Abstract
Reduced heart rate variability (HRV) is reflective of autonomic imbalance. However, its impact on non-alcoholic fatty liver disease (NAFLD) is unknown. We investigated the association between 10-s HRV and incident NAFLD. A cohort of 154,286 Korean adults with no NAFLD at baseline were followed up. 10-s electrocardiograms were used to estimate two time-domain HRV, the standard deviation of normal-to-normal intervals (SDNN) and the root mean square of successive differences in RR intervals (RMSSD). Hepatic steatosis (HS) and liver fibrosis were assessed using ultrasonography and the fibrosis-4 index (FIB-4). A total of 27,279 incident HS (median follow up of 4.2 years) and 1250 incident HS plus high FIB-4 (median follow up of 4.2 years) cases were identified at follow-up. The multivariable adjusted hazard ratios (aHRs) (95% confidence intervals [CIs]) in a model with time-dependent variables for incident HS, comparing the lowest quintile to the highest and reference quintile of the RMSSD, was 1.43 (1.37–1.49), and the corresponding HR for incident HS plus intermediate/high FIB-4 was 1.70 (1.35–2.15). Similarly, SDNN was inversely associated with incident HS and HS plus intermediate/high FIB-4. The results were similar using the NAFLD fibrosis score. Autonomic imbalance assessed by HRV may help to identify individuals at a high risk of HS and its progression and warrant further studies.
Similar content being viewed by others
Introduction
Heart rate variability (HRV), defined by the variation in consecutive beat-to-beat intervals, reflects the constant interaction between the sympathetic and parasympathetic nervous systems and is widely used as a noninvasive tool for evaluating autonomic nervous system (ANS) imbalance1,2. A body of evidence suggests that reduced HRV is associated with cardiometabolic risk factors (obesity, hypertension, and diabetes), cardiovascular morbidity and mortality, and all-cause mortality3,4,5. Although 5‐min electrocardiographic (ECG) recordings are the standard measures for evaluating HRV1, recent studies have reported that HRV time-domain parameters derived from 10-s ECG recordings6,7,8,9 are also reliable measures for assessing HRV. Since the 10-s ECG is one of the most widely measured tests in clinical practice, the 10-s ECG-derived HRV can be used to evaluate the relationship between autonomic imbalance and health in large population-based studies.
Non-alcoholic fatty liver disease (NAFLD) is a leading cause of chronic liver disease worldwide, with an estimated global prevalence of approximately 25%10,11. NAFLD is associated with increased risks of mortality related to cardiometabolic disease, as well as increased liver-related morbidity and mortality12. As there are currently no licensed drugs available for the treatment of NAFLD, it is of considerable importance to identify modifiable risk factors and manage them to prevent this disease10,11,12.
The pathogenesis of NAFLD is not fully understood, although insulin resistance is implicated in both the development and progression of NAFLD13. The liver is innervated by both the sympathetic and parasympathetic nervous systems, both of which play an important role in the autonomic regulation of glucose and lipid metabolism14,15. Interestingly, several experimental studies have demonstrated that increased sympathetic nervous activity could induce NAFLD and influence its progression, even non-alcoholic steatohepatitis (NASH)-cirrhosis, whereas parasympathetic activation reduces progression16, suggesting its potential role in the autonomic imbalance in the pathogenesis of NAFLD. To date, no cohort studies have addressed whether low HRV, reflective of autonomic imbalance, is associated with the risk and progression of NAFLD.
Therefore, this study aimed to investigate the prospective association between HRV, based on 10-s ECG recordings, and the development of hepatic steatosis (HS) both with and without an intermediate/high probability of advanced fibrosis.
Results
Baseline characteristics
At baseline, the mean (SD) of SDNN and RMSSD were 36.8 ms (25.3) and 44.6 ms (37.7), respectively. Of the 154,286 participants with 611,478 person-years of follow-up (median follow-up of 4.2 years, interquartile range of 2.3–6.0 years), 27,279 cases of incident HS were identified (incidence rate 44.6 per 103 person-years). The median frequency of visits was 3 (interquartile range, 2–5) and median interval between the baseline and 2nd visit was 1.8 years (interquartile range, 1.1–2.1). Incident HS was positively associated with age, male sex, obesity, current smoking, alcohol intake, hypertension, diabetes, medication for hyperlipidemia, unfavorable lipid profiles, and levels of liver enzymes, hsCRP, and HOMA-IR (Table 1).
Incident hepatic steatosis by heart rate variability
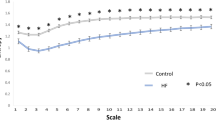
Both SDNN and RMSSD were inversely associated with the risk of incident HS. After adjustment for confounders, multivariable-adjusted HRs (95% CIs) for incident HS, comparing the first, second, third, and fourth quintiles with the highest quintile of the RMSSD, were only attenuated slightly: 1.31 (1.26–1.38), 1.20 (1.15–1.25), 1.13 (1.08–1.17), and 1.05 (1.01–1.10), respectively (P for trend < 0.001). In a model with time-dependent variables, HRs (95% CIs) for incident HS, comparing the first, second, third, and fourth quintiles with the highest quintile of the RMSSD were 1.43 (1.37–1.49), 1.25 (1.19–1.30), 1.18 (1.13–1.23), and 1.06 (1.02–1.11), respectively (P for trend < 0.001). The HRs (95% CIs) for the four quintile with the highest quintile of SDNN (reference) in multivariable-adjusted model 2 were 1.22 (1.17–1.27), 1.14 (1.09–1.18), 1.08 (1.04–1.13), and 1.02 (0.98–1.06), respectively (P for trend < 0.001). The corresponding HRs (95% CIs) for incident HS in time-dependent analysis, comparing the first, second, third, and fourth quintiles with the highest quintile of the SDNN were 1.30 (1.25–1.36), 1.19 (1.15–1.24), 1.10 (1.05–1.14), and 1.03 (0.99–1.08), respectively (P for trend < 0.001). For time-dependent analyses, the updated status of HRV and other confounders were incorporated as time-varying covariates (Table 2).
Incident hepatic steatosis with intermediate/high FIB-4 by heart rate variability
During a median follow-up of 4.2 years (interquartile range 2.3–6.0), 1250 cases of incident HS plus intermediate/high FIB-4, and 2834 cases of incident HS plus intermediate/high NFS were identified (incidence rate of 2.9 per 103 person-years and 2.7 per 103 person-years, respectively). Both SDNN and RMSSD were also significantly and inversely associated with the risk of incident HS plus intermediate/high FIB-4. Specifically, the multivariable-adjusted HR (95% CIs) in a model with time-dependent variables for incident HS plus intermediate/high FIB-4, comparing the first, second, third, and fourth quintile with the highest quintile of the RMSSD (reference), were 1.70 (1.35–2.15), 1.47 (1.16–1.88), 1.36 (1.06–1.75), and 1.30 (1.00–1.70), respectively. The lowest quintile of both SDNN and RMSSD also was significantly associated with an increased risk of incident HS plus intermediate/high NFS (Table 3).
Sensitivity and mediation analysis
In a sensitivity analysis based on NFS, low values of both SDNN and RMSSD were significantly associated with an increased risk of incident HS plus intermediate/high NFS in fixed and time-dependent models. After further adjustment for BMI or HOMA-IR, the association between RMSSD and incident HS plus intermediate/high FIB-4 was attenuated and no longer significant; after adjustment for hsCRP, the association was attenuated but remained significant. For analyses based on NFS instead of FIB-4, the BMI was not adjusted because it is a component of the NFS score. Further adjustment for HOMA-IR or hsCRP attenuated the association between HRV and HS plus intermediate/high NFS, but the associations remained statistically significant (Supplementary Table 1). All these associations between low HRV measured by both SDNN and RMSSD and a increased risk of HS or HS plus intermediate/high fibrosis markers based on FIB-4 were similarly observed in sub-groups of non-obese individuals (Supplementary Table 2).
When NAFLD was used as endpoint which restricted to only HS without secondary causes (use of steatogenic medication, significant alcohol consumption, and B or C viral seropositivity) throughout the follow-up period was used as an endpoint, the associations between low HRV, SDNN, RMSSD, and incident NAFLD were similarly observed (Supplementary Table 3). Similarly, low RMSSD was inversely and significantly associated with incident NAFLD with an intermediate-to-high probability of advanced fibrosis, while low SDNN tended to show an elevated risk of incident NAFLD with an intermediate/high FIB-4 score; however, this association was not significant in the multivariable-adjusted model (P for trend = 0.087) (Supplementary Table 4).
We additionally performed a sensitivity analysis using Hepatic Steatosis Index (HSI) of > 36 as an endpoint which has been validated for detection of HS in a Korean population17. In the sensitivity analysis using HSI > 36 as an endpoint, a low SDNN and a RMSSD were independently associated with an increased incidence of suspected HS (Supplementary Table 5).
Additionally, the associations between potential confounders with HRV and HS are presented in Supplementary Tables 6–8.
Discussion
In this large-scale cohort study of apparently healthy adults, low HRV, measured by the SDNN and RMSSD, which reflect global autonomic regulation and parasympathetic activity of the heart, respectively, were associated with increased risk of both incident HS and HS plus intermediate/high fibrosis markers based on FIB-4 or NFS. This association was similarly observed when changes in HRV and confounders during follow-up were treated as time-varying covariates and was independent of a wide range of potential confounders, including sleep duration and depressive symptoms, which influence HRV18,19. Similar findings were observed in analyses among non-obese individuals to address potential residual confounding by obesity, all of which are strong risk factors for NAFLD and its progression20,21. Our findings indicate that ANS function estimated by HRV may play an independent role in NAFLD risk and severity.
To the best of our knowledge, no previous cohort study has investigated the prospective association between HRV and NAFLD development. Our novel findings support and extend the results of previous cross-sectional studies22,23,24,25. One previous cross-sectional study of 497 subjects by Liu et al. (with a measure of 5 min HRV) showed a significant association between autonomic alteration (decreased SDNN and RMSSD) and increased prevalence of NAFLD, which was independent of traditional CVD risk factors, and HOMA-IR25. Another cross-sectional study of 96 sedentary individuals by Houghton et al. found that increased levels of fat in the liver were significantly associated with impaired cardiac and autonomic function, including detailed HRV parameters, when compared with individuals without fatty liver23. However, previous studies were limited by temporal ambiguity due to the cross-sectional study designs, relatively small sample sizes22,23,24,25, and the lack of adjustment for important confounders, including comorbidities23,24.
In our cohort study of 160,150 adults with no evidence of NAFLD at baseline, low HRV, measured by both SDNN and RMSSD, was significantly and consistently associated with an increased risk of developing both HS and HS plus intermediate/high fibrosis based on either FIB-4 or NFS. On the other hand, whereas low HRV measured by both SDNN and RMSSD was significantly associated with incident NAFLD and NAFLD plus intermediate/high NFS, only low HRV measured by both RMSSD was significantly associated with incident NAFLD plus intermediate/high FIB-4 in multivariable proportional hazard model. There are several possible explanations for this observation. First, SDNN reflects the overall dysfunction of the ANS, while the RMSSD is more influenced by PNS than SDNN, and is reflective of PNS activity. PNS alteration might precede SNS alteration26,27, and the RMSSD is considered a sensitive and reliable marker for parasympathetic activity1,2. Second, previous validation studies suggest that even a single 10-s (standard ECG) recording yields valid RMSSD measurements, while reliable measures for SDNN require a longer duration of at least 30 s or multiple 10-s ECGs6,8,9. Thus, in our study, HRV estimation based on a single 10-s ECG recording might explain the consistent finding based on the RMSSD; the RMSDD may be a more reliable HRV measure than SDNN in the setting using a single 10-s ECG recording, but also reflects the relative importance of PNS activity in NAFLD risk and its progression.
The mechanisms underlying the association between HRV and NAFLD are not yet fully understood, but there is growing evidence to suggest that autonomic dysfunction affects the risk of NAFLD and disease progression. Preclinical studies have demonstrated that an increase in SNS activity and adrenergic signaling causes HS and NASH-cirrhosis, while an increase in PNS activity inhibits the process from HS to NASH-cirrhosis16. Moreover, selective hepatic sympathetic denervation in mice led to almost complete resolution of HS in 1 week28, while hepatic vagotomy was found to exacerbate HS and hepatic inflammation in a mouse model16,29. In a human study of 34 individuals with biopsy-proven NAFLD and 34 matched controls, objective measures of ANS dysfunction based on 24-h BP and head tilt testing were prevalent in the group with NAFLD30. Furthermore, ANS dysfunction may also influence insulin resistance and inflammation, both of which are involved in the key pathogenesis of NAFLD31,32,33. Several studies have found that lowered HRV is associated with increased levels of inflammatory markers and HOMA‐IR31,32,33. Furthermore, an altered balance of the PNS and SNS activity, mainly explained by attenuated PNS activity, might contribute to the development of insulin resistance34. Additionally, sympathetic over activity might have an important role in metabolic alterations including central obesity and insulin resistance35. Intriguingly, HRV appears to improve with weight loss or adoption of a healthy lifestyle, including regular exercise, diet choice, and adequate sleep18,19. As the balance of ANS is a modifiable risk factor18,19,36, improving ANS function might help to reduce the development of NAFLD and its progression.
ANS dysfunction has been reported to increase the risk of obesity, and, at the same time, obesity may also influence autonomic imbalance, indicating that the two conditions affect each other37. Given that obesity is a strong risk factor for NAFLD21, we evaluated whether obesity and obesity-associated derangements, including insulin resistance and chronic inflammation, mediate the association between HRV and incident NAFLD by further adjusting for BMI, HOMA-IR, and hsCRP. The association between low HRV measured by SDNN and RMSSD and incident HS was attenuated but remained statistically significant, and the association with incident HS plus intermediate/high FIB-4 was more attenuated; however, longer follow-up studies may be required to validate this finding. Another possible explanation is that ANS dysfunction might be involved in the early stage of NAFLD, independent of obesity and its related metabolic abnormalities, whereas fibrosis progression appears to be more complex and mediated by obesity and its consequences related to ANS dysfunction.
This study has several limitations that should be discussed. First, because we used HRV based on 10-s ECG, more detailed information on high frequency, low frequency, or their ratio, all of which are also known to reflect the balance between sympathetic and parasympathetic activity, were unavailable. Second, HS and liver fibrosis were determined by liver ultrasonography and noninvasive fibrosis scores in the absence of liver biopsy. FIB-4 and NFS are the most commonly used and validated indices for excluding or identifying advanced liver fibrosis38. However, these indices can reliably exclude advanced fibrosis and not all cases classified as having an intermediate-to-high probability of advanced fibrosis may have advanced fibrosis39; thus, future studies using more sophisticated measures are required to assess the association between HRV and severe NAFLD. Lastly, the majority of participants in this cohort were relatively young, healthy, and well-educated Korean workers and their spouses, possibly limiting the generalizability of our findings to other populations and different age groups.
In conclusion, low HRV measured by 10-s ECG was associated with an increased risk of incident HS and HS plus intermediate/high fibrosis markers, independent of other existing risk factors. This finding supports that ANS dysfunction, especially decreased RMSSD, which is reflective of decreased parasympathetic activity, is involved in the pathophysiology of HS and its progression to fibrosis. Further studies are needed to clarify the exact role of ANS dysfunction in the pathogenesis of NAFLD and its progression, and to confirm whether approaches that improve HRV can help prevent NAFLD and its consequences.
Methods
Study population
This cohort study is part of the Kangbuk Samsung Health Study including Korean adults who underwent a comprehensive health screening examination at the Kangbuk Samsung Hospital Total Healthcare Centres located in Seoul and Suwon, South Korea40. To investigate the association between HRV and incident HS with/without intermediate/high fibrosis score, study participants were restricted to those who received a health examination from 2011 (the year from which 10-s ECG recordings were available) to 2017 and had at least one follow-up visit by December 31, 2019 (n = 307,456). A total of 153,170 participants were excluded based on the criteria listed in Fig. 1. The final analytic sample included 154,286 participants. All procedures involved in this study were in accordance with the 1964 Helsinki declaration and approved by the Institutional Review Board of Kangbuk Samsung Hospital (IRB 2021-01-033), which waived the requirement for informed consent since we performed analysis using a de-identified dataset that was routinely collected during the health screening process.
Data collection
Health screening examinations included liver ultrasound, ECG, and blood laboratory and anthropometric measurements at both baseline and follow-up visits. A standardized, self-administered questionnaire was used to collect information on demographic characteristics, medical history, depressive symptoms and lifestyle behaviors (see further details in the supporting information).
Abdominal ultrasound was performed by experienced radiologists who diagnosed HS based on standard criteria, including the presence of a diffuse increase in fine echoes in the liver parenchyma compared with the kidney or spleen parenchyma, deep beam attenuation, and bright vessel walls41. The inter-observer and intra-observer reliability values for HS diagnoses were substantial (kappa statistic = 0.74) and excellent (kappa statistic = 0.94), respectively40.
The severity of NAFLD was assessed based on two noninvasive indices of liver fibrosis: the Fibrosis 4 score (FIB-4) and the NAFLD fibrosis score (NFS), which are adopted and recommended by most guidelines38,42. Subjects were classified as having low, intermediate, or high risk for advanced liver fibrosis for each score based on the following cutoff: FIB-4 (< 1.30, 1.30–2.66, and ≥ 2.67, respectively)38 and NFS (< − 1.455, − 1.455 to 0.676, and > 0.676, respectively)42. As the number of incidents with high probability of advanced fibrosis was not sufficient to examine a separate category, the combined outcome of intermediate or high fibrosis score was used as an endpoint.
Standard 12-lead, 10-s ECGs were performed as a routine part of the health screening process in all subjects on the same day as the other examinations were performed. The two time-domain HRV parameters, the standard deviation of normal-to-normal RR intervals (SDNN), and the root mean square of successive differences (RMSSD) were calculated based on the 10-s ECG recordings. The SDNN is affected by both sympathetic and parasympathetic nervous system (PNS) activity, while the RMSSD is the primary time-domain known to be more influenced by the PNS than the SDNN2. Low values of either SDNN or RMSSD are correlated with an increased risk of both cardiovascular morbidity and mortality2,3,4,5.
Physical activity levels were determined using the validated Korean version of the international Physical Activity Questionnaire (IPAQ) Short Form43,44. Health-enhancing physical activity (HEPA) was defined as physical activity that meets one of two following criteria: (1) vigorous activity on three or more days per week with ≥ 1500 of accumulated metabolic equivalent (MET)-min/week (1 MET is energy expenditure at rest); or (2) 7 days of any combination of walking, moderate intensity, or vigorous intensity activities achieving at least 3000 MET min/week44.
The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality and sleep duration over the month prior to study initiation45. Sleep duration was categorized as ≤ 5, 6, 7, 8, and ≥ 9 h. Depressive symptoms were assessed using the Korean version of the Centre for Epidemiologic Studies Depression (CES-D) Scale, and were categorized as CES-D scores < 16 and ≥ 1646,47.
The sitting blood pressure (BP) and anthropometric parameters were measured by trained nurses. Obesity was defined as a body mass index (BMI) ≥ 25 kg/m2, the proposed cutoff for obesity diagnosis in Asians48. Hypertension was defined as a systolic BP ≥ 140 mmHg, diastolic BP ≥ 90 mmHg, or current use of antihypertensive medication.
Blood specimens were obtained after at least 10 h of fasting. Blood measurements included lipid profiles, liver enzymes, glucose, hemoglobin A1c, insulin, high-sensitivity C-reactive protein (hsCRP), and platelet count. The homeostatic model assessment of insulin resistance (HOMA-IR) index was calculated as follows: fasting blood insulin (mU/mL) × fasting blood glucose (mmol/L)/22.5. Diabetes mellitus was defined as a fasting serum glucose level ≥ 126 mg/dL, hemoglobin A1c ≥ 6.5%, or current use of medication for the treatment of diabetes.
Assessment of electrocardiogram
ECG was performed as a routine part of the health screening process in all subjects on the same day as the other examinations were performed. All ECGs were performed in a silent and relaxing private space in the absence of external stimuli, but the testing order was not specified. Thus, in some participants, the ECG was conducted after blood sampling, which may not have occurred due to exposure or outcome status; thus, this type of non-differential measurement error would have underestimated the true association between HRV and outcomes. Standard 12-lead ECGs were obtained at a paper speed of 25 mm/s and an amplification of 1 mV/cm with an ECG recorder (CARDIMAX FX-7542; Fukuda Denishi Co., Ltd., Tokyo, Japan). All ECGs were initially inspected for technical errors and quality by trained ECG technicians and then interpreted by three experienced cardiologists who were blinded to the aim of this study. All ECG data were digitalized and analyzed using an automated ECG analysis system (PI-19E; Fukuda Denishi Co., Ltd., Tokyo, Japan), which automatically detects the QRS complex and calculates the RR intervals.
Statistical analysis
The baseline characteristics of the study participants are presented as percentages, means (standard deviations), and medians (interquartile ranges) according to incident HS. The SDNN and RMSSD were categorized into quintiles based on their own distributions because there is no clear established cutoff value of either measurement to define autonomic dysfunction. The highest quintile was set to the reference group given that low HRV is known to be associated with cardiometabolic disease2,3,4,5. The primary endpoints were: (a) development of incident HS (regardless of fibrosis score), and (b) the development of incident HS plus intermediate/high probability of liver fibrosis at follow-up. Incident HS and incident HS plus an intermediate or high probability of liver advanced fibrosis based on FIB-4 or NFS were treated as separate endpoints in each model.
The risk of incident HS and incident HS plus an intermediate/high probability of liver fibrosis were separately evaluated according to each HRV index. The hazard ratios (HRs) and 95% CIs were calculated using the parametric proportional hazards model. The models were initially adjusted for age and sex, and were then further adjusted for study centre (Seoul, Suwon), year of screening exam, smoking (never, past, current, or unknown), alcohol intake (none, < 10 or ≥ 10 g/day, or unknown), physical activity (inactive, minimally active, health-enhancing physical activity, or unknown), CES-D (< 16, ≥ 16, or unknown), sleep duration (≤ 5, 6, 7, 8, ≥ 9 h, or unknown), education level (< community college graduate, ≥ community college graduate, or unknown), total energy intake (quintiles or unknown), and systolic BP. Furthermore, to evaluate the impact of changes in HRV and covariates over follow-up, we conducted additional analyses by introducing HRV and other covariates as time-varying covariates in the models. To explore whether BMI, HOMA-IR, or hsCRP mediates the association between HRV and the primary endpoints, we included these variables in a multivariable-adjusted model (see further details in the supporting information). We assessed the proportional hazards assumption by examining graphs of estimated log (− log(survival)) versus the log of the survival time graph; no violation of the assumption was found.
The event detection date was defined as the earliest date of HS or HS identification with an intermediate or high probability of liver fibrosis. The person-years were calculated as the sum of the follow-up duration from baseline to the event detection date, or until the final examination (before December 31, 2019), whichever came first. The incidence rates were calculated as the number of incident cases divided by the person-years of follow-up. Because the primary endpoints would have occurred at an unknown time point between the event detection date and the previous screening visit, a parametric proportional hazards model was used to account for this type of interval censoring. In these models, the baseline hazard function was parameterized with natural cubic splines of log time with 3 internal knots at the 25th, 50th, and 75th percentiles (Stata package stpm)49.
To explore whether BMI, HOMA-IR, or hsCRP mediates the association between HRV and the primary endpoints, we included these variables in a multivariable-adjusted model. The following criteria for potential mediators were used: (1) The predictor of interest (HRV) was significantly related to the mediator (BMI, HOMA-IR, or hsCRP); (2) the mediator (BMI, HOMA-IR, or hsCRP) was significantly related to the outcome (HS or HS plus fibrosis); and (3) the addition of the mediator (BMI, HOMA-IR, or hsCRP) to the model both attenuated the coefficient of the predictor and had a statistically significant mediation effect.
We then evaluated whether or not the associations between HRV and the risk of HS and incident HS combined with an intermediate/high probability of liver fibrosis existed in individuals without obesity. The interactions between subgroup characteristics and HRV categories on the risk of HS and the intermediate/high probability of advanced liver fibrosis were tested using likelihood ratio tests, which compare models with and without multiplicative interaction terms. Statistical analyses were performed using STATA version 16.0 (StataCorp LP, College Station, TX, USA). All reported P-values were two-tailed, and differences were considered statistically significant at P < 0.05.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Kangbuk Samsung Hospital (IRB 2021-01-033), which waived the requirement for informed consent since we performed analysis using a de-identified dataset that was routinely collected during the health screening process.
Consent for publication
The authors agree to the publication of this study.
Data availability
Data are available from the Kangbuk Samsung Health Study whose authors may be contacted through the corresponding author. Unfortunately, the data are not available to be shared publicly as we do not have IRB permission for distributing the data.
Change history
09 December 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41598-022-25977-7
Abbreviations
- ALT:
-
Alanine aminotransferase
- ANS:
-
Autonomic nervous system
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CES-D:
-
Centre for Epidemiologic Studies Depression
- CI:
-
Confidence interval
- hs-CRP:
-
High-sensitivity C-reactive protein
- CVD:
-
Cardiovascular disease
- ECG:
-
Electrocardiography
- GGT:
-
Gamma-glutamyl transferase
- HDL-C:
-
High-density lipoprotein cholesterol
- FIB-4:
-
Fibrosis-4 scores
- HEPA:
-
Health-enhancing physical activity
- HOMA-IR:
-
Homeostatic model assessment–insulin resistance
- HR:
-
Hazard ratio
- HRV:
-
Heart rate variability
- HS:
-
Hepatic steatosis
- HSI:
-
Hepatic Steatosis Index
- LDL-C:
-
Low-density lipoprotein cholesterol
- NAFLD:
-
Non-alcoholic fatty liver disease
- NFS:
-
NAFLD fibrosis score
- PNS:
-
Parasympathetic nervous system
- PSQI:
-
Pittsburgh Sleep Quality Index
- RMSSD:
-
Root mean square of successive differences in RR intervals
- SDNN:
-
Standard deviation of normal-to-normal intervals
- SNS:
-
Sympathetic nervous system
References
Malik, M. et al. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Eur. Heart J. 17, 354–381. https://doi.org/10.1093/oxfordjournals.eurheartj.a014868 (1996).
Shaffer, F. & Ginsberg, J. P. An overview of heart rate variability metrics and norms. Front. Public Health 5, 258. https://doi.org/10.3389/fpubh.2017.00258 (2017).
Hillebrand, S. et al. Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: Meta-analysis and dose-response meta-regression. Europace 15, 742–749. https://doi.org/10.1093/europace/eus341 (2013).
Fang, S. C., Wu, Y. L. & Tsai, P. S. Heart rate variability and risk of all-cause death and cardiovascular events in patients with cardiovascular disease: A meta-analysis of cohort studies. Biol. Res. Nurs. 22, 45–56. https://doi.org/10.1177/1099800419877442 (2020).
Thayer, J. F., Yamamoto, S. S. & Brosschot, J. F. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int. J. Cardiol. 141, 122–131. https://doi.org/10.1016/j.ijcard.2009.09.543 (2010).
Nussinovitch, U. et al. Reliability of ultra-short ECG indices for heart rate variability. Ann. Noninvasive Electrocardiol. 16, 117–122. https://doi.org/10.1111/j.1542-474X.2011.00417.x (2011).
Takahashi, N., Kuriyama, A., Kanazawa, H., Takahashi, Y. & Nakayama, T. Validity of spectral analysis based on heart rate variability from 1-minute or less ECG recordings. Pacing Clin. Electrophysiol. 40, 1004–1009. https://doi.org/10.1111/pace.13138 (2017).
Munoz, M. L. et al. Validity of (ultra-)short recordings for heart rate variability measurements. PLoS One 10, e0138921. https://doi.org/10.1371/journal.pone.0138921 (2015).
Hamilton, R. M., McKechnie, P. S. & Macfarlane, P. W. Can cardiac vagal tone be estimated from the 10-second ECG?. Int. J. Cardiol. 95, 109–115. https://doi.org/10.1016/j.ijcard.2003.07.005 (2004).
Byrne, C. D. & Targher, G. NAFLD: A multisystem disease. J. Hepatol. 62, S47–S64. https://doi.org/10.1016/j.jhep.2014.12.012 (2015).
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease. Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64, 73–84. https://doi.org/10.1002/hep.28431 (2016).
Younossi, Z. et al. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 15, 11–20. https://doi.org/10.1038/nrgastro.2017.109 (2018).
Stefan, N., Häring, H. U. & Cusi, K. Non-alcoholic fatty liver disease: Causes, diagnosis, cardiometabolic consequences, and treatment strategies. Lancet Diabetes Endocrinol. 7, 313–324. https://doi.org/10.1016/s2213-8587(18)30154-2 (2019).
Mizuno, K. & Ueno, Y. Autonomic nervous system and the liver. Hepatol. Res. 47, 160–165. https://doi.org/10.1111/hepr.12760 (2017).
Nonogaki, K. New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia 43, 533–549. https://doi.org/10.1007/s001250051341 (2000).
Amir, M., Yu, M., He, P. & Srinivasan, S. Hepatic autonomic nervous system and neurotrophic factors regulate the pathogenesis and progression of non-alcoholic fatty liver disease. Front. Med. (Lausanne) 7, 62. https://doi.org/10.3389/fmed.2020.00062 (2020).
Lee, J.-H. et al. Hepatic steatosis index: A simple screening tool reflecting nonalcoholic fatty liver disease. Dig. Liver Dis. 42, 503–508 (2010).
Young, H. A. & Benton, D. Heart-rate variability: a biomarker to study the influence of nutrition on physiological and psychological health? Behav. Pharmacol. 29, 140 (2018).
Lehrer, P. et al. Heart rate variability biofeedback improves emotional and physical health and performance: a systematic review and meta analysis. Appl. Psychophysiol. Biofeedback 45, 109–129 (2020).
Tilg, H., Moschen, A. R. & Roden, M. NAFLD and diabetes mellitus. Nat. Rev. Gastroenterol. Hepatol. 14, 32–42 (2017).
Li, L. et al. Obesity is an independent risk factor for non‐alcoholic fatty liver disease: evidence from a metaanalysis of 21 cohort studies. Obes. Rev. 17, 510–519 (2016).
Liu, Y.-C. et al. Influence of Non-Alcoholic Fatty Liver Disease on Autonomic Changes Evaluated by the Time Domain, Frequency Domain, and Symbolic Dynamics of Heart Rate Variability. PLoS One 8, e61803. https://doi.org/10.1371/journal.pone.0061803 (2013).
Kumar, M. S. et al. Cardiovascular autonomic dysfunction in patients of nonalcoholic fatty liver disease. Int. J. Hepatol. 2016 (2016).
Selvamari, K. Evaluation of Autonomic Functions and Serum Leptin Levels in Postmenopausal Women with Non Alcoholic Fatty Liver, Madras Medical College, Chennai, (2017).
Houghton, D. et al. The degree of hepatic steatosis associates with impaired cardiac and autonomic function. J. Hepatol. 70, 1203–1213. https://doi.org/10.1016/j.jhep.2019.01.035 (2019).
Ewing, D., Campbell, I. & Clarke, B. Heart rate changes in diabetes mellitus. The Lancet 317, 183–186 (1981).
Freccero, C., Svensson, H., Bornmyr, S., Wollmer, P. & Sundkvist, G. Sympathetic and parasympathetic neuropathy are frequent in both type 1 and type 2 diabetic patients. Diabetes Care 27, 2936–2941 (2004).
Hurr, C., Simonyan, H., Morgan, D. A., Rahmouni, K. & Young, C. N. Liver sympathetic denervation reverses obesity-induced hepatic steatosis. J. Physiol. 597, 4565-4580. https://doi.org/10.1113/JP277994 (2019).
Nishio, T. et al. Hepatic vagus nerve regulates Kupffer cell activation via α7 nicotinic acetylcholine receptor in nonalcoholic steatohepatitis. J. Gastroenterol. 52, 965–976 (2017).
Newton, J. L., Pairman, J., Wilton, K., Jones, D. E. & Day, C. Fatigue and autonomic dysfunction in nonalcoholic fatty liver disease. Clin. Auton. Res. 19, 319–326 (2009).
Saito, I. et al. Heart rate variability, insulin resistance, and insulin sensitivity in Japanese adults: The Toon Health Study. J. Epidemiol., JE20140254 (2015).
Williams, D. P. et al. Heart rate variability and inflammation: a meta-analysis of human studies. Brain. Behav. Immun. 80, 219–226 (2019).
Sajadieh, A. et al. Increased heart rate and reduced heart-rate variability are associated with subclinical inflammation in middle-aged and elderly subjects with no apparent heart disease. Eur. Heart J. 25, 363–370. https://doi.org/10.1016/j.ehj.2003.12.003 (2004).
Lindmark, S., Wiklund, U., Bjerle, P. & Eriksson, J. W. Does the autonomic nervous system play a role in the development of insulin resistance? A study on heart rate variability in first-degree relatives of Type 2 diabetes patients and control subjects. Diabet. Med. 20, 399–405. https://doi.org/10.1046/j.1464-5491.2003.00920.x (2003).
Schlaich, M., Straznicky, N., Lambert, E. & Lambert, G. Metabolic syndrome: a sympathetic disease? Lancet Diabetes Endocrinol. 3, 148-157 (2015).
Routledge, F. S., Campbell, T. S., McFetridge-Durdle, J. A. & Bacon, S. L. Improvements in heart rate variability with exercise therapy. Can. J. Cardiol. 26, 303–312 (2010).
Guarino, D., Nannipieri, M., Iervasi, G., Taddei, S. & Bruno, R. M. The role of the autonomic nervous system in the pathophysiology of obesity. Front. Physiol. 8, 665 (2017).
Shah, A. G. et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 7, 1104–1112. https://doi.org/10.1016/j.cgh.2009.05.033 (2009).
Kaya, E. et al. Simple noninvasive scores are clinically useful to exclude, not predict, advanced fibrosis: A study in Turkish patients with biopsy-proven nonalcoholic fatty liver disease. Gut Liver 14, 486 (2020).
Chang, Y. et al. Alcoholic and non-alcoholic fatty liver disease and associations with coronary artery calcification: Evidence from the Kangbuk Samsung Health Study. Gut 68, 1667–1675. https://doi.org/10.1136/gutjnl-2018-317666 (2019).
Mathiesen, U. L. et al. Increased liver echogenicity at ultrasound examination reflects degree of steatosis but not of fibrosis in asymptomatic patients with mild/moderate abnormalities of liver transaminases. Dig. Liver Dis. 34, 516–522 (2002).
Angulo, P. et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 45, 846–854. https://doi.org/10.1002/hep.21496 (2007).
Chun, M. Y. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean J. Fam. Med. 33, 144–151. https://doi.org/10.4082/kjfm.2012.33.3.144 (2012).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453.FB (2003).
Buysse, D. J., Reynolds, C. F. 3rd., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. https://doi.org/10.1016/0165-1781(89)90047-4 (1989).
Cho, M. J. & Kim, K. H. Diagnostic validity of the CES-D (Korean version) in the assessment of DSM-III R major depression. J. Korean Neuropsychiatr. Assoc. 32, 381–399 (1993).
Radloff, L. S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385–401 (1977).
World Health Organization and Regional Office for the Western Pacific. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment (Health Communications Australia, 2000).
Royston, P. & Parmar, M. K. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat. Med. 21, 2175–2197. https://doi.org/10.1002/sim.1203 (2002).
Funding
This study was supported by SKKU Excellence in Research Award Research Fund, Sungkyunkwan University, 2020 and by the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (NRF-2017R1A2B2008401). CDB is supported in part by the Southampton NIHR Biomedical Research Centre (IS-BRC-20004), UK. This research was also supported by CDM-based precision medical data integration platform technology development program through the Korea Evaluation Institute of Industrial Technology funded by the Ministry of Trade, Industrial and Energy (No. 20005037).
Author information
Authors and Affiliations
Contributions
I.Y.C.: drafting of the manuscript and critical revision of the manuscript. Y.C.: study concept and design; acquisition of data; interpretation of data; drafting of the manuscript and critical revision of the manuscript. G.K.: acquisition of data; interpretation of data; and critical revision of the manuscript. H.S.J.: acquisition of data; interpretation of data; and critical revision of the manuscript. H.S.: technical, or material support; and study supervision. S.H.W.: interpretation of data; and critical revision of the manuscript. C.D.B.: interpretation of data; and critical revision of the manuscript. S.R.: study concept and design; acquisition of data; analysis and interpretation of data and critical revision of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The Funding section in the original version of this Article was incomplete. It now reads: “This study was supported by SKKU Excellence in Research Award Research Fund, Sungkyunkwan University, 2020 and by the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (NRF-2017R1A2B2008401). CDB is supported in part by the Southampton NIHR Biomedical Research Centre (IS-BRC-20004), UK. This research was also supported by CDM-based precision medical data integration platform technology development program through the Korea Evaluation Institute of Industrial Technology funded by the Ministry of Trade, Industrial and Energy (No. 20005037)."
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, I.Y., Chang, Y., Kang, G. et al. Low heart rate variability from 10-s electrocardiograms is associated with development of non-alcoholic fatty liver disease. Sci Rep 12, 1062 (2022). https://doi.org/10.1038/s41598-022-05037-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05037-w
This article is cited by
-
Changes in heart rate variability over time from symptom onset of transient global amnesia
Scientific Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.