Abstract
Endoscopic retrograde cholangiopancreatography is not always successful even with needle knife precut sphincterotomy (NKPS). How to manage these patients with initial NKPS failure has not been well studied. We report the outcomes of patients who received endoscopic and non-endoscopic rescue treatment after the initial NKPS failure. During the 15 years from 2004 to 2018, 87 patients with initial NKPS failure received interval endoscopic treatment (IET group, n = 43), percutaneous transhepatic biliary drainage (PTBD group, n = 25), or bile duct surgery (BDS group, n = 19) were retrospectively studied. Compared with the PTBD group, the prevalence of choledocholithiasis was higher (69.8% vs. 16.0%, p < 0.001), and malignant bile duct stricture were lower (20.9% vs. 76.0%, p < 0.001) in the IET group. Furthermore, the IET group had a significantly longer time interval between the first and second treatment procedures (4 days vs. 2 days, p = 0.001), a lower technique success rate (79.1% vs. 100%, p = 0.021), and a shorter length of hospital stay (7 days vs. 18 days, p < 0.001). Compared to the BDS group, the only significant finding was that the patients in the IET group were older. Although not statistically significant, the complication rate was lowest in the IET group (7.0%) while highest in the BDS group (15.8%). Complications in the IET group were also mild, as compared with the other two groups. In conclusion, IET should be considered after initial failed NKPS for deep biliary cannulation before contemplating more invasive treatment such as BDS. PTBD may be the alternative therapy for patients with malignant biliary obstruction.
Similar content being viewed by others
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) has been widely used in the treatment of biliary diseases in recent decades. Deep bile duct cannulation is a critical step for the success of therapeutic ERCP but it cannot be always successful1. Conventional biliary cannulation methods include the use of a catheter or sphincterotome with or without guidewire assistance2. Using conventional methods, bile duct cannulation cannot be achieved in about 5%–15% of cases3. In this case, needle knife precut sphincterotomy (NKPS) is often used as a rescue technique3,4,5,6,7. However, the NKPS technique is very difficult and carries the risk of pancreatitis and perforation8. As a result, it was reported that the initial success rate of NKPS ranges widely from 71.3 to 92%9,10,11,12,13,14,15,16. Once NKPS fails, how to manage these patients optimally has not been well studied. In clinical practice, either endoscopic methods such as interval ERCP and percutaneous-transhepatic-endoscopic rendezvous procedures (PTE-RVs) or non-endoscopic methods such as percutaneous transhepatic cholangiography and drainage (PTCD) or bile duct surgery (BDS), can be the option of the rescue treatment17,18,19,20,21,22,23. However, no studies have compared the results of these rescue treatment methods in patients with initial NKPS failure. Therefore, we conducted this study to report the outcomes of patients with biliary diseases who received endoscopic and non-endoscopic rescue treatment after the initial NKPS failure due to difficult biliary cannulation.
Patients and methods
Definition of difficult biliary cannulation
Bile duct cannulation methods in our department included cannulation using a cannula and/or a sphincterotome, with or without guidewire assistance. After the cannula/sphincterotome methods failed to achieve deep bile duct cannulation, if the pancreatic duct was cannulated, whether to perform double guidewire method or cannulation after the insertion of a pancreatic duct stent depended on the individual endoscopist. All the above-mentioned methods were regarded as conventional cannulation methods. Difficult biliary cannulation was defined when the conventional cannulation methods failed to achieve deep bile duct cannulation. Although there was no strict definition of difficult biliary cannulation in terms of cannulation frequency, the cannulation time for difficult cases usually exceeded 20 min before 2015. After 2015, the early NKPS strategy was usually adopted24, 25. Early NKPS was performed when cannulation time more than 5 min or unintentional pancreatic duct cannulation more than once25.
Procedures of NKPS
For patients with difficult biliary cannulation, NKPS was performed immediately after the failure of the conventional cannulation methods during the same endoscopic session. The needle-knife sphincterotome (Rx Needle-Knife XL; Boston Scientific Corporation, Marlborough, USA) and an ICC 200 or VIO 200D electrosurgical unit (ERBE, Tübingen, Germany), which produced blended current, were used for NKPS. After making a puncture in the papilla above the orifice, the incision was made upward along the axis of the bile duct from the papillary orifice. The cut was extended until the common bile duct (CBD) was exposed, followed by a small incision in the biliary sphincter muscle. The CBD was then cannulated directly with the closed needle-knife or with a wire-guided cannula/sphincterotome. Failure of the initial NKPS procedure was defined as failure to expose the CBD or failure to place a catheter/sphincterotome deeply into the CBD to obtain satisfactory cholangiography.
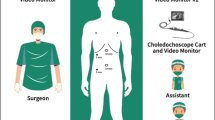
Patients and study design
During the 15 years from January 2004 to December 2018, we consecutively enrolled patients who underwent NKPS due to difficult biliary cannulation in our institution. The patients’ data were retrospectively retrieved from the database of our Therapeutic Endoscopy Center. During the study period, five endoscopists (A–E) performed 512 NKPS procedures for patients with difficult biliary cannulation. This study was reviewed and approved by the Ethics Committee of the Chang Gung Memorial Hospital (IRB No.: 202100304B0). Since this is a retrospective study using clinical routine treatment or diagnostic medical records, and no human immunodeficiency virus-positive cases were involved, the Chang Gung Medical Foundation Institutional Review Board approved the waiver of the participant's consent. All methods were carried out in accordance with relevant guidelines and regulations.
The exclusion criteria were (1) patients with successful deep bile duct cannulation by the NKPS (n = 398 or 77.7%); (2) patients with initial NKPS failure but not receiving a second interventional procedure, n = 27). Therefore, a total of 87 patients who met the inclusion and exclusion criteria were enrolled in this study (Fig. 1). Among these 87 patients with a second interventional procedure, 31 patients (35.6%) received interval ERCP, 12 patients (13.8%) received interval ERCP via PTE-RVs, 21 patients (24.1%) received PTCD, 4 patients (4.36%) received percutaneous transhepatic gallbladder drainage (PTGBD), and 19 patients (21.8%) received BDS. What kind of second interventional procedure was performed depending on the decision of the attending physician in the ward. For statistical analysis, patients who received interval ERCP and interval ERCP via PTE-RVs were combined as interval endoscopic treatment group (IET group, n = 43); patients who received PTCD and PTGBD were combined as percutaneous transhepatic biliary drainage group (PTBD group, n = 25), and patients who received BDS were classified as BDS group.
In the IET group, in case of the first ERCP failure, we tended to reserve the second ERCP to the most experienced endoscopist (71% of procedures were performed by endoscopist A). In the second ERCP, conventional cannulation methods were performed when the bile duct had been exposed (especially by bile staining or bile flow identification). If the conventional cannulation methods failed to achieve deep bile duct cannulation under the above circumstance, or if the bile duct could not be found on the second ERCP, a second pre-cut was performed.
The comparisons between groups were divided into three parts. The first part was the patients’ baseline characteristics, including demographic data, liver biochemistry tests, and the major papilla morphology. Demographic data included age and gender. Liver biochemistry tests included serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (Alk-P), and total bilirubin. The major papilla morphology included periampullary diverticulum and surgically altered anatomy. The second part was the factors that might affect the choice of endoscopic treatment or non-endoscopic treatment for the second interventional procedure. These factors included indications and adverse events of the first ERCP procedures, and inpatient departments. The indications for the first ERCP were choledocholithiasis, malignant biliary stricture, and benign biliary stricture or leakage. The adverse events of the first ERCP included bleeding and hemostasis during the NKPS, delayed post-ERCP bleeding, and post-ERCP pancreatitis. Bleeding and hemostasis during the NKPS referred to bleeding caused by precut, and hemostasis was to prevent bleeding from blocking the endoscopic view. The criteria of delayed post-ERCP bleeding and post-ERCP pancreatitis were defined according to Cotton et al.26. Inpatient departments included internal medicine and surgery. The third part was the comparison of the results of the second interventional procedures, including time interval between the first and second interventional procedures, technical success rate, early adverse events, length of hospital stay, and 30-day mortality.
Statistical analysis
Since the aim of the study was to report the outcomes between endoscopic and non-endoscopic treatments, comparisons were made between the IET group and the PTBD group and between the IET group and the BDS group. Continuous variables were shown as median with range, and statistical analysis for continuous variables was performed with the Mann–Whitney U test. For categorical variables, the chi-square test or Fisher exact test was used for statistical analysis whenever appropriate. Logistic regression analysis was performed to identify predictors associated with the second ERCP cannulation failure in the IET group. Statistical analyses were performed using SPSS software (version 20.0; SPSS, Inc., Chicago, IL). A two-tailed p-value of < 0.05 was considered statistically significant.
Results
There were 43 (49.4%), 25 (28.7%), and 19 (21.8%) patients in the IET, PTBD, and BDS groups, respectively. The patients’ baseline characteristics are demonstrated in Table 1. Compared with the PTBD group, patients in the IET group had significantly lower serum levels of Alk-P (median, 127 U/L vs. 211 U/L, p = 0.028) and total bilirubin (median, 2.6 mg/dL vs. 9.5 mg/dL, p = 0.007). Furthermore, the periampullary diverticulum was found to be significantly more prevalent in the IET group (41.9% vs. 8.0%, p = 0.003). Compared with the BDS group, the only significant finding was that patients in the IET group were older (median, 75 years vs. 60 years, p = 0.004).
Table 2 lists the factors that might affect the choice of endoscopic versus non-endoscopic treatment for the second interventional procedure. Indication of first ERCP included choledocholithiasis (n = 50), malignant biliary stricture (n = 30), and benign biliary stricture or leakage (n = 7). Among the 30 patients with malignant biliary stricture, 26 cases were distal bile duct stricture and 4 cases were hilar obstruction. Compared with the PTBD group, the incidence of choledocholithiasis in the IET group was significantly higher (69.8% vs. 16.0%, p < 0.001), and the incidence of malignant biliary stricture was lower (20% vs. 77.3%, p < 0.001). There was no significant difference in any ERCP indication between the IET group and the BDS group. However, most of the indications for ERCP in the BDS group were choledocholithiasis (16/19 or 84.2%). Compared with the BDS group, there were significantly fewer patients referred from the surgical department to the IET group (46.5% vs. 89.5%, p = 0.001). In fact, of the 19 patients who received BDS as the second interventional procedure, 17 (89.5%) came from the surgical department, while only 2 (10.5%) came from the medical department. Regarding ERCP complications, there were no significant differences between the IET and PTBD groups and between the IET and BDS groups.
The outcomes of the second interventional treatment are listed in Table 3. In the IET group, 15 patients (34.9%) needed a second NKPS during the interval ERCP. Compared with the PTBD group, the IET group had a significantly longer time interval between the first and second interventional procedures (median, 4 days vs. 2 days, p = 0.001), lower technique success rate (34/43 or 79.1% vs. 100%, p = 0.021), and shorter length of hospital stay after the second procedure (median, 7 days vs. 18 days, p < 0.001). Among the 9 patients in the IET group with failed second ERCP, two patients received a third ERCP, one patient received PTBD, five patients received BDS, and one patient did not receive a third interventional procedure. The factors associated with the cannulation failure of the second ERCP in the 31 patients who did not undergo rendezvous procedures were further evaluated (Table 4). However, there were no predictors determined in univariate and multivariate analysis. Compared with the BDS group, there were no significant differences in any outcome parameters in the IET group. The rate of complications related to the second interventional procedure was 7% (3/43) in the IET group, 8% (2/25) in the PTBD group, and 15.8% (3/19) in the BDS group. Although there was no statistical difference in the rate of complications, the types of complications in each group were quite different. The types of complications in the IET group included 1 case of precut bleeding and 2 cases of biliary tract infection. In the PTBD group, there was 1 case of biliary tract infection and 1 case of acute biliary perforation with bile peritonitis. In the BDS group, there was 1 case of hemobilia, 1 case of hemoperitoneum, and 1 case of bile duct perforation. The 30-day mortality rate in IET, PTBD and BDS groups was 7% (3/43), 16% (4/25) and 0%, respectively (p = not significant). The causes of death of the 3 patients in the IET group were new onset of ischemic stroke, decompensated liver cirrhosis, and advanced hepatocellular carcinoma. Among the 4 patients in the PTBD group, the causes of death were advanced Klatskin tumor, advanced lung cancer, frequent seizure attacks, and decompensated liver cirrhosis combined with hepatocellular carcinoma. In each group, none with 30-day mortality was caused by the second interventional procedure.
Discussion
ERCP, PTBD, and BDS are alternative interventions used in the management of biliary diseases. ERCP has become the preferred treatment for most biliary diseases, however, it is not always successful even with NKPS even in high-volume medical centers3. There is no consensus or guidelines on the management of these patients with initial NKPS failure due to difficult biliary cannulation. Several studies have shown that interval ERCP may be a viable treatment option after the initial NKPS failure, with a success rate of 68%–78%17, 18, 27,28,29. Our success rate was 79.1% (34/43), which added to the evidence for the feasibility of interval ERCP. However, 12 of our 43 patients received interval ERCP via PTE-RVs. The success rate of interval ERCP with PTE-RVs was significantly higher than that of interval ERCP without PTE-RVs (12/12 or 100% vs. 22/31 or 71%, p = 0.04). To our knowledge, no study compares the results between interval ERCP with and without PTE-RVs. Besides, PTE-RV appears to be preferable to PTBD because PTE-RV allows physicians to perform transhepatic punctures using only small-caliber catheters, thereby reducing complications19. Therefore, PTE-RVs can be used to achieve biliary access when the standard methods for biliary cannulation fail25.
In theory, hyperemia and edema of the papilla caused by NKPS will improve over time, which may increase the success rate of the second ERCP. However, the optimal interval between the first and second ERCP has not yet been determined. Kim J. et al. reported that the success rate after one day was significantly lower than that 2–3 days later (65.7% vs. 88.2%, P = 0.027)27. Another study conducted by Colan-Hernandez et al. concluded that a second ERCP should be delayed by at least 4 days because the procedure within 4 days after the initial precut was the only significant factor associated with the second ERCP failure17. However, we were unable to determine any factors related to the failure of the second ERCP, including the time interval.
The use of PTBD as an initial treatment for biliary diseases has declined in recent decades because PTBD is associated with adverse events accounting for 9%–13% and serious adverse events accounting for 4%–8%3, 23. Besides, PTBD reduces the patient's quality of life due to external drainage, and the drainage often needs to be replaced. Furthermore, it is difficult to carry out when the intrahepatic bile ducts (IHDs) are not dilated. Nevertheless, endoscopic biliary drainage is considered better than PTBD in patients with coagulopathy or ascites21. However, as shown in this study, PTBD is still a useful rescue therapy in which initial ERCP fails, especially for resectable malignant biliary obstruction30, 31.
In a recent US nationwide longitudinal study, ERCP has almost completely replaced the BDS to treat choledocholithiasis, which may be due to the improvement of the therapeutic capacity and safety of ERCP23. However, due to lack of study, it is unclear whether patients who fail the initial ERCP will still experience this trend. No trend toward ERCP was found in the present study because the inpatient department seemed to affect the decision-making on the endoscopic or surgical treatment. Among the patients receiving BDS, 84.2% of patients had choledocholithiasis, and all were from the surgical department. In contrast, none of the patients with choledocholithiasis in the medical department received BDS. Just like the treatment of colon polyps, this is an interesting phenomenon because physician expertise is often closely related to treatment strategy32. However, compared with the IET group, the BDS group had a higher incidence of procedure-related complications (15.8% vs. 7%, although not statistically significant) and more serious. As mentioned above, IET has an acceptably high success rate. Therefore, it is reasonable to provide endoscopic rather than surgical treatment for these patients with choledocholithiasis.
The major limitation of this study is its retrospective design, therefore, the patients in each group were not randomized. Most patients in the PTBD group were patients with malignant biliary obstruction (hence, dilated IHD). This selection bias might be the reason for the higher technical success rate of the PTBD group than the IET group. However, due to the low initial failure rate of NKPS in an experienced center, it was difficult to conduct prospective randomized studies. Second, endoscopic ultrasound-guided biliary drainage (EUS-BD) is increasingly used in patients who fail standard ERCP. EUS-BD may be preferred over PTBD because of better clinical success, fewer post-procedure adverse events, and a lower rate of re-intervention33. However, due to a lack of adequate expertise, it was not available in our institution during the study period.
In conclusion, IET has an acceptable success rate and less severe complications and should be tried after initial failed NKPS before contemplating more invasive interventions such as BDS. PTBD may be an alternative rescue therapy for patients with malignant biliary obstruction.
References
Harewood, G. C. & Baron, T. H. An assessment of the learning curve for precut biliary sphincterotomy. Am. J. Gastroenterol. 97, 1708–1712. https://doi.org/10.1111/j.1572-0241.2002.05829.x (2002).
Freeman, M. L. & Guda, N. M. ERCP cannulation: A review of reported techniques. Gastrointest. Endosc. 61, 112–125. https://doi.org/10.1016/s0016-5107(04)02463-0 (2005).
Chen, Q., Jin, P., Ji, X., Du, H. & Lu, J. Management of difficult or failed biliary access in initial ERCP: A review of current literature. Clin. Res. Hepatol. Gastroenterol. 43, 365–372. https://doi.org/10.1016/j.clinre.2018.09.004 (2019).
Sundaralingam, P., Masson, P. & Bourke, M. J. Early precut sphincterotomy does not increase risk during endoscopic retrograde cholangiopancreatography in patients with difficult biliary access: A meta-analysis of randomized controlled trials. Clin. Gastroenterol. Hepatol. 13, 1722-1729.e1722. https://doi.org/10.1016/j.cgh.2015.06.035 (2015).
Ang, T. L., Kwek, A. B., Lim, K. B., Teo, E. K. & Fock, K. M. An analysis of the efficacy and safety of a strategy of early precut for biliary access during difficult endoscopic retrograde cholangiopancreatography in a general hospital. J. Dig. Dis. 11, 306–312. https://doi.org/10.1111/j.1751-2980.2010.00454.x (2010).
Chen, J. et al. Assessing quality of precut sphincterotomy in patients with difficult biliary access: An updated meta-analysis of randomized controlled trials. J. Clin. Gastroenterol. 52, 573–578. https://doi.org/10.1097/MCG.0000000000001077 (2018).
Yasuda, I., Isayama, H. & Bhatia, V. Current situation of endoscopic biliary cannulation and salvage techniques for difficult cases: Current strategies in Japan. Digest. Endosc. 28(Suppl 1), 62–69. https://doi.org/10.1111/den.12591 (2016).
Anastassiades, C. P. & Saxena, A. Precut needle-knife sphincterotomy in advanced endoscopy fellowship. Gastrointest. Endosc. 77, 637–640. https://doi.org/10.1016/j.gie.2013.01.023 (2013).
Testoni, P. A. et al. Precut sphincterotomy, repeated cannulation and post-ERCP pancreatitis in patients with bile duct stone disease. Digest. Liver Dis. 43, 792–796. https://doi.org/10.1016/j.dld.2011.05.010 (2011).
Rabenstein, T., Ruppert, T., Schneider, H. T., Hahn, E. G. & Ell, C. Benefits and risks of needle-knife papillotomy. Gastrointest. Endosc. 46, 207–211. https://doi.org/10.1016/s0016-5107(97)70087-7 (1997).
Foutch, P. G. A prospective assessment of results for needle-knife papillotomy and standard endoscopic sphincterotomy. Gastrointest. Endosc. 41, 25–32. https://doi.org/10.1016/s0016-5107(95)70272-5 (1995).
Cennamo, V. et al. Timing of precut procedure does not influence success rate and complications of ERCP procedure: A prospective randomized comparative study. Gastrointest. Endosc. 69, 473–479. https://doi.org/10.1016/j.gie.2008.09.037 (2009).
Tang, S. J. et al. Precut papillotomy versus persistence in difficult biliary cannulation: A prospective randomized trial. Endoscopy 37, 58–65. https://doi.org/10.1055/s-2004-826077 (2005).
Catalano, M. F., Linder, J. D. & Geenen, J. E. Endoscopic transpancreatic papillary septotomy for inaccessible obstructed bile ducts: Comparison with standard pre-cut papillotomy. Gastrointest. Endosc. 60, 557–561. https://doi.org/10.1016/s0016-5107(04)01877-2 (2004).
Halttunen, J., Keranen, I., Udd, M. & Kylanpaa, L. Pancreatic sphincterotomy versus needle knife precut in difficult biliary cannulation. Surg. Endosc. 23, 745–749. https://doi.org/10.1007/s00464-008-0056-0 (2009).
Bailey, A. A. et al. Needle-knife sphincterotomy: factors predicting its use and the relationship with post-ERCP pancreatitis (with video). Gastrointest. Endosc. 71, 266–271. https://doi.org/10.1016/j.gie.2009.09.024 (2010).
Colan-Hernandez, J. et al. Optimal timing for a second ERCP after failure of initial biliary cannulation following precut sphincterotomy: An analysis of experience at two tertiary centers. Surg. Endosc. 31, 3711–3717. https://doi.org/10.1007/s00464-016-5410-z (2017).
Pavlides, M. et al. Repeat endoscopic retrograde cholangiopancreaticography after failed initial precut sphincterotomy for biliary cannulation. World J. Gastroenterol. 20, 13153–13158. https://doi.org/10.3748/wjg.v20.i36.13153 (2014).
Bokemeyer, A. et al. Percutaneous-transhepatic-endoscopic rendezvous procedures are effective and safe in patients with refractory bile duct obstruction. Unit. Eur. Gastroenterol. J. 7, 397–404. https://doi.org/10.1177/2050640619825949 (2019).
Fidelman, N. Benign biliary strictures: Diagnostic evaluation and approaches to percutaneous treatment. Tech. Vasc. Interv. Radiol. 18, 210–217. https://doi.org/10.1053/j.tvir.2015.07.004 (2015).
Lorenz, J. M. Management of malignant biliary obstruction. Semin. Intervent. Radiol. 33, 259–267. https://doi.org/10.1055/s-0036-1592330 (2016).
David, O., & Irabor, M. The pattern of fall of serum bilirubin after operative relief of obstructive jaundice. A preliminary report. Rev. Cienc. Salud. Bogotá (Colombia) (2009).
Huang, R. J. et al. Evolution in the utilization of biliary interventions in the United States: Results of a nationwide longitudinal study from 1998 to 2013. Gastrointest. Endosc. 86, 319-326.e315. https://doi.org/10.1016/j.gie.2016.12.021 (2017).
Dumonceau, J. M. et al. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline: Updated June 2014. Endoscopy 46, 799–815. https://doi.org/10.1055/s-0034-1377875 (2014).
Testoni, P. A. et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 48, 657–683. https://doi.org/10.1055/s-0042-108641 (2016).
Cotton, P. B. et al. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest. Endosc. 37, 383–393. https://doi.org/10.1016/s0016-5107(91)70740-2 (1991).
Kim, J. et al. Results of repeat endoscopic retrograde cholangiopancreatography after initial biliary cannulation failure following needle-knife sphincterotomy. J. Gastroenterol. Hepatol. 27, 516–520. https://doi.org/10.1111/j.1440-1746.2011.06914.x (2012).
Donnellan, F. et al. Outcome of repeat ERCP after initial failed use of a needle knife for biliary access. Dig. Dis. Sci. 57, 1069–1071. https://doi.org/10.1007/s10620-011-1982-6 (2012).
Kevans, D., Zeb, F., Donnellan, F., Courtney, G. & Aftab, A. R. Failed biliary access following needle knife fistulotomy: Is repeat interval ERCP worthwhile?. Scand. J. Gastroenterol. 45, 1238–1241. https://doi.org/10.3109/00365521.2010.495418 (2010).
Dorcaratto, D. et al. Is percutaneous transhepatic biliary drainage better than endoscopic drainage in the management of jaundiced patients awaiting pancreaticoduodenectomy? A systematic review and meta-analysis. J. Vasc. Interv. Radiol. 29, 676–687. https://doi.org/10.1016/j.jvir.2017.12.027 (2018).
Al Mahjoub, A. et al. Preoperative biliary drainage in patients with resectable perihilar cholangiocarcinoma: Is percutaneous transhepatic biliary drainage safer and more effective than endoscopic biliary drainage? A meta-analysis. J. Vasc. Interv. Radiol. 28, 576–582. https://doi.org/10.1016/j.jvir.2016.12.1218 (2017).
Aziz Aadam, A. et al. Physician assessment and management of complex colon polyps: A multicenter video-based survey study. Am. J. Gastroenterol. 109, 1312–1324. https://doi.org/10.1038/ajg.2014.95 (2014).
Sharaiha, R. Z. et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: A systematic review and meta-analysis. Gastrointest. Endosc. 85, 904–914. https://doi.org/10.1016/j.gie.2016.12.023 (2017).
Author information
Authors and Affiliations
Contributions
M.H.L. designed and performed the research and wrote the paper; Y.K.T. designed the research and supervised the report; C.H.L. designed the research and contributed to the analysis; C.H.W. contributed to the data collection; M.H.L., K.F.S., and N.J.L. provided clinical advice.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lo, MH., Lin, CH., Wu, CH. et al. Management of biliary diseases after the failure of initial needle knife precut sphincterotomy for biliary cannulation. Sci Rep 11, 14968 (2021). https://doi.org/10.1038/s41598-021-94361-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94361-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.