Abstract
Intestinal microbiota (IM) diversity and composition regulates host immunity and affects outcomes after allogeneic stem cell transplantation (allo-HSCT). We evaluated if the oral mucosa microbiota (OM) could impact the outcomes in patients who underwent allo-HSCT. Samples from the oral mucosa of 30 patients were collected at three time points: before the conditioning regimen, at aplasia, and at engraftment. We analyzed the associations of OM diversity and composition with allo-HSCT outcomes. Lower OM diversity at preconditioning was associated with a higher risk of relapse at 3 years (68% versus 33%, respectively; P = 0.04). Dominance (relative abundance ≥ 30%) by a single genus at preconditioning was also associated with a higher risk of relapse (63% versus 36% at 3 years, respectively; P = 0.04), as well as worse progression-free survival (PFS; 19% versus 55%, respectively; P = 0.01), and overall survival (OS) at 3 years (38% versus 81%, respectively; P = 0.02). In our study we observed that OM dysbiosis is associated with a higher risk of relapse and worse survival after allo-HSCT.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) remains the only therapeutic option for several hematological neoplasms1. Although transplant outcomes have markedly improved in recent decades, relapse of the underlying condition remains the leading cause of death after allo-HSCT2. Despite conflicting results, several risk factors have been shown to affect relapse, including the intensity of the conditioning regimen3,4,5, pre-HSCT disease status6, donor age7,8, graft source9, killer immunoglobulin-like receptor compatibility10, graft versus host disease (GVHD) prophylaxis11,12,13, and the occurrence of chronic GVHD (cGVHD)14. Infections, acute GVHD (aGVHD), cGVHD, and secondary neoplasia are the main causes of non-relapse mortality (NRM)2,15. The disease risk index (DRI) stratifies the risk of mortality in patients after allo-HSCT, according to diagnosis and disease status16.
The intestinal microbiota (IM) has been shown to play a vital role in regulating host immunity17 and improving antineoplastic activity18,19. In addition, IM disruption, characterized by significant changes in microbiota diversity and composition, is associated with allo-HSCT clinical outcomes. Common complications after allo-HSCT, such as infections, mucositis, and GVHD, are associated with significant changes in IM diversity and composition. In allo-HSCT, IM disruption is also associated with the incidence of GVHD20,21,22, overall survival (OS)23,24,25,26, and underlying disease relapse27,28.
The human oral cavity harbors the second most abundant microbiota after the gastrointestinal tract. As observed for the IM, the oral microbiota (OM) directly influences human health29. OM disruption has been observed in several diseases, including diabetes, autoimmune diseases, endocarditis, gastrointestinal cancer, head and neck cancer30,31,32, and acute lymphoblastic leukemia33. Changes in the OM in patients undergoing allo-HSCT are known to be associated with respiratory signs and symptoms34 and oral mucositis35; however, no correlation between OM and allo-HSCT outcomes have been reported to date.
Accordingly, in this study, we evaluated whether the OM disruption is related to outcomes in patients who underwent allo-HSCT.
Methods
Patient characteristics and sample collection
We collected samples from the oral mucosa of patients who underwent allo-HSCT at Hospital Sírio Libanês, São Paulo, Brazil between January 2016 and April 2018.
Samples were collected by rubbing the dorsal tongue and andwith sterile swabs at three time points: before the conditioning regimen and before the oral medicine specialist intervention (preconditioning), at aplasia (defined as the first day of neutrophils under 0.5 × 103/uL), and at engraftment. All patients were requested not to perform oral hygiene for at least 6 h before collection. Informed consent was obtained from all patients before collection. The study was approved by the local ethics committee (Comite de Ética em Pesquisa—Hospital Sírio Libanês), according to the Declaration of Helsinki. No tissue was procured from prisoners in this study. All patients were examined by an oral medicine specialist for potential infections, and all followed the same protocol for oral mucositis prophylaxis with photobiomodulation and oral hygiene with fluoride toothpaste and 0.12% chlorhexidine mouthwash. The standard antimicrobial prophylaxis in our institution included oral levofloxacin, acyclovir, and antifungal prophylaxis according to the patient's risk of fungal infection (voriconazole for high-risk patients, and fluconazole for low risk patients).
DNA extraction
Bacterial cells were recovered from oral mucosa swabs through vortexing in TE buffer supplemented with 6 μL PureLink RNAse A (20 mg/mL; Thermo Fisher Scientific, Waltham, MA, USA). DNA was extracted using a QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocol (DNA Purification from Blood or Body Fluids) and stored at − 80 °C.
16S rRNA amplicon sequencing
For 16S rRNA amplicon sequencing, 12.5 ng DNA and prevalidated primers36 were used to amplify 16S rRNA hypervariable regions V3–V4. Amplicons were sequenced as described elsewhere37 on an Illumina MiSeq platform (Illumina, San Diego, CA, USA).
Bioinformatics pipeline
Reads were demultiplexed, and primer sequences were removed using the MiSeq Reporter software. Within the QIIME 2 framework38, using experiment-specific adaptive error models39, forward and reverse sequences were filtered for quality and bimeras, denoised, and merged into consensus sequences with the DADA2 pipeline40, generating unique amplicon sequencing variants (ASVs). ASVs were further filtered for chimeric sequences using the SILVA database41 and UCHIME42. ASVs were taxonomically assigned using SILVA database and VSEARCH tool43.
Statistical analyses
For alpha diversity analyses, the samples were rarefied to 12,500 reads before calculating the Shannon index, Simpson index, or the number of observed ASVs as bacterial diversity measures with the QIIME 2 q2-diversity plugin. Alpha diversity across groups was compared with the Mann–Whitney U test. OM diversity was classified based on the median Shannon index diversity measure across the study population at a given collection time point. Patients were classified as high diversity (above the Shannon index median) and low diversity (below Shannon index median). Fisher’s exact tests and two-sided Student's t-tests were used to evaluate the associations between alpha diversity status and categorical and numerical clinical parameters, respectively. The relative abundance of each taxa was calculated with the QIIME 2 q2-taxa plugin. The taxa shown on relative abundance longitudinal plots are all those showing dominance (relative abundance ≥ 30%) in at least one study sample or relative abundance ≥ 5% in at least 25% of study samples. Differentially abundant genera across transplantation phases were identified using ANCOM test, with relative differences represented by the log-transformed average relative abundance fold change between groups. ANCOM W represents the proportion of null hypotheses rejected when sub-testing the differential abundance of a genus normalized by the abundance of each one of the genera in the dataset. W > 0.7 was considered as statistically significant. The relative abundance of a genus was considered to increase during allo-HSCT for a given patient when the relative abundance at engraftment was greater than at preconditioning and the final relative abundance was ≥ 0.1%. The probabilities of progression-free survival (PFS) and OS were calculated using the Kaplan–Meier method and compared using log-rank tests. Cumulative incidence rates were calculated for aGVHD, cGVHD, NRM, and relapse/progression. Ninety-five percent confidence intervals (95% CIs) were estimated using the Greenwood formula. Adjusted probabilities for outcomes after transplantation were estimated using the Cox proportional hazards method (PFS and OS) and Fine-Gray risk regression model (aGVHD, cGVHD, NRM, and relapse/progression). The association between OM parameters and HSCT outcome was investigated in the final model after adjusting for the DRI. First-order interactions between OM parameters and each variable of interest were examined. The results are presented as relative risks of failure (adverse prognostic factors versus good prognostic factors), with 95% CIs and two-tailed P values. To examine the association between genus presence at preconditioning and relapse, only genera present in 25–75% of samples were evaluated, where presence was defined as relative abundance ≥ 0.1%. R software (version 3.5.0) and RStudio (version 1.2.5033) were used for statistical analyses. The statistical package cmprsk was used to evaluate relapse across groups with transplant-related death as the competing risk.
Ethics approval and consent to participate
The study was approved by the local ethics committee, according to the Declaration of Helsinki.
Results
Patient characteristics
Between January 2016 and April 2018, 30 patients who underwent allo-HSCT for hematologic malignancies and had oral mucosa samples collected were included in this study. The most common underlying diseases were acute myeloid leukemia and acute lymphoblastic leukemia (60%). Conditioning regimens and intensity, graft source, T-cell depletion, and other clinical characteristics are listed in Table 1. The underlying disease, disease status, and OM diversity at preconditioning are presented in Table S1. The median follow-up time for survivors was 41 (30–50) months.
Microbiota dynamics analyses
In total, 5,920,836 high-quality bacterial assigned sequencing reads were analyzed, representing 1723 unique ASVs. Out of the 90 samples sequenced, nine were excluded from diversity analyses owing to an insufficient number of high-quality reads (< 12,500 reads per sample, as determined using alpha diversity rarefaction curves) after the read-filtering steps employed in the pipeline. Therefore, adequate preconditioning samples were available for 27 of the 30 patients included in this study.
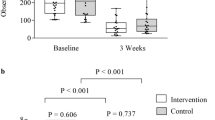
The intrasample bacterial diversity (Fig. 1A) and richness (Fig. S1) of OM samples decreased significantly during the clinical course. This drop in diversity is associated with changes in taxa relative abundance during the same period (Fig. S2). Notably, all patients showed bacterial dominance by a single genus after preconditioning. In Fig. 1B, we show three representative patients with major dominance (relative abundance > 80%) by a single genus (Stenotrophomonas, Rothia, and Veillonella, respectively) at engraftment.
Bacterial diversity within the oral mucosa decreases during allo-HSCT. (A) Oral microbiota (OM) bacterial diversity boxplot at preconditioning (n = 27), aplasia (n = 28), and engraftment (n = 26) as measured by either Shannon index (left panel) or Simpson index (right panel). Mann–Whitney U tests were used with the preconditioning collection as the reference for comparisons. The boxes highlight the median values and cover the 25th and 75th percentiles, with whiskers extending to the more extreme value within 1.5 times the length of the box. Outliers are represented explicitly. Asterisks represent statistical significance: *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001. (B) OM genera relative abundance composition across transplantation phases for three representative patients showing the decrease in bacterial diversity. Only genera showing relative abundance ≥ 30% in at least one study sample or relative abundance ≥ 5% in at least 25% of study samples are shown. P preconditioning, A aplasia, E engraftment.
For a broader assessment of the relative abundance changes from preconditioning to subsequent transplantation phases, we employed the ANCOM test at the genus level. We observed statistically significant variations in the abundance of both opportunistic pathogenic and commensal genera (Fig. S3). From preconditioning to aplasia, there was a significant increase in the abundance of the potentially pathogenic genera Enterococcus and Lactobacillus, which were even more increased in the engraftment phase in terms of relative abundance fold change from preconditioning. Staphylococcus and Mycoplasma were other potentially pathogenic genera increased at engraftment. Contrarily, there was a significant decrease in the abundance of the commensal genera Haemophilus (at aplasia) and Gemella (at engraftment).
A global increase of potentially pathogenic genera occurs during allo-HSCT. However, evaluating each patient individually, we noticed irregular changes in the relative abundance of those same genera from preconditioning to engraftment. An increase in the relative abundance of Enterococcus, Lactobacillus, Staphylococcus, and Mycoplasma was observed in 32%, 40%, 56%, and 68% of patients (Fig. S4). Patients who presented an increase in Enterococcus relative abundance had a higher incidence of cGVHD when compared with patients without the increase of relative abundance (P = 0.03). No other associations between the increase in the relative abundance of potentially pathogenic genera and allo-HSCT outcomes was observed (Table S2).
Impact of OM diversity on transplant outcomes
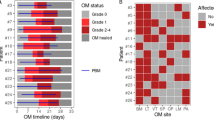
In order to elucidate the impact of OM bacterial diversity on allo-HSCT outcomes, we stratified patients into low or high diversity at each collection time (Table S3). A swimmer plot was used to illustrate these correlations at preconditioning (Fig. 2A). When we compared those with high or low OM diversity at preconditioning, no differences were found in PFS (36% versus 32%, respectively; hazard ratio [HR] 0.75, 95% CI 0.28–2.00, P = 0.57), or in OS at 3 years (54% versus 57%, respectively; HR 0.96, 95% CI 0.33–2.89, P = 0.96). We also did not observe any differences in aGVHD at 100 days (43% versus 62%, respectively; HR 1.77, 95% CI 0.66–4.81, P = 0.26). At 3 years, no difference between high and low diversity in the incidence of cGVHD (30% versus 7%, respectively; HR 4.79, 95% CI 0.56–40.8, P = 0.15), and NRM (18% vs. 0%, respectively, HR 4.12, 95% CI 0.86–19.32, P = 0.07). However, lower OM diversity at preconditioning was associated with a higher risk of relapse at 3 years when compared with higher diversity (68% versus 33%, respectively; HR, 95% CI, P = 0.04; Fig. 2B, Table S4).
Oral microbiota bacterial dominance and bacterial diversity at preconditioning increased the risk of relapse in patients who underwent allo-HSCT. (A) Oral microbiota (OM) composition and diversity at preconditioning and the respective transplant course in each patient (n = 27). Patients are sorted based on descending Shannon diversity index, with the measures shown in the left subplot y-axis. The asterisk in the Shannon index indicates patients with at least one dominant (relative abundance > 30%) genus at preconditioning. Only genera showing relative abundance ≥ 30% in at least one preconditioning sample or relative abundance ≥ 5% in at least 10% of preconditioning samples are shown. Relevant outcomes (relapse and death) after infusion (aplasia) are shown in a timeline (in months) subplot (right). The plus sign represents censoring. R relapse. (B) Cumulative incidence of relapse with patients (n = 27) stratified by OM bacterial diversity at preconditioning (high versus low). (C) The DRI-adjusted hazard ratio for the association of OM bacterial diversity at preconditioning and relapse (n = 27).
Notably, 16 (59%) patients presented some type of bacterial dominance at preconditioning. Such events encompassed 4 different genera, all of which are oral commensal: Streptococcus (dominant in 9/16 patients) and Veillonella (dominant in 2/16 patients), both members of the Firmicutes phylum; Neisseria (dominant in 3/16 patients) and Rothia (dominant in 2/16 patients). Genus dominance was detected even among patients classified as having high diversity at preconditioning (Fig. 2A). The presence of dominance by any genus at preconditioning was also associated with an increased risk of relapse at 3 years when compared with the absence of dominance (63% versus 36%, respectively; HR 4.59, 95% CI 1.11–19, P = 0.03; Fig. 3A). When evaluating dominance by specific genera or types of genera at preconditioning, neither dominance by Streptococcus (56% versus 39%, respectively; HR 1.64, 95% CI 0.52–5.14, P = 0.4), nor dominance by facultative anaerobic genera (Streptococcus or Rothia; 56% versus 39%, respectively; HR 2.05, 95% CI 0.67–6.27, P = 0.21) were associated with an increased risk of relapse. Due to the very unequal group sizes, we could not evaluate the association between dominance by Rothia (2/27 patients), Veillonella (the only dominant anaerobe; 2/27 patients) or Neisseria (the only dominant aerobe; 3/27 patients) at preconditioning and the risk of relapse.
Association of any genus dominance with relapse, progression-free survival, and overall survival. (A) Cumulative incidence of relapse with patients (n = 27) stratified by any genus dominance at preconditioning. (B) Progression-free survival (PFS) with patients (n = 27) stratified by any genus dominance at preconditioning. (C) Overall survival (OS) with patients (n = 27) stratified by any genus dominance at preconditioning. (D) The DRI-adjusted hazard ratio for the association of dominance (relative abundance > 30%) of any genus at preconditioning and relapse (n = 27). (E) The DRI-adjusted hazard ratio for the association of dominance (relative abundance > 30%) of any genus at preconditioning and PFS (n = 27). (F) The DRI-adjusted hazard ratio for the association of dominance (relative abundance > 30%) of any genus at preconditioning and OS (n = 27).
Additionally, the presence of dominance by any genus at preconditioning was associated with inferior PFS (19% versus 55%, respectively; HR 4.75, 95% CI 1.78–12.7, P = 0.01; Fig. 3B) and OS (38% versus 81%, respectively; HR 4.73, 95% CI 1.59–14.08, P = 0.02; Fig. 3C). No differences in aGVHD at 100 days (43% versus 63%, respectively; HR 0.50, 95% CI 0.18–1.37, P = 0.18), cGVHD at 3 years (19% versus 18%, respectively; HR 1.07, 95% CI 0.19–5.93, P = 0.94), or NRM at 3 years (20% versus 9%, respectively; HR 2.35, 95% CI 0.27–20.60, P = 0.44) were observed.
As expected, we also observed that patients with a high DRI had a significantly higher risk of relapse/progression, as compared with those with low-intermediate DRI at 3 years (62% versus 12%, respectively; HR 10.2, 95% CI 2.24–46.7, P < 0.01) and worse OS (77% versus 30%, respectively; HR 4.07, 95% CI 1.38–11.97, P = 0.01).
After adjusting analyses for the DRI, there was a trend toward a higher risk of relapse/progression in those with low OM diversity (HR 0.30, 95% CI 0.08–1.09, P = 0.07; Fig. 2C), and bacterial dominance of any genus remained significantly associated with the risk of relapse (HR 4.19, 95% CI 1.25–14.1, P = 0.02; Fig. 3D) and worse PFS (HR 4.14, 95% CI 1.15–14.89, P = 0.03; Fig. 3E). There was also a trend for bacterial dominance of any genus to be associated with worse OS (HR 4.12, 95% CI 0.89–19.13, P = 0.07; Fig. 3F).
Other relevant clinical parameters, such as conditioning intensity, underlying disease, and graft source, were not significantly associated with the risk of relapse (Fig. S5, Table S5).
Genus presence and transplant outcomes
As the genus level represents the most specific taxonomic level that still provides reliable taxonomic classification for V3–V4 amplicons, to further evaluate the association between preconditioning OM and transplant outcomes, we analyzed whether any non-core genus (those present in 25–75% of samples) was associated with a higher risk of relapse. In this exploratory analysis (without adjustment for multiple comparisons), of the 18 genera that matched the selection criteria tested in a univariate analysis for relapse (Fig. 4A, Fig. S6), only Solobacterium was significantly associated with lower relapse risk (9% versus 56%, respectively; HR 0.23, 95% CI 0.05–0.94, P = 0.04; Fig. 4B), and this association remained significant after adjusting for DRI (HR 0.20, 95% CI 0.06–0.67, P = 0.01; Fig. 4C). However, after adjusting for multiple comparisons using the Bonferroni correction, because of the limited statistical power of this study, the univariate association between Solobacterium presence and lower relapse risk lost significance (P = 0.72). The relative abundance of Solobacterium at preconditioning per patient is depicted in Fig. S7. No differences in the presence of Solobacterium were found in other outcomes (aGVHD at 100 days: 64% versus 44%, respectively [HR 1.84, 95% CI 0.68–4.95, P = 0.23]; cGVHD: 27% versus 13%, respectively [HR 2.41, 95% CI 0.43–13.4, P = 0.31]; PFS: 55% versus 37%, respectively [HR 0.83, 95% CI 0.31–0.83, P = 0.71]; and OS at 3 years: 55% versus 28%, respectively [HR 0.99, 95% CI 0.32–3.08, P = 0.99]).
Solobacterium absence at preconditioning was associated with an increased risk of relapse in patients who underwent allo-HSCT. (A) Volcano plot for the univariate competing risk analysis of the association of relapse with the presence of specific genera at preconditioning (P value versus hazard ratio). The Solobacterium data point is indicated as it was the only genus significantly associated with relapse (P < 0.05). (B) Cumulative incidence of relapse with patients (n = 27) stratified by Solobacterium presence. (C) The DRI-adjusted hazard ratio for the association of Solobacterium presence at preconditioning and relapse (n = 27).
Antibiotic use
From one week before until the first day of the conditioning regimen, 4 (13%) patients received antibiotics. From the first day of the conditioning regimen until engraftment, 28 (93%) patients received antibiotics: 20 (67%) used cefepime, 16 (53%) meropenem, 14 (47%) vancomycin, and four (13%) piperacillin-tazobactam. The use of these antibiotics were not associated with the risk of relapse (Fig. S5). We could not analyze the association between the use of antibiotics before transplant (30 days before starting the conditioning regimen) and OM bacterial diversity because of the small number of patients who used antibiotics at that time point.
Discussion
In this single-center observational study, we prospectively collected samples from the oral mucosa of patients who underwent allo-HSCT. To the best of our knowledge, this is the first study to evaluate the possible impact of the OM using ASVs on allo-HSCT outcomes. ASVs, which are read sequences denoised to single-nucleotide resolution, is a more reproducible and comprehensive technique with higher sensitivity and specificity than operational taxonomic units (OTU) in analyzing microbiota44,45,46. The OTU can identify bacteria at the genus level, while ASVs allow to distinguish bacteria at the species level, which could explain discrepancies between our findings when compared to previous studies.
We observed that patients who presented low OM diversity or dominance of any genus before conditioning had a significantly increased risk of relapse. The dominance of any genus was also associated with worse PFS and OS. Although a low oral microbiota diversity and the dominance of any genus are proxies for microbiota dysbiosis, the former was not associated with worse PFS and OS. Only 7 (25%) patients share the binomial: low OM diversity and dominance of any genus, or high OM diversity and absence of dominance. The dominance of a single genus may denote a deeper immune imbalance and could represent a more sensitive predictor of alloHSCT outcomes when compared with OM diversity.
The OM has different niches in the same environment and is as diverse as the IM. Previous studies evaluating OM and allo-HSCT have shown conflicting results, likely because of the use of low-resolution techniques for microbiota analysis and the small sample sizes. In one case series, there were no changes in OM after allo-HSCT. The most common oral organisms, e.g., Streptococcus, Gemella, and Veillonella, remained relatively stable after transplant34. However, another study showed a reduction in alpha diversity after allo-HSCT when compared with the pretransplant OM35, and this reduction was more pronounced in patients who developed oral mucositis47. Besides, we did not find any direct correlation between the use of antibiotics after conditioning and transplant outcomes, as other studies have shown for IM diversity23,24.
Recently, IM has attracted attention as a potential predictive marker for allo-HSCT outcomes. Previous studies have shown that low IM diversity is associated with a higher risk of mortality, but not with the risk of relapse25,26,27, diverging from our findings.
Higher risk of aGVHD in patients with low IM diversity48 and a higher risk of transplant-related mortality attributable to GVHD26 were also reported. In the oral mucosa samples analyzed in the current study, low OM diversity was associated with an increased risk of relapse but did not change the risk of mortality, aGVHD or cGVHD.
The dominance of a specific bacterial group in IM, Eubacterium limosum, has also been shown to be related to relapse and disease progression. In our series, the dominance of any genus was associated with a higher risk of relapse.
As opposed to what has been observed for IM27, all dominant genera at preconditioning reported herein are commensal organisms. Thus, it is unlikely that they all have detrimental roles in the allo-HSCT setting, being more plausible that the presence of dominance by any genus is a proxy for low diversity/dysbiotic OM.
Furthermore, the presence of Solobacterium in the OM before conditioning seems to have a protective effect against relapse. S. moorei, the only species in the Solobacterium genus, is normally associated with halitosis49,50 and endodontic infection51,52. However, in the allo-HSCT scenario, the lack of Solobacterium could be a marker of dysbiosis, pretransplant disease status, or previous treatments. Alternatively, this genus may also play a role as an immune mediator by producing hydrogen sulfide49, a metabolite associated with decreased oxidative stress and increased sensitivity to antibiotics53. Although, the low overall Solobacterium relative abundance even in patients where it was present makes the latter alternative more unlikely, this finding need to be validated in future studies.
A previous study analyzed the tongue microbiota in patients who underwent alloHSCT and compared it with community-dwelling adults. AlloHSCT patients have a lower tongue microbiota alpha diversity when compared to community adults. Moreover, the presence of Staphylococcus haemolyticus or Ralstonia pickettii was associated with a higher risk of mortality. Nevertheless, no relationship was observed between alpha diversity of the tongue microbiota and incidence of transplant complications46. A study of salivary microbiota showed a reduction in alpha diversity during the course of transplantation. Again, no correlation between salivary microbiota diversity and alloHSCT outcomes was found54. The discrepancies between these studies and our findings may be related to different sites of sample collections, and different distinct microbiome analysis techniques.
Our study had several limitations of a relatively small and heterogenous single-center transplant cohort. However, as observed in studies of IM, in our series, OM showed a significant correlation with relapse and may also provide valuable information on host-related microbial dysbiosis, providing a simple, reproducible technique for collection and analysis prior to transplantation.
In conclusion, in the current study, we focused on preconditioning samples in order to identify potential clinical effects of OM on allo-HSCT outcomes and observer that lower OM diversity was associated with a higher risk of relapse after allo-HSCT and dominance by a single genus was associated with a higher risk of relapse and worse survival after allo-HSCT.
Prospective trials and validation cohorts are needed to confirm these findings and to test whether early interventions to correct OM dysbiosis or more aggressive strategies to prevent relapse in OM dysbiotic patients, such as early immunosuppression withdrawal, maintenance therapy, or prophylactic donor lymphocyte infusions, could improve the predicted adverse outcome.
Abbreviations
- 95% Cis:
-
Ninety-five percent confidence intervals
- aGVHD:
-
Acute GVHD
- allo-HSCT:
-
Allogeneic stem cell transplantation
- ASVs:
-
Amplicon sequencing variants
- cGVHD:
-
Chronic GVHD
- DRI:
-
Disease risk index
- GVHD:
-
Graft versus host disease
- IM:
-
Intestinal microbiota
- NRM:
-
Non-relapse mortality
- OM:
-
Oral mucosa microbiota
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
References
Gyurkocza, B. & Sandmaier, B. M. Conditioning regimens for hematopoietic cell transplantation: One size does not fit all. Blood 124, 344–353 (2014).
Styczyński, J. et al. Death after hematopoietic stem cell transplantation: Changes over calendar year time, infections and associated factors. Bone Marrow Transplant. 55, 126–136 (2020).
Ossenkoppele, G. J., Janssen, J. J. W. M. & van de Loosdrecht, A. A. Risk factors for relapse after allogeneic transplantation in acute myeloid leukemia. Haematologica 101, 20–25 (2016).
Martino, R. et al. Comparison of conditioning regimens of various intensities for allogeneic hematopoietic SCT using HLA-identical sibling donors in AML and MDS with <10% BM blasts: A report from EBMT. Bone Marrow Transplant. 48, 761–770 (2013).
Bornhäuser, M. et al. Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: A prospective, open-label randomised phase 3 trial. Lancet Oncol. 13, 1035–1044 (2012).
Shen, Z. et al. Influence of pre-transplant minimal residual disease on prognosis after Allo-SCT for patients with acute lymphoblastic leukemia: Systematic review and meta-analysis. BMC Cancer 18, 1–12 (2018).
Rezvani, A. R. et al. Impact of donor age on outcome after allogeneic hematopoietic cell transplantation. Biol. Blood Marrow Transplant. 21, 105–112 (2015).
Bastida, J. M. et al. Influence of donor age in allogeneic stem cell transplant outcome in acute myeloid leukemia and myelodisplastic syndrome. Leuk. Res. 39, 828–834 (2015).
Milano, F. et al. Cord-blood transplantation in patients with minimal residual disease. N. Engl. J. Med. 375, 944–953 (2016).
Willemze, R. et al. KIR-ligand incompatibility in the graft-versus-host direction improves outcomes after umbilical cord blood transplantation for acute leukemia. Leukemia 23, 492–500 (2009).
Soiffer, R. J. et al. Prospective, randomized, double-blind, phase III clinical trial of anti-T-lymphocyte globulin to assess impact on chronic graft-versus-host disease-free survival in patients undergoing HLA-matched unrelated myeloablative hematopoietic cell transplantation. J. Clin. Oncol. 35, 4003–4011 (2017).
Walker, I. et al. Addition of anti-thymocyte globulin to standard graft-versus-host disease prophylaxis versus standard treatment alone in patients with haematological malignancies undergoing transplantation from unrelated donors: Final analysis of a randomised, open-label. Lancet Haematol. 7, e100–e111 (2020).
Nykolyszyn, C. et al. Posttransplantation cyclophosphamide vs antithymocyte globulin as GVHD prophylaxis for mismatched unrelated hematopoietic stem cell transplantation. Bone Marrow Transplant. 55, 349–355 (2020).
Signori, A. et al. Chronic GVHD is associated with inferior relapse risk irrespective of stem cell source among patients receiving transplantation from unrelated donors. Bone Marrow Transplant. 47, 1474–1478 (2012).
Tanaka, Y. et al. Analysis of non-relapse mortality and causes of death over 15 years following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 51, 553–559 (2016).
Armand, P. et al. Validation and refinement of the disease risk index for allogeneic stem cell transplantation. Blood 123, 3664–3671 (2014).
Belkaid, Y. & Hand, T. W. Role of the microbiota in immunity and inflammation. Cell 157, 121–141 (2014).
Zitvogel, L. et al. Cancer and the gut microbiota: An unexpected link. Sci. Transl. Med. 7, 271 (2015).
Vetizou, M. et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science 350, 1079–1084 (2015).
Holler, E. et al. Metagenomic analysis of the stool microbiome in patients receiving allogeneic stem cell transplantation: Loss of diversity is associated with use of systemic antibiotics and more pronounced in gastrointestinal graft-versus-host disease. Biol. Blood Marrow Transplant. 20, 640–645 (2014).
Mathewson, N. D. et al. Gut microbiome-derived metabolites modulate intestinal epithelial cell damage and mitigate graft-versus-host disease. Nat. Immunol. 17, 505–513 (2016).
Eriguchi, Y. et al. Graft-versus-host disease disrupts intestinal microbial ecology by inhibiting Paneth cell production of α-defensins. Blood 120, 223–231 (2012).
Jenq, R. R. et al. Intestinal blautia is associated with reduced death from graft-versus-host disease. Biol. Blood Marrow Transplant. 21, 1373–1383 (2015).
Shono, Y. et al. Increased GVHD-related mortality with broad-spectrum antibiotic use after allogeneic hematopoietic stem cell transplantation in human patients and mice. Sci. Transl. Med. 8, 339 (2016).
Taur, Y. et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood 124, 1174–1182 (2014).
Peled, J. U. et al. Microbiota as predictor of mortality in allogeneic hematopoietic-cell transplantation. N. Engl. J. Med. 382, 822–834 (2020).
Peled, J. U. et al. Intestinal microbiota and relapse after hematopoietic-cell transplantation. J. Clin. Oncol. 35, 1650–1659 (2017).
Shono, Y. & Van Den Brink, M. R. M. Gut microbiota injury in allogeneic haematopoietic stem cell transplantation. Nat. Rev. Cancer 18, 283–295 (2018).
Idris, A., Hasnain, S. Z., Huat, L. Z. & Koh, D. Human diseases, immunity and the oral microbiota—Insights gained from metagenomic studies. Oral Sci. Int. 14, 27–32 (2017).
Mascitti, M. et al. Beyond head and neck cancer: The relationship between oral microbiota and tumour development in distant organs. Front. Cell Infect. Microbiol. https://doi.org/10.3389/fcimb.2019.00232 (2019).
Zhao, H. et al. Variations in oral microbiota associated with oral cancer. Sci. Rep. 7, 11773 (2017).
Zhang, Y., Niu, Q., Fan, W., Huang, F. & He, H. Oral microbiota and gastrointestinal cancer. Onco Targets Ther. 12, 4721–4728 (2019).
Wang, Y. et al. Oral microbiota distinguishes acute lymphoblastic leukemia pediatric hosts from healthy populations. PLoS ONE 9, e102116 (2014).
Ames, N. J. et al. A characterization of the oral microbiome in allogeneic stem cell transplant patients. PLoS ONE. https://doi.org/10.1371/journal.pone.0047628 (2012).
Ames, N. J. et al. The oral microbiome of patients undergoing treatment for severe aplastic anemia: A pilot study. Ann. Hematol. 98, 1351–1365 (2019).
Klindworth, A. et al. Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res. 41, e1 (2013).
Wang, H. et al. Breast tissue, oral and urinary microbiomes in breast cancer. Oncotarget 8, 88122. https://doi.org/10.18632/oncotarget.21490 (2017).
Bolyen, E. et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 37, 852–857 (2019).
Edgar, R. C. & Flyvbjerg, H. Error filtering, pair assembly and error correction for next-generation sequencing reads. Bioinformatics 31, 3476–3482 (2015).
Callahan, B. J. et al. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods 13, 581–583 (2016).
Quast, C. et al. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 41, D590–D596 (2012).
Edgar, R. C., Haas, B. J., Clemente, J. C., Quince, C. & Knight, R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics 27, 2194–2200 (2011).
Rognes, T., Flouri, T., Nichols, B., Quince, C. & Mahé, F. VSEARCH: A versatile open source tool for metagenomics. PeerJ 4, e2584 (2016).
Edgar, R. C. UPARSE: Highly accurate OTU sequences from microbial amplicon reads. Nat. Methods 10, 996–998 (2013).
Callahan, B. J., McMurdie, P. J. & Holmes, S. P. Exact sequence variants should replace operational taxonomic units in marker-gene data analysis. ISME J. 11, 2639–2643 (2017).
Oku, S. et al. Disrupted tongue microbiota and detection of nonindigenous bacteria on the day of allogeneic hematopoietic stem cell transplantation. PLoS Pathog. 16, e1008348 (2020).
Shouval, R. et al. Salivary microbial and metabolic determinants of oral mucositis in recipients of allogeneic hematopoietic stem cell transplantation. Biol. Blood Marrow Transplant. 26, S50 (2020).
Golob, J. L. et al. Stool microbiota at neutrophil recovery is predictive for severe acute graft vs host disease after hematopoietic cell transplantation. Clin. Infect. Dis. 65, 1984–1991 (2017).
Haraszthy, V. I. et al. Characterization and prevalence of Solobacterium moorei associated with oral halitosis. J. Breath Res. 2, 017002 (2008).
Vancauwenberghe, F. et al. The role of Solobacterium moorei in oral malodour. J. Breath Res. 7, 046006 (2013).
Rolph, H. J. et al. Molecular identification of microorganisms from endodontic infections. J. Clin. Microbiol. 39, 3282–3289 (2001).
Rôças, I. N., Hülsmann, M. & Siqueira, J. F. Microorganisms in root canal-treated teeth from a German population. J. Endod. 34, 926–931 (2008).
Yang, R., Yu, T., Liu, D., Shi, S. & Zhou, Y. Hydrogen sulfide promotes immunomodulation of gingiva-derived mesenchymal stem cells via the Fas/FasL coupling pathway. Stem Cell Res. Ther. 9, 62 (2018).
Shouval, R. et al. Patterns of salivary microbiota injury and oral mucositis in recipients of allogeneic hematopoietic stem cell transplantation. Blood Adv. 4, 2912–2917 (2020).
Acknowledgements
We are grateful to all patients from Hospital Sírio Libanês, São Paulo, Brazil. We thank our colleagues from Hospital Sírio Libanês.
Funding
V.C.M. was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq process no. 141575/2018-2). J.S.B. was supported by Coordenação de Aperfeiçoamento de pessoal de Nível Superior (CAPES process no. 001). V.H. was supported by Fundação de Amapro à Pesquisa do Estado de São Paulo (FAPESP process no. 13996-0/2018).
Author information
Authors and Affiliations
Contributions
Conception and design: A.A.C., E.R.F. and C.A.-R. Collection and assembly of data: V.H., J.S.B., F.H.K., W.M.-S., P.F.A., V.C.d.M. and C.A.-R. Data analysis and interpretation: V.C.d.M., V.H., J.S.B., A.A.C., E.R.F. and C.A.-R. Manuscript writing: All authors. Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Molla, V.C., Heidrich, V., Bruno, J.S. et al. Disruption of the oral microbiota is associated with a higher risk of relapse after allogeneic hematopoietic stem cell transplantation. Sci Rep 11, 17552 (2021). https://doi.org/10.1038/s41598-021-96939-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96939-8
This article is cited by
-
Association between oral and fecal microbiome dysbiosis and treatment complications in pediatric patients undergoing allogeneic hematopoietic stem cell transplantation
Scientific Reports (2024)
-
Temporal variation in oral microbiome composition of patients undergoing autologous hematopoietic cell transplantation with keratinocyte growth factor
BMC Microbiology (2023)
-
Oral microbial changes and oral disease management before and after the treatment of hematological malignancies: a narrative review
Clinical Oral Investigations (2023)
-
Commensal oral microbiota impacts ulcerative oral mucositis clinical course in allogeneic stem cell transplant recipients
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.