Abstract
Cerebral autoregulation (CA) is impaired during acute high-altitude (HA) exposure, however, effects of temporarily living high and working higher on CA require further investigation. In 18 healthy lowlanders (11 women), we hypothesized that the cerebral autoregulation index (ARI) assessed by the percentage change in middle cerebral artery peak blood velocity (Δ%MCAv)/percentage change in mean arterial blood pressure (Δ%MAP) induced by a sit-to-stand maneuver, is (i) reduced on Day1 at 5050 m compared to 520 m, (ii) is improved after 6 days at 5050 m, and (iii) is less impaired during re-exposure to 5050 m after 7 days at 520 m compared to Cycle1. Participants spent 4-8 h/day at 5050 m and slept at 2900 m similar to real-life working shifts. High/low ARI indicate impaired/intact CA, respectively. With the sit-to-stand at 520 m, mean (95% CI) in ΔMAP and ΔMCAv were − 26% (− 41 to − 10) and − 13% (− 19 to − 7), P < 0.001 both comparisons; mean ± SD in ARI was 0.58 ± 2.44Δ%/Δ%, respectively. On Day1 at 5050 m, ARI worsened compared to 520 m (3.29 ± 2.42Δ%/Δ%), P = 0.006 but improved with acclimatization (1.44 ± 2.43Δ%/Δ%, P = 0.039). ARI was less affected during re-exposure to 5050 m (1.22 ± 2.52Δ%/Δ%, P = 0.027 altitude-induced change between sojourns). This study showed that CA (i) is impaired during acute HA exposure, (ii) improves with living high, working higher and (iii) is ameliorated during re-exposure to HA.
Similar content being viewed by others
Introduction
Recent developments had led to an increase in the number of settlements and work places at altitude, especially, astronomical observation centers and resource extraction facilities that are often situated at very high altitudes (4000–5000 m). At the Atacama Large Millimeter/Submillimeter Array (ALMA), the largest ground-based telescope station worldwide, employees sleep at 2900 m and work at 5050 m for 7 days, and recover for 7 days at their permanent residence, normally near sea level. These repeated live high, work higher periods may have adverse effects on health, performance and safety of workers1,2,3.
Cerebral autoregulation (CA) protects the brain by a negative feedback loop mechanism, maintaining constant cerebral blood flow and oxygen delivery independent of fluctuations in systemic blood pressure4. Impaired CA results in systemic blood pressure associated cerebral blood flow fluctuations and may cause under-perfusion and inadequate oxygen delivery, or over-perfusion of capillaries with consequent disruption of the blood–brain barrier, capillary damage and micro-hemorrhages5. Furthermore, impaired CA has been shown to have consequences on the cerebral function and is related to cognitive impairment5.
At altitude, the arterial partial pressures of O2 and CO2, two key factors influencing CA functionality, are reduced6. Studies investigating CA functionality at different altitudes have reported persistent CA impairment with acute7 and prolonged high altitude exposure of up to 2 weeks compared to values reported near sea level8. However, real-life working shifts as implied in ALMA require workers to sleep at 2900 m and work at 5050 m. This pattern of exposure to high altitude (living high, working higher) induces an intermittent hypobaric hypoxic exposure, which might have beneficial effects on the CA functionality as suggested for intermittent hypoxic training in patients with Alzheimer diseases9. Furthermore, studies investigating the effects of repeated high altitude exposure showed milder reductions in O2 and CO2 when compared to previous altitude sojourns2,10. However, whether these improvements in arterial blood gases might have a beneficial effect on the CA has not been studied. Therefore, the purpose of this study was to test the hypotheses that CA is impaired during acute high-altitude exposure and that acclimatization (with an intermittent schedule of daily ascents to very high altitude, but sleeping at moderate altitude), and a 2nd altitude sojourn, ameliorates CA functionality compared to the first acute high altitude exposure. Furthermore, this study assessed whether altitude exposure has sustained effects on CA functionality after descending to low altitude.
Methods
Design and study setting
Data of the current study were collected within a prospective cohort study with the purpose to investigate the effects of acute, prolonged and repeated altitude exposure on cognitive performance in healthy subjects2. Results of the present study have not been published elsewhere.
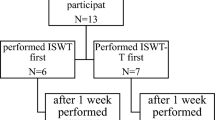
The ascent and assessment schedule is illustrated in Fig. 1. At Santiago de Chile (520 m), participants performed a familiarization and baseline session separated by a one-day rest interval. The day after, participants traveled by plane and bus (2 h each) to the ALMA Operation Support Facility (ASF; 2900 m) and spent seven consecutive nights at 2900 m. Each morning, participants were driven by car (45 min travel time) to the ALMA Operation Site (AOS; 5050 m), where they stayed up to 8 h without oxygen supplementation or any mediation against symptoms of acute mountain sickness. Measurements at 5050 m were performed on the 1st and 6th day and repeated on the day after descending to 520 m. This assessment schedule was repeated after a 7-day recovery period at 520 m. Measurements within each participant were conducted during the same time of day. To ensure balanced between-subject total exposure time to 5050 m, individual transportation schedules to 5050 m were applied. Participants were asked to refrain from alcohol throughout the expedition and to keep caffeine intake and exercise sequence and intensity as usual.
Study design. After a familiarization session at Santiago de Chile (520 m), participants underwent baseline assessments the day preceding travelling to high altitude. Participants travelled to the ALMA Operations Support Facility (ASF—2900 m) and stayed for one night before beginning daily sojourns to the Array Operations Site (AOS—5050 m). Participants alternated between 2900 m (sleeping) and 5050 m (up to 8 h/day). After a one-week recovery period at 520 m, participants performed a second, identical altitude cycle. Arrows indicate experimental testing days and headings indicate the condition of interest.
Participants
Healthy, altitude-naïve men and women, aged between 18 to 30 years were recruited from the University of Calgary, Canada (N = 18, altitude of 1100 m). Participants were instructed to avoid any overnight stays at altitudes > 1500 m within four weeks before the study. All participants provided written informed consent. The study was approved by the Conjoint Health Research Ethics Board of the University of Calgary (Ethics ID: REB 15-2709) and the Cantonal Ethics Committee of Zurich (2016-00048). The main trial was registered at ClinicalTrials.gov (NCT02731456). All methods were carried out in accordance with relevant guidelines and regulations.
Protocol and measurements
Sitting values were collected and averaged over 120 stable and artifact-free heart beats at the end of a 10-min sitting position in a comfortable chair. To assess CA functionality, participants stood up in less than 1 s and remained in standing position for 1 min11. The effect of standing up was measured by averaging the first 15 beats in standing position. This procedure was repeated and values were averaged within each subject. Due to the unknown effects of acute, prolonged and repeated exposures to high altitude on orthostatic tolerance and the blood pressure response to standing up, no threshold for a successful maneuver was applied (i.e. a minimum reduction of 15 mmHg from sitting to standing).
Clinical assessments
Clinical assessment included height, weight, oxygen saturation by pulse oximetry (SpO2) and heart rate measurements, as well as the environmental symptoms questionnaire cerebral score (AMSc) to assess acute mountain sickness (AMS)12. The AMSc comprises 11 questions on AMS symptoms (feel sick, feel hungover, coordination off, dim vision, lightheaded, headache, dizzy, loss of appetite, feel weak, nausea, faint) rated from 0 (not at all) to 5 (extreme). A weighted AMSc score ≥ 0.7 were assumed to indicate the presence of AMS.
Transcranial Doppler ultrasound
A 2-MHz Doppler probe (TOCM, Multigon Industries, New York, USA) was placed over the right temporal window to measure the peak blood velocity (MCAv) in the middle cerebral artery. The MCA was identified by systematic searches over the zygomatic arch and by varying the angle and position of the probe13. After adjustment and optimization of depth and angle of the probe, a marker was placed on the skin. A headband device was installed around the subject’s head and the Doppler probe was attached. This setting allowed optimal insonation position and angle during the complete protocol. To ensure a high standardization and reproducibility, the Doppler settings, probe position, insonation angle and depth were assessed during the familiarization period and the same settings were applied throughout the study. The cerebral autoregulation index (ARI) was defined by the ability of the CA to maintain a constant MCAv despite a rapid change in systemic blood pressure during a sit-to-stand maneuver. ARI was calculated as previously reported14:
Therefore, higher values in ARI represent larger MAP-induced MCAv fluctuations, corresponding to worse cerebral autoregulation, whereas smaller values in ARI corresponded to intact cerebral autoregulation. Cerebrovascular resistance and conductance indexes were calculated as MAP divided by the MCAv (CVRi) or vice versa (CVCi).
Additional physiological assessments
Continuous SpO2, heart rate and beat-by-beat systemic mean artery blood pressure (MAP) were assessed non-invasively by the finger-cuff technique (Finometer Midi, FMS, The Netherlands) and calibrated by brachialis sphygmomanometric measurements. Breath-by-breath end-expiratory partial pressure of CO2 (PETCO2) and breathing frequency were assessed by capnography (Capnocheck Sleep, Smiths Medical PM Inc., Waukesha, Wi, USA). The capnograph was calibrated daily with a calibration gas containing 5% CO2 and the continuous PETCO2 curve was re-calculated based on (if any) observed deviations.
Outcomes
The main outcome of this study was the ARI (Δ%MCAv/Δ%MAP) and the effects of acute, prolonged and re-exposure to very high altitude. Additional outcomes were changes in explanatory cerebral, respiratory and cardiac variables. No a priori sample size estimation has been performed.
Hypotheses
The three main hypotheses were that (i) acute high-altitude exposure impairs ARI (Δ%MCAv/Δ%MAP), (ii) 6 days of live high, work higher improves ARI (Δ%MCAv/Δ%MAP) and (iii) a 2nd compared to the 1st ascent to 5050 m has a lower impact on the altitude-related ARI impairment. An additional hypothesis was that CA functionality is immediately restored the day after descending to 520 m.
Data analysis
The primary outcome was tested for normality by the Shapiro Wilk test. Due to the non-normally distributed data, mixed ordered logistic regression using the interaction between altitude (520 m and 5050 m), day at altitude (1st and 6th day) and number of altitude sojourns (1st and 2nd sojourn) as fixed effects, and participants as random effects was applied. Secondary outcomes were analyzed using mixed linear regression models. To avoid unnecessary multiple testing and false positive results, comparisons between day 6 at 5050 m vs. baseline (both, during the 1st and 2nd sojourn), descent vs. day 1 at 5050 m (both, during the 1st and 2nd sojourn) and baseline during the 2nd vs 1st sojourn were not statistically compared. To elucidate the underlying factors influencing ARI (Δ%/Δ%) or AMS, univariate and multivariate mixed linear regressions including baseline characteristics, SpO2, PETCO2, MAP and MCAv were performed. Statistical significance was assumed when P < 0.05 and 95% confidence intervals of mean differences did not overlap zero.
Results
A total of 18 healthy participants (11 women) with a mean age of 24 ± 4 years and BMI of 22.8 ± 3.1 kg/m2 were included in the final analysis. From a total of 216 planned 8 h sessions at 5050 m, 14 (6%) had to be terminated prematurely due to severe AMS symptoms. Participant characteristics are presented in Table 1. Cardiorespiratory and cerebrovascular outcomes are described in Table 2.
Effect of acute altitude exposure (1st day at 5050 m compared to 520 m)
With acute exposure to 5050 m, participants had lower values in SpO2, mean ± SD, 77.6 ± 3.4% vs. 96.5 ± 3.4%, lower values in PETCO2, 24.5 ± 3.0 mmHg vs. 33.9 ± 2.5 mmHg and higher heart rates, 93 ± 13 bpm vs. 70 ± 13 bpm and more symptoms of AMS assessed by the AMSc score, 0.94 ± 0.38 vs. 0.12 ± 0.38 compared to 520 m (P < 0.001 all comparisons). There was no acute altitude effect on MAP compared to 520 m (P = 0.939), whereas sitting mean MCAv significantly increased from 57.9 ± 10.2 cm/s to 62.1 ± 10.2 cm/s (P = 0.036) without altering CVRi or CVCi. The sit-to-stand maneuver at 5050 m caused a stronger drop in MCAv despite a milder drop in MAP, resulting in a significantly worse ARI compared to 520 m (3.29 ± 2.42 Δ%/Δ% vs. 0.58 ± 2.44 Δ%/Δ%, P = 0.007; 3.50 ± 2.91 Δ%/ΔmmHg vs. 0.85 ± 2.90 Δ%/ΔmmHg, P = 0.017) (Table 2, Fig. 2).
Cerebral autoregulation index assessed during a sit-to-stand maneuver. Panel (A) Mean arterial pressure (MAP) percentage change between standing versus sitting. Panel (B) Mean middle cerebral artery peak blood velocity (MCAv) percent change between standing versus sitting. Panel (C) Cerebral autoregulation index calculated by Δ%MCAv/Δ%MAP with a sit-to-stand maneuver. Standing values were obtained by averaging 15 beats following standing up < 1 s. #P < 0.05 between the acute altitude-induced effect during the 2nd compared to the 1st sojourn; *P < 0.05 between the acclimatization effect during the 2nd compared to the 1st sojourn; †P < 0.05 between the descent effect during the 2nd compared to the 1st sojourn.
Effect of prolonged intermittent altitude exposure (6th versus 1st day at 5050 m)
After 6 days of intermittingly ascending to 5050 m and sleeping at 2900 m, hemoglobin concentration and SpO2 were higher (83.0 ± 2.5% vs. 77.6 ± 2.5%, P < 0.001) and AMS symptoms lower, without altering PETCO2 or breathing frequency compared to the 1st day at 5050 m. With acclimatization, MAP, MCAv, CVRi and CVCi remained unchanged. Compared to the 1st day at 5050 m, the sit-to-stand test caused a similar MCAv decrease despite a stronger drop in MAP, resulting in significantly improved ARI (Δ%/Δ%) compared to the 1st day at 5050 m (P = 0.039) (Table 2, Fig. 2).
Effect of descent from high altitude (520 m versus 6th day at 5050 m)
On the day after descending from 5050 to 520 m, participants showed persistent PETCO2 reductions (P = 0.027) and worse ARI (Δ%/Δ%) (P = 0.017) values compared to pre-ascent evaluations. After 1-week recovery period at 520 m, SpO2 and PETCO2 recovered to pre-ascent values. ARI (Δ%/Δ%) tended to remain impaired but was not statistically different compared to pre-ascent assessments (P = 0.067).
Effect of a second altitude sojourn (2nd compared to 1st sojourn at 5050 m)
Acute exposure during the 2nd compared to the 1st sojourn at 5050 m was accompanied with less hypoxemia and less hypocapnia. Heart rate similarly increased and breathing frequency remained unchanged as seen during the 1st sojourn at 5050 m. Compared to the 1st sojourn, MCAv did not increase during acute altitude exposure and ARI (Δ%/Δ%) deteriorated less compared to the 1st sojourn (Odds ratio of 0.10, 95% CI 0.01–0.76, P = 0.027) (Table 2, Fig. 2).
SpO2 and PETCO2 remained higher after acclimatization in the 2nd compared to the 1st sojourn at 5050 m. This was accompanied with a further increase in hemoglobin concentration. MCAv, MAP and ARI (Δ%/Δ%) remained stable after acclimatization (Odds ratio for ARI of 7.3, 95% CI 0.95–56.7, P = 0.056) (Table 2).
When the participants descended from the 2nd sojourn at 5050 m, they persistently showed lower PETCO2, lower MAP and better ARI (Δ%/Δ%) values compared to the values obtained on the day after descending from the 1st sojourn (Odds ratio of 0.12, 95% CI 0.02–0.82, P = 0.030).
Predictors for AMS and ARI (Δ%/Δ%)
Predictors of AMS severity at 5050 m assessed by multivariate regression analysis were acute exposure, low sitting PETCO2 and high ARI (Δ%/Δ%) values (Table 3). Only higher MAP values remained as an independent predictor of CA impairment defined by ARI (Δ%/Δ%) (Table 4).
Discussion
This study focused on the cerebral autoregulatory ability to protect the brain from rapid systemic blood pressure falls in maneuvers like the sit-to-stand test during acute, prolonged and repeated exposure to very high altitude (5050 m), a schedule often seen in high altitude shift workers, temporarily living high and working higher. The present findings suggest that cerebral autoregulation was impaired during acute exposure, but improved after a 7-day stay at high altitude (with a sleeping and working altitude of 2900 m and 5050 m, respectively). Strikingly, descending to lower altitude did not immediately improve CA and some impairments of the CA persisted. Moreover, novel findings of this study suggest that a 2nd altitude sojourn after one week at low altitude had a milder effect on the CA functionality, indicating that workers exposed to repeated high altitude exposures might be protected from initial CA impairments seen during the first acute high-altitude exposure. Exploratory analysis revealed that acute exposure to 5050 m, worse ARI (Δ%/Δ%) and lower PETCO2 values were associated with higher AMS severity.
This study used a straightforward approach to describe CA proposed by a recent meta-analysis, by calculating the percent change in MCAv divided by the percent change from baseline in MAP14. The meta-analysis comprised 49 studies, whereas 41 studies used transcranial Doppler measurements to assess MCAv, a surrogate for cerebral blood flow. The average slopes proposed by the meta-analysis for a healthy population were 0.82 ± 0.77%ΔMCAv/%ΔMAP and 0.97 ± 0.91%ΔMCAv/ΔmmHg MAP. Therefore, the obtained baseline values at 520 m in our cohort were within the 95% confidence intervals of the cited study (Table 2, 0.58 ± 2.67%ΔMCAv/%ΔMAP and 0.85 ± 3.18%ΔMCAv/mmHg MAP). Furthermore, the current study used the sit-to-stand maneuver to provoke a change in MAP and MCAv. Although other interventions might have resulted in larger changes in these variables, the applied sit-to-stand maneuver showed a mean difference (95% CI) in MAP and MCAv at 520 m of − 26% (− 41 to − 10) and − 13% (− 19 to − 7) from sitting values, respectively. These changes are comparable with previous studies11,15. Notably, the effect of standing up on the CA was calculated by averaging 15 beats following the maneuver, and is in contrast to other studies choosing the nadir in MAP and MCAv following standing up15. However, by averaging 15 beats following the maneuver, findings remained less prone to artifacts and selection bias and were easily reproducible. In contrast, when averaging 15 beats, a shorter observation time of the CA due to higher heart rates at 5050 m was assessed and might have influenced our results.
Several previous field studies suggested that acute high-altitude exposure impairs CA functionality3,16,17,18,19. However, only a few studies have focused on the high-altitude acclimatization effect on the CA functionality. Subudhi et al. showed in 21 healthy subjects exposed to 3800–5260 m for 15 days that CA remained impaired compared to measurements near sea level and compared to the 1st day at 5260 m. This was confirmed by another study exposing 11 individuals for 4 weeks to 5260 m17. Both studies used transfer function analysis in comparison to the 2-point assessment of MCAv and MAP used in the current trial. However, these findings are in accordance with the current study showing that acclimatization does not restore sea-level values in CA.
The CA functionality depends on the ability to vasodilate or vasoconstrict cerebral arterioles in response to a stimulus. Acute high altitude exposure was associated with hypoxemia and hypocapnia, whereas hypoxemia presumably dominantly dilated cerebral arterioles, therefore, the MCAv increased during acute exposure to 5050 m. In the current study, 6 days of intermittently sleeping and working at 2900 and 5050 m, respectively, did improve arterial oxygenation by an increase in hemoglobin concentration and to a lower extend due to progressive hyperventilation, normally observed with altitude acclimatization. Whether the absent progression of hypocapnia is a result of the intermittent exposure schedule or due to lack of statistical power, remains to be elucidated. However, this finding is relevant since it has been shown that hypocapnia does augment CA functionality under hypoxic conditions20. Therefore, improvement of CA functionality with acclimatization seems to be more related to improved oxygenation than progressive hypocapnia. However, this study was not able to investigate other important factors potentially explaining alterations of CA functionality during acute or prolonged altitude exposure, i.e. altered CBF sensitivity to acute O2 and CO2 changes, sympathetic hyperactivity, alteration of endothelial function or neural nitric oxide synthase activity among others7,17.
In contrast, the current findings also support the thesis that acclimatization, at least partly, mitigated CA impairment, which was not observed in the two mentioned studies. A possible explanation might be the unique intermittent hypobaric hypoxic protocol used in this study (staying at 5050 m and sleeping at 2900 m), which might have altered autonomic nervous system activity, endothelial function or enhanced the sensitivity to hypoxia and hypocapnia, which might have improved the CA functionality over the time course of 6 days. Although, this has never been studied in detail, one trial applying 14 days of intermittent hypoxia (FiO2 0.10, sessions of 5 × 4 min per day) showed diminished cerebral blood flow fluctuation to hypocapnia and hypercapnia after the intervention22, indicating improved CA functionality. Furthermore, beneficial effects of intermittent hypoxic training on the cerebrovascular response in Alzheimer patients have been reported9. This might explain the improved CA functionality with prolonged hypoxia during acclimatization. Other possible factors explaining the inconsistent findings of the acclimatization effect on CA between studies might be differences in the definition of “day 1” at high altitude, duration of the high altitude stay, intervention (sit-to-stand versus rest), analysis method (2-point assessment of MCAv and MAP versus transfer function analysis) or study protocol (staying at 5050 m and sleeping at 2900 m versus staying at 5260 m). Furthermore, in healthy lowlanders, it has been shown that the functionality of cerebral autoregulation is more protective to blood pressure elevations (CA ability to vasoconstrict blood vessels) than blood pressure reductions (CA ability to vasodilate)14. Since spontaneous blood pressure changes assessed by transfer function analysis includes both blood pressure elevations and reductions, this might provide different information about the CA functionality than exclusive blood pressure reductions induced by a sit-to-stand maneuver. This non-linear CA functionality might partly explain previously reported opposite findings at high altitude8,23. However, whether the altitude-induced CA impairment differs in the ability to protect the brain from blood pressure elevations versus blood pressure reductions has not been studied in detail.
Moreover, this study provides novel findings supporting the hypothesis that CA is less impaired during a second sojourn at very high altitude. Contrary to a previous study by Subudhi et al.10, which concluded that re-exposure to 5260 m after 7 days at sea level similarly impaired CA (based on transfer function analysis). Apart of the methodological differences outlined above, they have not performed a second baseline measurement and might have missed the circumstance that the participants had some retained CA impairments after 1 week at low altitude, as seen in the current study (Table 2). This would result in a different baseline and therefore, smaller altitude-induced difference in CA functionality. The observed smaller altitude-induced impact on CA functionality might be partly explained by preserved oxygen delivery towards the brain by elevated hemoglobin concentration, altered sensitivity to O2 and CO2, less altitude-induced hypoxemia, or by less vasodilatation of the small cerebral arteries allowing the CA to induce vasodilation in response to the sit-to-stand maneuver.
Whether the trend (P = 0.067) of persistent impairment of CA throughout 1-week post-altitude exposure was by chance or by lacking power to reach statistical significance requires further investigation. Findings on the day after the second descent to 520 m suggest already improved CA after the 2nd sojourn, indicating that CA functionality was normalized at low altitude after repeated exposure. Nevertheless, persistent impairment of CA after altitude sojourns would have an unknown impact on the safety and health of high-altitude workers and needs further investigation.
The assessment of the CA at high altitude remains challenging; many influential physiological parameters change, therefore, invasive and highly sophisticated measurements would be required and large sample sizes would be needed to account for the influence of various confounders. Often, changes of the MCAv assessed by TCD are assumed to reflect changes in cerebral blood flow. However, MCAv assessments at an altitude of 5050 m are influenced by changes of PaO2 and PaCO2, potentially changing the diameter of the MCA. In accordance, MCA diameter increases under isocapnic hypoxic condition (FiO2 11%, equivalent to 5200 m)24 whereas the MCA cross-sectional area decreased after a reduction of PETCO2 of 11–13 mmHg by voluntary hyperventilation (5.6–5.3 mm2, P < 0.01). However, 6/15 (40%) showed < 5% changes in the MCA cross-sectional area with hypocapnia25. In contrast, under hypocapnic hypoxic conditions seen at altitude, measurements have shown no26 or increased MCA diameter and cross-sectional area21. Therefore, one study in 24 participants applying 3-T Magnetic Resonance Imaging showed no changes of MCA diameter up to 5300 m (5.33 mm at sea level, 5.23 mm at 5300 m), and marked changes at 6400 m (6.66 mm), while another study found an increase in MCA diameter in 8 participants at 5050 m21,26. Although, the current study observed physiological changes in O2 and CO2 between altitudes, sojourns and with acclimatization, within the limits of the above mentioned studies (9.5 mmHg PetCO2 difference between baseline and day 6 at 5050 m during the first sojourn), no assessment of the MCA vessel caliber has been performed and any alterations in the MCA diameter cannot be ruled out. Nevertheless, the applied orthostatic challenge by the sit-to-stand maneuver is unlikely to have induced changes in the MCA diameter. Therefore, computed ARI values are reasonable assumed to reflect CA functionality. As mentioned before, this study applied a simple sit-to-stand maneuver to assess CA functionality rather than previously applied transfer function analysis, lower body negative pressure or injection of phenylephrine. The rationale was the practicality of the sit-to-stand test and the limited accessibility of the research facility at 5050 m as well as the rationale to provide data on the CA functionality representative for common daily activities of high altitude workers. In line with this rationale, calculation of the CA functionality by ARI (Δ%MCAv/Δ%MAP), suggested by Numan et al.14, was applied. Therefore, obtained high altitude ARI values can be compared to lowland reference values provided in the meta-analysis from Numan et al., avoiding differences in technical settings often seen during transfer function analyses (e.g. differences in sampling frequency, normalization, de-trending, filtering, window size). However, no threshold for a minimum MAP reduction with standing up was applied. The rationale was to avoid one-sided eliminations of potentially correct measurements due to improvements in orthostatic tolerance and blood pressure regulations. However, including maneuvers provoking only small MAP changes might have introduced some variability of ARI and might have resulted in lower statistical power to detect effects of acute, prolonged and repeated high altitude exposure on CA.
Conclusions
First, this study confirmed CA impairment during acute exposure to very high altitude. Further, novel findings reported here are the partial improvements in CA over 7 days living high (sleeping at 2900 m) and working higher (5050 m). Additionally, we found a milder altitude-induced impact on the CA functionality during a 2nd similar sojourn at high altitude but a trend of persistent CA impairment up to 1-week post-altitude exposure, which resolved after the 2nd high altitude sojourn. Taken together, these findings suggest that workers commencing their high altitude work based on a repeated living high and working higher work schedule might be initially at risk for over and under-perfusion of brain areas, whereas staying and a 2nd working cycles at high altitude ameliorate CA functionality. Whether the improved CA functionality during the second high-altitude cycle indicates a protection also for several repeated work-shift cycles at high altitude remains to be determined.
Data availability
Anonymized data underlying this study can be requested by qualified researchers providing an approved proposal.
Abbreviations
- ALMA:
-
Atacama Large Millimeter/Submillimeter Array
- ALMA ASF:
-
ALMA Operation Support Facility, 2900 m
- ALMA AOS:
-
ALMA Operation Site, 5050 m
- AMS:
-
Acute mountain sickness
- AMSc:
-
Environmental symptom questionnaire, cerebral score
- ARI:
-
Cerebral autoregulation index
- CA:
-
Cerebral autoregulation
- CVCi:
-
Cerebrovascular conductance index
- CVRi:
-
Cerebrovascular resistance index
- MAP:
-
Mean arterial blood pressure
- MCA:
-
Middle cerebral artery
- MCAv:
-
Middle cerebral artery peak blood velocity
- PETCO2 :
-
End-tidal partial pressure of carbon dioxide
- SpO2 :
-
Arterial oxygen saturation measured by pulse oximetry
References
Pun, M. et al. Effects on cognitive functioning of acute, subacute and repeated exposures to high altitude. Front. Physiol. 9, 1131. https://doi.org/10.3389/fphys.2018.01131 (2018).
Pun, M. et al. Effect of Acute, subacute, and repeated exposure to high altitude (5050 m) on psychomotor vigilance. Front. Physiol. 9, 677. https://doi.org/10.3389/fphys.2018.00677 (2018).
Subudhi, A. W. et al. AltitudeOmics: Cerebral autoregulation during ascent, acclimatization, and re-exposure to high altitude and its relation with acute mountain sickness. J. Appl. Physiol. 1985(116), 724–729. https://doi.org/10.1152/japplphysiol.00880.2013 (2014).
Fantini, S., Sassaroli, A., Tgavalekos, K. T. & Kornbluth, J. Cerebral blood flow and autoregulation: Current measurement techniques and prospects for noninvasive optical methods. Neurophotonics 3, 031411. https://doi.org/10.1117/1.NPh.3.3.031411 (2016).
Toth, P., Tarantini, S., Csiszar, A. & Ungvari, Z. Functional vascular contributions to cognitive impairment and dementia: Mechanisms and consequences of cerebral autoregulatory dysfunction, endothelial impairment, and neurovascular uncoupling in aging. Am. J. Physiol. Heart Circ. Physiol. 312, H1–H20. https://doi.org/10.1152/ajpheart.00581.2016 (2017).
West, J. B., Schoene, R. B., Luks, A. M. & Milledge, J. S. High Altitude Medicine and Physiology 5th edn. (CRC Press, 2012).
Brugniaux, J. V., Hodges, A. N., Hanly, P. J. & Poulin, M. J. Cerebrovascular responses to altitude. Respir. Physiol. Neurobiol. 158, 212–223. https://doi.org/10.1016/j.resp.2007.04.008 (2007).
Subudhi, A. W. et al. Cerebral autoregulation index at high altitude assessed by thigh-cuff and transfer function analysis techniques. Exp. Physiol. 100, 173–181. https://doi.org/10.1113/expphysiol.2014.082479 (2015).
Manukhina, E. B., Downey, H. F., Shi, X. & Mallet, R. T. Intermittent hypoxia training protects cerebrovascular function in Alzheimer’s disease. Exp. Biol. Med. (Maywood, N.J.) 241, 1351–1363. https://doi.org/10.1177/1535370216649060 (2016).
Subudhi, A. W. et al. AltitudeOmics: The integrative physiology of human acclimatization to hypobaric hypoxia and its retention upon reascent. PLoS ONE 9, e92191. https://doi.org/10.1371/journal.pone.0092191 (2014).
Lipsitz, L. A., Mukai, S., Hamner, J., Gagnon, M. & Babikian, V. Dynamic regulation of middle cerebral artery blood flow velocity in aging and hypertension. Stroke 31, 1897–1903. https://doi.org/10.1161/01.str.31.8.1897 (2000).
Sampson, J. B., Cymerman, A., Burse, R. L., Maher, J. T. & Rock, P. B. Procedures for the measurement of acute mountain sickness. Aviat. Space Environ. Med. 54, 1063–1073 (1983).
Poulin, M. J., Fatemian, M., Tansley, J. G., O’Connor, D. F. & Robbins, P. A. Changes in cerebral blood flow during and after 48 h of both isocapnic and poikilocapnic hypoxia in humans. Exp. Physiol. 87, 633–642 (2002).
Numan, T. et al. Static autoregulation in humans: A review and reanalysis. Med. Eng. Phys. 36, 1487–1495. https://doi.org/10.1016/j.medengphy.2014.08.001 (2014).
Labrecque, L. et al. Dynamic cerebral autoregulation is attenuated in young fit women. Physiol. Rep. 7, e13984. https://doi.org/10.14814/phy2.13984 (2019).
Ainslie, P. N. et al. Differential effects of acute hypoxia and high altitude on cerebral blood flow velocity and dynamic cerebral autoregulation: Alterations with hyperoxia. J. Appl. Physiol. 1985(104), 490–498. https://doi.org/10.1152/japplphysiol.00778.2007 (2008).
Iwasaki, K. et al. Impaired dynamic cerebral autoregulation at extreme high altitude even after acclimatization. J. Cereb. Blood Flow Metab. 31, 283–292. https://doi.org/10.1038/jcbfm.2010.88 (2011).
Subudhi, A. W., Panerai, R. B. & Roach, R. C. Effects of hypobaric hypoxia on cerebral autoregulation. Stroke 41, 641–646. https://doi.org/10.1161/STROKEAHA.109.574749 (2010).
Tymko, M. M. et al. UBC-Nepal expedition: Dynamic cerebral autoregulation is attenuated in lowlanders upon ascent to 5050 m. Eur. J. Appl. Physiol. 120, 675–686. https://doi.org/10.1007/s00421-020-04307-7 (2020).
Ogoh, S., Nakahara, H., Ainslie, P. N. & Miyamoto, T. The effect of oxygen on dynamic cerebral autoregulation: critical role of hypocapnia. J. Appl. Physiol. 108, 538–543. https://doi.org/10.1152/japplphysiol.01235.2009 (2010).
Willie, C. K. et al. Regional cerebral blood flow in humans at high altitude: Gradual ascent and 2 wk at 5,050 m. J. Appl. Physiol. 1985(116), 905–910. https://doi.org/10.1152/japplphysiol.00594.2013 (2014).
Zhang, P., Shi, X. & Downey, H. F. Two-week normobaric intermittent-hypoxic exposures stabilize cerebral perfusion during hypocapnia and hypercapnia. Exp. Biol. Med. 240, 961–968. https://doi.org/10.1177/1535370214562339 (2014).
Smirl, J. D. et al. Cerebral pressure-flow relationship in lowlanders and natives at high altitude. J. Cereb. Blood Flow Metab. 34, 248–257. https://doi.org/10.1038/jcbfm.2013.178 (2014).
Mikhail Kellawan, J., Harrell, J. W., Roldan-Alzate, A., Wieben, O. & Schrage, W. G. Regional hypoxic cerebral vasodilation facilitated by diameter changes primarily in anterior versus posterior circulation. J. Cereb. Blood Flow Metab. 37, 2025–2034. https://doi.org/10.1177/0271678x16659497 (2017).
Coverdale, N. S., Gati, J. S., Opalevych, O., Perrotta, A. & Shoemaker, J. K. Cerebral blood flow velocity underestimates cerebral blood flow during modest hypercapnia and hypocapnia. J. Appl. Physiol. 117, 1090–1096. https://doi.org/10.1152/japplphysiol.00285.2014 (2014).
Wilson, M. H. et al. Cerebral artery dilatation maintains cerebral oxygenation at extreme altitude and in acute hypoxia—An ultrasound and MRI study. J. Cereb. Blood Flow Metab. 31, 2019–2029. https://doi.org/10.1038/jcbfm.2011.81 (2011).
Acknowledgements
The ALMA observatory supported this project by providing access to their infrastructures, transportation and lodging of all investigators and participants. Philips Respironics and Siemens Healthcare AG provided some equipment of the study.
Funding
Study was funded by an NSERC Discovery Grant (PI = MJP; RGPIN-2014-05554). MJP holds the Brenda Strafford Foundation Chair in Alzheimer Research in the Cumming School of Medicine at the University of Calgary.
Author information
Authors and Affiliations
Contributions
M.F. is the guarantor of the manuscript. Concept and design: S.E.H., M.J.P., K.E.B. and M.F. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: L.C.G., M.J.P. and M.F. Critical revision of the manuscript: All authors. Statistical analysis: L.C.G., K.E.B., M.F. Obtained funding: M.J.P., K.E.B. Supervision: K.E.B., M.J.P. and M.F.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Graf, L.C., Hartmann, S.E., Lichtblau, M. et al. A prospective cohort study about the effect of repeated living high and working higher on cerebral autoregulation in unacclimatized lowlanders. Sci Rep 12, 2472 (2022). https://doi.org/10.1038/s41598-022-06270-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06270-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.