Abstract
This cross-sectional study of 136 patients with chronic obstructive pulmonary disease (COPD) investigated the mechanism underlying overlap syndrome, defined as coexisting COPD and obstructive sleep apnea (OSA). OSA was defined as a respiratory event index (REI) ≥ 5 events/h, determined using type-3 portable monitors. The mean REI was 12.8 events/h. Most participants (60.1%) had mild OSA (REI: 5–15 events/h). The REI was positively correlated with forced expiratory volume in one second (%FEV1) (r = 0.33, p < 0.001), body mass index (BMI) (r = 0.24, p = 0.005), and fat-free mass index (r = 0.31, p = 0.005), and negatively correlated with residual volume divided by total lung capacity (r = −0.27, p = 0.003). Receiver-operating characteristic curve analysis revealed an optimal BMI cutoff of 21.96 kg/m2 for predicting moderate/severe OSA. A BMI ≥ 21.96 kg/m2 was associated with OSA among participants with %FEV1 ≥ 50%, but not those with %FEV1 < 50%. This study revealed an interaction between airflow limitation and hyperinflation, nutritional status, and OSA.
Similar content being viewed by others
Introduction
The term “overlap syndrome” was originally introduced in 1985 to describe the association between two disorders, namely chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA)1. Epidemiological studies have indicated a highly diverse prevalence of this syndrome, ranging from 1–3% in the general population to >60% in COPD cohorts2. To date, the clinical importance of overlap syndrome has increased due to its association with an increased risk of pulmonary hypertension, COPD exacerbation, and death3. Overlap syndrome is frequently undiagnosed4. To investigate the appropriate method of diagnostic evaluation and treatment of OSA, it is necessary to elucidate the associated risk factors and pathologies.
Recently, Zhu et al. reported that the apnea hypopnea index (AHI) was inversely correlated with airflow limitation5. Although the mechanisms of this phenomenon have not been clarified, COPD-elicited hyperinflation may improve apneas and hypopneas in overlap syndrome through the hyperinflation-elicited increase in stiffness at the pharyngeal site, which precludes the extrathoracic upper airway from collapsing6.
Moreover, cachexia is a major comorbidity in advanced COPD7, COPD-related hyperinflation and emphysema are associated with cachexia and muscle wasting8, and COPD patients with low muscle mass (as measured by the Fat Free Mass Index, FFMI) have a higher mortality7. Therefore, the task force for nutritional assessment recommended an evaluation of body composition for the clinical management of COPD. In contrast, obesity is the most common risk factor for obstructive sleep apnea (OSA), especially in Caucasians9. In consequence, the relationship between obesity and the severity of overlap syndrome remains controversial. The link between severity of COPD and sleep apnea, and the nutritional status of the patient is expected to be complex.
While polysomnography (PSG) is widely accepted as the gold standard for the diagnosis of OSA, the procedure is complicated, time-consuming, expensive, and not readily available in most hospitals. Recently, portable monitoring equipment comprising at least four channels (airflow, respiratory movements, oxyhemoglobin saturation, and heart rate) has been classified as a type-3 portable monitor and has been used as an alternative diagnostic test for OSA in high-risk patients with OSA, and more recently, their usefulness in COPD patients has been reported10 as well as their cost effectiveness11. Especially in the primary care setting, the usefulness of a type-3 portable monitor for diagnostic evaluation in outpatients is reported12.
Hence, we hypothesized that both physiological abnormalities of the lung and body composition might be associated with OSA, determined using portable sleep testing. The aims of the current study were to determine whether airflow limitation and/or hyperinflation and nutritional status, are associated with increased or decreased apnea and/or hypopnea formation using type-3 portable monitors.
Methods
Study population
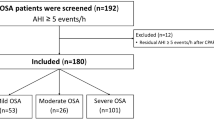
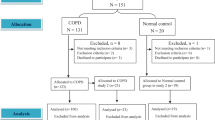
This study was conducted at the Keio University and Nihon Kokan Hospital in Japan. The inclusion criteria for this cross-sectional study were: (1) age>40 years; (2) lifelong cigarette consumption≥10 pack-years; (3) COPD diagnosis; and (4) forced expiratory volume in one second/forced vital capacity ratio (FEV1/FVC) < 70%. The exclusion criteria were as follows: (1) severe systemic diseases, including malignancy in any organ, severe heart failure, or recent history of unstable myocardial infarction or stroke; (2) exacerbations or changes in medications in at least three months prior to study entry; and (3) prescription of long-term oxygen therapy. Sleep patterns and lung function were cross-sectionally examined in 136 patients with COPD. The research protocol was approved by the respective human ethics committees of the two institutions at Keio University School of Medicine (reference number: 2009–0008), and Nihon Kokan Hospital (reference number: 2015-2). All participants provided written informed consent.
Sleep studies
The patients underwent unattended home monitoring for abnormal respiratory events during sleep with a type-3 portable device (Morpheus, Teijin Home Healthcare, Tokyo, Japan). The portable device recorded chest and abdominal respiratory movements, nasal air pressure, oxyhemoglobin saturation (SpO2), heart rate, and body position. The results were manually converted to scores by trained technicians based on the recommendations proposed by the American Academy of Sleep Medicine (AASM). Apnea was diagnosed based on the criteria that there was a drop in the respiratory signal by ≥90% of the pre-event baseline that lasted for ≥10 s. Hypopnea was measured based on the criteria that there was a drop in the respiratory signal by ≥30% but <90% of pre-event baseline in combination with ≥3% oxygen desaturation. Patients with a respiratory event index (REI, representing the sum of apnea and hypopnea events) above 5 events/h were defined as having overlap syndrome and compared with those without overlap syndrome (REI < 5 events/h).
Lung function tests
All participants underwent spirometry and measurement of lung volume by helium dilution under stable conditions during baseline examination. Spirometric tests, including forced vital capacity (FVC), forced expiratory volume in one second (FEV1), forced expiratory flow-volume curve, and forced inspiratory flow-volume curve, were conducted using an electric spirometer (HI-801, CHEST MI, Tokyo, Japan). Residual volume (RV) and total lung capacity (TLC) were measured using the multi-breath helium dilution method. The value of diffusing capacity for carbon monoxide (CO) divided by the alveolar volume (DLCO/VA) was determined using the single breath method.
Maneuvers were performed according to the standardization of lung function testing recommended by the task force of the American Thoracic Society (ATS) and European Respiratory Society (ERS). Reference values for lung function parameters were calculated using equations reported by the Japanese Respiratory Society (JRS). The severity of airflow limitation was defined as grade 1 (FEV1 ≥ 80% of predicted value), grade 2 (FEV1 50–80% of predicted value), grade3 (FEV1 30–50% of predicted value) and grade 4 (FEV1 < 30% of predicted value) based on the 2017 Global Initiative for Chronic Obstructive Disease (GOLD) criteria.
To estimate extrathoracic upper airway collapsibility, the indicator of peak inspiratory flow rate (PIF) divided by peak expiratory flow rate (PEF) (PIF/PEF) was introduced13,14. The denominator and numerator on this indicator are in reverse order compared to the original FEF50/FIF50 indicator15,16 that has been used to evaluate extrathoracic airway obstruction in a functional sense. FIF50 corresponds to the forced inspiratory flow rate at 50% of inspiratory vital capacity (VC), and approximately corresponds to PIF in our equation. The usefulness of FEF50/FIF50 in subjects with no expiratory airflow limitation was extensively argued by many authors. Instead of FEF50, we adopted PEF in this study because FEF50 is crucially influenced by the intrathoracic peripheral airway obstruction, which is remarkably exaggerated in COPD. Hence, we considered that the PIF/PEF indicator might be better suited than FEF50/FIF50 and could act as a surrogate measure for extrathoracic upper airway collapsibility in lungs with COPD pathologies. A higher PIF/PEF implies a diminished collapsibility of the extrathoracic upper airway.
Questionnaire and other measurements
At enrollment, full medical and smoking history, Epworth sleepiness scale (ESS), COPD assessment test (CAT), St. George’s Respiratory Questionnaire (SGRQ), and information on the current pharmacologic treatment and exacerbations were obtained.
Standing height and body weight were measured, and bioelectrical impedance analysis was performed using the BC309 (TANITA, Tokyo, Japan) to assess body composition, fat mass index (FMI), and fat-free mass index (FFMI). The study participants were divided into four groups to evaluate the mutual effects of airflow limitation and nutritional status modulation on apnea and hypopnea formation: Group 1 (BMI < 21.96 kg/m2 and %FEV1 < 50%), Group 2 (BMI ≥ 21.96 kg/m2 and %FEV1 < 50%), Group 3 (BMI < 21.96 kg/m2 and %FEV1 ≥ 50%), and Group 4 (BMI ≥ 21.96 kg/m2 and %FEV1 ≥ 50%). The cutoff value for BMI was calculated as the BMI that best predicts moderate/severe OSA.
Furthermore, based on the history of exacerbations and CAT scores, patients were divided into three groups of A, B, and E with GOLD classification 202317: Group A is defined as a group with few subjective symptoms (CAT scores <10) and few exacerbations (one or fewer exacerbations not requiring hospitalization); Group B is a group with strong subjective symptoms (CAT score ≥10) but few exacerbations; and Group E is a group with many exacerbations (two or more exacerbations or at least one exacerbation requiring hospitalization) regardless of subjective symptoms.
Statistical analysis
Data were compared among three or more groups using the Kruskal-Wallis and Steel-Dwass tests. The Jonckheere-Terpstra trend test was used to evaluate secular trends of the REI between the four groups stratified according to the Global Initiative Chronic Obstructive Lung Disease (GOLD) grade. Correlations between continuous variables were evaluated using the Pearson’s correlation coefficient. Receiver operating characteristic (ROC) curves were constructed to assess the areas under the curve (AUC). The optimal cutoff value was investigated by maximizing the Youden index. All calculations were performed using the IBM SPSS package (Version 22.0, IBM SPSS Inc., New York, NY, USA). The values are expressed as mean ± SD. Statistical significance was set at P < 0.05.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Results
Prevalence of overlap syndrome
The patient characteristics are shown in Table 1. The mean age was 72.8 ± 7.8 years. At baseline, 28.7%, 43.4%, 25.0%, and 2.9% of the patients were diagnosed with GOLD grades 1, 2, 3, and 4, respectively. The mean REI was 12.8 events per hour and 22.8%, 47.1%, 22.8%, and 7.4% of the patients had a normal (REI < 5), mild (5 ≤ REI < 15), moderate(15 ≤ REI < 30), and severe (REI ≥ 30) OSA status, respectively. The mean ESS score was 4.2 ± 2.4, and only one patient had an ESS > 10 and was considered sleepy.
Comparison of clinical characteristics of patients grouped according to the severity of sleep apnea
The characteristics of participants discriminated by REI values are shown in Table 2. Body mass index (BMI) was significantly different (p = 0.022) and FFMI was inclined to be different (p = 0.063) between the three groups, and both parameters increased in parallel with the severity of OSA (p = 0.007 and 0.014, respectively). There were no differences in age, smoking status, and ESS across the three groups.
Relationships between airflow limitation, hyperinflation and apnea/hypopnea formation
The relationships between the spirometric parameters and the REI are shown in Fig. 1. The comparison of REI stratified by FEV1 predicted value was shown in Fig. 1a. The REI decreased significantly with COPD severity. There was a significant correlation between FEV1 and the REI (r = 0.33, p < 0.001; Fig. 1b), and between DLco/VA and the REI (r = 0.18, p = 0.045; Fig. 1c). The hyperinflation-associated parameters, such as RV/TLC, were significantly correlated with the REI (r = -0.27, p = 0.003) (Fig. 1d). Evaluation of the relationships among airflow limitation, hyperinflation, and upper airway collapsibility was performed using the PIF/PEF ratio. PIF/PEF increased as airflow limitation (FEV1: r = -0.46, p < 0.001; Fig. 2a) and hyperinflation (RV/TLC: r = 0.34, p < 0.001; Fig. 2b) deteriorated. In addition, PIF/PEF tended to correlate with the REI (r = -0.14, p = 0.094) (Fig. 2c).
a Comparison of REI between the four groups stratified by the Global Initiative for Chronic Obstructive Lung Disease criteria: %FEV1 ≥ 80%; 80% > %FEV1 ≥ 50%; 50% > %FEV1 ≥ 30%; 30% > %FEV1. Correlation between REI and %FEV1 b, %DLCO/VA c, and RV/TLC d. REI respiratory event index, RV/TLC residual volume divided by total lung capacity, %DLco/VA percent predicted diffusing capacity for carbon monoxide divided by the alveolar volume, FEV1 forced expiratory volume in one second.
Relationships between nutritional status and apnea/hypopnea formation
The BMI (r = 0.24, p = 0.005; Fig. 3a) and the FFMI (r = 0.31, p = 0.005; Fig. 3b) were significantly and positively correlated with the REI. ROC curves revealed that the optimal cutoffs for the BMI (AUC: 0.64, sensitivity: 80.5%, specificity: 49.5%; Fig. 3c) and the FFMI (AUC: 0.64, sensitivity: 82.8%, specificity: 42.9%; Fig. 3d) for predicting moderate/severe OSA were 21.96 and 17.30, respectively. In contrast with the association between FEV1 or RV/TLC and PIF/PEF, the BMI did not correlate with PIF/PEF (r = -0.08, p = 0.35).
Comparison of apnea hypopnea index using classification of airflow limitation and BMI
The study participants were divided into four groups to evaluate the mutual effects of airflow limitation and BMI modulation on apnea and hypopnea formation: Group 1 (BMI < 21.96 kg/m2 and %FEV1 < 50%), Group 2 (BMI ≥ 21.96 kg/m2 and %FEV1 < 50%), Group 3 (BMI < 21.96 kg/m2 and %FEV1 ≥ 50%), and Group 4 (BMI ≥ 21.96 kg/m2 and %FEV1 ≥ 50%). Group 4 revealed a higher REI compared to Groups 1, 2, and 3 (Group1, 2, 3 vs. 4: n = 24, 14, 31, 67; REI = 8.3 ± 6.2, 9.4 ± 6.2, 9.2 ± 8.2 vs. 16.7 ± 11.4, p < 0.001, p = 0.022, p < 0.001 respectively; Fig. 4). On the other hand, there were no significant differences in REI between the three groups of A, B, and E based on the GOLD classification 2023 (Group A and B, vs. E: n = 32, 39, 8; REI = 13.0 ± 10.4, 12.7 ± 10.5, vs. 9.6 ± 8.8, p = 0.63; Supplemental Fig. 1).
Group 1 (n = 24); BMI < 21.96 kg/m2 and FEV1 < 50 %predicted, Group 2 (n = 14); BMI ≥ 21.96 kg/m2 and FEV1 < 50% predicted, Group 3 (n = 31); BMI < 21.96 kg/m2 and FEV1 ≥ 50 % predicted, and Group 4 (n = 67); BMI ≥ 21.96 kg/m2 and FEV1 ≥ 50 % predicted. *Group 4 revealed a higher REI than groups 1, 2, and 3 (Group 4 vs. Group 1; p < 0.001, Group 4 vs. Group 2; p = 0.022, Group 4 vs. Group 3; p < 0.001). REI respiratory event index, BMI body mass index, FEV1 forced expiratory volume in one second.
Discussion
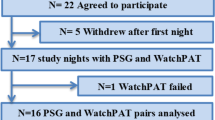
This is a study to investigate the clinical characteristics of patients with COPD having OSA, determined using type-3 portable monitors. We believe that the results of the study are useful even in primary care settings, as PSG is often not available in primary care centers. In this study, type-3 portable monitors objectively revealed an OSA prevalence of 77.2% in Japanese patients with COPD. The observed prevalence is slightly higher than those reported previously2. The reason for this discrepancy is not clear, but it may reflect the different populations under investigation and the different methods or criteria for the diagnosis of overlap syndrome. As coexisting OSA worsens the prognosis of COPD patients3 and the survival of patients with overlap syndrome that is not treated with nocturnal positive airway pressure is significantly inferior to that of patients with overlap syndrome that is appropriately treated3,18, the diagnosis of OSA in COPD patients is important. However, overlap syndrome is frequently undiagnosed4. This study showed that OSA is a common comorbidity in Japanese patients with COPD. Two novel observations of potential relevance were made. First, the severity of airflow limitation, hyperinflation, and upper airway collapsibility were found to affect the REI in COPD patients through detailed spirometric assessment. Second the nutritional status, represented by BMI, is one of the most influential factors on the REI in COPD patients, even within the normal range.
Many factors related to coexisting COPD have been reported to modify the formation of apnea and hypopneas in overlap syndrome. Among them, decreased tethering of airways through the loss of lung recoil19, hyperinflation-augmented vagal-mediated reflex20, neural reflex-induced nasal obstruction21, and blunted responses of the respiratory center to various stimuli, particularly during REM sleep22, have been considered as supporting factors for apneas and hypopneas. On the other hand, hyperinflation-augmented stiffness of the upper airway walls23 is thought to be an important inhibitory factor against apnea and hypopnea formation. In fact, data from clinical trials revealed inverse relationships between AHI and FEV1 or radiological emphysema in patients with overlap syndrome5,6. The significant role of high lung volume in the inhibition of extrathoracic upper airway obstruction in subjects with no COPD was originally demonstrated by Spann and Hyatt in 197123. Caudal traction through hyperinflation may unfold the airway or stiffen the airway walls to create a net ventral force that opens the extrathoracic upper airway, which leads to the inhibition of obstructive apnea and hypopnea formation (tracheal tug theory)23,24,25. Herein, we showed an important role of airflow limitation or TLC- and RV-related hyperinflation in restraining apnea and hypopnea formation. Our findings are consistent with the view that the hyperinflation-related inhibitory force against apnea and hypopnea formation is practically canceled out by the forces that promote apnea and hypopnea formation, including the decreased tethering of airways caused by the loss of elastic recoil in the destroyed lung parenchyma in patients with COPD.
The upper airway collapsibility provided by the PIF/PEF was associated with airflow limitation and hyperinflation, but the correlation between PIF/PEF and the REI was not significant (p = 0.09). Taken together, these findings suggest that although the PIF/PEF detects upper airway collapsibility under a specific condition, the PIF/PEF-represented upper airway opening force may be insufficient to alleviate the airflow limitation-related apnea and hypopnea formation, or the PIF/PEF does not reflect a dynamic change in upper airway collapsibility during sleep. No reports on the association between the PIF/PEF and other spirometric parameters in COPD patients are available. Therefore, to draw a definite conclusion regarding the effect of airflow limitation on upper airway collapsibility in association with apnea and hypopnea formation, it may be necessary to introduce a more precise method that allows the detection of dynamic changes in the upper airway cross-sectional area during sleep, such as CT26, MRI27, fluoroscopy28, or video-assisted nasoendoscopy29. However, these methods present difficulty in preserving natural sleep when applied to a sleeping subject.
The BMI and FFMI were significantly correlated with the REI. These results were consistent with those of a previous study, which showed that obesity is the most common risk factor for OSA in the general population9. Even if the BMI was within the normal range, a BMI > 21.96 kg/m2 was a predictor of moderate to severe OSA in our COPD population, especially in the preserved lung function groups (FEV1 ≥ 50% of predicted value). The relationship between obesity and the REI of overlap syndrome patients remains controversial3. While the reason for this discrepancy is not known, ethnic differences may be partly responsible. Asians including Japanese are generally less obese than Westerners. Thus, the threshold of BMI to predict the occurrence of OSA may differ among countries. Further, several studies, including our previous study, have demonstrated that the cachexia and emphysema phenotypes are more common in Japanese patients with COPD than in Western patients with COPD30. Therefore, whether this examination applies to Westerners should be determined henceforth. According to the results of this study, high BMI was associated with high AHI in patients with mild obstructive disorders, but not in those with severe obstructive disorders. Asians who are generally less obese than Westerners have been reported to be at a risk for OSA even in mild obesity31. It can be deduced that even a mild increase in BMI in this study was associated with high AHI in the mild COPD group. On the other hand, nutritional modulation has no effect on apnea and hypopnea development among patients with advanced COPD having an FEV1 below 50% of the predicted value. There are two possible reasons for the lack of such an association in severe COPD. One is that the effects of obstructive dysfunction and hyperinflation were more strongly associated with AHI than with high BMI. Therefore, the association with BMI may not have been apparent. The other reason is that few cases with a high BMI were included in the severe COPD group, making it difficult to appreciate the differences. In previous studies, severe COPD has been associated with a lower BMI and FFMI32,33. In fact, in our study, only 10.3% (N = 14/136) of patients with severe COPD had a higher BMI > 21.96 kg/m2. To examine the exact group differences, it may be necessary to study an even larger number of GOLD 1–4 patients.
In addition to airflow obstruction, we also investigated the impact of CAT score and history of exacerbations. There were no differences in REI between the three groups of A, B, and E based on the GOLD classification 2023. These results indicate that it may be appropriate to first focus on the degree of airflow obstruction and the risk of OSA complications rather than on subjective symptoms and exacerbations in primary care settings. In this study, there was only a small number of patients in Group E. This result was consistent with previous studies that reported that Japanese patients with COPD have a lower frequency of exacerbations34,35; however, more extensive studies are needed. There are several limitations to the present study. First, this is a cross-sectional study with only a single time point evaluation. As such, no conclusion can be drawn regarding the causal relationship between the abnormality of spirometric parameters or nutritional status and OSA severity. Second, the proportion of women was relatively small (8.8%), and the average age of the participants was higher than in the studies conducted in Western countries. Third, the study population included outpatients of a relatively large hospital. Therefore, caution should be exercised while applying the results of our study to patients visiting a clinic. Further, the number of cases is relatively small, and further investigations, such as a multicenter study in a clinic or a population-based study, are needed to determine whether our findings are applicable to the Japanese population as a whole as well as to the world general population. Fourth, the mechanism of upper airway obstruction has not yet been determined, as it has not been possible to directly observe the pharyngeal area in otolaryngology; some inferences about the mechanism have been made based on indirect data. Finally, lung function tests were not performed under the post-bronchodilator condition, and tests to exclude asthmatic elements, such as FeNO and peripheral blood eosinophils, were also not performed. Therefore, COPD may have been overdiagnosed, and cases with a combined asthmatic component were not completely removed. Many studies have shown that asthma has a negative impact on sleep apnea19,36,37,38, and it is possible that asthma complications have some impact on the pathogenesis of sleep apnea. The present study also did not measure eosinophils or FeNO, nor did it confirm the degree of reversibility, as mentioned above. Therefore, the effect of asthma complications on the results needs to be further investigated.
In conclusion, In Japanese COPD patients, airflow limitation and lung hyperinflation had a significant impact on the severity of OSA, with higher severity leading to lower REI. Further, BMI and FFMI were correlated with REI, especially in the preserved lung function groups. These findings may be useful in identifying high-risk groups for OSAS and the pathogenesis of overlap syndromes.
Data availability
The data that support the findings of this study are available from the corresponding author, S.C.
References
Flenley, D. C. Sleep in chronic obstructive lung disease. Clin. Chest Med. 6, 651–661 (1985).
Shawon, M. S. et al. Current evidence on prevalence and clinical outcomes of co-morbid obstructive sleep apnea and chronic obstructive pulmonary disease: a systematic review. Sleep Med. Rev. 32, 58–68 (2017).
Marin, J. M., Soriano, J. B., Carrizo, S. J., Boldova, A. & Celli, B. R. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am. J. Respir. Crit. Care Med. 182, 325–331 (2010).
Gunduz, C., Basoglu, O. K. & Tasbakan, M. S. Prevalence of overlap syndrome in chronic obstructive pulmonary disease patients without sleep apnea symptoms. Clin. Respir. J. 12, 105–112 (2018).
Zhu, J. et al. Effect of lung function on the apnea-hypopnea index in patients with overlap syndrome: a multicenter cross-sectional study. Sleep Breath 24, 1059–1066 (2020).
Krachman, S. L. et al. COPDGene investigators. effect of emphysema severity on the apnea-hypopnea index in smokers with obstructive sleep apnea. Ann. Am. Thorac Soc. 13, 1129–1135 (2016).
Putcha, N. et al. Mortality and exacerbation risk by body mass index in patients with COPD in TIOSPIR and UPLIFT. Ann. Am. Thorac Soc. 19, 204–213 (2022).
Spelta, F., Fratta Pasini, A. M., Cazzoletti, L. & Ferrari, M. Body weight and mortality in COPD: focus on the obesity paradox. Eat Weight Disord. 23, 15–22 (2018).
Lecube, A. et al. Asymptomatic sleep-disordered breathing in premenopausal women awaiting bariatric surgery. Obes. Surg. 20, 454–461 (2010).
Chang, Y. et al. Validation of the Nox-T3 portable monitor for diagnosis of obstructive sleep apnea in patients with chronic obstructive pulmonary disease. J. Clin. Sleep Med. 15, 587–596 (2019).
Guerrero, A. et al. Management of sleep apnea without high pretest probability or with comorbidities by three nights of portable sleep monitoring. Sleep 37, 1363–1373 (2014).
Chai-Coetzer, C. L. et al. A simplified model of screening questionnaire and home monitoring for obstructive sleep apnoea in primary care. Thorax 66, 213–219 (2011).
Nouraei, S. A. et al. Physiological comparison of spontaneous and positive-pressure ventilation in laryngotracheal stenosis. Br. J. Anaesth. 101, 419–423 (2008).
Nouraei, S. A. et al. Quantifying the physiology of laryngotracheal stenosis: changes in pulmonary dynamics in response to graded extrathoracic resistive loading. Laryngoscope 117, 581–588 (2007).
Jordanoglou, J. & Pride, N. B. A comparison of maximum inspiratory and expiratory flow in health and in lung disease. Thorax 23, 38–45 (1968).
Haponik, E. F., Bleecker, E. R., Allen, R. P., Smith, P. L. & Kaplan, J. “Abnormal inspiratory Flow-volume curves in patients with sleep-disordered breathing. Am. Rev. Respir. Dis. 124, 571–574 (1981).
Global strategy for the diagnosis, management and prevention of COPD. Gold. 2023. Available from: https://goldcopd.org/2023-gold-report-2/. [cited 2 May 2023]
Machado, M. C. et al. CPAP and survival in moderate-to-severe obstructive sleep apnoea syndrome and hypoxaemic COPD. Eur. Respir. J. 35, 132–137 (2010).
Ioachimescu, O. C. & Teodorescu, M. Integrating the overlap of obstructive lung disease and obstructive sleep apnoea: OLDOSA syndrome. Respirology 18, 421–431 (2013).
van Lunteren, E. et al. Phasic volume-related feedback on upper airway muscle activity. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 56, 730–736 (1984).
Hurst, J. R. Upper airway. 3: Sinonasal involvement in chronic obstructive pulmonary disease. Thorax 65, 85–90 (2010).
McNicholas, W. T. Impact of sleep in COPD. Chest 117, 48S–53S (2000).
Spann, R. W. & Hyatt, R. E. Factors affecting upper airway resistance in conscious man. J. Appl. Physiol. 31, 708–712 (1971).
Stanchina, M. L. et al. The influence of lung volume on pharyngeal mechanics, collapsibility, and genioglossus muscle activation during sleep. Sleep 26, 851–856 (2003).
Owens, R. L., Malhotra, A., Eckert, D. J., White, D. P. & Jordan, A. S. The influence of end-expiratory lung volume on measurements of pharyngeal collapsibility. J. Appl. Physiol. (1985) 108, 445–451 (2010).
Engstroem, H., Grimby, G. & Soederholm, B. Dynamic spirometry in patients with tracheal stenosis. Acta Med. Scand. 176, 329–334 (1964).
Deegan, P. C. & McNicholas, W. T. Pathophysiology of obstructive sleep apnoea. Eur. Respir. J. 8, 1161–1178 (1995).
Morrell, M. J., Arabi, Y., Zahn, B. & Badr, M. S. Progressive retropalatal narrowing preceding obstructive apnea. Am. J. Respir. Crit Care Med. 158, 1974–1981 (1998).
Andrade, R. G. et al. Impact of acute changes in CPAP flow route in sleep apnea treatment. Chest 150, 1194–1201 (2016).
Takahashi, S. & Betsuyaku, T. The chronic obstructive pulmonary disease comorbidity spectrum in Japan differs from that in western countries. Respir Investig 53, 259–270 (2015).
Dudley, K. A. & Patel, S. R. Disparities and genetic risk factors in obstructive sleep apnea. Sleep Med. 18, 96–102 (2016).
Mete, B., Pehlivan, E., Gulbas, G. & Gunen, H. Prevalence of malnutrition in COPD and its relationship with the parameters related to disease severity. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 3307–3312 (2018).
Ischaki, E. et al. Body mass and fat-free mass indices in COPD: relation with variables expressing disease severity. Chest 132, 164–169 (2007).
Sato, M. et al. Impact of mild exacerbation on COPD symptoms in a Japanese cohort. Int. J. Chron. Obstruct Pulmon Dis. 11, 1269–1278 (2016).
Suzuki, M. et al. Clinical features and determinants of COPD exacerbation in the Hokkaido COPD cohort study. Eur. Respir. J. 43, 1289–1297 (2014).
Julien, J. Y. et al. Prevalence of obstructive sleep apnea-hypopnea in severe versus moderate asthma. J. Allergy Clin. Immunol. 124, 371–376 (2009).
Larsson, L. G., Lindberg, A., Franklin, K. A. & Lundbäck, B. Symptoms related to obstructive sleep apnoea are common in subjects with asthma, chronic bronchitis and rhinitis in a general population. Respir. Med. 95, 423–429 (2001).
Teodorescu, M. et al. Association between asthma and risk of developing obstructive sleep apnea. JAMA 313, 156–164 (2015).
Acknowledgements
We would like to acknowledge Tomoko Betsuyaku for her contribution towards much useful pieces of advice and Chiyomi Uemura for data collection.
Author information
Authors and Affiliations
Contributions
M.H. participated in the design of the study, performed the statistical analyses, and had a major contribution in writing the manuscript. K.F. planned the study design and contributed to the interpretation of the results. H.N., K.A., and T.B. conceived the study, participated in its design and coordination, and helped draft the manuscript. S.C., W.Y., K.O., N.H., and N.M. contributed to the collection of data and interpretation of results. All authors read and approved the final manuscript. K.F. was the guarantor for this study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hashiguchi, M.H., Chubachi, S., Yamasawa, W. et al. Interaction of BMI and respiratory status in obstructive sleep apnea, a cross-sectional COPD study. npj Prim. Care Respir. Med. 33, 30 (2023). https://doi.org/10.1038/s41533-023-00351-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-023-00351-w