Abstract
FMR1 premutation (55–200 CGG repeats) results in fragile X-associated primary ovarian insufficiency (FXPOI). We evaluated expression levels of folliculogenesis-related mediators, follicle-stimulating hormone (FSH) receptor and anti-Mullerian hormone (AMH), to gain insights into the mechanisms underlying the reduced ovarian function. Mural granulosa cells (MGCs) were collected from FMR1 premutation carriers and noncarriers undergoing IVF treatments. At baseline, MGCs of carriers demonstrated significantly higher mRNA expression levels of AMH (3.5 ± 2.2, n = 12 and 0.97 ± 0.5, n = 17, respectively; p = 0.0003) and FSH receptor (5.6 ± 2.8 and 2.7 ± 2.8, respectively; p = 0.02) and higher AMH protein expression on immunostaining. Accordingly, FMR1 premutation-transfected COV434 cells exhibited higher AMH protein expression than COV434 cells transfected with 20 CGG repeats. We conclude that FMR1 premutation may lead to dysregulation of AMH expression levels, probably due to a compensatory mechanism. Elucidating the pathophysiology of FXPOI may help in early detection of ovarian dysfunction and tailoring IVF treatments to FMR1 premutation carriers.
Similar content being viewed by others
Introduction
Fragile X syndrome (FXS) is a trinucleotide repeat disorder commonly accompanied by male intellectual disability1. It is the major cause of inherited mental retardation2 and the prominent known reason for autism spectrum disorders3. Patients carrying the full CGG repeat expansion mutation (> 200 repeats) lack expression of the fragile X mental retardation 1 (FMR1) protein (FMRP) due to hypermethylation of the promoter region of the FMR1 gene4. Carrying the FMR1 premutation CGG repeat expansion (55–200 repeats) leads to two different phenotypes: fragile X-associated primary ovarian insufficiency (FXPOI) in females5,6 and fragile X-associated tremor/ataxia syndrome (FXTAS) mainly in males7,8.
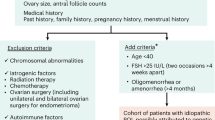
Unlike individuals with the full mutation, female premutation carriers have elevated FMR1 mRNA expression levels such that FMRP expression remains normal or only slightly decreased4. They have been shown to exhibit abnormal levels of ovarian reserve biomarkers, poor response to controlled ovarian hyperstimulation (COH), and early menopause5,9, all indicative of deteriorating fertility. Occurrences of primary ovarian insufficiency (POI) are mainly idiopathic. However, some etiologies such as autoimmune and infectious ovarian impairments, toxins and genetic aberrations have been associated with POI10. Within FMR1 premutation carriers, about 20% have POI and diminished ovarian reserve compared to 1% of the general population11.
Several studies have reported an association of premature ovarian insufficiency with dysregulations of folliculogenesis-related genes, including genes coding stem cell factor (SCF)12, growth and differentiation factor 9 (GDF9)13, follicle-stimulating hormone (FSH), and anti-Mullerian hormone (AMH)14,15. AMH, secreted by granulosa cells, might be involved in the recruitment of dormant primordial follicles12. AMH's inhibitory role is suspected to assist in dominant follicle selection, possibly by reducing the follicle's sensitivity to FSH stimulation16,17. Moreover, it seems that the role of AMH during follicular development is stage dependent, and species specific18. Studies have suggested that AMH promotes pre-antral follicle growth, but inhibits antral follicle maturation and dominant follicle selection in rats, non-human-primates and humans18,19. We hypothesized that an imbalance in folliculogenesis mediators may be involved in the decreased fertility of female FMR1 premutation carriers. The aim of the present study was to evaluate the mRNA and protein expression of AMH, a well-defined marker of ovarian reserve, and FSH receptor in mural granulosa cells (MGCs) of FMR1 premutation carriers and noncarriers undergoing in vitro fertilization (IVF) treatments and in FMR1 premutation-transfected tumor cells in order to gain insight into the pathophysiologic mechanisms underlying FXPOI.
Results
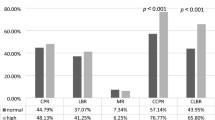
Higher AMH and FSH receptor mRNA expression levels were found in FMR1 premutation carriers. At baseline (before FSH stimulation), MGCs of FMR1 premutation carriers demonstrated higher AMH mRNA expression levels than MGCs of noncarriers (3.5 ± 2.2, n = 12 and 0.97 ± 0.5, n = 17 respectively; p = 0.0003 (Fig. 1a). Stratification of the groups by response to COH (≤ 5 or > 5 oocytes produced) showed that MCGs of poor responders who carried the FMR1 premutation had significantly higher AMH mRNA levels than MCGs of poor responders without the premutation (3.97 ± 2.7, n = 7 and 1.0 ± 0.4, n = 9, respectively; p = 0.01) (Fig. 1b). After 48 h of FSH stimulation, AMH expression was still higher (by 3.2 fold) in MCGs of the carriers than the noncarriers (p = 0.03) (Fig. 1c) and in MCGs of poor responders in the carrier group than poor responders in the noncarrier group (7.9 ± 3.8, n = 5 and 1.5 ± 1.4, n = 8 p = 0.007, respectively) (Fig. 1d).
Higher AMH and FSH receptor expression levels in MGCs of FMR1 premutation carriers compared to MGCs of noncarriers. (a) AMH and (e) FSH receptor mRNA expression levels in MGCs of FMR1 premutation carriers (FMR PM) and non-carriers (CTL) without FSH stimulation. (b) AMH and (f) FSH receptor mRNA expression levels in MGCs in sub-groups according to the oocytes number retrieved in OPU; GR > 5, PR ≤ 5. (c) AMH and (g) FSH receptor mRNA expression levels in MGCs following 48 h of FSH stimulation. (d) AMH and (h) FSH receptor mRNA expression levels in FSH-stimulated MGCs by number of oocytes number retrieved in OPU: GR > 5, PR ≤ 5. *p < 0.05, **p < 0.01, ***p < 0.001. Graphs show fold change in expression relative to control ± STDEV.
Baseline expression levels of FSH receptor mRNA were significantly higher (by 2.1 fold) in FMR1 premutation carriers than noncarriers (p = 0.02) (Fig. 1e). Stratification of the groups by response to COH showed a significantly higher FSH receptor expression level (by 3.4 fold) in MCGs of good responders in the carrier group than in MCGs of good responders in the noncarrier group (p = 0.04, n = 7 and n = 9 respectively). However, there was a nonsignificant trend-level decrease in FSH receptor expression in MCGs of poor responders in the carriers group compared to the noncarriers group (n = 5) (Fig. 1f). Indeed, within the noncarrier group, poor responders had a higher FSH receptor mRNA level (by 3.1fold) than good responders (p = 0.03; n = 6 and n = 9 respectively) (Fig. 1f). After FSH stimulation, premutation carriers had significantly higher base line levels of FSH receptor mRNA expression than noncarriers (3.1 ± 1.5, n = 12 and 1.9 ± 1.2, n = 14, respectively; p = 0.03) (Fig. 1g). However, FSH stimulation did not instigates significant differences between the groups (Fig. 1h).
Following detection of a dysregulation in mRNA expression of folliculogenesis-related genes in MGCs from FMR1 premutation carriers, we explored AMH protein expression. Immunostaining with anti-AMH antibody revealed an elevated protein expression in MGCs of FMR1 premutation carriers compared to MGCs of noncarriers (Fig. 2).
Src-associated substrate in mitosis of 68 kDa (SAM68) is a RNA-binding protein that plays an important role in RNA signal transduction. Evaluation of baseline expression of SAM68 mRNA revealed significantly higher levels in MGCs of FMR1 premutation carriers than noncarriers (1.6 ± 0.8, n = 12 and 1.0 ± 0.5, n = 17, p = 0.03 respectively). The same trend was observed following FSH stimulation (1.7 ± 1.0, n = 12 and 1.0 ± 0.5, n = 17, p = 0.03 respectively) (Fig. 3a,c). On comparison of poor responders between the groups, expression levels of SMA68 were significantly higher in carriers than noncarriers both before and after FSH stimulation (Fig. 3b,d).
Higher SAM68 and FMR1 mRNA expression levels in MGCs of FMR1 premutation carriers compared to noncarriers. (a) SAM68 and (e) FMR1 mRNA expression levels in MGCs of FMR1 premutation carriers (FMR PM) and noncarriers (CTL) without FSH stimulation. (b) SAM68 and (f) FMR1 mRNA expression levels in MGCs in sub-groups according to the oocytes number retrieved in OPU; GR > 5, PR ≤ 5. (c) SAM68 and (g) FMR1 mRNA expression levels in MGCs following 48 h of FSH stimulation. (d) SAM68 and (h) FMR1 mRNA expression levels in FSH-stimulated MGCs by number of oocytes retrieved in OPU: GR > 5, PR ≤ 5. *p < 0.05, **p < 0.01, ***p < 0.001. Graphs show fold change relative to control expression ± STDEV.
FMR1 mRNA expression levels were also higher in premutation carriers than non-carriers (1.2 ± 0.5, n = 11 and 0.6 ± 0.4, n = 14, respectively; p = 0.007) (Fig. 3e). A twofold increase was observed following FSH stimulation (p = 0.002) (Fig. 3g). Similar findings were noted on analysis of poor responders both before and after FSH stimulation (Fig. 3f,h).
We cultured the human isolated MGCs (obtained following follicular puncture at the end of an ovarian stimulation) for 4 days in FSH-deprived conditions to achieve a steady state resembling antral preovulatory follicles (described in the methods). To confirm that, we examined the expression levels of luteinizing hormone (LH) receptor in MGCs from FMR1 premutation carriers and noncarriers. No between- or within-group differences in expression were noted (Fig. 4a–d).
Similar LHR mRNA expression levels in MGCs of FMR1 premutation carriers and noncarriers. (a) Expression levels in MGCs of FMR1 premutation carriers (FMR PM) and non-carriers (CTL) without FSH stimulation. (b) Expression levels in MGCs by number of oocytes retrieved in OPU: GR > 5, PR ≤ 5. (c) Expression levels in MGCs following 48 h of FSH stimulation. (d) Expression levels in FSH-stimulated MGCs by number of oocytes retrieved in OPU: GR > 5, PR ≤ 5. Graphs show fold change relative to control expression ± STDEV.
Given the dysregulation of AMH expression in the FMR1 premutation carriers, we investigated the impact of CGG repeats on AMH expression. We examined AMH expression in COV434 cells transfected with 99 CGG repeats, with and without FMRpolyG expression (GFP signal represented transfected cells) compared to COV434 cells transfected with 20 CGG repeats. Following immunostaining with AMH antibody, we noted higher AMH protein expression in the premutation model of transfected COV434 cells regardless of the ability of the cells to produce the toxic FMRpolyG protein (Fig. 5).
COV434 premutation model expressing higher AMH once in the premutation range. (a) 99xCGG-transfected COV434 cells displaying higher AMH expression than 20xCGG- transfected COV434 cells. GFP signal represents transfected cells. Bar = 10 µm. (b) Quantification of AMH expression in transfected COV434 cells shown in panel (a). (c) Western blot showing higher expression in COV434 transfected with 99xCGG with and without FMRpolyG expression. Values were normalized with untreated COV434. All groups were harvested 72 h following transfection.
The clinical and IVF cycle characteristics of the FMR1 premutation carriers and noncarriers are shown in Table 1.
Discussion
In the present study, we observed elevated levels of AMH and FSH receptor at both the RNA and protein levels in FMR1 premutation carriers, suggesting a dysregulation in ovarian folliculogenesis.
The mechanism underlying the pathogenesis of FXPOI syndrome is poorly understood. We hypothesized that dysregulations in mediators of folliculogenesis were involved in the decline in fertility of FMR1 premutation carriers. Our analysis of the expression of FSH receptor and AMH, major participants in follicular recruitment, growth, and maturation14,15,20, revealed higher levels in carriers of the FMR1 premutation than in noncarriers. In light of the high diversity in expression within the groups at the mRNA (Fig. 1a–d) and protein (Fig. 2) levels, we further stratified them by response to COH. (We abstained stratifying according to CGG repeats number' due to the small sample size of only three FMR1 premutation carriers, which is not statistically powered). We found that carriers who were poor responders (i.e., produced < 5 oocytes in response to COH for IVF) had an elevated AMH expression (Fig. 1b).
AMH is presumed to play many key roles in folliculogenesis. Although levels in serum remain constant during the menstrual cycle, the expression pattern of AMH in granulosa cells differ. In previous studies, AMH expression was first detected in granulosa cells of early primary follicles and was highest in preantral and antral follicles14,21. Using a rhesus macaque model, Xu et al. demonstrated that the activity of AMH in the ovary of primates could be stage-dependent, encouraging preantral follicle growth. AMH is associated with the recruitment of dormant follicles at the beginning of the cycle and with inhibiting further maturation of antral follicles in the late follicular stage, as part of the negative feedback process to assist selection of the dominant follicle20. Kedem et al. found that in women with polycystic ovarian syndrome (PCOS), there was a negative correlation between the size of antral follicles and expression levels of AMH in granulosa cells. Note that in PCOS the higher AMH expression is due to the high number of small follicles secreting AMH, reflecting the intrinsic characteristics of their granulosa cells. However, among patients undergoing in vitro maturation, levels were higher in older women with lower ovarian reserve than in younger ones22, supporting a compensatory role of AMH in promoting pre-antral follicle growth and increasing the antral-follicle pool. In another study by Kedem et al.23, higher AMH mRNA expression was detected in cumulus granulosa cells of large preovulatory follicles in non- metaphase II (MII) oocytes compared to MII oocytes. As with poor responder FMR1 premutation carriers, abnormal follicullogenesis, manifested by either reduce oocytes cohort or abnormal maturation, might be the culprit of higher AMH mRNA expression, aiming to encourage preantral follicle growth. The role of AMH in folliculogenesis in humans has not been investigated in detail. It is generally presumed that AMH serves as a gate keeper, inhibiting primordial follicles recruitment (directly and via inhibiting FSH induced recruitment), mainly in rodents. Nevertheless, an additional possible mechanism might be related to an accelerated activation of dormant/primordial follicles by the higher expression of AMH in human FMR1 premutation carriers. Further studies with a larger sample size, enabling the observation of earlier stages of primordial follicles recruitment, are required to determine and elucidate which mechanisms are involved in FMR1 premutation carriers' pathophysiology.
FMR1 premutation carriers are at higher risk of diminished ovarian reserve and in most cases demonstrate poorer response to COH. In accordance with the study of Kedem et al.22, we demonstrated significantly higher AMH expression levels in poor responders with a low oocyte yield. We therefore suggest that in FMR1 premutation carriers, the early impaired follicle activity is followed by a compensatory mechanism that upregulates genes involved in folliculogenesis. In poor responders, the elevated expression of AMH and FSH receptor might initially accelerate follicular recruitment, but later it evokes a vicious cycle causing secondary damage to the ovarian reserve and resulting in POI. Moreover, the possibility of accelerating follicular recruitment in FMR1 premutation carriers might explain our observations; women who carry the premutation exhibited higher AMH secretion, this might cause an upraised recruitment of dormant follicles in each menstrual cycle, and results in a decreased ovarian reserve. Some FMR1 premutation carriers undergoing IVF treatments might obtain higher oocytes number following oocytes retrieval in the beginning, and less in later treatments. We found that the intensity of the AMH staining varied within the FMR1 premutation group. Apparently in some FMR1 premutation carriers another compensation mechanism might be involved and prevent them from deteriorating into a state of FXPOI. Further investigations are needed to understand the association between folliculogenesis mediators and to determine whether their elevation is the culprit or an epiphenomenon of POI.
Similar to poor responders, good responders in the FMR1 premutation carrier group expressed significantly higher FSH receptor than noncarriers (Fig. 1f). Again, FSH receptor upregulation may be due to a compensatory process, mitigating a lower response of carrier follicles to COH. The trend of decreased expression levels in the poor responders implies that the compensatory mechanism is not functional, which would explain the decreased number of follicles retrieved from poor responders in the FMR1 premutation carrier group. In good responders, however, FSH receptor levels are apparently elevated more efficiently, as suggested by the higher number of oocytes produced compared to poor responders. Within the noncarrier group, poor responders exhibited higher FSH receptor levels compared to good responders. Since FSH receptor has a role in the growth and maturation of the follicles, we suggest that when a lower number of oocytes are retrieved, an upregulation of FSH receptor expression might be evoked. While noncarriers' MGCs were able to elevate FSH receptor levels, FMR1 premutation carriers' MGCs kept low levels of FSH receptor. To conclude this hypothesis, further investigation is needed with a larger cohort and data analysis comparing clinical characterizations.
The molecular mechanisms underlying FXTAS have been relatively explored and defined. Two major mechanisms were identified: RNA gain-of-function toxicity and toxic cryptic polyglycine-containing protein (FMRpolyG) expression (Sellier et al.24,25). Their role in the decline in fertility in individuals with the FMR1 premutation is not known.
The RNA gain-of-function mechanism induces the CGG extended repeats tract to avidly sequester more than 30 RNA binding proteins, such as hnRNP A2, Pur α, SAM68, and Drosha and its partner DGCR8, thereby inducing their loss of function8,24,25,26,27,28). Sam68 has several functions in RNA editing one of which is alternative splicing. High expression levels of Sam68 have been shown in the gonads. Bianchi et al.29 observed direct binding of Sam68 to FSH receptor mRNA causing its downregulation in ovaries of adult knockout females. Accordingly, we observed elevated Sam68 mRNA levels in MGCs of FMR1 premutation carriers (Fig. 3a–d) both before and after FSH stimulation. Interestingly, when the groups were stratified by response, the poor responders in the carrier group maintained the significantly high Sam68 expression levels relative to poor responders in the noncarrier group. Immunostaining with Sam68 antibody did not distinguish FMR1 premutation MGCs from normal CGG repeat tract cells (Supplementary Fig. 1). Nevertheless, the elevation in mRNA levels might imply impaired Sam68 function which could trigger an upregulation of FSH receptor to compensate for the loss of function. These interactions between Sam68 and FSH receptor might play a role in FSH receptor dysregulation in FMR1 premutation carriers and warrant further investigation.
FMR1 mRNA levels were elevated in the FMR1 premutation group (Fig. 3e–h), in accordance with previous reports30,31. Stratifying the premutation carrier group to poor and good responders, revealed that the elevation in FMR1 expression levels was significant in the poor responder group only. For further conclusions regarding the relation between FMR1 expression levels and the ovarian response of the carriers, a larger sample size is required. Together the increased levels of Sam68 and of FMR1 suggests that RNA toxicity might be involved in FXPOI pathobiology.
Todd et al.32 proved that the CGG expansion prompts non-AUG-initiated (RAN) translation of mainly FMRpolyG, which accumulates in a large ubiquitin-positive inclusion body in the nervous system, and Buijsen et al.33 reported inclusions in ovarian stromal cells, but not in follicles of female FMR1 premutation carriers. In a recent study in our laboratory evaluating the suitability of premutation-transfected COV434 cells as a disease model, we noted similar FMRpolyG expression to MGCs from FMR1 premutation carriers34. In the present study, we used the transfected COV434 disease models (99 CGG repeats with or without the ability to express the FMRpolyG protein) to investigate the expression of AMH. Immunostaining and western blot revealed significant elevations of AMH elevations regardless of FMRpolyG expression (Fig. 5a–c). Therefore, we postulate that the premutation state (55–200 CGG repeats) might be a primary cause of the overexpression of AMH due to a compensatory mechanism via upregulation of folliculogenesis mediators, and FMRpolyG might not be associated with the dysregulation in AMH expression.
In conclusion, we demonstrated a dysregulation of the folliculogenesis regulators, FSH receptor and AMH. The association between the elevated levels of these regulators and the proposed RNA and protein toxicity mechanisms in FXPOI remains unclear. The present study is an important step in elucidating the consequences of the FMR1 premutation range and should facilitate future studies of the pathophysiology of FXPOI. The findings may have implications for improving the early detection of deteriorating fertility and developing IVF treatments tailored to FMR1 premutation carriers.
Material and methods
Experimental model and subject details
Mural granulosa cells (MGCs) of women undergoing IVF treatments.
Ethics approval was granted by the Institutional Ethics Review Board of Sheba Medical Center, Israel (8707-11-SMC and 6140-19-SMC), and all patients provided written informed consent. In Israel, all women are encouraged to undergo genetic testing before conceiving, including FMR1 CGG carrier status. Therefore, the CGG repeat number is known for all FMR1 premutation carriers (55–200 CGG repeats) and noncarriers (< 55 CGG repeats). FMR1 premutation carriers are often referred for IVF with pre-implantation genetic testing (PGT) to exclude embryos with pathological CGG expansion.
The study group included 12 FMR1 premutation carriers referred for IVF-PGT who reached the ovum pick-up (OPU) stage. For the control group, the study patients were age-matched with 17 noncarriers undergoing IVF-intracytoplasmic sperm injection (ICSI) for male infertility during the same period at the same hospital. The controlled ovarian hyperstimulation (COH) protocol was determined by the treating physician. Variable doses of gonadotropins were administrated according to the woman's age and ovarian response in the previous treatment cycle. Doses were further adjusted on the basis of serum estradiol (E2) levels and follicle diameters measured by vaginal ultrasound every 2 or 3 days. Oocyte aspiration was performed under ultrasound guidance by the transvaginal route 36–38 h after human chorionic gonadotropin (HCG) injection. Mural granulosa cells (MGCs) were collected from pooled follicular fluids of each woman in both groups. The basic clinical and IVF treatment cycle characteristics are shown in Table 1.
COV434 cell line for transfection
The human ovarian granulosa tumor cell line COV434 was purchased from Sigma-Aldrich (cat. No. ECACC 07071909; St. Louis, MO, USA) maintained according to the manufacturer’s instructions.
Mural granulosa cell culture
MGC culture was performed as previously described by our group33,34. MGCs from follicular fluid were washed and plated on plastic tissue culture plates containing Dulbecco’s Minimum Essential Medium (DMEM) with 5% fetal bovine serum, 1% l-Glutamine, and 1% penicillin/streptomycin, all from Biological Industries (Beit Haemek, Israel). Starting at 24 h after seeding, the culture medium was replaced every 24 h for 4 days. Half the cells from each FMR1 premutation carrier were subjected to an additional 48 h of stimulation with 75 U/ml FSH. Cells were incubated at 37 °C in a humidified atmosphere of 5% CO2 in air.
Transfection
Transfection was carried out as previously described33. COV434 cells were transfected with three plasmids generously provided by Dr. Charlet-Berguerand at the Department of Neurobiology and Genetics, University of Strasbourg, Illkirch, France25,31,32. In brief, two of the plasmids contained 99 CGG repeats, one expressing FMRpolyG and one not, in both plasmids the FMRP ORF is GFP-tagged, and the third (control) plasmid contained 20 CGG repeats (Without GFP tag). For the transfection, we used a mixture of 0.5 µg DNA (NucleoBond Xtra Midi Plus Kit, Macherey–Nagel, Duren, Germany), extracted according to the manufacturer's protocol, and 1.5 µl Mirus (Mirus Bio, Madison, WI, USA) at a final volume of 50 µl DMEM (Biological Industries).
RNA isolation and molecular analysis
Total RNA was extracted using TRIzol reagent (Life Technologies, Invitrogen, Rhenium, Modi'in, Israel) followed by cDNA reverse transcription using the qScript cDNA Synthesis Kit (Quanta BioSciences, Beverly, MA, USA).
For real-time qualitative polymerase chain reaction (qPCR) analysis, we used the StepOnePlus System (Applied Biosystems, Waltham, MA, USA) with SYBR Green Fast assay (Invitrogen, Rhenium) under the following cycling parameters: 1 cycle at 95 °C for 20 s, 40 cycles each at 95 °C for 3 s and 60 °C for 30 s. Human beta-actin, a housekeeping gene, served as the control. Transcript expression levels were obtained by the relative quantification (DDCt) method using SDS software (Applied Biosystems).
Primer sequences were as follows:
-
h-AMH_F: GCTGCCTTGCCCTCTCTAC.
-
h-AMH_R: GAACCTCAGCGAGGGTGTT.
-
h-FSHR_F: GAGAGCAAGGTGACAGAGATTCC.
-
h-FSHR_R: CCTTTTGGAGAGAATGAATCTT.
-
h-FMR1_F: AACAAAGGACAGCATCGCTAATG.
-
h-FMR1_R: CAA ACGCAACTGGTCTACTTCCT.
-
h-SAM68_F: GACTATGGACATGGGGAGGTTC.
-
h-SAM68_R: ATTCCAGTCGTCCTGGCCAT.
-
h-LHR_F: AGAGTGAACTGAGTGGCTGG.
-
h-LHR_R: CAACACGGCAATGAGAGTAG.
-
h-b-ACTIN_F: CCTGGACTTCGAGCAAGAGA.
-
h-b-ACTIN_R: CAGCGGAACCGCTCATTGCCAATGG.
Cell fixation and immunofluorescence
The permeabilization protocol consisted of 0.5% Triton X-100 in 4% paraformaldehyde (PFA) for 15 min, followed by incubation in 4% PFA for 20 min to fixate the cells; 5% bovine serum albumin (BSA) blocking solution was used to prevent nonspecific binding. Cells were incubated with the primary AMH antibody (Ab229212, 1:400, Abcam, Cambridge, UK) overnight at 4 °C followed by the secondary antibody (goat anti-rabbit IgG, Alexa Fluor 568, Abcam Ab175471, 1:200 RRID:AB_2576207) for 1 h at room temperature. Nuclear counterstaining was performed using DAPI Fluoromount-G (Southern Biotech, Birmingham, AL, USA). Images were acquired with a confocal microscope (LSM710, Zeiss, Oberkochen, Germany). The identical acquisition parameters were defined for both groups.
Western blot analysis
Transfected COV434 cells were harvested and homogenized with a RIPA buffer, pH 7.4 (BioBasic, Toronto, Canada) containing phosphatase and protease inhibitors (Roche, Basel, Switzerland). A Bicinchoninic Acid Protein Assay Kit (Thermo Scientific, Rockford, IL, USA) was to calculate protein concentrations, and plates were read in a Varioskan multimode plate reader (Thermo Scientific). Criterion XT precast gels (4–20% bis–tris) (Biorad, Hercules, CA, USA) were loaded with 50 µg of total protein per well and transferred to a nitrocellulose membrane. Primary antibodies were anti-AMH (Ab229212, 1:2000, Abcam) and anti-glyceraldehyde 3-phosphate dehydrogenase (GAPDH) (Ab8245; 1:10,000, mouse monoclonal, RRID: AB2107448, Abcam). ChemiDocTM XRS + imager was used to scan the membrane, and Image Lab software (Biorad) assisted in quantifying the intensity of the bands of interest.
Statistical analysis
Parameters were compared between groups using two-tailed unpaired Student's t-test. P values < 0.05 were considered statistically significant. (P values < 0.05 were marked*; < 0.01**; < 0.001***).
All methods were carried out in accordance with relevant guidelines and regulations.
Materials availability
All reagents used in this study are available from the Lead Contact without restriction.
Code availability
This study did not generate any unique datasets or code.
Data availability
All data generated or analyzed during this study are included in this published article or in the data repositories listed in References. Upon request further data will be provided by the Lead Contact, Yoram Cohen (ycohen1@gmail.com).
References
McLennan, Y., Polussa, J., Tassone, F. & Hagerman, R. Fragile x syndrome. Curr. Genom. 12, 216–224 (2011).
Bontekoe, C. J. et al. Instability of a (CGG)98 repeat in the Fmr1 promoter. Hum. Mol. Genet. 10, 1693–1699 (2001).
Hagerman, R. J. et al. Intention tremor, parkinsonism, and generalized brain atrophy in male carriers of fragile X. Neurology 57, 127–130 (2001).
Willemsen, R., Levenga, J. & Oostra, B. A. CGG repeat in the FMR1 gene: size matters. Clin. Genet. 80, 214–225 (2011).
Coffey, S. M. et al. Expanded clinical phenotype of women with theFMR1 premutation. Am. J. Med. Genet. A 146A, 1009–1016 (2008).
Peprah, E. Understanding decreased fertility in women carriers of the FMR1 premutation: A possible mechanism for Fragile X-Associated Primary Ovarian Insufficiency (FXPOI). Reprod. Health 11, 67 (2014).
Hall, D. A. & O’keefe, J. A. Fragile x-associated tremor ataxia syndrome: the expanding clinical picture, pathophysiology, epidemiology, and update on treatment. Tremor Other Hyperkinet. Mov. 2, 1–10 (2012).
Kong, H. E., Zhao, J., Xu, S., Jin, P. & Jin, Y. Fragile X-Associated Tremor/Ataxia Syndrome: From Molecular Pathogenesis to Development of Therapeutics. Front. Cell. Neurosci. 11, 128 (2017).
Allingham-Hawkins, D. J. et al. Fragile X premutation is a significant risk factor for premature ovarian failure: The international collaborative POF in fragile X study: Preliminary data. Am. J. Med. Genet. 83, 322–325 (1999).
Ebrahimi, M. & Asbagh, F. A. Pathogenesis and causes of premature ovarian failure: An update. Int. J. Fertil. Steril. 5, 54–65 (2011).
Murray, A., Ennis, S., MacSwiney, F., Webb, J. & Morton, N. E. Reproductive and menstrual history of females with fragile X expansions. Eur. J. Hum. Genet. 8, 247–252 (2000).
Parrott, J. A. & Skinner, M. K. Kit-ligand/stem cell factor induces primordial follicle development and initiates folliculogenesis1. Endocrinology 140, 4262–4271 (1999).
Vitt, U. A., McGee, E. A., Hayashi, M. & Hsueh, A. J. W. In vivo treatment with GDF-9 stimulates primordial and primary follicle progression and theca cell marker CYP17 in ovaries of immature rats. Endocrinology 141, 3814–3820 (2000).
Durlinger, A. L. L. et al. Anti-Müllerian hormone attenuates the effects of FSH on follicle development in the mouse ovary. Endocrinology 142, 4891–4899 (2001).
Kumar, T. R., Wang, Y., Lu, N. & Matzuk, M. M. Follicle stimulating hormone is required for ovarian follicle maturation but not male fertility. Nat. Genet. 15, 201–204 (1997).
Visser, J. A. & Themmen, A. P. N. Anti-Müllerian hormone and folliculogenesis. Mol. Cell. Endocrinol. 234, 81–86 (2005).
Dewailly, D. et al. Interactions between androgens, FSH, anti-Müllerian hormone and estradiol during folliculogenesis in the human normal and polycystic ovary. Hum. Reprod. Update 22, 709–724 (2016).
Xu, J., Bishop, C. V., Lawson, M. S., Park, B. S. & Xu, F. Anti-Müllerian hormone promotes pre-antral follicle growth, but inhibits antral follicle maturation and dominant follicle selection in primates. Hum. Reprod. 31, 1522–1530 (2016).
Mcgee, E. A. et al. Müllerian inhibitory substance induces growth of rat preantral ovarian follicles 1. Biol. Reprod. 64, 293–298 (2001).
Durlinger, A. L. L., Visser, J. A. & Themmen, A. P. N. Regulation of ovarian function: The role of anti-Müllerian hormone. Reproduction 124, 601–609 (2002).
Salmon, N. A., Handyside, A. H. & Joyce, I. M. Oocyte regulation of anti-Müllerian hormone expression in granulosa cells during ovarian follicle development in mice. Dev. Biol. 266, 201–208 (2004).
Kedem, A. et al. Anti Müllerian Hormone (AMH) level and expression in mural and cumulus cells in relation to age. J. Ovarian Res. https://doi.org/10.1186/s13048-014-0113-3 (2014).
Kedem-Dickman, A. et al. Anti-Müllerian hormone is highly expressed and secreted from cumulus granulosa cells of stimulated preovulatory immature and atretic oocytes. Reprod. Biomed. Online 24, 540–546 (2012).
Sellier, C. et al. The multiple molecular facets of fragile X-associated tremor/ataxia syndrome. J. Neurodev. Disord. 6, 23 (2014).
Sellier, C. et al. Translation of expanded CGG repeats into FMRpolyG is pathogenic and may contribute to fragile X tremor ataxia syndrome. Neuron 93, 331–347 (2017).
Jin, P. et al. Pur alpha binds to rCGG repeats and modulates repeat-mediated neurodegeneration in a Drosophila model of fragile X tremor/ataxia syndrome. Neuron 55, 556–564 (2007).
Hagerman, P. Fragile X-associated tremor/ataxia syndrome (FXTAS): Pathology and mechanisms. Acta Neuropathol. 126, 1–19 (2013).
Sofola, O. A. et al. RNA-binding proteins hnRNP A2/B1 and CUGBP1 suppress fragile X CGG premutation repeat-induced neurodegeneration in a drosophila model of FXTAS. Neuron 55, 565–571 (2007).
Bianchi, E. et al. Ablation of the Sam68 gene impairs female fertility and gonadotropin-dependent follicle development. Hum. Mol. Genet. 19(24), 4886–4894. https://doi.org/10.1093/hmg/ddq422 (2010).
Tassone, F. et al. Elevated FMR1 mRNA in premutation carriers is due to increased transcription. RNA 13, 555–562 (2007).
Elizur, S. E. et al. Elevated levels of FMR1 mRNA in granulosa cells are associated with low ovarian reserve in FMR1 premutation carriers. PLoS ONE 9, e105121 (2014).
Todd, P. K. et al. CGG Repeat-associated translation mediates neurodegeneration in fragile X tremor ataxia syndrome. Neuron 78, 440–455 (2013).
Buijsen, R. A. M. et al. Presence of inclusions positive for polyglycine containing protein, FMRpolyG, indicates that repeat-associated non-AUG translation plays a role in fragile X-associated primary ovarian insufficiency. Hum. Reprod. 31, 158–168 (2016).
Friedman-Gohas, M. et al. FMRpolyG accumulates in FMR1 premutation granulosa cells. J. Ovarian Res. 13, 623 (2020).
Ophir, L. et al. Establishment and validation of a model for non-luteinized human mural granulosa cell culture. Mol. Cell. Endocrinol. 384, 165–174 (2014).
Acknowledgements
We are thankful for the assistance of N. Charlet-Berguerand and C. Sellier, Department of Neurobiology and Genetics, University of Strasbourg, Illkirch, France, who kindly provided the antibody against FMRpolyG, the plasmids used for the transfection, and wise substantial counsel. We also thank the patients included in this study for their valuable contribution.
Funding
The Azrieli Foundation Canada-Israel generously supported this research.
Author information
Authors and Affiliations
Contributions
M.F.-G. designed and performed the experiments, examined and analyzed the results, wrote and edited the first draft, proofread the paper, and took part in discussions regarding the results. R.O. analyzed the results, provided oversight and assisted in manuscript editing, proofread the paper, and took part in discussions regarding the results and critical review. A.M. conducted the experiments and assisted in analysis of the results. A.A. assisted in collecting the samples, proofread the paper, and took part in discussions regarding the results. M.K. analyzed the results, provided oversight and assisted in manuscript editing, proofread the paper, and took part in discussions regarding the results. Y.C. provided oversight and support in development of the research question, analyzed the results and proofread the paper, and took part in discussions regarding the results and critical review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Friedman-Gohas, M., Orvieto, R., Michaeli, A. et al. Dysregulation of anti-Mullerian hormone expression levels in mural granulosa cells of FMR1 premutation carriers. Sci Rep 11, 14139 (2021). https://doi.org/10.1038/s41598-021-93489-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93489-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.