 0.3 and − 7.8 ± 0.6 in controls and patients without and with MHE, respectively.
According to PHES score at 3 months, 21 (66%) of the 32 patients that received rifaximin responded to treatment. None of non-responders at 3 months improved at 6 months. Mean PHES in responders was − 7.3 ± 0.7, − 3.2 ± 0.3 and − 3.3 ± 0.6 at study initiation and at 3 and 6 months of rifaximin, respectively. Mean PHES in non-responders was − 8.7 ± 1.1, − 8.3 ± 0.9 and − 10.5 ± 0.9 at baseline, 3 and 6 months of treatment, respectively. No significant differences in baseline PHES were found between responders and non-responders (p = 0.281).
Mean duration of treatment was 20 ± 3 months. Adverse events were registered in four (14%) patients (two headaches, one dizziness and one aggressiveness), with drug withdrawal in three cases (two non-responders) associated with symptomatic improvement. Adherence rate was 72% and was associated with better response to therapy (78% vs. 29% in the adherent and non-adherent groups, respectively; OR = 8.8; 95CI = 1.2–63.4; p = 0.021).
Mean follow-up from study inclusion until loss to follow-up, death or study closure was 33 ± 3 months. Only one patient (3%) was lost at follow-up, and six (19%) died during the study period. No differences were observed on follow-up between responding and non-responding groups (log-rank = 0.870; p = 0.351).
Influence of metabolic syndrome manifestations
Clinical factors according to rifaximin response are shown in Table 2. Risk factors of non-response to treatment were older age at study inclusion (mean difference 95CI = 1.7–12), all metabolic manifestations including metabolic syndrome (OR = 25; 95CI = 2.3–176), obesity (OR = 20; 95CI = 1.4–282), hypertension (OR = 8.5; 95CI = 1.5–49.5), DM (OR = 2.1; 95CI = 1.3–3.5), dyslipidemia (OR = 8.5; 95CI = 1.5–49.5) and NAFLD (OR = 14; 95CI = 1.3–150), and treatment with metformin (OR = 12; 95CI = 1.9–76.2) (Table 2). Accordingly, significantly higher overnight fasting glucose levels were observed in non-responding patients (mean difference 95CI = 12–64; p = 0.006) (Supplementary Table S1). The mean number of manifestations was 1 ± 0.2 in responders and 3 ± 0.4 in non-responders (mean difference 95CI = 1.3–3.2; p < 0.001). Moreover, a linear association was seen between number of metabolic manifestations and risk of non-response to rifaximin, so that 0%, 14%, 29%, 33% and 100% of patients with 0, 1, 2, 3 and ≥ 4 manifestations, respectively, failed to respond to treatment (p < 0.001). Clinical factors in patients with and without metabolic manifestations are shown in Table 2. No differences were observed in adherence depending on whether or not patients had metabolic manifestations (OR = 0.262; 95CI = 0.026–2.664; p = 0.362).
In multivariable analysis including age (OR = 1.05; 95CI = 1.005–1.097; p = 0.030) and metabolic manifestations (OR = 0.045; 95CI = 0.002–0.912; p = 0.043), both remained as independent predictors of response to rifaximin.
Ammonia levels showed no significant differences between baseline (44 ± 8 vs. 37 ± 12; 95CI = − 37.3–22.7; p = 0.620) and 3 months of rifaximin treatment (44 ± 7 vs. 40 ± 10; 95CI = − 30–22; p = 0.769) but were significantly higher at 6 months (52 ± 10 vs. 24 ± 6; 95CI = − 54–1.7; p = 0.038) in patients with metabolic syndrome-related disease than in those without this condition (Table 3).
Mean follow-up from study inclusion until loss to follow-up, death or study closure showed no differences either by presence of any metabolic manifestation (log-rank = 0.732; p = 0.392) or by manifestation subtypes (p > 0.05).
Cognitive and motor alterations
Considering specific cognitive and motor alterations, MHE patients showed worse performance in all psychometric tests compared to patients without MHE and controls. Although less marked, patients without MHE showed cognitive and motor impairment compared to controls (Table 4, and Supplementary Table S2).
Among patients with MHE, those with or without signs of metabolic syndrome did not show significant differences in baseline PHES (− 8.2 ± 0.7 vs. − 7.3 ± 1.1; p = 0.510) but displayed worse mental processing speed and selective attention in Oral SDMT (95CI = 4–22; p = 0.008); working memory with Digit Span (95CI = 0.2–4.6; p = 0.037); letter-number sequencing test (95CI = 1.1–5.4; p = 0.005) (Fig. 1), and visuo-motor coordination (95CI = 0.2–1.3; p = 0.013) (Table 4). Moreover, there was a significant correlation between increasing number of metabolic signs and worse performance in these tests: in Oral SDMT (r = − 0.438; p = 0.015), Digit Span (r = − 0.401; p = 0.028), letter-number sequencing (r = − 0.404; p = 0.033) and visuo-motor coordination (r = 0.431; p = 0.025) at baseline.
Performance of specific oral psychometric tests by controls, patients without MHE and patients with MHE according to presence of manifestations of metabolic syndrome at baseline. Oral SDMT: oral version of Symbol digit modalities test, expressed in correct pairings. Digit Span and Letter-Number sequencing test are expressed as right answers. Punctuation expressed as mean (SEM). *significant differences from controls (*p < 0.05; **p < 0.01; ***p < 0.001). αsignificant differences from no MHE (αp < 0.05; ααp < 0.01; αααp < 0.001). ^significant differences from patients with MHE without metabolic syndrome manifestations (^p < 0.05; ^^p < 0.01; ^^^p < 0.001).
At 3-month of rifaximin treatment, patients without manifestations of metabolic syndrome produced a significantly better PHES score than patients with manifestations (− 2.78 ± 0.4 vs. − 5.9 ± 0.7; 95CI = 1.4–4.8; p = 0.001). A strong inverse correlation was observed between PHES and number of metabolic syndrome-related alterations (r = − 0.623; p < 0.001) with reduced mean PHES score across categorized numbers of metabolic signs (− 4 ± 1.1, − 6.3 ± 1.4, − 7 ± 4 and − 7.6 ± 1.3 in patients with 1, 2, 3 and ≥ 4 manifestations, respectively; p = 0.002) (Fig. 2a). Patients with metabolic syndrome-related alterations not only failed to improve in psychometric test scores at 3 months of rifaximin treatment, but also showed slower mental processing speed and selective attention, with worse performance in the total number of words (95CI = 4–34; p = 0.015) and colours (95CI = 0.9–20; p = 0.032) in the Stroop test (Fig. 2b), worse concentration with total responses (95CI = 7.5–136; p = 0.030) in the d2 test, and worse bimanual coordination (95CI = 0.2–1.2; p = 0.007) (Table 4). Patients performed progressively worse in these tests as the number of metabolic manifestations increased: in total number of words (r = − 0.395; p = 0.038) and colours (r = − 0.375; p = 0.049) in the Stroop test, total responses (r = − 0.467; p = 0.019) in the d2 and in bimanual coordination test (r = 0.528; p = 0.004).
(a) Correlation between PHES and categorized number of metabolic manifestations at 3 months of rifaximin treatment. (b) Performance of Stroop test by controls, patients without MHE and patients with MHE according to presence of manifestations of metabolic syndrome at 3 months of rifaximin treatment. Stroop test: Congruent task: number of words read in 45 s; Neutral task: number of colours read in 45 s; Incongruent task: number of items completed in 45 s. Punctuation expressed as mean (SEM). *significant differences from controls (*p < 0.05; **p < 0.01; ***p < 0.001). α significant differences from no MHE (αp < 0.05; ααp < 0.01; αααp < 0.001). ^significant differences from patients with MHE without metabolic syndrome manifestations (^p < 0.05; ^^p < 0.01; ^^^p < 0.001).
At 6-month follow-up, patients with signs of metabolic syndrome showed a trend towards lower PHES compared to patients without these manifestations (− 6.3 ± 1.2 vs. − 3.6 ± 0.6; 95CI = − 0.2–5.6; p = 0.066). A moderate inverse correlation was maintained between PHES and number of metabolic syndrome manifestations (r = − 0.465; p = 0.034).
Inflammatory parameters
Treatment with rifaximin reduced the percentage of intermediate proinflammatory monocytes (CD14++CD16+), autoreactive T CD4+ lymphocytes (CD4+CD28−) and increased classical monocytes (CD14++CD16−) and non-autoreactive T CD4+ lymphocytes (CD4+CD28+) to almost normal values at 6 months in the responding group. Regarding percentage of activated T CD4+ lymphocytes (CD69), responding patients presented elevated baseline levels which were reversed with rifaximin, in contrast with the absence of elevated activated levels at study start or during follow-up in non-responding patients. Levels of IgG at the beginning of treatment were similar in both groups of response, but these levels dropped at 3 and 6 months in responding patients, with significant differences compared to non-responding patients (Supplementary Table S3).
Inflammatory parameters in patients with and without metabolic syndrome manifestations are described in Table 5 and Fig. 3. Rifaximin treatment reduced serum levels of several proinflammatory interleukins (IL) such as IL22 and CCL20 in both groups of patients, while IL17 and CXCL13 were only reduced in patients without metabolic syndrome manifestations.
Inflammatory parameters at baseline and at 3 and 6 months of rifaximin treatment according to metabolic syndrome manifestations. *significant differences from controls (*p < 0.05; **p < 0.01; ***p < 0.001). αsignificant differences from no MHE (αp < 0.05; ααp < 0.01; αααp < 0.001). βSignificant differences from patients without metabolic syndrome manifestations (βp < 0.05; ββp < 0.01; βββp < 0.001). ∂significant differences from baseline (∂p < 0.05; ∂∂p < 0.01; ∂∂∂p < 0.001). Abbreviations: CTL: controls; MHE and NMHE: patients with or without minimal hepatic encephalopathy, respectively; MM: metabolic syndrome manifestations.
Analysing by manifestations, lower levels of baseline activated T CD4+ lymphocytes (CD69) were observed in patients with obesity (1 ± 0.2 vs. 2.4 ± 0.7%; p = 0.076) and metabolic syndrome (1 ± 0.2 vs. 2.2 ± 0.5%; p = 0.039).
At 3 months of treatment, CX3CL1 levels were higher in patients with hypertension (1.1 ± 0.1 vs. 0.9 ± 0.1 ng/mL; p = 0.070) or metabolic syndrome (1.1 ± 0.1 vs. 0.9 ± 0.1 ng/mL; p = 0.047). AHR expression was also higher in patients with hypertension (1.7 ± 0.2 vs. 1.0 ± 0.1; p = 0.010), with increased levels compared to those prior to treatment initiation. IgG levels showed a tendency to be higher in patients with hypertension (157 ± 8 vs. 127 ± 11; p = 0.081) or metabolic syndrome (161 ± 11 vs. 130 ± 10; p = 0.090), correlating positively with the increasing number of metabolic syndrome manifestations (r = 0.635; p = 0.066).
Six months of treatment with rifaximin induced a higher reversion rate of classical (92.6 ± 0.7 vs. 88.4 ± 2.7; p = 0.047) and intermediate (5.8 ± 0.8 vs. 10.7 ± 1.9; p = 0.026) monocytes in patients without, than with, metabolic syndrome. We also observed increased levels of IL17 in patients with metabolic manifestations (3.0 ± 0.5 vs. 1.4 ± 0.3 pg/mL; p = 0.022) (Fig. 3e), and of CX3CL1 in patients with dyslipidaemia (1.2 ± 0.2 vs. 0.8 ± 0.1; p = 0.009), hypertension (1.2 ± 0.1 vs. 0.8 ± 0.1; p = 0.028) or metabolic syndrome (1.3 ± 0.2 vs. 0.9 ± 0.1; p = 0.020). Like the results at 3 months, at 6 months of rifaximin IgG levels tended to be raised in patients with hypertension (176 ± 34 vs. 112 ± 12; p = 0.062), metabolic syndrome (176 ± 34 vs. 112 ± 12; p = 0.062) or obesity (149 ± 7 vs. 99 ± 8; p = 0.040).
Discussion
The current post-approval, prospective follow-up study addresses the influence of metabolic syndrome clinical features on response to rifaximin in patients with MHE. Our findings demonstrate that metabolic syndrome-related diseases are associated with poorer response to rifaximin for management of MHE, with more cognitive and motor alterations and higher levels of inflammation compared to patients without these conditions.
Risk factors for MHE in our study were use of diuretics and decompensated cirrhosis, as previously described21,22, suggesting that our population was appropriate to evaluate response to rifaximin.
Rifaximin is an oral non-systemic broad spectrum antibiotic which inhibits bacterial RNA/protein synthesis by binding to bacterial DNA-dependent RNA-polymerase. Over the last decade, experimental and clinical evidence has suggested that rifaximin could modulate gut microbiota, reducing intestinal ammonia and toxin formation, and thus systemic inflammation23,24,25. Although hyperammonaemia and inflammatory response are the main pathogenic mechanisms of MHE26, there is still a subset of patients who do not respond to rifaximin, whose features are not well established.
The results of our study show a 66% response rate to rifaximin with a good adherence that lifted the response rate up to 78%, similar to previous clinical trials13,14. Response to treatment was evaluated at 3 and 6 months, with no response observed at 6 months in patients without response at 3 months indicating that no benefit is obtained by prolonging rifaximin in patients without response at 3 months.
An improvement in neurological alterations and quality of life has been reported with administration of rifaximin in patients with MHE13,14,23. A similar, progressive improvement of cognitive and motor alterations was observed in our treatment responder group. Nevertheless, working memory showed a subtler response, therefore, MHE patients are likely to maintain certain limitations in information storage and processing despite treatment.
Turning to rifaximin mechanisms of action, a reduction in ammonia levels occurred only non-significantly in the responding patient group, suggesting that rifaximin exerts its effect primarily by modulating the inflammatory changes associated with this entity, as has been proposed by Mangas-Losada et al.27. Parameters that improved selectively in responding patients were percentages of classical and intermediate monocytes, levels of IL-17, IL-21, IL-22, CXCL13 and IgG, so that reversing these alterations may be necessary to obtain a therapeutic response.
Interestingly, when analysing response-related immune alterations, the non-responding group did not present an increase in percentage of activated T CD4+ lymphocytes at treatment initiation. Since CD69 is an early activation marker28,29, it is conceivable that non-responding patients could be in a more advanced activation phase in which CD69 is not expressed, and which cannot be reversed by rifaximin. Thus, CD69 could be used as a biomarker in patient selection for treatment.
Several comorbidities, such as DM and insulin resistance, contribute to the development of OHE18. In other metabolic syndrome-related conditions such as NAFLD, cognitive dysfunction is an associated extrahepatic manifestation in up to 70% of cases15,16,17,30,31. The results of our study confirmed that patients with metabolic syndrome-associated disease exhibit cognitive impairment, with greater severity of these alterations as the number of manifestations increases. In response to the question of whether cognitive impairment in this group of patients was due to MHE or secondary to metabolic disorders, we could see that the control group had a similar proportion of metabolic syndrome and, nevertheless, had no cognitive abnormalities. Thus, there must be a synergy between chronic liver disease and metabolic disorders that conditions neurological alterations.
As a novel finding, patients with metabolic syndrome-related disease present poorer response to rifaximin prescribed for MHE. Also noteworthy was the fact that risk of non-response increases with the number of metabolic syndrome manifestations. Therefore, obtaining better response to rifaximin probably requires treating metabolic alterations concomitantly in this group of patients.
Several features of metabolic syndrome have been described in the pathogenesis of cognitive disturbances, such as systemic inflammation and vascular dysfunction, as well as NAFLD-linked features such as gut microbiota disruption or impairment of urea synthesis in the liver16. Nevertheless, the mechanisms underlying the worse treatment response in this patient subgroup are unknown. The results in our cohort showed that patients with metabolic syndrome clinical features have a more exacerbated pro-inflammatory environment that besides predisposing to neurological alterations leads to worse response to treatment. When comparing inflammatory alterations observed in patients with clinical manifestations of the metabolic syndrome to those that selectively improved in responding patients, the parameters determining lack of treatment response in this patient group may be percentage of intermediate monocytes, IL-17 and IgG levels. Intermediate (CD14++CD16+) monocytes are both producers of TNFα, IL-1β, IL-6, IL-18 and CCL20 and macrophage precursors, also with an inflammatory phenotype32,33. In turn monocytes and macrophages act as presenting antigen cells contributing to lymphocyte activation34. The humoral response plays an important role in development and progression of autoimmune and inflammatory disease35 and probably in MHE, demonstrated by increased IgG levels as a reflection of B lymphocyte activation in MHE patients. Moreover, patients with metabolic syndrome associated lower levels of activated T CD4+ lymphocytes at treatment initiation which could contribute to worse rifaximin response.
Among other factors, older age was also associated with non-response to treatment and multivariable analyses confirmed that both age and metabolic syndrome manifestations were independent predictors of response to rifaximin. For this reason, we believe that early establishment of treatment is crucial to bring benefits. Unlike in the Ampuero J study20, in ours, treatment with metformin was associated with higher risk of treatment non-response. Two factors could account for this: metformin treatment was prescribed in diabetic patients, and clinical data was collected transversally at the beginning of the study, a limitation that precluded establishing a causal relationship between treatment initiation and development of cognitive alterations.
The study also has several strengths to be highlighted. The findings are based on a well-characterized patient cohort, whose response to treatment was prospectively evaluated. Moreover, the study included a group of voluntary healthy controls as a reference for evaluation of neurological and inflammatory parameters. Nevertheless, further studies with blinded administration of rifaximin in patients with and without metabolic syndrome and larger sample size are warranted to confirm and establish more robust results.
In conclusion, patients with clinical signs of metabolic syndrome have poor response to rifaximin for MHE. They exhibit a higher proportion of neurological alterations which increase in severity as the number of metabolic syndrome disorders rises. This is associated with non-elevated levels of activated T CD4+ lymphocytes at treatment initiation and a pro-inflammatory environment not completely reversible with treatment. Careful and early evaluation, predominantly in patients with risk factors, and treating both MHE and metabolic syndrome manifestations, are crucial to obtain improvements in cognitive dysfunction in patients with cirrhosis.
Materials and methods
Study design and patient selection
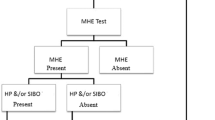
A multicentre, post-approval study with prospective follow-up was performed. Patients with cirrhosis treated in the Hepatology Unit of two tertiary centres (Clinic University Hospital of Valencia or Arnau de Vilanova, Spain) were screened for eligibility. Diagnosis of cirrhosis was based on liver histology or a combination of clinical, biochemical and imaging signs. Exclusion criteria were previous overt hepatic encephalopathy (OHE), neurological or psychiatric disorder, alcohol or drug consumption during the last 6 months, infection or antibiotic use (other than quinolones for spontaneous bacterial peritonitis) or gastrointestinal bleeding during the last 6 weeks, active antiviral treatment, transjugular intrahepatic portosystemic shunt or hepatocellular carcinoma. Patients were recruited consecutively between 2015 and 2019 and classified as with or without MHE using the Psychometric Hepatic Encephalopathy Score (PHES)36,37. A random group of these patients was selected to achieve the minimum sample size. A group of healthy voluntary controls without liver disease who met the same applicable exclusion criteria were included during the same study period. Patients and controls underwent clinical evaluation, psychometric tests and blood analyses to determine ammonia levels and biochemical measurements on the same day.
Definitions
Metabolic syndrome was defined according to the National Cholesterol Education Program Adult Treatment Panel III criteria38. Clinical manifestations of metabolic syndrome considered were obesity (waist circumference > 102 cm in men or > 88 cm in women); dyslipidemia (fasting triglycerides level ≥ 150 mg/dl, fasting high-density lipoprotein cholesterol level < 40 mg/dl in men or < 50 mg/dl in women, or on lipid-lowering treatment); hypertension (blood pressure ≥ 130/85 mmHg or on antihypertensive treatment); fasting blood sugar ≥ 110 mg/dl or on antidiabetic treatment, and NAFLD.
Model for End stage Liver Disease (MELD)39 and Child-Pugh40 score were used to evaluate disease severity. Cirrhosis decompensations assessment was made using clinical guideline diagnostic criteria41.
Psychometric tests
Diagnosis of MHE was made with a PHES score ≤ − 436,37.
Other psychometric tests performed to study specific cognitive and motor alterations were: (I) Stroop and oral version of Symbol Digit modalities test (Oral SDMT) from the Wechsler Adults Intelligence Scale to evaluate processing speed and selective attention; (II) d2 test to assess concentration; (III) Digit Span and Letter-Number sequencing tests from the Wechsler Adults Intelligence Scale to evaluate working memory; and (IV) bimanual and visuo-motor coordination tests to assess coordination42,43,44.
Laboratory measurements
Blood ammonia was measured with the Ammonia Test Kit II for the Pocket Chem BA system (Arkray, Inc., Kyoto, Japan).
Several inflammatory parameters were studied related to immunophenotype, cytokine levels in serum, transcription factors and IgG levels in plasma by flow cytometry, ELISA, quantitative PCR and Western Blot, respectively as described by Mangas-Losada et al.23.
Rifaximin treatment and follow-up
All MHE patients received treatment with rifaximin (400 mg/8 h orally) for at least 3 months. PHES was repeated at 3 months to evaluate response to treatment. Response to therapy was considered when PHES score was > − 4. Responding patients were maintained on treatment, while in non-responders treatment was maintained or withdrawn according to patient and physician preferences. Adverse events and withdrawal due to side effects were registered. Adherence was evaluated by direct patient interview and by the electronic medical prescription system45. Besides PHES, other psychometric tests and biochemical measurements were repeated at 3 months in all patients and at 6 months in those who continued on treatment.
Clinical surveillance was performed at 1, 3 and 6 months after inclusion and then every 6 months thereafter unless clinical deterioration occurred, until loss to follow-up, death or study closure in January 2020.
Statistical analysis
Differences according to rifaximin response were compared using Student’s t or Mann–Whitney U tests for continuous data and the chi-square, Fisher test or linear association for categorical data, as required. Measures of association between qualitative variables were reported as odds ratio (OR) with 95% confidence intervals (95CI) and p values. To study the independent contribution of each factor to rifaximin response, multivariate logistic regression analysis was performed including significant and relevant variables from the univariable analysis. Between-group comparison before and after rifaximin treatment was made using a paired t-test or Wilcoxon test for continuous data, and the McNemar test for categorical data. Follow-up was calculated with the Kaplan–Meier curve from day of study inclusion to date of censoring (loss of follow-up, death or study closure, whichever came first). Survival curves were compared by log-rank test. Correlations between number of metabolic syndrome signs and performance in psychometric tests or inflammatory levels were calculated by Spearman’s rank correlation. An ANOVA post-hoc Bonferroni test was also used to differentiate psychometric test performance and inflammatory parameters across categorized groups of metabolic manifestations. For sample size calculation, accepting an alpha risk of 0.05 and a beta risk of 0.2 in a two sided test, 22 and 11 subjects with and without metabolic syndrome manifestations were necessary to find a statistically significant proportion difference, expected to be of 0.9 in group 1 and 0.4 in group 2 with an anticipated drop-out rate of 10%. To our knowledge there are no studies that evaluate the influence of metabolic syndrome manifestations on response to Rifaximin. Therefore, parameters for proportion difference were estimated according to our past clinical experience23. The variable used for the calculation was the expected percentage of response in each of the study groups (with and without manifestations of the metabolic syndrome).
All tests were two sided and a p value < 0.05 was considered statistically significant. Analyses were performed using SPSS Statistics Version 22.
Ethics
The study was approved by the Clinic University Hospital of Valencia Institutional Review Board in 2015 (F-CE-GEva-15) and classified by the Spanish Agency of Medicines and Medical Devices (CMF-NRT-2017). The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki. All participants were enrolled after signing written informed consent.
Data availability
All data generated or analysed during this study is included in the published article.
References
Goyal, O., Sidhu, S. & Kishore, H. Incidence, prevalence and natural history of minimal hepatic encephalopathy in cirrhosis. J. Hepatol. 64, S279. https://doi.org/10.1016/S0168-8278(16)00334-2 (2016).
Groeneweg, M., Moerland, W., Quero, J. C., Krabbe, P. F. & Schalm, S. W. Screening of subclinical hepatic encephalopathy. J. Hepatol. 32, 748–753. https://doi.org/10.1016/s0168-8278(00)80243-3 (2000).
Sharma, P., Sharma, B. C., Puri, V. & Sarin, S. K. Critical flicker frequency: Diagnostic tool for minimal hepatic encephalopathy. J. Hepatol. 47, 67–73. https://doi.org/10.1016/j.jhep.2007.02.022 (2007).
Wang, J. et al. Prevalence of minimal hepatic encephalopathy and quality of life evaluations in hospitalized cirrhotic patients in China. World J. Gastroenterol. 19, 4984–4991. https://doi.org/10.3748/wjg.v19.i30.4984 (2013).
Nardone, R. et al. Minimal hepatic encephalopathy: A review. Neurosci. Res. 111, 1–12. https://doi.org/10.1016/j.neures.2016.04.009 (2016).
Damulin, I. V. Minimal hepatic encephalopathy: Current clinical and pathogenetic aspects. Ter. Arkh. 90, 89–93. https://doi.org/10.26442/terarkh201890289-93 (2018).
Wang, A.-J. et al. Natural history of covert hepatic encephalopathy: An observational study of 366 cirrhotic patients. World J. Gastroenterol. 23, 6321. https://doi.org/10.3748/wjg.v23.i34.6321 (2017).
Wong, R. J., Gish, R. G. & Ahmed, A. Hepatic encephalopathy is associated with significantly increased mortality among patients awaiting liver transplantation. Liver Transpl. 20, 1454–1461. https://doi.org/10.1002/lt.23981 (2014).
Agrawal, S., Umapathy, S. & Dhiman, R. K. Minimal hepatic encephalopathy impairs quality of life. J. Clin. Exp. Hepatol. 5, S42–S48. https://doi.org/10.1016/j.jceh.2014.11.006 (2015).
Ridola, L., Nardelli, S., Gioia, S. & Riggio, O. Quality of life in patients with minimal hepatic encephalopathy. World J. Gastroenterol. 24, 5446–5453. https://doi.org/10.3748/wjg.v24.i48.5446 (2018).
Ridola, L., Cardinale, V. & Riggio, O. The burden of minimal hepatic encephalopathy: From diagnosis to therapeutic strategies. Ann. Gastroenterol. 31, 151–164. https://doi.org/10.20524/aog.2018.0232 (2018).
Romero-Gómez, M., Boza, F., García-Valdecasas, M. S., García, E. & Aguilar-Reina, J. Subclinical hepatic encephalopathy predicts the development of overt hepatic encephalopathy. Am. J. Gastroenterol. 96, 2718–2723. https://doi.org/10.1111/j.1572-0241.2001.04130.x (2001).
Sidhu, S. S. et al. Rifaximin improves psychometric performance and health-related quality of life in patients with minimal hepatic encephalopathy (the RIME Trial). Am. J. Gastroenterol. 106, 307–316. https://doi.org/10.1038/ajg.2010.455 (2011).
Bajaj, J. S. et al. Rifaximin improves driving simulator performance in a randomized trial of patients with minimal hepatic encephalopathy. Gastroenterology 140, 478–487. https://doi.org/10.1053/j.gastro.2010.08.061 (2011).
Colognesi, M., Gabbia, D. & De Martin, S. Depression and cognitive impairment—Extrahepatic manifestations of NAFLD and NASH. Biomedicines. 8, 229. https://doi.org/10.3390/biomedicines8070229 (2020).
Kjærgaard, K. et al. Cognitive dysfunction in non-alcoholic fatty liver disease-current knowledge, mechanisms and perspectives. J. Clin. Med. https://doi.org/10.3390/jcm10040673 (2021).
Weinstein, A. A. et al. Cognitive performance in individuals with non-alcoholic fatty liver disease and/or type 2 diabetes mellitus. Psychosomatics 59, 567–574. https://doi.org/10.1016/j.psym.2018.06.001 (2018).
Ampuero, J., Ranchal, I., del Mar Díaz-Herrero. M., del Campo, J.A., Bautista, J.D., & Romero-Gómez, M. Role of diabetes mellitus on hepatic encephalopathy. Metab. Brain Dis. 28, 277–9. https://doi.org/10.1007/s11011-012-9354-2 (2013).
Biessels, G. J. & Despa, F. Cognitive decline and dementia in diabetes mellitus: Mechanisms and clinical implications. Nat. Rev. Endocrinol. 14, 591–604. https://doi.org/10.1038/s41574-018-0048-7 (2018).
Ampuero, J. et al. Metformin inhibits glutaminase activity and protects against hepatic encephalopathy. PLoS ONE 7, e49279. https://doi.org/10.1371/journal.pone.0049279 (2012).
Tapper, E. B. et al. Incidence and bedside predictors of the first episode of overt hepatic encephalopathy in patients with cirrhosis. Am. J. Gastroenterol. 115, 2017–2025. https://doi.org/10.14309/ajg.0000000000000762 (2020).
Guevara, M. et al. Risk factors for hepatic encephalopathy in patients with cirrhosis and refractory ascites: Relevance of serum sodium concentration. Liver Int. 30, 1137–1142. https://doi.org/10.1111/j.1478-3231.2010.02293.x (2010).
Mangas-Losada, A. et al. Selective improvement by rifaximin of changes in the immunophenotype in patients who improve minimal hepatic encephalopathy. J. Transl. Med. 17, 293. https://doi.org/10.1186/s12967-019-2046-5 (2019).
Bajaj, J. S. Review article: Potential mechanisms of action of rifaximin in the management of hepatic encephalopathy and other complications of cirrhosis. Aliment. Pharmacol. Ther. 43, 11–26. https://doi.org/10.1111/apt.13435 (2016).
Caraceni, P. et al. The use of rifaximin in patients with cirrhosis. Hepatology https://doi.org/10.1002/hep.31708 (2021).
Felipo, V. et al. Contribution of hyperammonemia and inflammatory factors to cognitive impairment in minimal hepatic encephalopathy. Metab. Brain Dis. 27, 51–58. https://doi.org/10.1007/s11011-011-9269-3 (2012).
Mangas-Losada, A. et al. Minimal hepatic encephalopathy is associated with expansion and activation of CD(4+)CD28(-), Th22 and Tfh and B lymphocytes. Sci. Rep. 7, 6683. https://doi.org/10.1038/s41598-017-05938-1 (2017).
González-Amaro, R., Cortés, J. R., Sánchez-Madrid, F. & Martín, P. Is CD69 an effective brake to control inflammatory diseases?. Trends Mol. Med. 19, 625–632. https://doi.org/10.1016/j.molmed.2013.07.006 (2013).
Shinoda, K. et al. Type II membrane protein CD69 regulates the formation of resting T-helper memory. Proc. Natl. Acad. Sci. U.S.A. 109, 7409–7414. https://doi.org/10.1073/pnas.1118539109 (2012).
Doward, L. C. et al. Development of a patient-reported outcome measure for non-alcoholic steatohepatitis (NASH-CHECK): Results of a qualitative study. Patient https://doi.org/10.1007/s40271-020-00485-w (2020).
Kennedy-Martin, T., Bae, J. P., Paczkowski, R. & Freeman, E. Health-related quality of life burden of nonalcoholic steatohepatitis: A robust pragmatic literature review. J. Patient Rep. Outcomes. 2, 28. https://doi.org/10.1186/s41687-018-0052-7 (2018).
Shi, C. & Pamer, E. G. Monocyte recruitment during infection and inflammation. Nat. Rev. Immunol. 11, 762–774. https://doi.org/10.1038/nri3070 (2011).
Ghosh, M., Xu, Y. & Pearse, D. D. Cyclic AMP is a key regulator of M1 to M2a phenotypic conversion of microglia in the presence of Th2 cytokines. J. Neuroinflammat. 13, 9. https://doi.org/10.1186/s12974-015-0463-9 (2016).
Chaplin, D. D. Overview of the immune response. J. Allergy Clin. Immunol. 125, S3-23. https://doi.org/10.1016/j.jaci.2009.12.980 (2010).
Meffre, E. & O’Connor, K. C. Impaired B-cell tolerance checkpoints promote the development of autoimmune diseases and pathogenic autoantibodies. Immunol. Rev. 292, 90–101. https://doi.org/10.1111/imr.12821 (2019).
Romero-Gómez, M., et al; Red Nacional de Investigación en Encefalopatía Hepática. Normality tables in the Spanish population for psychometric tests used in the diagnosis of minimal hepatic encephalopathy. Med. Clin. (Barc). 127, 246–9. https://doi.org/10.1157/13091264 (2006).
Weissenborn, K. Diagnosis of minimal hepatic encephalopathy. J. Clin. Exp. Hepatol. 5, S54–S59. https://doi.org/10.1016/j.jceh.2014.06.005 (2015).
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 285, 2486–97. https://doi.org/10.1001/jama.285.19.2486 (2001).
Malinchoc, M. et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31, 864–871. https://doi.org/10.1053/he.2000.5852 (2000).
Child, C. G. & Turcotte, J. G. Surgery and portal hypertension. Major Probl. Clin. Surg. 1, 1–85 (1964).
European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J. Hepatol. 69, 406–460. https://doi.org/10.1016/j.jhep.2018.03.024 (2018).
Felipo, V. et al. Patients with minimal hepatic encephalopathy show impaired mismatch negativity correlating with reduced performance in attention tests. Hepatology 55, 530–539. https://doi.org/10.1002/hep.24704 (2012).
Giménez-Garzó, C. et al. The PHES battery does not detect all cirrhotic patients with early neurological deficits, which are different in different patients. PLoS ONE 12, e0171211. https://doi.org/10.1371/journal.pone.0171211 (2017).
Erdodi, L. A. et al. Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV) processing speed scores as measures of noncredible responding: The third generation of embedded performance validity indicators. Psychol. Assess. 29, 148–157. https://doi.org/10.1037/pas0000319 (2017).
Osterberg, L. & Blaschke, T. Adherence to medication. N. Engl. J. Med. 353, 487–497. https://doi.org/10.1056/NEJMra050100 (2005).
Acknowledgements
This research was funded by Instituto de Salud Carlos III (FIS PI18/00150); Fundación Ramón Areces, Consellería de Educación Generalitat Valenciana (PROMETEOII/2018/051), cofunded with European Regional Development Funds (ERDF) and RFBR, grant number 18-015-00106. AF, JG and FCF have pre-doctoral contracts from Generalitat Valenciana (GRISOLIAP/2019/003; ACIF/2018/284, ACIF/2019/232), MPB has a Rio-Hortega contract from Instituto de Salud Carlos III (CM19/00011). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. Writing and statistical assistance was provided by INCLIVA Biomedical Research Institute.
Author information
Authors and Affiliations
Contributions
Study concept and design: MPB, DEG, MAS, VF, CMontoliu. Experiments and procedures: MPB, JJG, AF, FCF, TSM, CGG, EK, AU. Data collection: MPB, JJG, AF, FCF, CGG, DEG, JT, MR, CMontón, LD, JB, SB, EK, TSM, AU. Data analysis and interpretation: MPB, DEG, MAS, VF, CMontoliu. Drafting of final manuscript: MPB. Critical revision of manuscript: all authors. Study supervision: DEG, MAS, VF, CMontoliu. All authors have seen and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ballester, MP., Gallego, JJ., Fiorillo, A. et al. Metabolic syndrome is associated with poor response to rifaximin in minimal hepatic encephalopathy. Sci Rep 12, 2463 (2022). https://doi.org/10.1038/s41598-022-06416-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06416-z
This article is cited by
-
Improved cognition after rifaximin treatment is associated with changes in intra- and inter-brain network functional connectivity
Journal of Translational Medicine (2024)
-
Diabetes mellitus – risk factor and potential future target for hepatic encephalopathy in patients with liver cirrhosis?
Metabolic Brain Disease (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.