Abstract
Pregnant women may be at higher risk of severe complications associated with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which may lead to obstetrical complications. We performed a case control study comparing pregnant women with severe coronavirus disease 19 (cases) to pregnant women with a milder form (controls) enrolled in the COVI-Preg international registry cohort between March 24 and July 26, 2020. Risk factors for severity, obstetrical and immediate neonatal outcomes were assessed. A total of 926 pregnant women with a positive test for SARS-CoV-2 were included, among which 92 (9.9%) presented with severe COVID-19 disease. Risk factors for severe maternal outcomes were pulmonary comorbidities [aOR 4.3, 95% CI 1.9–9.5], hypertensive disorders [aOR 2.7, 95% CI 1.0–7.0] and diabetes [aOR2.2, 95% CI 1.1–4.5]. Pregnant women with severe maternal outcomes were at higher risk of caesarean section [70.7% (n = 53/75)], preterm delivery [62.7% (n = 32/51)] and newborns requiring admission to the neonatal intensive care unit [41.3% (n = 31/75)]. In this study, several risk factors for developing severe complications of SARS-CoV-2 infection among pregnant women were identified including pulmonary comorbidities, hypertensive disorders and diabetes. Obstetrical and neonatal outcomes appear to be influenced by the severity of maternal disease.
Similar content being viewed by others
Introduction
Altered immunity, reduced respiratory capacity, vascular and hemodynamic changes put pregnant women at higher risk of complications, while specific harm to the exposed fetus/newborn may be observed. Although, early reports from the SARS-CoV-2 epidemic1 suggested that the clinical course for infected pregnant women was similar to the general population, more recent data suggest a higher risk of severe outcomes in pregnant women compared to the general population at an equivalent age, with severe outcomes observed in 8 to 11%2,3,4,5,6. In the general population, preexisting health conditions, namely pulmonary pathologies, hypertension and diabetes have been associated with severe outcomes7,8. Information on the impact of these determinants on the maternal disease evolution and other risk factors specific to pregnancy is still fragmented, although evidence suggest that they might contribute to the severity of the disease6,9. Furthermore, fetal/newborn risks still need to be better assessed as vertical transmission of the virus and placental infection appears to be possible with newborns potentially demonstrating related symptoms10,11,12,13, while a significantly higher rate of preterm deliveries (25–30%) among women with Coronavirus disease 19 (COVID-19) has been reported3,4.
Information on specific risks among pregnant women are urgently needed to provide evidence-based guidelines for the management of this vulnerable population. To accomplish this, we developed an international web registry14 in March 2020, to promote a structured collection of data regarding pregnant women and their fetuses exposed to SARS-CoV-2. Using this dataset, we performed a case–control study to assess the risk of severe maternal outcomes and associated risk factors as well as a description of pregnancy/neonatal outcomes stratified for the severity of the disease among pregnant women with a confirmed SARS-CoV-2 infection.
Materials and methods
Study setting and population
The patients enrolled in this study are part of the COVI-Preg international registry investigating the consequences of SARS-Cov-2 infection during pregnancy14. All pregnant women tested for SARS-CoV-2 infection at any stage of gestation were eligible for inclusion in this multicenter study except those < 18 years of age as well as individuals declining to consent or not able to consent for themselves. Informed oral or written consent was obtained for all participants. Deidentified data were prospectively recorded by each center (Table S1) using the REDCap (Research Electronic Data Capture) electronic data capture tool15,16. Quality checks were performed as described in the Supplementary Materials. Using this dataset, we performed a case control study among pregnant women with a confirmed SARS-CoV-2 infection.
The study was approved by both the Swiss Ethical Board (CER-VD-2020-00548) and the local ethics boards at each participating center. The study was conducted from March 24th to July 26th, 2020. All methods were carried out in accordance with relevant guidelines and regulations in the manuscript.
Inclusion criteria and SARS-CoV-2 status
Pregnant women were tested for SARS-CoV-2 either because of a suspected infection due to ongoing symptoms compatible with COVID-19 or an history of potential exposure or through routine systematic screening instituted during the pandemic in some hospitals depending on local capacities and guidelines. Maternal testing was performed using a nasopharyngeal RT-PCR for SARS-CoV-2 swab test. Pregnant women with a positive RT- PCR test result at any stage during pregnancy irrespective of clinical signs and symptoms were considered as having a confirmed infection and included in the present study. Pregnant women with a SARS-CoV-2 negative test and no other positive test result during the entire follow-up period were excluded.
Case and control definition
Pregnant women with severe adverse outcomes, defined as any of the following: (1) the need for advanced oxygen support (i.e. high flow cannula, non-invasive ventilation through CPAP or mechanical ventilation), (2) admission to the intensive care unit (ICU) and (3) maternal death, were classified as cases. The control group included pregnant women with either mild adverse outcomes, defined as maternal hospitalization requiring oxygen supplementation, or no adverse outcomes, defined as outpatient management or hospitalization not requiring oxygen supplementation.
Identification of risk factors for severe adverse maternal outcome
Pregnant women with severe adverse outcomes (cases) were compared to pregnant women with mild or no adverse outcomes (controls). The effect of maternal characteristics known to be risk factors7,8,17 for SARS-CoV-2 severe adverse outcomes in the general population were tested (i.e. maternal age > 35 years old, obesity defined as a BMI > 30, hypertensive disorders, pre-and gestational diabetes, preexisting pulmonary, cardiovascular, renal, or oncologic disease and immunosuppression), as well as pregnancy related risk factors such as nulliparity (dichotomized as yes/no), ethnicity (defined as Caucasian yes/no), multiple pregnancy, gestational age at infection (dichotomized as < or > 20 WG)9.
Secondary outcomes: absolute risk (%) of obstetrical outcomes and neonatal outcomes
For completed pregnancies (i.e. pregnancy ending in either fetal loss > 14 WG or livebirth, obstetrical outcomes (pregnancy outcome, GA at delivery, mode of delivery) and neonatal outcomes (neonatal death, neonatal admission to the ICU (NICU), birthweight and rates of suspected perinatal SARS-CoV-2) were assessed. For multiple gestations (n = 26), the analysis considered the whole pregnancy. Fetal loss was defined as a spontaneous antepartum fetal death > 14 WG (i.e. late miscarriage (14–24 WG) and stillbirth (fetal demise > 24 WG). Suspected perinatal SARS-CoV-2 transmission was defined as a positive RT-PCR result performed at birth.
Statistical analysis
We performed a multivariate analysis to estimate odds ratios (OR) with 95% CIs adjusting for risk factors of COVID-19 severity (i.e. maternal age, BMI, pre- and gestational hypertensive disorders (including pre-eclampsia), pre-and gestational diabetes, pre-existent pulmonary comorbidities, other pre-gestational comorbidities (cardiovascular, renal, oncological diseases and immunosuppression), and gestational risk factors of severe maternal outcomes (ethnicity, parity, pregnancy conditions (threatened preterm labor, placenta previa, placental malfunction and PPROM) and exposure after 20WG) and accounting for missing values as described in the supplementary material.
Statistical analyses were performed using Stata 14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). A P value less than 0.05 was considered as statistically significant.
Results
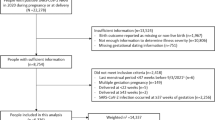
Between March 24 and July 26, 2020, 1079 pregnant women tested for SARS-CoV-2 were enrolled in the registry among which 926 had a confirmed SARS-CoV-2 infection (Fig. 1). Socio-demographic characteristics are presented in Table 1. A third of the women were asymptomatic (31.9% n = 295/926), while cough (40.4%, n = 374/926), fever (32.4%, n = 300/926) and anosmia/ageusia (17.8%, n = 165/926) were the most reported symptoms. 9.9% (n = 92/926) experienced severe maternal outcomes, including 7.3% (n = 68/926) requiring advanced oxygen support and 4.0% (n = 37/926) requiring ICU admission; 6 maternal deaths were recorded (0.6%) (Table 2).
Flow chart. The COVI-Preg international registry was launched in March 2020. To date, 120 centers from 16 countries have contributed patients (supplementary Table 1). All pregnant women tested for SARS-CoV-2 infection at any stage of gestation were eligible for inclusion in this multicenter study except those < 18 years of age as well as individuals declining to consent or not able to consent for themselves. Deidentified data were prospectively recorded by each center using the REDCap (Research Electronic Data Capture) electronic data capture tool15,16. At inclusion (i.e. at the time of SARS-CoV-2 screening), the following data were recorded: socio-demographic characteristics, obstetrical history and information on SARS-CoV-2 exposure. Pregnancies were monitored as clinically indicated according to local protocols. After inclusion, the following data were collected: results of maternal testing (SARS-CoV-2 and/or other infectious pathogens), COVID-19 history, maternal, pregnancy and neonatal outcomes. Data were analyzed using Stata 14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). SARS-CoV-2, severe acute respiratory syndrome coronavirus 2WG, weeks ‘gestation.
Risk factors for severe maternal outcomes among positive pregnant women
In a univariate analysis pulmonary comorbidities [crude OR 3.9, 95% CI 1.6–8.9], hypertensive disorders [crude OR 3.5, 95% CI 1.2–9.1], diabetes [crude OR 2.6, 95% CI 1.2–5.3] and BMI > 30 [crude OR 1.7, 95% CI 1.1–2.9] were significantly associated with an increased risk of severe maternal outcomes (Table 3). In a multivariate analysis adjusting for risk factors of COVID-19 severity, gestational risk factors of severe maternal outcomes, and accounting for missing values through multiple imputation, pulmonary comorbidities [aOR 4.3, 95% CI 1.9–9.5], hypertensive disorders [aOR 2.7, 95% CI 1.0–7.0] and diabetes [2.2, 95% CI 1.1–4.5] remained significantly associated, while BMI > 30 did not retain significance [aOR 1.3, 95% CI 0.8–2.2]. When adjusting for COVID-19 risk factors only, similar results were obtained (Table 3). Common pregnancy related risk factors were not associated with severe maternal outcomes (i.e. nulliparity, ethnicity, multiple pregnancy, gestational age at infection).
Secondary outcomes
Absolute risk of pregnancy, obstetrical and neonatal outcomes
No differences were observed in terms of livebirth rate among positive women with severe adverse outcomes (i.e. cases) compared to women with no or mild adverse outcomes (i.e. controls) [absolute rate 92.6% (n = 75/81) compared to 98.1% (n = 656/669)] (Table 4), although a trend toward poorer obstetrical outcomes was observed among women with severe adverse outcomes [absolute rate of fetal loss > 14 WG 7.4% (n = 6/81) compared to 1.9% (n = 13/669)]. An increased risk of caesarean section was observed among patients with severe adverse outcomes [absolute caesarean sections rate 70.7% (n = 53/75) compared to 30.9% (n = 203/656)]. Similarly, women with severe maternal outcomes were at increased risk of preterm delivery < 37WG [absolute risk 62.7% (n = 32/51) compared to 36.3% (78/215)] and < 34 WG [absolute risk 51.9% (n = 14/27) compared to 20.5% (24/117)], most of which were iatrogenic [81.3% (n = 26/32) and 85.7% (n = 12/14), respectively]. Newborns born to mothers with severe adverse pregnancy outcomes were more frequently admitted to NICU [absolute risk 41.3% (n = 31/75) compared to 11.6% (n = 76/656)]. The most frequent reasons for admission were prematurity [71.0% (n = 22/31)] and respiratory distress [48.5% (n = 15/31)] (Table 4). A positive SARS-CoV-2 test at birth was observed in 2.9% of neonates (n = 11/384).) The rates of suspected perinatal transmission and reduced birthweight were similar between newborns born to mothers with severe outcomes compared to those with no or mild outcomes.
Discussion
In this study, we present the largest cohort of pregnant women tested for SARS-Cov-2 worldwide and the first analysis of primary data stratified by the severity of maternal disease, allowing us to identify specific risk factors associated with adverse maternal outcomes.
Severe adverse outcomes, defined by maternal death, admission to ICU and/or advanced oxygen support were observed in 9.9% of cases. Pulmonary comorbidities, hypertensive disorders and diabetes mellitus were significantly associated with an increased risk of severe maternal outcomes, while usual pregnancy related risk factors were not. No difference in the livebirth rate was observed between pregnant women with severe adverse outcomes and patients with an uncomplicated course. Nevertheless, a significant increased risk of caesarean section, preterm birth and neonatal admission to the intensive care unit was observed, highlighting that obstetrical and neonatal outcomes are influenced by the severity of maternal disease.
The rate of severe disease observed here is similar to what has been previously reported in other large cohorts3,4,5 and summarized in a recent meta-analysis6,where the risk of severe disease among pregnant women with COVID-19 was estimated to be 13% (95%CI 6–21%). Importantly, this risk of severe maternal complications appears significantly higher when compared to a non-pregnant population at an equivalent age, with an increased odds of ICU admission or mechanical ventilation up to 1.6 (95%CI 1.3–2.0) and 1.9 (95%CI 1.4–2.6) respectively6.
Risk factors for severe maternal disease appear to be similar to what has been previously described in the general population, namely pulmonary pathologies, hypertension and diabetes7,8. Congruently, in their meta-analysis, Allotey et al. observed an increased risk of severe disease among pregnant women > 35 y.o., those with chronic hypertension, pre-existing diabetes, or body mass index > 306. Interestingly, in our study, after adjustment, obesity was not independently associated with an increased risk of severe adverse outcomes. This could be explained by the fact that overweight patients often suffer from hypertension and diabetes (metabolic syndrome), which could act as the predominant causal factors. Both are associated with macro- and micro-vascular complications, and endothelial dysfunction has been suggested as a major pathophysiological mechanism associated with COVID-19 severity18,19. In pregnancy, endothelial change is a well-known mechanism of obstetrical complications, such as gestational hypertension, HELLP (Hemolysis, elevated liver enzymes, low platelets) and pre-eclampsia20, and may contribute to the increased risk of COVID-19 complications. In our study, we did not observe any association with maternal age. This could be explained by the low number of patients > 35 y.o. included. Similarly, ethnicity (non-Caucasian versus Caucasian) was not associated with poorer outcomes, unlike previously described21.
We observed a 2.9% rate of positive test among newborns born to mothers with a positive SARS-CoV-2 test. The clinical relevance of this finding remains unclear, as, at the time of the study, we were lacking comprehensive data regarding COVID-related symptoms or COVID-suspected symptoms among newborns, repeated testing and long-term follow-up. Perinatal transmission of SARS-CoV-2 has been reported by others, both in case of vaginal and cesarean sections, and was associated in some cases with neonatal symptoms1,4,22. In all reported cases, the possibility of postnatal infection through contacts with parents or medical personal remains difficult to exclude1,4. Alternatively, transplacental transmission has been suspected in few cases, where specific IgM were detected among newborns23,24. Nevertheless, perinatal/vertical transmission appear to be rare and mainly associated with good neonatal outcomes1,4,23,24.
Our study has several limitations. First, we present here the outcomes among pregnant women with a confirmed SARS-CoV-2 infection and therefore only observational conclusions can be drawn regarding the absolute risks of severe disease and adverse obstetrical/neonatal outcomes, as a control group of negative patients was not included. Nevertheless, this was beyond the scope of the present study, whose first aim was to identify specific risk factors.
Second heterogeneities exist between participating centers in the testing of pregnant women. While some centers performed routine systematic screening of presenting women independently of compatible symptoms, other only tested symptomatic pregnant women. This could have led to a selections bias of more severe symptomatic COVID-19 cases. If a symptomatic SARS-CoV-2 infection is associated with poorer maternal, obstetrical and neonatal outcomes, this selection bias may have resulted in an overestimation of the absolute risk of adverse outcomes. However, the rate of asymptomatic infections among included positive women of 31.9% (n = 295/926) is quite similar to the rate of asymptomatic infection described in the general population, estimated to range around 40–45%25,26 and suggests a low impact of this potential bias. Similarly, patients admitted with severe disease were very likely systematically tested for SARS-CoV-2, which may have led to a possible overestimation of the actual rate of severe adverse outcome among positive patients. Follow-up analysis, including patients with ongoing pregnancies with an uncomplicated course based on systematic screening will help assess the exact risk in a more general population of pregnant women.
Third, most patients were included during the 3rd trimester of gestation, with the majority included close to delivery, while 130 pregnancies were still ongoing at the time of analysis. Although, we did not observe any impact of the gestational age (i.e. > 20 WG) on the severity of maternal disease, this could be related to a lack of statistical power. Pregnancy-related vascular complications only occur after 20 WG, which would suggest an increased risk of maternal complications in cases of maternal infection at a later stage of the pregnancy, as observed by others9. In our cohort, severe maternal outcomes were also observed in women exposed at < 20 WG, with an overall similar risk (n = 8/89, 9.0%) to what was described in the whole cohort. Therefore, caution should also be taken with pregnant women infected in early pregnancy.
Although our data regarding obstetrical outcomes are reassuring, definite conclusions cannot be drawn. Infections occurring at an earlier stage of gestation may be associated with poorer obstetrical outcomes. Viral particles have been detected within the placentas of women infected earlier during pregnancy10,12,13,27. Although placental infection seems rare, it has been associated with evidence of malperfusion28,29,30, which is known to be associated with reduced fetal growth and intra-uterine fetal death. Of note, Khalil et al. have shown an increase in the number of stillbirths during the epidemic peak, without being able to determine whether this is a direct effect of the virus31. At the time of analysis, pregnancies < 37WG that were exposed during the 1st and 2nd-trimesters were still ongoing (Fig. 1), suggesting an uncomplicated course. Subsequent analysis, including those patients, are needed to better define obstetrical and neonatal outcomes.
In conclusion, pregnant women, particularly those with associated comorbidities, seem to be at higher risk of severe complications of SARS-CoV-2 infection. Obstetrical and neonatal outcomes appear to be influenced by the severity of maternal disease; complications include caesarean sections, neonatal prematurity and neonatal admission to the intensive care unit. Further studies are needed to assess maternal and neonatal outcomes for cases of earlier exposure.
References
Yu, N. et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: A retrospective, single-centre, descriptive study. Lancet Infect. Dis. 20(5), 559–564 (2020).
Collin, J., Byström, E., Carnahan, A. & Ahrne, M. Public Health Agency of Sweden’s Brief Report: Pregnant and postpartum women with severe acute respiratory syndrome coronavirus 2 infection in intensive care in Sweden. Acta Obstet. Gynecol. Scand. 99, 819–822 (2020).
Knight, M. et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: National population based cohort study. BMJ 369, m2107 (2020).
Martínez-Perez, O. et al. Association between mode of delivery among pregnant women with COVID-19 and maternal and neonatal outcomes in Spain. JAMA https://doi.org/10.1001/jama.2020.10125 (2020).
Vivanti, A. J. et al. Retrospective description of pregnant women infected with severe acute respiratory syndrome coronavirus 2, France. Emerg. Infect. Dis. 26, 2069 (2020).
Allotey, J. et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 370, m3320 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395, 1054–1062 (2020).
Petrilli, C. M. et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 369, m1966 (2020).
Badr, D. A. et al. Are clinical outcomes worse for pregnant women ≥ 20 weeks’ gestation infected with COVID-19? A multicenter case-control study with propensity score matching. Am. J. Obstet. Gynecol. https://doi.org/10.1016/j.ajog.2020.07.045 (2020).
Sisman, J. et al. Intrauterine transmission of SARS-COV-2 infection in a preterm infant. Pediatr. Infect. Dis. J. https://doi.org/10.1097/INF.0000000000002815 (2020).
Zeng, L. et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2020.0878 (2020).
Baud, D. et al. Second-trimester miscarriage in a pregnant woman with SARS-CoV-2 infection. JAMA https://doi.org/10.1001/jama.2020.7233 (2020).
Algarroba, G. N. et al. Visualization of severe acute respiratory syndrome coronavirus 2 invading the human placenta using electron microscopy. Am. J. Obstet. Gynecol. 223, 275–278 (2020).
Panchaud, A. et al. An international registry for emergent pathogens and pregnancy. Lancet 395, 1483–1484 (2020).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
Harris, P. A. et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 95, 103208 (2019).
CDC COVID-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12-March 28, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 382–386 (2020).
Monteil, V. et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell 181, 905-913.e7 (2020).
Varga, Z. et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet 395, 1417–1418 (2020).
Roberts, J. M. et al. Preeclampsia: An endothelial cell disorder. Int. J. Gynecol. Obstet. 32, 299–299 (1990).
Sze, S. et al. Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 29, 100630 (2020).
Wang, S. et al. A case report of neonatal COVID-19 infection in China. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa225 (2020).
Dong, L. et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA https://doi.org/10.1001/jama.2020.4621 (2020).
Zeng, H. et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA https://doi.org/10.1001/jama.2020.4861 (2020).
Oran, D. P. & Topol, E. J. Prevalence of asymptomatic SARS-CoV-2 infection: A narrative review. Ann. Intern. Med. https://doi.org/10.7326/M20-3012 (2020).
Lavezzo, E. et al. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo’. Nature https://doi.org/10.1038/s41586-020-2488-1 (2020).
Penfield, C. A. et al. Detection of SARS-COV-2 in placental and fetal membrane samples. Am. J. Obstet. Gynecol. MFM 100133, 438. https://doi.org/10.1016/j.ajogmf.2020.100133 (2020).
Prabhu, M. et al. Pregnancy and postpartum outcomes in a universally tested population for SARS-CoV-2 in New York City: A prospective cohort study. BJOG https://doi.org/10.1111/1471-0528.16403 (2020).
Shanes, E. D. et al. Placental pathology in COVID-19. Am. J. Clin. Pathol. 154, 23–32 (2020).
Hosier, H. et al. SARS-CoV-2 infection of the placenta. J. Clin. Investig. https://doi.org/10.1172/JCI139569 (2020).
Khalil, A. et al. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA https://doi.org/10.1001/jama.2020.12746 (2020).
Acknowledgements
We thank all patients, midwives and nurses involved in this project for their contribution and for providing crucial help in data management, data entry and ethical procedures, especially Mrs Karine Lepigeon and Caroline Lombard (Lausanne University Hospital), Véronique Othenin-Girard, Marika Santagata and Monia Moreau (Geneva University Hospital).
Author information
Authors and Affiliations
Contributions
M.V., G.F., O.M.P., L.P., D.B. and A.P. conceived and designed COVI-Preg. All authors (n = 129) provided cases in COVI-Preg. M.V. and A.P. performed the statistical analysis. M.V., G.F., L.P., D.B. and A.P. interpreted the results, did the literature review and wrote the first draft. All authors provided critical inputs to the paper, reviewed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vouga, M., Favre, G., Martinez-Perez, O. et al. Maternal outcomes and risk factors for COVID-19 severity among pregnant women. Sci Rep 11, 13898 (2021). https://doi.org/10.1038/s41598-021-92357-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-92357-y
This article is cited by
-
Neonatal outcomes of maternal prenatal coronavirus infection
Pediatric Research (2024)
-
Management of neonates with maternal prenatal coronavirus infection and influencing factors
Pediatric Research (2024)
-
Die Schwangere mit COVID-19-ARDS auf der Intensivstation
Die Anaesthesiologie (2024)
-
Late miscarriage and stillbirth in asymptomatic and symptomatic hospitalised pregnant women in Belgium during the first and second waves of COVID-19: a prospective nationwide population-based study
BMC Pregnancy and Childbirth (2023)
-
Timing and severity of COVID-19 during pregnancy and risk of preterm birth in the International Registry of Coronavirus Exposure in Pregnancy
BMC Pregnancy and Childbirth (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.