Abstract
Bacterial endophthalmitis is a rare intraocular infection, and prompt administration of intravitreal antibiotics is crucial for preventing severe vision loss. The retrospective study is to investigate the in vitro susceptibility to the antibiotics vancomycin, amikacin, and ceftazidime of bacterial endophthalmitis isolates in specimens at a tertiary referral center from January 1996 to April 2019 in Taiwan. Overall, 450 (49.9%) isolates were Gram positive, 447 (49.6%) were Gram negative, and 4 (0.4%) were Gram variable. In Gram-positive isolates, coagulase-negative staphylococci were the most commonly cultured bacteria (158, 35.1%), followed by Streptococci (100, 22.2%), Enterococci (75, 16.7%), and Staphylococcus aureus (70, 15.6%). In Gram-negative isolates, they were Klebsiella pneumoniae (166, 37.1%) and Pseudomonas aeruginosa (131, 29.3%). All Gram-positive organisms were susceptible to vancomycin, with the exception of one Enterococcus faecium isolate (1/450, 0.2%). Of the Gram-negative isolates, 96.9% and 93.7% were susceptible to ceftazidime and amikacin, respectively. Nine isolates (9/447, 2.0%) were multidrug-resistant Gram-negative bacteria, comprising K. pneumoniae (4/164, 2.4%), Acinetobacter baumannii (2/3, 67%), and Stenotrophomonas maltophilia (3/18, 17%). In conclusion, in vitro susceptibility testing revealed that vancomycin remains the suitable antibiotic treatment for Gram-positive endophthalmitis. Ceftazidime and amikacin provide approximately the same degree of Gram-negative coverage. Multidrug-resistant bacterial endophthalmitis was uncommon.
Similar content being viewed by others
Introduction
Bacterial endophthalmitis is a rare intraocular infection that can occur following ocular surgery or trauma, as well as through the hematogenous spread of microorganisms from endogenous infection. Prompt administration of intravitreal antibiotics with or without pars plana vitrectomy is crucial for preventing severe vision loss. Both the bacterial spectrum and antibiotic susceptibility patterns in bacterial endophthalmitis isolates must be considered in the context of treatment. Vancomycin is a first-line drug for managing Gram-positive bacterial endophthalmitis, whereas ceftazidime or amikacin are typically used for Gram-negative coverage. Amid growing concern over the emergence of multidrug-resistant (MDR) bacteria, selecting antibiotics for infection treatment has become a critical issue. Common MDR organisms include (1) vancomycin-resistant enterococci; (2) methicillin-resistant S. aureus; (3) extended-spectrum β-lactamase (ESBL)-producing Gram-negative bacteria; (4) carbapenemase-producing K. pneumoniae; and (5) MDR Gram-negative bacteria, such as K. pneumoniae, Enterobacter spp., Escherichia coli, A. baumannii, P. aeruginosa, and S. maltophilia. This group of Gram-positive and Gram-negative bacteria has been named the ESKAPE group (E. faecium, S. aureus, K. pneumoniae, A. baumannii, P. aeruginosa, and Enterobacter spp.)1. Studies have been conducted on MDR bacterial endophthalmitis2,3,4,5,6,7,8. Although most isolates causing ocular infection are not caused by MDR bacteria, antibiotic susceptibility testing may reveal trends in antimicrobial susceptibility and resistance.
This study investigated the in vitro susceptibility of Gram-positive and Gram-negative bacterial endophthalmitis isolates collected over 23 years to vancomycin, ceftazidime, and amikacin. MDR pathogens were also examined.
Methods
The protocol of this retrospective, noncomparative laboratory case series was approved by the Institutional Review Board (IRB number: 201900614B0C601, 10 Aug 2019) of Chang Gung Memorial Hospital in Taiwan, and the requirement for written informed consent from the patients from whom the specimens were collected was waived. All clinical procedures were conducted according to the principles of the Declaration of Helsinki. The microbiological data of bacterial cultures isolated from culture-confirmed bacterial endophthalmitis at the Department of Microbiology of the participating hospital between January 1996 and April 2019 were reviewed. To protect the patients’ privacy, the data were deidentified. Data on clinical presentations and visual outcomes were not part of the laboratory records.
The bacterial isolates are from intraocular samples (anterior chamber, vitreous, and/or vitrectomy specimens). All microbiology investigations were performed at Microbiology Department, Chang Gung Memorial Hospital, Taoyuan, Taiwan. Bacterial culture isolates were identified by conventional microbiological methods (January 1996 to December 2013) and matrix-assisted laser desorption/ionization time of flight mass spectrometry (MALDI-TOF-MS) (January 2014 to April 2019). Conventional microbiological methods included Gram-staining and biochemical tests. In MALDI-TOF-MS, automatic measurement of the spectrum and comparative analysis with reference spectra of bacteria were performed using an Ultraflextreme mass spectrometer and MALDI-Biotyper 3.0 software (Bruker Daltonics). The reliability of identification in the MALDI Biotyper system was expressed in points. A log(score) ≥ 2.0 indicated identification to the species level. The isolates were tested for susceptibility to various antibiotics using the Kirby Bauer Disk diffusion method on Mueller Hinton blood agar. The Clinical and Laboratory Standards Institute (Wayne, PA) standards were used for interpretation and quality control for each corresponding year9. In vitro susceptibility of cultured bacterial organisms, the tested antibiotics mostly included either vancomycin for Gram-positive bacteria or ceftazidime and amikacin for Gram-negative bacteria. All data from the antibiotic susceptibility testing were further reviewed in the Gram-positive bacterial isolates resistant to vancomycin and in the Gram-negative bacteria resistant to either ceftazidime or amikacin. To be considered MDR, organisms must be resistant to antimicrobial drugs of three or more classes. Although methicillin-resistant S. aureus (MRSA) was susceptible to vancomycin, MRSA was not defined as an MDR organism in this study.
Results
A total of 901 bacterial endophthalmitis isolates were cultured over the 23-year study period. An overview of the isolates is provided in Table 1.
Organismal spectrum
Overall, 450 (49.9%) of isolates were Gram positive, 447 (49.6%) were Gram negative, and 4 (0.4%) were Gram variable. In the 450 Gram-positive isolates, coagulase-negative staphylococci (CoNS) were the most commonly cultured bacterial organisms (158, 35.1%), followed by streptococci (100, 22.2%), enterococci (75, 16.7%), and S. aureus (70, 15.6%). In the 447 Gram-negative isolates, they were K. pneumoniae (166, 37.1%) and P. aeruginosa (131, 29.3%).
Susceptibility of Gram-positive isolates to vancomycin
Table 2 presents the susceptibility of the Gram-positive isolates to vancomycin. All Gram-positive bacteria, with the exception of one E. faecium isolate, were susceptible to vancomycin, including CoNS, S. aureus, Enterococcus faecalis, and streptococci (Table 2).
Susceptibility of Gram-negative isolates to amikacin and ceftazidime
Table 3 presents the susceptibility of the Gram-negative isolates to amikacin and ceftazidime. Overall, 96.9% (413/426) were susceptible to ceftazidime and 93.7% (401/428) were susceptible to amikacin. Regarding the most commonly isolated Gram-negative organisms, 98% of the K. pneumoniae isolates were susceptible to both ceftazidime and amikacin. Of the P. aeruginosa isolates, 98% and 95% were susceptible to ceftazidime and amikacin, respectively. Of the S. maltophilia isolates, 8% and 46% were susceptible to ceftazidime and amikacin, respectively. All the Haemophilus influenzae, Serratia marcescens, Enterobacter spp., Citrobacter spp., and E. coli isolates were susceptible to ceftazidime and amikacin. Among them, MDR Gram-negative bacteria comprised K. pneumoniae (4/164, 2.4%), A. baumannii (2/3, 67%), and S. maltophilia (3/18, 17%). The S. maltophilia isolates exhibited high resistance to ceftazidime (11/12, 94%) and amikacin (7/13, 54%).
Susceptibility of Gram-variable isolates
Two Mycobacterium chelonae, one Mycobacterium abscessus, and one Nocardia spp. isolate comprised the Gram-variable isolates. Three Mycobacterium isolates were susceptible to amikacin but were not tested for susceptibility to ceftazidime. The Nocardia spp. isolate was not tested for susceptibility to amikacin and ceftazidime.
MDR organisms
Ten isolates (10/901, 1.1%), including one E. faecium, four K. pneumoniae, two A. baumannii, and three S. maltophilia, were MDR organisms. Table 4 shows the antibiotic susceptibility testing results for multidrug resistance. The E. faecium isolate was susceptible to linezolid and tigecycline but resistant to teicoplanin. ESBL production was detected in the four K. pneumoniae isolates, of which only one was susceptible to amikacin. All four isolates were susceptible to carbapenems (imipenem, meropenem, or ertapenem). One of the A. baumannii isolates was susceptible to imipenem. The other was resistant to meropenem but susceptible to colistin and tigecycline. All three MDR S. maltophilia isolates were susceptible to amikacin but resistant to ceftazidime, trimethoprim-sulfamethoxazole, and fluoroquinolones, including levofloxacin and moxifloxacin.
Discussion
Understanding of the various organisms causing bacterial endophthalmitis is critical to the development of effective treatments. Case studies on bacterial endophthalmitis have reported variability in the microbiological spectrum of causative pathogens according to the types of endophthalmitis and to the regions and countries where the studies were conducted. Bacterial endophthalmitis is caused by Gram-positive and Gram-negative organisms, as well as some Gram-variable organisms. Empirically supported antibiotic treatments for infectious endophthalmitis are developed on the basis of likely causative organisms and their susceptibility patterns. In this study, the proportions of Gram-positive and Gram-negative bacteria (49.9% and 49.6%, respectively) were approximately equal, with Gram-variable bacteria accounting for a considerably lower proportion (0.4%). Exogenous bacterial endophthalmitis mostly arises form Gram-positives because Gram-negatives are not common on the eyelid margins. This is partially attributable to the large number of reported cases of endogenous K. pneumoniae endophthalmitis and P. aeruginosa keratitis-related endophthalmitis in Taiwan4,6,10,11,12. Our data differ from those of other published reviews of endophthalmitis isolates (Table 5)13,14,15,16,17,18,19. Gram-positive bacteria account for most bacterial isolates of endophthalmitis in studies conducted in the United States, Canada, and Austria, whereas Gram-negative bacteria are predominant in India13,14,15,16,17,18,19. The higher proportion of Gram-negative isolates observed in one study17 from India may be explained by trauma and environmental factors. In this study, 1.1% (10/901) of the MDR bacterial isolates included one Gram-positive and nine Gram-negative bacterial organisms.
As mentioned, the most commonly cultured Gram-positive isolates were CoNS, followed by Streptococcus spp., Enterococcus spp., and S. aureus. These results are consistent with those from previous studies13,14,15,16,17. However, a higher proportion of Enterococcus spp., especially E. faecalis, was noted in this study, and it resulted from more E. faecalis endophthalmitis cases in Taiwan20,21. Gram-positive vancomycin-resistant endophthalmitis has become a critical clinical issue worldwide; this is indicated by the fact that Enterococcus spp. and Staphylococcus spp. were the most commonly reported organisms7. The rate of Gram-positive vancomycin resistance in the present study was 0.2%. All Staphylococcus spp. isolates were susceptible to vancomycin, but 1 of the 75 (1.3%) Enterococcus isolates, E. faecium, was resistant to vancomycin. Several case reports have examined vancomycin-resistant enterococcal endophthalmitis22,23,24. E. faecalis was less commonly resistant to vancomycin. In other case reports of endophthalmitis, E. casseliflavus25 and E. faecium2 exhibited higher rates of resistance to vancomycin. In a literature review7 of 27 types of vancomycin-resistant Gram-positive bacteria, Enterococcus spp., CoNS, S. aureus, and Bacillus spp. were the most common organisms.
In this study, 3.1% and 6.3% of the Gram-negative bacteria was resistant to ceftazidime and amikacin, respectively. In these resistant isolates, most Gram-negative bacteria were resistant to either ceftazidime or amikacin. However, five isolates (5/447, 1.1%) were resistant to both ceftazidime and amikacin. Apart from four K. pneumoniae isolates, most bacteria in the Enterobacteriaces family were susceptible to amikacin and ceftazidime. By comparison, nonfermenting Gram-negative bacteria not belonging to the Enterobacteriaces family were more likely to be resistant to ceftazidime and amikacin. P. aeruginosa had a comparable degree of susceptibility to ceftazidime (98%) and amikacin (95%). By contrast, the susceptibility of S. maltophilia to ceftazidime and amikacin differed substantially (8% and 46%, respectively).
Among the MDR bacteria, E. faecium was susceptible to linezolid and tigecycline. The nine MDR Gram-negative bacterial isolates comprised K. pneumoniae (4/164, 2.4%), A. baumannii (2/3, 67%), and S. maltophilia (3/18, 17%). The ceftazidime resistance of K. pneumoniae, a member of the Enterobacteriaceae family, was indicated by the presence of ESBL production. The ESBL-producing Gram-negative bacteria were resistant to all third-generation cephalosporins. Four MDR K. pneumoniae isolates were susceptible to carbapenems (imipenem, meropenem, or ertapenem). One of the A. baumannii isolates was susceptible to carbapenem, and the other was susceptible to colistin and tigecycline. All three MDR S. maltophilia isolates were susceptible to amikacin but resistant to ceftazidime, trimethoprim-sulfamethoxazole, and fluoroquinolones, including levofloxacin and moxifloxacin. In a case report of carbapenemase-producing K. pneumoniae endophthalmitis by Zhou et al.8, the K. pneumoniae isolate was resistant to amikacin, ceftazidime, and carbapenems but susceptible to polymyxin E and tigecycline. Roy et al.26 noted that four (100%) A. baumannii isolates were resistant to ceftazidime and one (25%) was resistant to amikacin. All four of those A. baumannii isolates were susceptible to ciprofloxacin26. Although S. maltophilia was typically susceptible to trimethoprim-sulfamethoxazole, levofloxacin, and moxifloxacin, Ji et al.5 reported on 14 patients with MDR S. maltophilia postcataract endophthalmitis. All eight S. maltophilia isolates were resistant to amikacin, imipenem, and ciprofloxacin but not to levofloxacin5. Five isolates were resistant to ceftazidime5.
Most bacteria are typically susceptible to vancomycin, ceftazidime, and amikacin at a concentration of ≤ 10 μg/mL. Interpretive standards for dilution susceptibility testing from the US Clinical and Laboratory Standards Institute indicate that the minimal inhibitory concentrations of vancomycin, ceftazidime, and amikacin are ≤ 4, ≤ 8, and ≤ 6 μg/mL, respectively27. The resistance concentrations of vancomycin, ceftazidime, and amikacin are ≥ 32, ≥ 32, and ≥ 64 μg/mL, respectively27. Intravitreal antibiotic injection is the principal treatment for infectious endophthalmitis. The susceptibility standards are based on serum standards used for systemic therapy from the Clinical and Laboratory Standards Institute. However, there are no standards for intravitreal therapy, and resistance is probably over-reported using the serum standards. In vitro resistance patterns may not be identical with in vivo susceptibility, and routinely administered intravitreal antibiotics typically deliver intraocular antibiotic concentrations that are considerably higher than the minimal inhibitory concentrations of most organisms. When patients’ conditions do not stabilize or improve after initial intravitreal antibiotic injection, additional injections of alternative antibiotics should be considered according to results in vitro susceptibility testing.
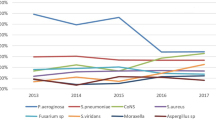
This study has some limitations. First, this was a single-center retrospective case series. Second, some Gram-negative isolates were not routinely tested at our hospital for susceptibility to amikacin and ceftazidime. Third, we did not retrieve accurate, detailed information on various types of endophthalmitis and visual outcomes, which may interest readers. Fourth, we did not analyze trends in the patterns of antibiotic susceptibility given the relatively small number of annual cases. Finally, we did not further analyze the MDR bacteria for specific resistance genes. Nevertheless, our findings contribute to the literature in providing a thorough analysis of the antimicrobial susceptibility of bacterial isolates from all patients diagnosed as having bacterial endophthalmitis over 23 years at a tertiary medical center.
In conclusion, the most commonly detected organisms in the Gram-positive and Gram-negative bacteria were CoNS and K. pneumoniae, respectively. MDR bacterial endophthalmitis was not common. Vancomycin remains the antibiotic of choice for the treatment of Gram-positive endophthalmitis. Amikacin and ceftazidime appear to provide approximately equal Gram-negative coverage.
References
Boucher, H. W. et al. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 48, 1–12. https://doi.org/10.1086/595011 (2009).
Bains, H. S., Weinberg, D. V., Feder, R. S. & Noskin, G. A. Postoperative vancomycin-resistant Enterococcus faecium endophthalmitis. Arch. Ophthalmol. (Chicago Ill. 1960) 125, 1292–1293. https://doi.org/10.1001/archopht.125.9.1292 (2007).
Chen, K. J. et al. Endophthalmitis caused by Acinetobacter baumannii: Report of two cases. J. Clin. Microbiol. 46, 1148–1150. https://doi.org/10.1128/jcm.01604-07 (2008).
Chen, K. J. et al. Endogenous Klebsiella endophthalmitis associated with Klebsiella pneumoniae pneumonia. Ocul. Immunol. Inflamm. 17, 153–159. https://doi.org/10.1080/09273940902752250 (2009).
Ji, Y. et al. Post-cataract endophthalmitis caused by multidrug-resistant Stenotrophomonas maltophilia: Clinical features and risk factors. BMC Ophthalmol. 15, 14. https://doi.org/10.1186/1471-2415-15-14 (2015).
Li, Y. H. et al. Infectious sources, prognostic factors, and visual outcomes of endogenous Klebsiella pneumoniae endophthalmitis. Ophthalmol. Retina 2, 771–778. https://doi.org/10.1016/j.oret.2017.11.013 (2018).
Relhan, N. et al. Endophthalmitis caused by Gram-positive organisms with reduced vancomycin susceptibility: Literature review and options for treatment. Br. J. Ophthalmol. 100, 446–452. https://doi.org/10.1136/bjophthalmol-2015-307722 (2016).
Zhou, Y., Wang, X., Shen, J., Lu, Z. & Liu, Y. Endogenous Endophthalmitis caused by Carbapenem-resistant Hypervirulent Klebsiella Pneumoniae: A case report and literature review. Ocul. Immunol. Inflamm. 27, 1099–1104. https://doi.org/10.1080/09273948.2018.1502786 (2019).
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard, 12th edn. M02-A13. (Clinical and Laboratory Standards Institute).
Chen, Y. H. et al. Prognostic factors and visual outcomes of pyogenic liver abscess-related endogenous Klebsiella pneumoniae endophthalmitis: A 20-year retrospective review. Sci. Rep. 9, 1071. https://doi.org/10.1038/s41598-018-37643-y (2019).
Chen, K. J. et al. Endophthalmitis caused by Pseudomonas aeruginosa in Taiwan. Retina (Phila. Pa.) 31, 1193–1198. https://doi.org/10.1097/IAE.0b013e3181fbce5c (2011).
Chen, K. J., Wu, W. C., Sun, M. H., Lai, C. C. & Chen, T. L. Pseudomonas endophthalmitis. Ophthalmology 117, 1657–1658. https://doi.org/10.1016/j.ophtha.2010.04.011 (2010) (author reply 1658–1659).
Gentile, R. C. et al. Microbiological spectrum and antibiotic sensitivity in endophthalmitis: A 25-year review. Ophthalmology 121, 1634–1642. https://doi.org/10.1016/j.ophtha.2014.02.001 (2014).
Reddy, A. K. et al. Susceptibility of bacterial isolates to vancomycin and ceftazidime from patients with endophthalmitis: Is there a need to change the empirical therapy in suspected bacterial endophthalmitis?. Int. Ophthalmol. 35, 37–42. https://doi.org/10.1007/s10792-014-0015-9 (2015).
Schimel, A. M., Miller, D. & Flynn, H. W. Jr. Endophthalmitis isolates and antibiotic susceptibilities: A 10-year review of culture-proven cases. Am. J. Ophthalmol. 156, 50-52.e51. https://doi.org/10.1016/j.ajo.2013.01.027 (2013).
Moloney, T. P. & Park, J. Microbiological isolates and antibiotic sensitivities in culture-proven endophthalmitis: A 15-year review. Br. J. Ophthalmol. 98, 1492–1497. https://doi.org/10.1136/bjophthalmol-2014-305030 (2014).
Joseph, J. et al. Trends in microbiological spectrum of endophthalmitis at a single tertiary care ophthalmic hospital in India: A review of 25 years. Eye (Lond.) 33, 1090–1095. https://doi.org/10.1038/s41433-019-0380-8 (2019).
Assaad, D. et al. Bacterial endophthalmitis: 10-year review of the culture and sensitivity patterns of bacterial isolates. Can. J. Ophthalmol. J. Can. D’ophtalmol. 50, 433–437. https://doi.org/10.1016/j.jcjo.2015.07.013 (2015).
Kodati, S., Eller, A. W. & Kowalski, R. P. The susceptibility of bacterial endophthalmitis isolates to vancomycin, ceftazidime, and amikacin: A 23 year-review. Ophthalmol. Retina 1, 206–209. https://doi.org/10.1016/j.oret.2016.11.010 (2017).
Chen, K. J. et al. Postcataract endophthalmitis caused by Enterococcus faecalis. Ocul. Immunol. Inflamm. 17, 364–369. https://doi.org/10.3109/09273940903105110 (2009).
Chen, K. J. et al. Enterococcus faecalis endophthalmitis: Clinical settings, antibiotic susceptibility, and management outcomes. Microorganisms https://doi.org/10.3390/microorganisms9050918 (2021).
Dave, V. P. et al. Enterococcus endophthalmitis: Clinical settings, antimicrobial susceptibility, and management outcomes. Retina (Phila. Pa.) 40, 898–902. https://doi.org/10.1097/iae.0000000000002462 (2020).
Rishi, E., Rishi, P., Nandi, K., Shroff, D. & Therese, K. L. Endophthalmitis caused by Enterococcus faecalis: A case series. Retina (Phila. Pa.) 29, 214–217. https://doi.org/10.1097/IAE.0b013e31818eccc7 (2009).
Tang, C. W., Cheng, C. K. & Lee, T. S. Community-acquired bleb-related endophthalmitis caused by vancomycin-resistant enterococci. Can. J. Ophthalmol. J. Can. D’ophtalmol. 42, 477–478 (2007).
Low, J. R., Teoh, C. S., Chien, J. M. & Huang, E. H. Enterococcus casseliflavus endophthalmitis due to metallic intraocular foreign body. Eye (Lond.) 29, 840–841. https://doi.org/10.1038/eye.2014.332 (2015).
Roy, R. et al. Endophthalmitis caused by Acinetobacter baumanni: A case series. Eye (Lond.) 27, 450–452. https://doi.org/10.1038/eye.2012.277 (2013).
Performance Standards for Antimicrobial Susceptibility Testing. Clinical and Laboratory Standards Institute (CLSI). M100 28th edition (2018).
Acknowledgements
The authors wish to acknowledge the support of the Taiwan Ministry of Science and Technology MOST 106-2314-B-182A-041, and Chang Gung Memorial Hospital CMRPG3F1243.
Author information
Authors and Affiliations
Contributions
K.-J.C. designed the study, performed statistical analysis, wrote the manuscript, and approved the final manuscript for publication; M.-H.S. collected and analyzed the data; H.-C.H., H.-C.C., Y.-P.C., N.-K.W., L.L., W.-C.W., H.-D.C., E.Y.-C.K. and C.-C.L. all provided patients’ data and assisted in data collection. All authors have reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, KJ., Sun, MH., Hou, CH. et al. Susceptibility of bacterial endophthalmitis isolates to vancomycin, ceftazidime, and amikacin. Sci Rep 11, 15878 (2021). https://doi.org/10.1038/s41598-021-95458-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-95458-w
This article is cited by
-
Global mapping of antibiotic resistance rates among clinical isolates of Stenotrophomonas maltophilia: a systematic review and meta-analysis
Annals of Clinical Microbiology and Antimicrobials (2024)
-
Triple Gram-negative bacterial endophthalmitis following intravitreal injection
Journal of Ophthalmic Inflammation and Infection (2024)
-
Preventive factors, diagnosis, and management of injection-related endophthalmitis: a literature review
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.