Abstract
The vagal nervous system is central to the physiological responses and systemic diseases of the liver. We evaluated the subsequent risk of liver and intrahepatic cancer (HCC/ICC) in non-H. pylori (HP)-infected perforated peptic ulcer (PPU) patients with and without vagotomy. Hospitalized PPU patients who underwent simple closure or truncal vagotomy/pyloroplasty (TVP) in the National Health Insurance Research Database from 2000 to 2008 were enrolled. The exclusion criteria included: (1) Multiple surgeries for PPU were received at the same admission; (2) Any cancer history; (3) Previous peptic ulcer-associated surgery; (4) HP infection history; (5) Viral hepatitis infection history; (6) Follow-up duration < 1 year; and (7) Age < 18 years. The risks of developing HCC/ICC in PPU patients with and without vagotomy were assessed at the end of 2013. To balance the baseline condition between groups, we used the propensity score matched method to select study subjects. Cox proportional hazard regression was used to estimate the hazard ratio and 95% confidence interval (CI) of HCC/ICC. Before propensity score matching, 675 simple suture patients and 54 TVP patients had HCC/ICC, which corresponded to incidences of 2.11 and 0.88 per 1000 person-years, respectively. After propensity score matching, 145 simple suture patients and 54 TVP patients experienced HCC/ICC, which corresponded to incidences of 1.45 and 0.88 per 1000 person-years, respectively. The TVP patients had a 0.71 (95% CI 0.54–0.95)- and 0.69 (95% CI 0.49–0.97)-fold risk of developing HCC/ICC compared to simple suture patients before and after propensity score matching. Our findings reported that, in the Asian population, TVP decreases the risk of HCC/ICC in non-HP-infected PPU patients compared to simple closure patients. However, further studies are warranted.
Similar content being viewed by others
Introduction
Liver cancer is the fifth most common cancer and accounted for 9.1% of all cancer deaths worldwide in 20121; it became the fourth most common cause of cancer-related death worldwide in 20192. Most liver cancer cases are noted in low- and middle-resource countries, particularly in Eastern Asia, and remain an important global health issue2.
The majority of primary liver cancers (75–90%) are hepatocellular carcinomas (HCCs), which are malignant tumors of liver parenchymal cells. The other primary liver cancer is intrahepatic cholangiocarcinoma (ICC), a tumor of intrahepatic ductal lining cells3. Common risk factors for HCC include hepatitis B virus (HBV) and hepatitis C virus (HCV) infection, obesity, diabetes, fatty liver disease, aflatoxin, alcoholic cirrhosis, smoking, and iron overload4, while risk factors for ICC include chemical exposure, parasites, sclerosing cholangitis, viral hepatitis, and cirrhosis5.
On the other hand, the vagus nerve and the inflammatory reflex are essential for immunity and metabolic homeostasis6. Anatomically, the hepatic parasympathetic nerves branch off the vagus nerve and innervate the liver7,8. It has been reported that increased vagal parasympathetic tone is associated with peptic ulcer diseases in humans9,10 and related to gastric stress ulceration development in rodent studies11. In addition, studies have shown an association between the hepatic nervous system and clinical diseases, such as type 2 diabetes mellitus12,13, obesity14, and cirrhosis15.
We hypothesized that the severance of the vagus nerve (vagotomy) would deinnervate the liver, resulting in unstable hepatic homeostasis and increasing the risk of liver cancer (HCC/ICC). Because it is impractical to obtain experimental data on vagal nerve severance in humans, we found that non-H. pylori (HP)-infected perforated peptic ulcer (PPU) patients who underwent simple suture (i.e., integrated vagal nerve) or truncal vagotomy and pyloroplasty (TVP) (i.e., vagal nerve severance) could be used to study the association between the hepatic vagal system and liver cancer.
Method
Data source
We used an inpatient database that was a part of the Taiwan National Health Insurance Database (TNHIRD) for this retrospective cohort study. TNHIRD was established by the Taiwan National Health Insurance Administration Ministry of Health and Welfare and covers over 99% of residents in Taiwan. Inhabitants of Taiwan are obligated to join this health program. People can be lost to follow-up due to emigration, imprisonment, joining the army, or death. Because people might withdraw from this program, study subjects were followed up until the date of withdrawal or the end of 2013. The quality and accuracy of this database have been reported previously16,17,18. In addition, the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) was used to identify diseases and treatment procedures in TNHIRD. The inpatient database included all inpatient claims (containing disease diagnosis and surgery) of each insurant from 1996 to 2013. To comply with research ethics and the Personal Information Protection Act, all identifiers of insured people were shuffled and substituted with surrogate numbers for this research. This study was approved, and the need for informed consent was waived from all participants by the Research Ethics Committee of the China Medical University and Hospital in Taiwan [CMUH104-REC2-115 (CR-3)].
Study subjects
Patients with ulcer-associated surgery [including simple suture (ICD-9-CM 44.4) and truncal vagotomy/pyloroplasty (TVP, ICD-9-CM 44.01 and 44.4)] at ulcer admission (ICD-9-CM 531-533) were enrolled from 2000 to 2008. HP infection was reported to be involved in liver diseases and has a close relationship with hepatocellular carcinoma19,20,21,22. To avoid confounding effects, PPU patients with HP infection were excluded from this study. Therefore, the exclusion criteria included: 1. Multiple surgeries for PPU were received at the same admission; 2. Any cancer history; 3. Previous peptic ulcer-associated surgery included truncal vagotomy, suture, gastrectomy, and truncal/highly selective vagotomy; 4. HP infection history; 5. Viral hepatitis infection history; 6. Follow-up duration < one year for limiting the effect of reverse causation; and 7. Age < 18 years. As a result, there were two groups of patients: simple sutures and TVPs. To balance the baseline condition between the two groups, propensity score matching was used to select study subjects. The propensity score was estimated by logistic regression based on age, sex, ulcer admission-year, and baseline comorbidities (including diabetes, cirrhosis, hypertension, hyperlipidemia, and stroke). The matched ratio was 1:1 (Fig. 1). The propensity score matching method was based on a greedy algorithm. Matches were first made within a caliper width of 0.0000001, and the caliper width was then increased to 0.1 for unmatched cases.
Confounder assessment and outcome
For all study participants, information on comorbidities prior to the index date was obtained, and the following comorbidities were considered: diabetes, cirrhosis, hypertension, hyperlipidemia, and stroke. These comorbidities were considered because there is an increased risk of cancer in diabetes23, cirrhosis24, hypertension25, hyperlipidemia25, and stroke26. These comorbidities were evaluated in the comparisons and the study cohort. The anticipated outcome was liver cancer (HCC/ICC) development (ICD-9-CM 155).
Diagnosis and follow up of liver cancer
In addition to the ICD-9-CM system, cancer patients were diagnosed by specialists based on pathology and clinical reports and then entered into a registry system of “catastrophic illness patients” in Taiwan. Thus, HCC and ICC patients were identified from this “catastrophic illness patients” registry. All study subjects were followed from ulcer admission to the date of liver cancer development, the date of withdrawal from the database, or December 31, 2013, whichever came first.
Statistical analysis
The distribution of categorical variables (including sex, age group, and comorbidity) is presented as numbers and percentages, and the distribution of age is presented as the mean and standard deviation (SD). The standardized difference was used to test the differences in categorical variables and continuous variables between patients with simple sutures and TVPs. The variable with the value of standardized difference > 0.1 was considered a significant difference between two cohorts. The incidence of liver cancer was calculated between groups as the sum of liver cancer development divided by the sum of follow-up duration (person-years).
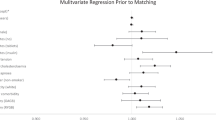
Cox proportional hazard regression was used to estimate the hazard ratio and 95% confidence interval (CI) of liver cancer, and the multivariable model was adjusted for age, sex, and all comorbidities (including diabetes, cirrhosis, hypertension, hyperlipidemia, and stroke). In propensity score-matched subjects, the Cox model was used after adjusting for matched pairs. Sex-, age-, and comorbidity-stratified analyses were also evaluated. Kaplan–Meier analysis was used to plot the cumulative incidence of liver cancer, and the log-rank test was used to test the differences between the two groups. All statistical tests were two-sided, and statistical significance was defined as a p-value < 0.05. All analyses were performed using SAS, version 9.4 (SAS Institute, Cary, North Carolina.). https://www.sas.com/zh_tw/home.html.
In addition, all study methods were carried out in accordance with relevant guidelines and regulations.
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee at China Medical University and Hospital. The need for informed consent was waived from all participants [CMUH104-REC2-115 (CR-3)]. To comply with research ethics and the Personal Information Protection Act, the identifications of all insured people were shuffled and replaced with surrogate numbers for research.
Result
Before propensity score matching
In total, 70,100 patients who underwent ulcer-associated surgery were enrolled. After exclusion, there were 43,439 ulcer patients with simple suture treatment (88.3%) and 5,744 ulcer patients with TVP treatment (11.7%). Compared to simple suture patients, the TVP group was younger (mean age 50.2 ± 16.6 vs. 60.9 ± 16.6 years old) and was more likely to be male (82.6% vs. 69.7%) (Table 1). Simple suture patients had more comorbidities than TVP patients, specifically hyperlipidemia (7.45% vs. 1.31%).
During follow-up, there were 675 simple suture patients, and 54 TVP patients had live cancer (Table 2). This corresponds to incidences of 2.11 and 0.88 per 1000 person-years, respectively. In the multivariable Cox model, TVP patients had a 0.71-fold higher risk of liver cancer than simple suture patients (95% CI 0.54–0.95). In the stratified analysis, except in the 20- to 44-year-old age group, TVP patients were more likely to have a lower risk of liver cancer than simple suture patients, but the difference was not significant. This may be due to few events in TVP patients. However, the cumulative incidence of liver cancer in TVP patients was lower than that in simple suture patients at the 14-year follow-up (1.64% vs. 2.99%, log-rank test p < 0.0001) (Fig. 2A).
After propensity score matching
There were 5737 simple suture patients and 5737 TVP patients enrolled. No significance in the distribution of age, sex, or comorbidities was noted (Table 1). During the follow-up duration, 145 simple suture patients and 54 TVP patients had liver cancer (Table 2). This corresponds to incidences of 1.45 and 0.88 per 1000 person-years, respectively. In the Cox model, TVP patients had a 0.69-fold higher risk of liver cancer than simple suture patients (95% CI 0.49–0.97). The cumulative incidence of liver cancer in TVP patients was lower than that in simple suture patients at the 14-year follow-up (1.64% vs. 2.02%, log-rank test p = 0.03) (Fig. 2b).
Discussion
At the first encounter, there was a decreased risk of developing liver cancer (HCC/ICC) in PPU patients who underwent TVP compared to those who underwent simple closure. After stratification by sex, age, and comorbidities, there were 71% and 69% decreased risks in the TVP cohort (i.e., vagal nerve severance) compared with the simple closure cohort (i.e., integrated vagal nerve) without and with propensity score matching, respectively (Table 2). These results indicate that there might be a protective effect of TVP on the risk of liver cancer development in non-HP-infected PPU patients.
The vagus nerve plays an important role in the regulation of inflammation and metabolic homeostasis27,28. Persistent vagal hyperactivity is associated with increased systemic inflammatory status and systemic diseases, such as peptic ulcers9,10,11. In addition, several cohort studies reported that peptic ulcer patients have higher incidences of inflammatory diseases, such as type 2 diabetes29, ischemic heart disease30, ischemic stroke31,32 and liver cirrhosis33. In the current series, we assume that the protective effect of TVP for decreased risk of liver cancer development in non-HP-infected PPU patients might be partly caused by the relief of persistent vagal hyperactivity.
One possible explanation for this result might be attributed to the role of hepatic stellate cells (HSCs) in the human liver. HSCs play an important role in liver development, regeneration and fibrotic change34,35; they are in the space of Disse between hepatic sinusoidal endothelial cells and epithelial cells, with a nucleus-to-nucleus distance of 40 µm36, producing contraction and relaxation of the hepatic sinusoidal walls37. Notably, the intrahepatic efferent nerves terminate at Disse’s space, close to HSCs and hepatocytes in humans38. This indicates an essential role of the vagus nerve in the activation of HSCs.
HSCs play an essential role in the development of liver cancer (HCC/ICC)39,40,41,42. In response to hepatic injury, quiescent HSCs are activated and undergo a mesenchymal-to-epithelial transition to transdifferentiate into hepatic progenitor cells (HPCs) and hepatocytes43. Under a permissive microenvironment, activated HSCs may contribute to HCC development40, which might occur through dysregulation of liver regeneration44. Activated HSCs may promote the process of fibrosis and transition into alpha-smooth muscle actin-expressing contractile myofibroblasts that result in increased vascular resistance and vascular distortion. Nonetheless, activated HSCs markedly express genes involved in fibrogenesis and fibrolysis, inflammation and apoptosis45.
Embryologically, hepatocytes and intrahepatic biliary ducts are both derived from hepatic diverticula that originate from the endoderm46, which indicates a close relationship between HCC and ICC. Moreover, data from ICC patients suggested that HSCs may be related to the progression of ICC and could be potential precursors to stromal myofibroblasts and promote the development of ICC47.
Numerous factors and signaling pathways are involved in the activation of HSCs, such as TGF-beta, platelet-derived growth factors (PDGF), hedgehog, Notch, and microRNAs40. However, the hepatic nervous system has been reported to modulate38 as well as activate HSCs during liver carcinogenesis47. The hepatic vagus nerve was reported to stimulate HSC proliferation via muscarinic receptor type 248 and stimulate activation of the HPC compartment via muscarinic acetylcholine receptor type 349. In addition, hepatic branch vagotomy may suppress liver regeneration in partially hepatectomized rats50,51. Together, the vagus nerve-mediated modulation of HSCs may play an important role in the development of HCC and ICC.
Persistent vagal hyperactivity is associated with systemic inflammation and immune paralysis52,53. In this study, PPU patients who underwent vagotomy had a lower hazard ratio of subsequent HCC and ICC than those who underwent simple suture (HR = 0.69, Table 2). It is likely that there was persistent vagal hyperactivity in PPU patients who underwent simple suture (i.e., integrated vagal nerve). Persistent vagal hyperactivity may stimulate HSC proliferation and activate HPC48,49, which promotes fibrosis and dysregulates liver regeneration, as well as lead to the progression of HCC and ICC44. It is plausible that vagotomy alleviates persistent vagal hyperactivity in PPU patients and results in a decreased incidence of HCC and ICC.
Concern exists whether such an association is direct or indirect. For instance, obesity is a common risk factor for peptic ulcers and nonalcoholic steatohepatitis54 and might be associated with the development of HCC55,56. Moreover, abdominal operation for PPU patients may have an impact on subsequent obesity development, indicating that such an association might only be an epiphenomenon of confounding factors (e.g., obesity). However, if surgery itself had an impact, the result should be similar either in the TVP or simple closure group. In the current study, there was a significant difference in subsequent HCC and ICC between the TVP and simple closure groups (Fig. 2).
To our knowledge, there have been no similar epidemiological studies focusing on this issue. Our results showed that non-HP-infected PPU patients receiving vagotomy were associated with a lower risk of developing HCC and ICC than those receiving simple sutures (Table 2). These results indicate that there might be a role for persistent vagal hyperactivity in the activation of HSCs and an increased risk of developing HCC and ICC. Although the mechanism is partly speculative, the clinical significance of this study may, in part, provide evidence for reappraisal of the current surgical treatment of non-HP-infected PPU patients. Further studies may focus on the role of the vagus nerve in diseases and the modulation of vagal hyperactivity.
Limitations of the study
Our study was strengthened by available data in a large population for longitudinal assessment and subgroup analysis of HCC and ICC in hospitalized non-HP-infected PPU patients undergoing various treatment procedures. However, certain limitations exist. First, lifestyle variables, such as dietary habits, smoking, drinking, socioeconomic status, and genetic information, were not obtainable for adjusting the risks of developing HCC and ICC. Second, all data used were anonymous, and there was a lack of relevant clinical variables, such as pathology findings, imaging results and laboratory data. Third, the diagnoses of patients with HCC and ICC were considered accurate based on double-checked ICD-9 codes and the “catastrophic illness patients registry” in Taiwan; however, there was a limited ability to distinguish between HCC and ICC as well as limited sample size. Fourth, biases related to retrospective studies and the limited number of patients should be noted. Because the study cohorts were well matched by sex, age, and comorbidities, the biases were likely to be minimal. The diagnosis regarding cancer diagnosis was highly reliable.
Conclusion
Our results reported that non-HP-infected PPU patients who underwent TVP are associated with a decreased risk of subsequent HCC and ICC, which might be partly attributed to the alleviation of persistent vagal hyperactivity. However, further studies are warranted.
Data availability
This study used inpatient claims data from the Taiwan National Health Insurance Research Database (NHIRD). This database contains detailed medical histories of the hospitalized enrollees in Taiwan. Based on the guideline of Taiwan Ministry of Health and Welfare (TMHW), only citizens of the Taiwan are eligible to apply the NHIRD for research projects (https://nhird.nhri.org.tw/en/Data_Protection.html). The database we applied is only limited to our research purpose. All applicants must follow the Computer-Processed Personal Data Protection Law and related regulations of National Health Insurance Administration and NHRI (http://www.winklerpartners.com/?p=987). The ownership of NHIRD is belong to TMHW and the right to use is belong to the researchers. However, other researchers are able to request data access following the regulations of TMHW.
References
Ferlay, J. et al. GLOBOCAN 2012 v1.0, Cancer incidence and mortality worldwide. IARC cancer base no. 11. Lyon, France: International Agency for Research on Cancer (2013).
Yang, J. D. et al. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 16(10), 589–604 (2019).
Center, M. M. & Jemal, A. International trends in liver cancer incidence rates. Cancer Epidemiol. Biomark. Prev. 20, 2362–2368 (2011).
Forner, A., Reig, M. & Bruix, J. Hepatocellular carcinoma. Lancet 391(10127), 1301–1314 (2018).
Gupta, A. & Dixon, E. Epidemiology and risk factors: intrahepatic cholangiocarcinoma. HepatoBiliary Surg. Nutr. 6(2), 101–104 (2017).
Pavlov, V. A. & Tracey, K. J. The vagus nerve and the inflammatory reflex–linking immunity and metabolism. Nat. Rev. Endocrinol. 8, 743–754 (2012).
Yi, C. X. et al. The role of the autonomic nervous liver innervation in the control of energy metabolism. Biochim. Biophys. Acta 1802, 416–431 (2010).
McCuskey, R. S. Anatomy of efferent hepatic nerves. Anat. Rec. A Discov. Mol. Cell Evol. Biol. 280, 821–826 (2004).
Nada, T. et al. Autonomic nervous function in patients with peptic ulcer studied by spectral analysis of heart rate variability. J. Med. 32(5–6), 333–347 (2001).
Yukinaka, M. et al. Evaluation of autonomic nervous function in patients with essential hypertension complicated with peptic ulcer. J. Gastroenterol. Hepatol. 15, 40–44 (2000).
Cho, C. H., Qui, B. S. & Bruce, I. C. Vagal hyperactivity in stress induced gastric ulceration in rats. J. Gastroenterol. Hepatol. 11, 125–128 (1996).
Burcelin, R., Dolci, W. & Thorens, B. Glucose sensing by the hepatoportal sensor is GLUT2-dependent: in vivo analysis in GLUT2-null mice. Diabetes 49, 1643–1648 (2000).
Nishizawa, M. et al. The hepatic vagal reception of intraportal GLP-1 is via receptor different from the pancreatic GLP-1 receptor. J. Auton. Nerv. Syst. 80, 14–21 (2000).
Oben, J. A. & Diehl, A. M. Sympathetic nervous system regulation of liver repair. Anat. Rec. A Discov. Mol. Cell Evol. Biol. 280, 874–883 (2004).
Ueno, T. et al. Innervation of the sinusoidal wall: regulation of the sinusoidal diameter. Anat. Rec. A Discov. Mol. Cell Evol. Biol. 280, 868–873 (2004).
Cheng, C. L. et al. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug Saf. 20(3), 236–242 (2011).
Cheng, C. L. et al. Validity of in-hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance Research Database in Taiwan. Int. J. Cardiol. 15(201), 96–101 (2015).
Kao, W. H. et al. Validity of cancer diagnosis in the National Health Insurance database compared with the linked National Cancer Registry in Taiwan. Pharmacoepidemiol. Drug Saf. 27(10), 1060–1066 (2018).
Cheng, D. D. et al. The possible role of helicobacter pylori infection in non-alcoholic fatty liver disease. Front. Microbiol. 10(8), 743 (2017).
Wu, X. Z. & Chen, D. Helicobacter pylori and hepatocellular carcinoma: correlated or uncorrelated?. J. Gastroenterol. Hepatol. 21(2), 345–347 (2006).
Wang, J. et al. Impact of Helicobacter pylori on the growth of hepatic orthotopic graft tumors in mice. Int. J. Oncol. 47, 1416–1428 (2015).
Wang, J. et al. Helicobacter pylori infection may increase the risk of progression of chronic hepatitis B disease among the Chinese population: a meta-analysis. Int. J. Infect. Dis. 50, 30–37 (2016).
Giovannucci, E. et al. Diabetes and cancer: a consensus report. Diabetes Care 33(7), 1674–1685 (2010).
La Vecchia, C. et al. Liver cirrhosis and the risk of primary liver cancer. Eur. J. Cancer Prev. 7(4), 315–320 (1998).
Kasmari, A. J. et al. Independent of cirrhosis, hepatocellular carcinoma risk is increased with diabetes and metabolic syndrome. Am. J. Med. 130(6), 746.e1-746.e7 (2017).
Dearborn, J. L., Urrutia, V. C. & Zeiler, S. R. Stroke and cancer—a complicated relationship. J. Neurol. Transl. Neurosci. 2(1), 1039 (2014).
Borovikova, L. V. et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405, 458–462 (2000).
Angus, D. C. & van der Poll, T. Severe sepsis and septic shock. N. Engl. J. Med. 369, 840–851 (2013).
Wu, S. C. et al. Association of vagus nerve severance and decreased risk of subsequent type 2 diabetes in peptic ulcer patients: an Asian population cohort study. Medicine (Baltimore) 95(49), e5489 (2016).
Wu, S. C. et al. Acid-reducing vagotomy is associated with reduced risk of subsequent ischemic heart disease in perforated peptic ulcer: an Asian population study. Medicine (Baltimore) 95(50), e5651 (2016).
Fang, C. W. et al. Association of vagotomy and decreased risk of subsequent ischemic stroke in perforated peptic ulcer patients: an Asian population study. World J. Surg. 41(12), 3171–3179 (2017).
Cheng, T. J. et al. The association between peptic ulcer disease and ischemic stroke: a population-based longitudinal study. Medicine (Baltimore) 95(22), e3797 (2016).
Wu, S. C. et al. A comparative study of subsequent liver cirrhosis risk in non-Helicobacter pylori-infected peptic ulcer patients with and without vagotomy: an Asian population cohort study. J. Gastroenterol. Hepatol. 34(2), 376–382 (2019).
Puche, J. E., Saiman, Y. & Friedman, S. L. HSC and liver fibrosis. Compr. Physiol. 3(4), 1473–1492 (2013).
Moreira, R. K. HSC and liver fibrosis. Arch. Pathol. Lab. Med. 131(11), 1728–1734 (2007).
Wake, K. Liver perivascular cells revealed by gold and silver impregnation methods and electron microscopy. In Biopathology of the liver, an ultrastructural approach (ed. Motta, P.) 23–26 (Kluwer, 1988).
Bioulac-Sage, P., Lafon, M. E., Saric, J. & Balabaud, C. Nerves and perisinu-soidal cells in human liver. J. Hepatol. 10, 105–112 (1990).
Peinado, M. A., del Moral, M. L., Jimenez, A., Rodrigo, J. & Esteban, F. J. The nitrergic autonomic innervation of the liver. Auton. Neurosci. 99, 67–69 (2002).
Okabe, H. et al. Hepatic stellate cells may relate to progression of intrahepatic cholangiocarcinoma. Ann. Surg. Oncol. 16(9), 2555–2564 (2009).
Coulouarn, C. & Clément, B. Stellate cells and the development of liver cancer: therapeutic potential of targeting the stroma. J. Hepatol. 60(6), 1306–1309 (2014).
Hsieh, C. C., Hung, C. H., Chiang, M., Tsai, Y. C. & He, J. T. Hepatic Stellate cells enhance liver cancer progression by inducing myeloid-derived suppressor cells through interleukin-6 signaling. Int. J. Mol. Sci. 20(20), 5079 (2019).
Thompson, A. I., Conroy, K. P. & Henderson, N. C. Hepatic stellate cells: central modulators of hepatic carcinogenesis. BMC Gastroenterol. 15, 63 (2015).
Hellstrom, M., Kalen, M., Lindahl, P., Abramsson, A. & Betsholtz, C. Role of PDGF-B and PDGFR-beta in recruitment of vascular smooth muscle cells and pericytes during embryonic blood vessel formation in the mouse. Development 126(14), 3047–3055 (1999).
Yin, C. et al. HSC in liver development, regeneration, and cancer. J. Clin. Investig. 123(5), 1902–1910 (2013).
De Minicis, S. et al. Gene expression profiles during hepatic stellate cell activation in culture and in vivo. Gastroenterology 132, 1937–1946 (2007).
Strazzabosco, M. & Fabris, L. Development of the bile ducts: essentials for the clinical hepatologist. J. Hepatol. 56(5), 1159–1170 (2012).
Yan, C., Yang, Q. & Gong, Z. Activation of hepatic stellate cells during liver carcinogenesis requires fibrinogen/integrin αvβ5 in zebrafish. Neoplasia 20(5), 533–542 (2018).
Bockx, I., Elst, I. V., Roskams, T. & Cassiman, D. The hepatic vagus nerve stimulates HSC proliferation in rat acute hepatitis via muscarinic receptor type 2. Liver Int. 30, 693–702 (2010).
Cassiman, D. et al. The vagal nerve stimulates activation of the HPC compartment via muscarinic acetylcholine receptor type 3. Am. J. Pathol. 161(2), 521–530 (2002).
Ohtake, M., Sakaguchi, T., Yoshida, K. & Muto, T. Hepatic branch vagotomy can suppress liver regeneration in partially hepatectomized rats. HPB Surg. 6, 277–286 (1993).
Tanaka, K., Ohkawa, S., Nishino, T., Niijima, A. & Inoue, S. Role of the hepatic branch of the vagus nerve in liver regeneration in rats. Am. J. Physiol. 253, G439–G444 (1987).
Kox, M. et al. Increased vagal tone accounts for the observed immune paralysis in patients with traumatic brain injury. Neurology 70, 480–485 (2008).
Huang, K. W. et al. Chronic obstructive pulmonary disease: an independent risk factor for peptic ulcer bleeding: a nationwide population-based study. Aliment Pharmacol. Ther. 35(7), 796–802 (2012).
Kim, J., Kim, K. H. & Lee, B. J. Association of peptic ulcer disease with obesity, nutritional components, and blood parameters in the Korean population. PLoS ONE 12(8), e0183777 (2017).
Caldwell, S. H. et al. Obesity and hepatocellular carcinoma. Gastroenterology 127(5 Suppl 1), S97-103 (2004).
Ohki, T. et al. Obesity is an independent risk factor for hepatocellular carcinoma development in chronic hepatitis C patients. Clin. Gastroenterol. Hepatol. 6(4), 459–464 (2008).
Funding
This study is supported in part by Ministry of Health and Welfare, Taiwan (109-TDU-B-212-114004), MOST Clinical Trial Consortium for Stroke (MOST 108-2321-B-039-003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
W.S.C. conceived and designed the study and wrote the initial draft of the manuscript; C.H.T. participated in the study design; M.C.H. performed the data analysis and interpretation and was involved in writing the initial draft of manuscript; W.Y.C., T.C.W., and H.C.H. participated in data collection; W.S.C. performed the data analysis and interpretation as well as manuscript drafting and revision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclosure
This study used the National Health Insurance Research Database established by the National Health Research Institutes with the authorization of the Bureau of National Health Insurance of the Department of Health of Taiwan. The interpretations and conclusions contained herein do not represent the opinions of the aforementioned agencies and institutions.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, SC., Cheng, HT., Wang, YC. et al. Decreased risk of liver and intrahepatic cancer in non-H. pylori-infected perforated peptic ulcer patients with truncal vagotomy: a nationwide study. Sci Rep 11, 15594 (2021). https://doi.org/10.1038/s41598-021-95142-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-95142-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.