Abstract
Continuous positive airway pressure (CPAP) is simple and effective treatment for obstructive sleep apnea (OSA) patients. However, the CPAP prediction equation in each country is different. This study aimed to predict CPAP in Thai patients with OSA. A retrospective study was conducted in Thai patients, who OSA was confirmed by polysomnography and CPAP titration from January 2015 to December 2018. Demographics, body mass index (BMI), neck circumference (NC), Epworth sleepiness scale, apnea–hypopnea index (AHI), respiratory disturbance index (RDI), mean and lowest pulse oxygen saturation (SpO2), and optimal pressure were recorded. A total of 180 subjects were included: 72.8% men, age 48.7 ± 12.7 years, BMI 31.0 ± 6.3 kg/m2, NC 40.7 ± 4.1 cm, AHI 42.5 ± 33.0 per hour, RDI 47.1 ± 32.8 per hour, and lowest SpO2 77.1 ± 11.0%. Multiple linear regression analysis identified NC, BMI, RDI, and lowest SpO2. A final CPAP predictive equation was: optimal CPAP (cmH2O) = 4.614 + (0.173 × NC) + (0.067 × BMI) + (0.030 × RDI) − (0.076 × lowest SpO2). This model accounted for 50.0% of the variance in the optimal pressure (R2 = 0.50). In conclusion, a CPAP prediction equation can be used to explain a moderate proportion of the titrated CPAP in Thai patients with OSA. However, the CPAP predictive equation in each country may be different due to differences of ethnicity and physiology.
Trial registration: TCTR20200108003.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) is a potentially serious sleep disorder which is characterized by complete or partial obstructions of the upper airway during sleep resulting in repetitive episodes of reduction or elimination of airflow, pressure, and increasing respiratory muscle activities1,2. It is usually associated with sleep disruption, oxygen desaturation2, cognitive impairment3, increased daytime sleepiness2, and decreased concentration and quality of life4,5. There is increasing evidence to support that OSA can cause several diseases such as cardiovascular disease6,7, stroke8,9, and hypertension10,11. The estimated prevalence of OSA is about 4% in men and 2% in women1. There are many factors that significantly affect the OSA. Obesity is the strongest factor12. Moreover, sex (male), snoring, and personal physiology are also factors that affect OSA13,14.
Continuous positive airway pressure (CPAP) is recognized as the most effective, standard, and safe treatment for OSA patients15. It is extremely effective in eliminating apnea, hypopnea, respiratory effort related arousal, snoring, and for correcting oxygen level during sleep. Also, it helps decrease daytime sleepiness and enhance quality of life16,17,18.
Generally, CPAP pressure is performed in laboratory for finding the optimal pressure. This is called CPAP titration19. However, some patients cannot find the optimal pressure the first time and have to repeat the test. The procedure of finding the CPAP pressure is time consuming, labor intensive, expensive, and delays prescription. Predictive equation of optimal CPAP pressure is another method to find the pressure. It is a simple way of obtaining an optimal CPAP pressure in a short period of time20. The equation is derived from demographic, anthropometric, and polysomnographic variables to determine the pressure21,22,23.
However, the CPAP predictive equation is different in each country. Race or ethnicity and difference of physiology may play an important role in determining body size and severity of OSA. The objective of this study was to predict of the optimal CPAP pressure in Thai patients with obstructive sleep apnea.
Methods
Study design and subjects
We retrospectively reviewed the data of Thai patients with OSA who were at least 18 years old, male or female, and had successfully undergone polysomnography and CPAP titration at Thammasat University Hospital, Thailand from January 2015 to December 2018. All subjects had had OSA indicated by apnea–hypopnea index (AHI) ≥ 5 events per hour. They had been diagnosed in the first part of the night of the study and the optimal pressure had been determined in the second part. We excluded patients who had high residual AHI (AHI ≥ 5 events per hour) after was used CPAP. We included only 180 subjects for whom we had succeeded to find the optimal pressure. The optimal pressure was defined as reduction of AHI < 5 events per hour and had supine rapid eye movement (REM) for at least 15 min.
We recorded demographic variables: age and sex, anthropometric variables: height, weight, BMI, neck circumference (NC), polysomnographic variables: AHI, respiratory disturbance index (RDI), mean and lowest pulse oxygen saturation (SpO2), and optimal CPAP. Moreover, Epworth sleepiness scale (ESS) was also recorded.
Ethic approval was obtained from the Ethics Review Sub-Committee for Research Involving Human Research Subjects of Thammasat University, No.3 (IRB project No. 158/2561), in compliance with Declaration of Helsinki, The Belmont Report, CIOMS Guidelines and The International Practice (ICH-GCP). All methods were performed in accordance with these guidelines and regulations. All participants provided written informed consent.
Polysomnography
Polysomnography (PSG) was performed according to established standard of American Academy of Sleep Medicine (AASM)24,25. It consisted of monitoring of sleep by electroencephalography (EEG), electrooculography (EOG), electromyography (EMG), electrocardiography (ECG), SpO2, body position, and snoring. In addition, airflow was monitored with oronasal thermistor and nasal transducer for detecting apnea and hypopnea. Respiratory effort was monitored with thoracoabdominal plethysmography.
Respiratory events
Respiratory events were manually scored according to the 2012 AASM recommendations25. Apnea and hypopnea were defined by standard criteria26. Apnea was defined as decrement of airflow ≥ 90% from baseline for at least 10 s. Hypopnea was defined as reduction of nasal pressure ≥ 30% from baseline for at least 10 s and with ≥ 3% oxygen desaturation or accompanied by an EEG arousal for 3 to 15 s. Respiratory effort related arousal (RERA) was defined as a sequence of breath that reduces of nasal pressure < 30% from baseline for at least 10 s and is followed by an EEG arousal. AHI was defined as the total number of apnea and hypopnea per hour during sleep. RDI was calculated by the total number of apnea, hypopnea, and RERA per hour during sleep. Oxygen desaturation index (ODI) was defined as the number of events per hour in which oxygen saturation decreased by ≥ 3% from baseline25. The severity of OSA was determined by AHI or RDI; mild (AHI or RDI ≥ 5–14.9), moderate (AHI or RDI 15.0 – 29.9), and severe (AHI or RDI ≥ 30.0).
CPAP titration
CPAP titration was performed by a trained polysomnographic technologist. The pressure was started at 4 cmH2O and the pressure was increased at least 1 cmH2O if there were 2 apneas, 3 hypopneas, 5 RERAs, or 3 min of loud snoring within 5 min. The pressure was increased until respiratory events were abolished. The optimal pressure was that which can control respiratory events while sleeping in supine position and included supine REM for at least 15 min (AHI < 5 events per hour).
Statistical analysis
Data is presented as mean ± standard deviation and number (%). All statistical analyses were performed using SPSS version 23.0 software (IBM Corp., Armonk, NY, USA). Pearson’s correlation coefficient was used to explore the relationship between the optimal pressure and all variables. Multiple linear regression by backward stepwise method was used to identify independent predictive variables and to develop a predictive equation of the optimal CPAP. A two-sided P value < 0.05 was considered statistically significant.
Results
One hundred and ninety-two subjects were initially screened, with 12 subsequently excluded from analysis. A total of 180 subjects were included in the final analysis (Fig. 1). The demographic, anthropometric, and polysomnographic variables are shown in Table 1.
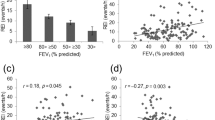
The correlation between the optimal pressure and demographic, anthropometric, and polysomnographic variables
Table 1 shows significant correlation between the optimal pressure and standard parameters. The results found that the optimal pressure was positively correlated with BMI, NC, diastolic blood pressure, heart rate, AHI, RDI, and ODI. In addition, the optimal pressure was negatively correlated with mean SpO2, and lowest SpO2 during sleep.
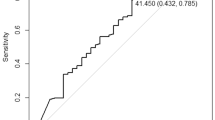
The CPAP predictive equation
The multiple linear regression by backward stepwise technique was used to identify independent predictive variables. A constant was 4.614. It indicated that NC (ß = 0.223, SE = 0.054, P = 0.003), BMI (ß = 0.150, SE = 0.034, P = 0.039), RDI (ß = 0.309, SE = 0.006, P < 0.001), and lowest SpO2 (ß = − 0.230, SE = 0.035, P = 0.001) were independent predictors of the optimal pressure. We used these parameters to develop a CPAP equation:
Optimal CPAP (cmH2O) = 4.614 + (0.173 × NC) + (0.067 × BMI) + (0.030 × RDI) − (0.076 × lowest SpO2).
This model accounted for 50% of the total variance (R2 = 0.50).
Discussion
Our study is the first retrospective study of CPAP prediction in Thai OSA patients. Our study showed that obesity (BMI and NC) and severity of OSA (RDI and lowest SpO2) were independent factors affecting the predictive optimal pressure. In adults, the most common cause of OSA is obesity which is associated with soft tissue of the mouth and throat. During sleep, throat and tongue muscles are more relaxed especially in REM. This soft tissue can cause the airway to become blocked27. Moreover, obesity is related to the fat deposition in the body, especially deposits around the neck resulting in more NC. These affect the severity of the OSA. If OSA is more severe, there is increased chance of higher CPAP pressure.
This study was similar to several previous studies. Loredo et al.21 generated a CPAP prediction formula from 67 patients in USA. They found that BMI, lowest SpO2, and mean SpO2 affect the prediction of their formula. Their final CPAP equation was 30.8 + (0.03 × RDI) − (0.05 × lowest SpO2) − (0.2 × mean SpO2). It explained 67% of variance. Besides, the study of Miljeteig et al.22 examined the factors that account for the variability in CPAP level in 38 OSA patients in Canada. They revealed that NC, BMI, and AHI were independent factors for their CPAP prediction formula. Their final CPAP equation was − 5.12 + (0.13 × BMI) + (0.16 × NC) + (0.04 × AHI). It explained 76% of variance. Furthermore, Lin and colleagues23 determined CPAP prediction from a 121 member Taiwanese population. They found that BMI and AHI were significant predictors of effective CPAP. Our study and the three previous studies21,22,23 showed measure of obesity (NC and BMI) and severity of OSA (AHI, RDI, and lowest SpO2) affected the generated the CPAP prediction formula. Although, the variables were similar, the final CPAP model was different. This may be due to the differences of ethnicity and physiology of the patients in each country.
However, our study found that ESS and sex were not significant predictive factors for our CPAP prediction model. This was similar to the study of Stadling et al.28. In contrast, some previous studies showed that ESS and sex were significant for their CPAP prediction models. Lee et al.29 developed an equation for optimal CPAP based on data from 178 Korean patients. They revealed that the degree of daytime sleepiness assessed by ESS was one of the independent predictors of their CPAP prediction model. Their final model was 6.656 + (0.156 × BMI)-(0.071 × lowest SpO2) + (0.041 × RDI) + (0.094 × ESS). Also, a study of Yong and colleagues30 developed a prediction equation for optimal CPAP pressure from 92 Malaysian patients. They reported that ESS and sex (male) were independent variables for their CPAP model. Their final model was 13.666 + (2.361 × male) + (0.154 × ESS) − (0.059 × lowest SpO2). In addition, a study of Schiza et al.31 evaluated the effect of sex on a CPAP predicting equation and they found that sex was a statistically significant factor to predict optimal pressure.
Our formula provided an optimal CPAP estimation of pressure for a moderate proportion (50% of variance) of subjects. CPAP prediction formula can potentially be useful for improving CPAP titration, as a guide for setting home auto CPAP, or for final adjustment of attended CPAP titration. Similarly, Rowley JA et al. reported that use of a CPAP prediction model increased the percentage of successful of CPAP titration from 50 to 68%32.
Our study did have limitations. Firstly, this study is limited by its retrospective nature, thus some variables might not have been collected. Secondly, the small sample size may limit the power of the regression model in detecting other potential predictors of optimal pressure. Lastly, a final predictive CPAP equation was not tested prospectively in a PSG laboratory. Therefore, a prospective cohort study is needed to verify this equation in the future.
Conclusions
A moderately predictive CPAP equation (50% of variance) can easily be derived from parameters of Thai patients with OSA. However, the CPAP predictive equation in each country may be different due to differences of ethnicity and physiology.
References
Young, T. et al. The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med. 328, 1230–1235 (1993).
Aloia, M. S., Arnedt, J. T., Davis, J. D., Riggs, R. L. & Byrd, D. Neuropsychological sequelae of obstructive sleep apnea-hypopnea syndrome: a critical review. J. Int. Neuropsychol. Soc. 10, 772–785 (2004).
El-Ad, B. & Lavie, P. Effect of sleep apnea on cognition and mood. Int. Rev. Psychiatry 17, 277–282 (2005).
Tsara, V., Kaimakamis, E., Serasli, E., Katsarou, Z. & Christaki, P. Health related quality of life in Greek patients with sleep apnea-hypopnea syndrome treated with continuous positive airway pressure. Sleep Med. 10, 217–225 (2009).
Finn, L., Young, T., Palta, M. & Fryback, D. G. Sleep-disordered breathing and self-reported general health status in the Wisconsin Sleep Cohort Study. Sleep 21, 701–706 (1998).
Gottlieb, D. J. et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation 122, 352–360 (2010).
Peker, Y., Carlson, J. & Hedner, J. Increased incidence of coronary artery disease in sleep apnoea: A long-term follow-up. Eur. Respir. J. 28, 596–602 (2006).
Arzt, M., Young, T., Finn, L., Skatrud, J. B. & Bradley, T. D. Association of sleep-disordered breathing and the occurrence of stroke. Am. J. Respir. Crit. Care Med. 172, 1447–1451 (2005).
Munoz, R. et al. Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke 37, 2317–2321 (2006).
Stoohs, R. A. et al. Sleep-disordered breathing and systemic hypertension in the older male. J. Am. Geriatr. Soc. 44, 1295–1300 (1996).
Hla, K. M. et al. Sleep apnea and hypertension. A population-based study. Ann. Intern. Med. 120, 382–388 (1994).
Jehan, S. et al. Obstructive sleep apnea and obesity: implications for public health. Sleep Med. Disord. 1, 00019 (2017).
Punjabi, N. M. The epidemiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 5, 136–143 (2008).
Yaggi, H. K. & Strohl, K. P. Adult obstructive sleep apnea/hypopnea syndrome: definitions, risk factors, and pathogenesis. Clin. Chest Med. 31, 179–186 (2010).
Wahab, N. A. & Ahmed, Y. N. Optimal level of continuous positive airway pressure: Auto-CPAP titration versus predictive formulas. Egypt. J. Chest Dis. Tuberc. 66, 353–361 (2016).
Freedman, N. Treatment of obstructive sleep apnea syndrome. Clin. Chest Med. 31, 187–201 (2010).
Kushida, C. A. et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J. Clin. Sleep Med. 4, 157–171 (2008).
Loredo, J. S., Ancoli-Israel, S., Kim, E. J., Lim, W. J. & Dimsdale, J. E. Effect of continuous positive airway pressure versus supplemental oxygen on sleep quality in obstructive sleep apnea: a placebo-CPAP-controlled study. Sleep 29, 564–571 (2006).
American Thoracic Society. Indications and standards for use of nasal continuous positive airway pressure (CPAP) in sleep apnea syndromes. American Thoracic Society. Official statement adopted March 1944. Am. J. Respir. Crit. Care Med. 150, 1738–1745 (1994).
Lai, C. C. et al. Clinical predictors of effective continuous positive airway pressure in patients with obstructive sleep apnea/hypopnea syndrome. Laryngoscope. 125, 1983–1987 (2015).
Loredo, J. S., Berry, C., Nelesen, R. A. & Dimsdale, J. E. Prediction of continuous positive airway pressure in obstructive sleep apnea. Sleep Breath. 11, 45–51 (2007).
Miljeteig, H. & Hoffstein, V. Determinants of continuous positive airway pressure level for treatment of obstructive sleep apnea. Am. Rev. Respir. Dis. 147, 1526–1530 (1993).
Lin, I. F., Chuang, M. L., Liao, Y. F., Chen, N. H. & Li, H. Y. Predicting effective continuous positive airway pressure in Taiwanese patients with obstructive sleep apnea syndrome. J. Formos. Med. Assoc. 102, 215–221 (2003).
American Academy of Sleep Medicine. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22, 667–689 (1999).
Berry, R. B. et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 8, 597–619 (2012).
Bonnet, M. et al. EEG arousals: Scoring rules and examples. A preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorder Association. Sleep 15, 173–184 (1992).
Schwartz, A. R. et al. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc. Am. Thorac. Soc. 5, 185–192 (2008).
Stradling, J. R., Hardinge, M., Paxton, J. & Smith, D. M. Relative accuracy of algorithm-based prescription of nasal CPAP in OSA. Respir. Med. 98, 152–154 (2004).
Lee, G. H., Kim, M. J., Lee, E. M., Kim, C. S. & Lee, S. A. Prediction of optimal CPAP pressure and validation of an equation for Asian patients with obstructive sleep apnea. Respir. Care 58, 810–815 (2013).
Yong, M. C., Shyang, K. S., Chan, S. K. & Tie, S. T. A prediction equation of CPAP pressure for obstructive sleep apnea in Malaysian. Respirology 23, 314 (2018).
Schiza, S. E. et al. Utility of formulas predicting the optimal nasal continuous positive airway pressure in a Greek population. Sleep Breath. 15, 417–423 (2011).
Rowley, J. A., Aboussouan, L. S. & Badr, M. S. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep 23, 929–938 (2000).
Acknowledgements
The authors would like to thank Michael Jan Everts who is a lecturer at Faculty of Medicine in Thammasat University for proofreading this manuscript. The financial support was provided by Thammasat University Hospital, Thailand.
Author information
Authors and Affiliations
Contributions
N.S. and K.L. contributed to the design of this study. K.L. and A.P. collected, analyzed and interpreted the data and drafted this manuscript. N.S. reviewed the final manuscript. All authors read, approved and agreed on the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saiphoklang, N., Leelasittikul, K. & Pugongchai, A. Prediction of optimal continuous positive airway pressure in Thai patients with obstructive sleep apnea. Sci Rep 11, 13935 (2021). https://doi.org/10.1038/s41598-021-93554-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93554-5
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.