Abstract
Early diagnosis of acute mesenteric ischemia (AMI) remains a clinical challenge, and no biomarker has been consistently validated. We aimed to assess the accuracy of three promising circulating biomarkers for diagnosing AMI—citrulline, intestinal fatty acid-binding protein (I-FABP), and d-lactate. A cross-sectional diagnostic study enrolled AMI patients admitted to the intestinal stroke center and controls with acute abdominal pain of another origin. We included 129 patients—50 AMI and 79 controls. Plasma citrulline concentrations were significantly lower in AMI patients compared to the controls [15.3 μmol/L (12.0–26.0) vs. 23.3 μmol/L (18.3–29.8), p = 0.001]. However, the area under the receiver operating curves (AUROC) for the diagnosis of AMI by Citrulline was low: 0.68 (95% confidence interval = 0.58–0.78). No statistical difference was found in plasma I-FABP and plasma d-lactate concentrations between the AMI and control groups, with an AUROC of 0.44, and 0.40, respectively. In this large cross-sectional study, citrulline, I-FABP, and d-lactate failed to differentiate patients with AMI from patients with acute abdominal pain of another origin. Further research should focus on the discovery of new biomarkers.
Similar content being viewed by others
Introduction
Early management of acute mesenteric ischemia (AMI) can avoid fatal outcomes and prevent related short bowel syndrome1,2,3,4. To this end, there is a dire need for tools to establish an immediate diagnosis. Mortality and intestinal resection rates have remained unchanged for decades despite the progress made in radiology, endovascular procedures, and intensive care medicine. However, recent reports suggest improved outcomes for patients if diagnosis and standardized multidisciplinary expert care are provided at an early stage1,5,6,7. Indeed, early AMI is a fully reversible condition, as opposed to "advanced" AMI with irreversible transmural necrosis2,8. However, AMI patients present unspecific acute abdominal pain, which renders clinical suspicion and identification challenging and can often lead to missed or delayed diagnosis and care2,9. Moreover, AMI may be underdiagnosed on contrast-enhanced computed tomography (CT) of the acute abdomen when the suspicion is not evoked10,11,12.
While biological abnormalities—such as leucocytosis or lactic acidosis—have been documented in patients with AMI, their performance to establish the early diagnosis is poor4,13. The high complexity of the layered intestinal wall structure increases the diversity of the proteins and metabolites released in AMI. Their hepatic metabolism through the hepatic portal system results in substantial overlap with liver proteins and metabolites. These factors, along with the heterogeneity of the disease, explain why identifying clinically reliable biological early markers of AMI has been unsuccessful so far2,4,9.
Three blood biomarkers have gained attention over the past decades: citrulline, a marker of enterocyte function; I-FABP, a marker of enterocyte damage; and d-lactate, a marker of intestinal barrier dysfunction and microbial translocation4,14,15,16. As a result, these tests are increasingly used in basic and clinical research as indirect markers of an ischemic intestinal injury in a broad range of emergency clinical settings. However, to date, their alleged diagnostic performances have only been assessed in small heterogeneous cohorts. Besides, conflicting results have been reported, and most of the studies consist of preoperative data in late-stage necrotic AMI patients3. As a consequence, the accuracy of these three biomarkers in identifying early-stage AMI remains to be conclusively tested17,18.
The aim of this cross-sectional diagnostic study was to assess the accuracy of these three promising circulating biomarker candidates—citrulline, I-FABP, and d-lactate—for the diagnosis of AMI.
Methods
Study design and setting
Following the results of a pilot study showing an improvement in survival and lower resection rates1, we created an intestinal stroke center (ISC) that provides 24/7 standardized multimodal and multidisciplinary care to AMI patients referred from the Paris region19. Since the creation of this center, we prospectively enrolled patients from the ISC department and the emergency room (ER) department who undergo a contrast-enhanced CT-scan for acute abdominal pain as part of the SURVIBIO cross-sectional diagnostic study. The patients' blood samples were collected on admission and stored in a biobank for further biomarker analysis and research. We used the blood samples from the biobank to assess the performance of three circulating candidate biomarkers—citrulline, I-FABP, and d-lactate—in the diagnosis of AMI. The study was approved by the Ethics Committee of Paris-Nord Val de Seine University Hospitals. The study complies with the Standards for Reporting Diagnostic Accuracy (STARD) guidelines20. Written informed consent was obtained from all patients.
Patients and controls
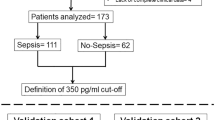
From January 4, 2016, to March 5, 2018, prospective patients who presented with acute abdominal pain requiring a contrast-enhanced CT scan to the ER department or referred to the ISC department were evaluated for inclusion in the SURVIBIO diagnostic study. Patients with AMI were admitted to the ISC, whereas those in whom the diagnosis of AMI was ruled out (controls) were admitted to the emergency room (see patient flowchart, Fig. 1). Patients presenting with a diagnosis of left-sided colon ischemia without small bowel injury, chronic mesenteric ischemia without acute injury, vascular lesions with no small bowel injury, or strangulated bowel obstruction were not included (see patient flowchart, Fig. 1).
AMI was defined by the association of (1) acute clinical, biological, and/or contrast-enhanced CT features of bowel injury, (2) vascular insufficiency (occlusive or non-occlusive) of the celiac trunk and/or the superior mesentery artery and/or superior mesenteric vein, and (3) the absence of an alternative diagnosis6. The diagnosis was subsequently confirmed by histology following intestinal resection8.
The diagnosis of AMI was ruled in or out by the CT scan, and alternative final diagnoses were based on clinical, biological, and CT findings. All the patients' clinical records, CT-scans, and pathologic specimens were reviewed in a multidisciplinary meeting, including gastroenterologists, radiologists, digestive and vascular surgeons, and intensivists, all experts in digestive vascular diseases, to avoid diagnostic misclassification before any blood sample analysis.
All the AMI patients were managed by a standardized multimodal and multidisciplinary approach in our intestinal stroke center, as previously described1. Briefly, the patients were systematically administered oral antibiotics and antithrombotics1,6, and emergency endovascular revascularization of arterial AMI was performed whenever technically feasible. Alternatively, open surgical revascularization was performed. Bowel viability was evaluated by laparotomy, decided based on published risk factors for irreversible transmural intestinal necrosis (occurrence of organ failure, elevated plasma lactate concentrations, small bowel dilatation, or perforation on CT)8. Irreversible transmural intestinal necrosis was confirmed upon pathological assessment.
AMI subgroups
AMI patients were characterized depending on the cause of the splanchnic vascular insufficiency as being arterial AMI (including arterial stenosis, thrombosis or embolus) or venous AMI (due to portal and/or mesenteric vein thrombosis or compression). Patients presenting with or without irreversible transmural intestinal necrosis were included in the late necrotic or early AMI subgroups, respectively. The presence of irreversible intestinal ischemic injury was defined, as previously proposed8, by: (a) pathology assessment as anoxic, extensive, transmural necrosis with hemorrhagic and/or gangrenous infarction or (b) evidence of bowel perforation on CT evaluation or (c) extensive necrosis assessed during open-close laparotomy procedures in unresected patients. Patients with superficial non-transmural ischemic necrosis upon pathological assessment and those who recovered from AMI with no need for digestive surgery were considered not to have irreversible transmural intestinal necrosis8.
Data collection and processing
Routine baseline clinical and biological characteristics were collected upon admission for all patients: age, gender, body mass index (BMI), history of cardiovascular disease or risk factors, general and digestive clinical signs, and common biological features. The origin of AMI (arterial—thrombotic or embolic—venous, or non-occlusive) was specified based on the patient's records, CT-scan, and pathologic review.
Blood samples were collected from all the patients on admission and stored for further biomarker analysis. Blood samples were collected in appropriate vacutainers before immediate centrifugation at 1500 × g for 15 min at room temperature, and isolated plasma samples underwent subsequent storage at − 80 °C until further analysis.
Blood samples were collected in appropriate vacutainers before immediate centrifugation at room temperature, and isolated plasma samples have undergone subsequent storage.
Biomarker measurements were performed in 2019 after the final diagnosis classification had been made in all patients. After randomization of all samples, Citrulline, d-lactate, and I-FABP levels were measured on plasma collected in heparin, oxalate, and EDTA-treated tubes, respectively.
I-FABP concentrations were measured in plasma using two different ELISA kits [Hycult Bioteck, Uden, The Netherlands, HK40602, range: 0–3000 ng/L21,22; and R&D Systems, Liey, DY3078, linearity range: 0–1000 ng/L23] according to the manufacturer's instructions. We used two quality controls (sample pool)—at the beginning and the end of the plates. Briefly, samples and standards were incubated in 96-well microtiter plates coated with antibodies recognizing human I-FABP. The biotinylated secondary antibody was then added to the wells. After washes, streptavidin-peroxidase conjugate, which binds the biotinylated secondary antibody, was added and reacted with tetramethylbenzidine (TMB) substrate. The absorbance was then measured with a spectrophotometer at 450 nm (Infinite 200 PEO, TECAN).
Citrulline plasma levels were assayed using an ultra-performance liquid chromatography-mass spectrometer (UPLC-MS; Xevo TQS, Waters). We first conducted a two-step extraction: 100 μL of heparin plasma were added to 300 μL of acetonitrile (ACN; VWR) with 0.05% citrulline C13 (Cambridge Isotope laboratories Inc.)and 1% formic acid (FA; VWR) to precipitate proteins. After 5 min of mechanical agitation, the mixes were centrifuged at 13,000 × g for 5 min at room temperature. Then, 300 µL of the supernatant was loaded onto an Ostro Plate (Waters) and extracted under positive pressure. The eluate was diluted 1:2 in ACN/H20 (90:10), and 2 µL were injected in the UPLC-MS. The mobile phase A was water with ammonium formate 10 mM (A.F.; VWR) and 0.15% FA, and the mobile phase B was A.F. 10 mM in ACN with 0.15% FA. The retention time was 1.43 min on the Xevo TQS, Waters. The results are presented as an average of two measurements (duplicate). If a coefficient of variation higher than 10% was observed between two measures, the sample was reanalyzed.
d-lactate plasma concentration was assayed by a kinetic spectrophotometric method using an adapted method of the Biosentec d-Lactic acid kit on a Cobas C111 analyzer (Roche). Briefly, the reaction used an endpoint analysis of the following reaction, catalyzed by the d-lactate dehydrogenase: Lactate + NAD → Pyruvate + NADH + H + Pyruvate + Glutamate → Alanine + α-ketoglutarate. NADH was measured at 340 nM. Low-and high-level quality controls were included at the beginning and the end of each batch.
Statistical analysis
For each of the continuous variables, we report the median and the interquartile range (IQR). Categorical variables are expressed as the number of observations and percentages. Normally distributed quantitative data were analyzed with the Student t-test. Mann–Whitney U test was used otherwise. Subgroup analyses were performed with the use of the Kruskal–Wallis tests for skewed distributions. When the result of a global test was significant (p < 0.05), post hoc Bonferroni-corrected pairwise comparisons were performed. Qualitative data were compared with either the Pearson χ2 test or the Fisher exact test, depending on the sample size. We determined that the enrollment of 50 patients in each group would provide a power of more than 95% for assessing diagnostic tests with AUC ≥ 0.7024. The diagnostic accuracy of each biomarker was evaluated by analyzing the receiver operating curve (ROC) with the calculation of the area under the ROC (AUROC). The maximum value of Youden's index was used as a criterion for selecting the optimal cut-off value of each biomarker, reported with its associated sensitivity, specificity, negative predictive values (NPV), and positive predictive values (PPV). All tests were two-sided. No imputation of missing data was performed. Analyses were performed using the Statistical Package for the Social Sciences (SPSS) for Mac OSX software (version 23.0, Chicago, IL, USA) and the pROC package25 in R software, version 3.6.2 (R Foundation for Statistical Computing).
Results
Characteristics of study subjects
A total of 179 patients with acute abdominal pain requiring a contrast-enhanced CT-scan were assessed for eligibility (Fig. 1). We included and collected blood samples from 131 patients, including 50 admitted to our intestinal stroke center for AMI and 79 admitted to the emergency room for non-AMI acute abdominal pain (see Flowchart, Fig. 1). We excluded 2 patients (controls) with missing samples upon biological analysis. The baseline characteristics of both populations are summarized in Table 1. The final diagnosis of the controls is presented in Table 2. Patients with AMI [median age: 65 years (IQR 55–75), 38% of women] included arterial and venous causes in 66% and 34% of cases, respectively. None of the patients included had non-occlusive AMI. AMI occurred in seven patients with past history of chronic mesenteric ischemia. Patients with AMI were significantly older, had a higher BMI, and were more likely to have risk factors or a history of cardiovascular disease than controls (Table 1). AMI patients were also more likely to present hematochezia, guarding, and organ dysfunction (as measured by a total Sequential Organ-Failure Assessment (SOFA) score ≥ 2)26 and a higher white blood cell count at baseline. Other clinical and biological characteristics, including l-lactate levels, did not differ significantly (Table 1). AMI patients were referred from primary care hospitals within a median of 8 h (range 6–12). After admission in the intestinal stroke center, AMI patients received antiplatelet therapy (n = 33, 100% arterial AMI), anticoagulants (n = 50, 100%), oral antibiotics (n = 49, 98%), and intravenous antibiotics (n = 21, 42%). Emergency revascularization was performed in 29 patients (88% of arterial AMI patients).
Main results
Median plasma citrulline concentrations were significantly lower in the AMI patients compared to the controls [15.3 μmol/L (IQR 12.0–26.0) vs. 23.3 μmol/L (18.3–29.8), p = 0.001], although the two distributions broadly overlapped (Fig. 2). Plasma I-FABP concentrations tended to be lower in the AMI population compared to the controls using Hycult kit [278 ng/L (209–544) vs. 348 ng/L (268–587), p = 0.06]. We then confirmed a similar trend using the R&D kit (Supplementary Data Fig. 1). Results obtained with the Hycult kit were further used for statistical analyses.
Citrulline, I-FABP and d-lactate plasma concentrations in AMI patients and controls. Abbreviations: I-FABP intestinal fatty-acid binding protein, AMI acute mesenteric ischemia. Comparison of acute abdominal pain controls (n = 79) and patients with AMI (n = 50). The horizontal line in the boxes represents the median, and the bottom and top of the boxes the 25th and 75th percentiles, respectively. I bars represent the upper adjacent value (75th percentile plus 1.5 times the interquartile range) and the lower adjacent value (corresponding formula below the 25th percentile). Outliers are represented by dots (outside of the I bars) and extreme outliers by asterisks (outside of the 75th percentile plus 3 times the interquartile range, or the 25th percentile minus 3 times the interquartile range).
Plasma d-lactate concentrations did not significantly differ between AMI patients and controls [0.042 mmol/L (0.025–0.095) vs. 0.073 mmol/L (0.031–0.115), p = 0.28)]. Performances of the three biomarkers for the diagnosis of AMI are summarized in Table 3.
Arterial versus venous AMI subgroups
Thirty-three patients (66%) presented with arterial AMI, and 17 patients (34%) presented with venous AMI. Compared to the controls, median plasma citrulline was significantly lower in patients with arterial AMI [14.5 μmol/L (11.1–29.1) vs. 23.3 μmol/L (18.3–29.8), p = 0.01] and slightly lower in patients with venous AMI [16.6 μmol/L (13.0–21.2) vs. 23.3 μmol/L (18.3–29.8), p = 0.06]. We did not observe significant differences in the concentration of plasma I-FABP in arterial and venous AMI versus control patients [281 ng/L (169–647) and 262 ng/L (248–487) vs. 348 ng/L (268–587), respectively, Kruskal–Wallis test p = 0.21]. Neither did we observe significant differences in the concentration of plasma d-Lactate concentrations [0.054 mmol/L (0.033–0.107) in arterial AMI and 0.025 mmol/L (0.022–0.088) in venous AMI vs. 0.073 mmol/L (0.031–0.115) in controls, Kruskal–Wallis test p = 0.24] (Supplemental data Fig. 2).
Early versus late necrotic AMI subgroups
During the follow-up period, 17 of the AMI patients (34%) required a laparotomy, and 12 (24%) required bowel resection. Irreversible transmural intestinal necrosis was pathologically confirmed in 10 of the 12 resected cases. Four additional patients had undergone open-close procedures (i.e., without performing bowel resection) showing visible extensive dark necrosis and were included in the late necrotic AMI subgroup (n = 14). Patients with superficial and non-transmural necrosis (n = 2), as well as those who recovered from AMI with no need for bowel resection (n = 34), were included in the early AMI subgroup (n = 36).
As presented in Fig. 3, plasma citrulline concentrations were significantly lower in both late necrotic AMI [13.5 (10.3–25.5) µmol/L, p = 0.02] and early AMI patients [17.9 (12.3–26.0) µmol/L, p = 0.02] as compared to controls [23.3 (18.3–29.8) μmol/L]. However, the comparison failed to discriminate late necrotic from early AMI patients. We observed a trend of higher plasma I-FABP concentrations in late necrotic AMI patients [619 ng/L (212–1632)] compared to early AMI patients [268 ng/L (205–403), p = 0.12] and controls [348 ng/L (268–587), p = 1.0]. However, I-FABP levels were significantly lower in early AMI patients compared to controls (p = 0.03). We did not find any significant difference in plasma d-lactate concentrations between late necrotic AMI patients [0.069 mmol/L (0.036–0.128)] or either early AMI patients or controls [0.035 mmol/L (0.024–0.091) and 0.073 mmol/L (0.031–0.115), respectively, Kruskal–Wallis test p = 0.26].
Citrulline, I-FABP, and d-lactate blood concentrations according to the severity of acute mesenteric ischemia (early or late—necrotic—ischemia). Abbreviations: AMI acute mesenteric ischemia, I-FABP intestinal fatty-acid binding protein. Comparison of acute abdominal pain controls (n = 79) and patients with early AMI (n = 36), and necrotic AMI (n = 14). Analyses were performed with the use of the Kruskal–Wallis test. When the result of a global test was significant (p < 0.05), post hoc Bonferroni-corrected pairwise comparisons were performed. The horizontal line in the boxes represents the median, and the bottom and top of the boxes, the 25th and 75th percentiles, respectively. I bars represent the upper adjacent value (75th percentile plus 1.5 times the interquartile range) and the lower adjacent value (corresponding formula below the 25th percentile). Outliers are represented by dots (outside of the I bars) and extreme outliers by asterisks (outside of the 75th percentile plus 3 times the interquartile range, or the 25th percentile minus 3 times the interquartile range).
Discussion
This cross-sectional diagnostic study of 129 patients admitted for acute abdominal pain found that the three most promising circulating biomarker candidates for AMI—citrulline, I-FABP, and d-lactate—were neither sensitive nor specific enough for differential diagnosis of AMI: I-FABP and d-lactate displayed low AUROC values, and citrulline assays had low sensitivity. These results contrast with published reports4,14,15,16. This could be explained by two critical differences in the experimental designs. Firstly, previous studies enrolled severe AMI patients at a late necrotic surgical stage. This may have created a selection bias leading to an overestimated performance of the studied biomarkers, not generalizable to earlier stages of the disease. Secondly, in most of the studies published so far, only a restricted number of AMI patients were included. They were merged with heterogeneous pathologic conditions labeled “ischemic bowel diseases”, such as strangulated bowel obstructions or left-side colon ischemia with no small bowel injury. This may have led to an overestimation of the specificity of the studied biomarkers for the diagnosis of genuine vascular-related AMI. For instance, Shi et al. studied 39 patients with “acute intestinal ischemic disease,” including 26 with strangulated bowel obstruction, six with colon ischemia with no small bowel injury, and only seven patients with genuine AMI at the infarction stage27. Similarly, Kanda et al. studied 52 preoperative patients with “small bowel ischemia,” including 45 cases of strangulated bowel or incarcerated hernia and only three patients with late necrotic AMI28. In the present study, we included a large and homogeneous population of 50 patients with confirmed arterial and venous AMI, treated with a standardized care protocol in an intestinal stroke center, enrolled on admission at the time of diagnosis, and at an early “non-transmural” AMI stage in 72% of cases. Therefore, our design yields reliable results on clinically applicable AMI biomarkers in its emergency “real-life” early-stage diagnosis.
I-FABP is a cytosolic protein expressed by mature enterocytes at the tip of the small bowel villi, which is the first region affected by ischemia29. In the past decades, a few studies on human samples have identified I-FABP as the most promising biomarker for diagnosing AMI. The recent meta-analysis by Sun et al. calculated a pooled sensitivity, specificity, and AUROC of 0.80, 0.85, and 0.86, respectively15. Nevertheless, it should be noted that only 60 of the 1246 patients studied in this meta-analysis had genuine vascular-related AMI, mainly at the infarction stage (after a careful review of seven of the nine English-language studies included)15. Furthermore, this meta-analysis included studies using various methods for I-FABP measurements and various blood sample types that could be significant confounding factors.
Although we observed higher I-FABP plasma concentrations in late necrotic AMI patients, its discriminative diagnostic performance for AMI was not confirmed. This result was supported by another ELISA assay to exclude any analytical bias (see Supplemental Data Fig. 1). We even observed higher I-FABP concentrations in controls in comparison with early-stage AMI patients. This observation is also in line with numerous published studies that observed high I-FABP blood concentrations in various other non-ischemic gastro-intestinal conditions such as Crohn's disease30, celiac disease31,32, acute pancreatitis33,34, or abdominal surgery/infection35.
d-Lactate is the stereoisomer of l-lactate and is almost exclusively produced by microbial fermentation in the gastro-intestinal tract. Consequently, animal experiments and a few clinical studies identified this molecule as a marker of intestinal barrier dysfunction and microbial translocation or overgrowth36,37. However, its accuracy has been questioned by studies such as the ones by Van Der Voort et al.38 and Block et al.39, reporting low (23%) specificity, consistent with the present findings.
Citrulline is an amino acid synthesized from glutamine by small bowel enterocytes. It is considered as a functional biomarker of total enterocyte mass and intestinal failure. Low citrulline plasma levels have been found to correlate with remnant small bowel length and intestinal failure in patients with short bowel syndrome40 and with the severity of villous atrophy in patients with celiac disease41. In a prospective single-center observational study that included adults without small bowel disease and chronic renal failure consecutively admitted in an intensive care unit, citrulline plasma concentrations were lower for the 24 h following the circulatory shock42. Concentrations < 10 µmol/L were highlighted as an independent risk factor of mortality, suggesting that low plasma citrulline at 24 h could be a marker of acute intestinal failure in critically ill patients. We observed significantly lower citrulline plasma levels in patients with AMI compared to the controls, consistent with prior reports16,43. As already reported—but here in a larger cohort—we confirm that the sensitivity of citrulline is insufficient in this setting. Our findings are consistent with the results obtained by Kulu et al. They found a sensitivity of 39% for citrulline for the identification of AMI in 23 patients, with the best cut-off value at 15.8 µmol/L43. Altogether, this corroborates that citrulline displays a low diagnostic performance for AMI, which, regrettably, limits its usefulness: sensitivity is more important than specificity for AMI given the severe consequences of misdiagnosis and offered that confirmation by a contrast-enhanced CT scan remains mandatory to guide emergency treatment (type of revascularization, need for intestinal resection).
A few limitations derived from the design of the present study deserve to be mentioned. First, we chose not to include patients with strangulated bowel obstruction, left-sided colon ischemia, and mesenteric vessel occlusion without evidence of acute minor bowel injury from both patients and control groups. Although these conditions may share pathophysiological processes comparable with AMI, they are different diseases with different prognoses. Although this might decrease the generalizability of our findings to these other conditions, we believe this selection is critical to reduce variability and avoid analytical bias, which are the main shortcomings of available reports in this field of research3. Nonetheless, our results are based on the largest population of well-characterized and homogeneous AMI patients. This is crucial as the diagnosis of AMI amongst emergency patients admitted for acute abdominal pain remains a critical clinical challenge3, and our findings indicate that the three tested biomarkers do not reach a sufficient diagnostic performance level. Moreover, as compared with previously published studies, we used two different assays for I-FABP, as well as two robust, standardized methods for both citrulline and d-lactate measurements. Furthermore, as no patients with non-occlusive mesenteric ischemia (NOMI) were included in the present study, our results are not generalizable to this specific cause of mesenteric ischemia. Indeed, NOMI is usually the complication of an underlying severe disease causing systemic hypoperfusion in intensive care patients, and such patients were not the target population of this diagnostic study.
In conclusion, Citrulline, I-FABP, and d-lactate failed to identify AMI from acute abdominal pain controls in a large cross-sectional diagnostic study from an Intestinal Stroke Center. Early diagnosis remains a critical clinical and research challenge as it would allow early management and consequently improve the dire prognosis of AMI. We believe that relevant new biomarkers may be identified using non-targeted multi-omics discovery approaches in large cohorts of early-stage AMI patients admitted in intestinal stroke centers to meet this challenge. This objective is of the utmost importance since the introduction of new biomarkers may genuinely alter the epidemiology, diagnosis, management, and outcome of AMI.
Data availability
Research data are not shared.
References
Corcos, O. et al. Effects of a multimodal management strategy for acute mesenteric ischemia on survival and intestinal failure. Clin. Gastroenterol. Hepatol. 11, 158e2-165e2 (2013).
Clair, D. G. & Beach, J. M. Mesenteric ischemia. N. Engl. J. Med. 374, 959–968 (2016).
Nuzzo, A., Ronot, M., Maggiori, L. & Corcos, O. Early acute mesenteric ischemia: Many rivers to cross. Ann. Surg. 268, e41 (2018).
Peoc’h, K., Nuzzo, A., Guedj, K., Paugam, C. & Corcos, O. Diagnosis biomarkers in acute intestinal ischemic injury: So close, yet so far. Clin. Chem. Lab. Med. 56, 373–385 (2018).
Ding, W. et al. Open abdomen improves survival in patients with peritonitis secondary to acute superior mesenteric artery occlusion. J Clin. Gastroenterol. 51, e77–e82 (2017).
Nuzzo, A. et al. Oral antibiotics reduce intestinal necrosis in acute mesenteric ischemia: A prospective cohort study. Am. J. Gastroenterol. 114, 348–351 (2019).
Nuzzo, A., Huguet, A. & Corcos, O. Modern treatment of mesenteric ischemia. Presse Med. 47, 519–530 (2018).
Nuzzo, A. et al. Predictive factors of intestinal necrosis in acute mesenteric ischemia: Prospective study from an intestinal stroke center. Am. J. Gastroenterol. 112, 597–605 (2017).
Corcos, O. & Nuzzo, A. Gastro-intestinal vascular emergencies. Best Pract. Res. Clin. Gastroenterol. 27, 709–725 (2013).
Lehtimaki, T. T. et al. Detecting acute mesenteric ischemia in CT of the acute abdomen is dependent on clinical suspicion: Review of 95 consecutive patients. Eur. J. Radiol. 84, 2444–2453 (2015).
Garzelli, L. et al. Contrast-enhanced CT for the diagnosis of acute mesenteric ischemia. AJR Am. J. Roentgenol. 215, 29–38 (2020).
Copin, P. et al. Inter-reader agreement of CT features of acute mesenteric ischemia. Eur. J. Radiol. 105, 87–95 (2018).
Derikx, J. P., Schellekens, D. H. & Acosta, S. Serological markers for human intestinal ischemia: A systematic review. Best Pract. Res. Clin. Gastroenterol. 31, 69–74 (2017).
Evennett, N. J., Petrov, M. S., Mittal, A. & Windsor, J. A. Systematic review and pooled estimates for the diagnostic accuracy of serological markers for intestinal ischemia. World J. Surg. 33, 1374–1383 (2009).
Sun, D. L. et al. Accuracy of the serum intestinal fatty-acid-binding protein for diagnosis of acute intestinal ischemia: A meta-analysis. Sci. Rep. 6, 34371 (2016).
Treskes, N., Persoon, A. M. & van Zanten, A. R. H. Diagnostic accuracy of novel serological biomarkers to detect acute mesenteric ischemia: A systematic review and meta-analysis. Intern. Emerg. Med. 12, 821–836 (2017).
Bjorck, M. et al. Editor’s choice—Management of the diseases of mesenteric arteries and veins: Clinical practice guidelines of the European Society of Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 53, 460–510 (2017).
Terlouw, L. G. et al. European guidelines on chronic mesenteric ischaemia—Joint United European Gastroenterology, European Association for Gastroenterology, Endoscopy and Nutrition, European Society of Gastrointestinal and Abdominal Radiology, Netherlands Association of Hepatogastroenterologists, Hellenic Society of Gastroenterology, Cardiovascular and Interventional Radiological Society of Europe, and Dutch Mesenteric Ischemia Study group clinical guidelines on the diagnosis and treatment of patients with chronic mesenteric ischaemia. United Eur. Gastroenterol. J. 8, 371–395 (2020).
Nuzzo, A. & Corcos, O. Management of mesenteric ischemia in the era of intestinal stroke centers: The gut and lifesaving strategy. Rev. Med Intern. 38, 592–602 (2017).
Bossuyt, P. M. et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 351, h5527 (2015).
Thuijls, G. et al. Early diagnosis of intestinal ischemia using urinary and plasma fatty acid binding proteins. Ann. Surg. 253, 303–308 (2011).
Guzel, M. et al. Value of the serum I-FABP level for diagnosing acute mesenteric ischemia. Surg. Today 44, 2072–2076 (2014).
Salim, S. Y., Young, P. Y., Churchill, T. A. & Khadaroo, R. G. Urine intestinal fatty acid-binding protein predicts acute mesenteric ischemia in patients. J. Surg. Res. 209, 258–265 (2017).
Obuchowski, N. A., Lieber, M. L. & Wians, F. H. Jr. ROC curves in clinical chemistry: Uses, misuses, and possible solutions. Clin. Chem. 50, 1118–1125 (2004).
Robin, X. et al. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 12, 77 (2011).
Vincent, J. L. et al. The SOFA (Sepsis-Related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710 (1996).
Shi, H., Wu, B., Wan, J., Liu, W. & Su, B. The role of serum intestinal fatty acid binding protein levels and d-lactate levels in the diagnosis of acute intestinal ischemia. Clin. Res. Hepatol. Gastroenterol. 39, 373–378 (2015).
Kanda, T. et al. Diagnosis of ischemic small bowel disease by measurement of serum intestinal fatty acid-binding protein in patients with acute abdomen: A multicenter, observer-blinded validation study. J. Gastroenterol. 46, 492–500 (2011).
Gollin, G., Marks, C. & Marks, W. H. Intestinal fatty acid binding protein in serum and urine reflects early ischemic injury to the small bowel. Surgery 113, 545–551 (1993).
Sarikaya, M. et al. Intestinal fatty acid binding protein (I-FABP) as a promising test for Crohn’s disease: A preliminary study. Clin. Lab. 61, 87–91 (2015).
Adriaanse, M. P. et al. Serum I-FABP as marker for enterocyte damage in coeliac disease and its relation to villous atrophy and circulating autoantibodies. Aliment Pharmacol. Ther. 37, 482–490 (2013).
Adriaanse, M. P. et al. Serum I-FABP detects gluten responsiveness in adult celiac disease patients on a short-term gluten challenge. Am. J. Gastroenterol. 111, 1014–1022 (2016).
Kupcinskas, J. et al. Intestinal fatty acid binding protein as a marker of necrosis and severity in acute pancreatitis. Pancreas 47, 715–720 (2018).
Goswami, P., Sonika, U., Moka, P., Sreenivas, V. & Saraya, A. Intestinal fatty acid binding protein and citrulline as markers of gut injury and prognosis in patients with acute pancreatitis. Pancreas 46, 1275–1280 (2017).
Bingold, T. M. et al. Intestinal fatty acid binding protein: A sensitive marker in abdominal surgery and abdominal infection. Surg. Infect. (Larchmt.) 16, 247–253 (2015).
Murray, M. J., Barbose, J. J. & Cobb, C. F. Serum d(-)-lactate levels as a predictor of acute intestinal ischemia in a rat model. J. Surg. Res. 54, 507–509 (1993).
Murray, M. J., Gonze, M. D., Nowak, L. R. & Cobb, C. F. Serum d(-)-lactate levels as an aid to diagnosing acute intestinal ischemia. Am. J. Surg. 167, 575–578 (1994).
van der Voort, P. H. et al. Can serum l-lactate, d-lactate, creatine kinase and I-FABP be used as diagnostic markers in critically ill patients suspected for bowel ischemia. BMC Anesthesiol. 14, 111 (2014).
Block, T., Nilsson, T. K., Bjorck, M. & Acosta, S. Diagnostic accuracy of plasma biomarkers for intestinal ischaemia. Scand. J. Clin. Lab. Investig. 68, 242–248 (2008).
Crenn, P., Coudray-Lucas, C., Thuillier, F., Cynober, L. & Messing, B. Postabsorptive plasma citrulline concentration is a marker of absorptive enterocyte mass and intestinal failure in humans. Gastroenterology 119, 1496–1505 (2000).
Crenn, P. et al. Plasma citrulline: A marker of enterocyte mass in villous atrophy-associated small bowel disease. Gastroenterology 124, 1210–1219 (2003).
Piton, G. et al. Plasma citrulline kinetics and prognostic value in critically ill patients. Intensive Care Med. 36, 702–706 (2010).
Kulu, R., Akyildiz, H., Akcan, A., Ozturk, A. & Sozuer, E. Plasma citrulline measurement in the diagnosis of acute mesenteric ischaemia. ANZ J. Surg. 87, E57–E60 (2017).
Acknowledgements
Anne Barnier for doing all the LC–MS measurements of citrulline. Estelle Marcault and the URC Paris-Nord team for the supervision of the SURVIBIO study.
Funding
Grants from MSD-Avenir and APHP funded the SURVIBIO study; Alexandre Nuzzo received Ph.D. Grants from “Fondation de l'Avenir” and the French Gastroenterology Society (SNFGE).
Author information
Authors and Affiliations
Consortia
Contributions
Study concept and design: Al.N., K.P., O.C., N.G.; acquisition of data: Al.N., K.P., K.G., S.C., C.H., C.B., A.T.-D.; radiological review: M.R., statistical analysis: Al.N., K.G.; drafting of the manuscript: Al.N., K.P., K.G.; data interpretation and critical revision of the manuscript for valuable intellectual content: S.C., C.H., C.B., An.N., Y.B., Y.C., N.G.; study supervision: O.C., K.P., N.G.; and patient’s inclusion and care: SURVI research group.
Corresponding author
Ethics declarations
Competing interests
SURVI research program is supported by MSD-AVENIR grant and institutional funding (APHP). All authors have no other competing interests than MSD-AVENIR Grant and institutional funding (APHP).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nuzzo, A., Guedj, K., Curac, S. et al. Accuracy of citrulline, I-FABP and d-lactate in the diagnosis of acute mesenteric ischemia. Sci Rep 11, 18929 (2021). https://doi.org/10.1038/s41598-021-98012-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98012-w
This article is cited by
-
Improving clinical suspicion of acute mesenteric ischemia among patients with acute abdomen: a cross-sectional study from an intestinal stroke center
World Journal of Emergency Surgery (2023)
-
Diagnostic accuracy of biomarkers to detect acute mesenteric ischaemia in adult patients: a systematic review and meta-analysis
World Journal of Emergency Surgery (2023)
-
Are Mortality and Morbidity Predictable in Acute Mesenteric Ischemia? The Importance of Serum Lactate, Lactate Dehydrogenase, and Blood Urea Nitrogen Levels
Indian Journal of Surgery (2023)
-
Prognostic factors in patients with acute mesenteric ischemia—novel tools for determining patient outcomes
Surgical Endoscopy (2022)
-
Acute mesenteric ischemia: updated guidelines of the World Society of Emergency Surgery
World Journal of Emergency Surgery (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.