Abstract
Objective
Characterize the prevalence of coronavirus disease 2019 (COVID-19) diagnosis among mothers with infants hospitalized in 294 neonatal intensive care units (NICUs), and demographics and outcomes of infants with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exposure in utero.
Study design
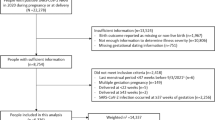
Cohort study of infants discharged from NICUs 01/2020–09/2021. We defined groups based on infant diagnosis, infant testing, and maternal SARS-CoV-2 infection status. We compared demographics, clinical characteristics, and outcomes.
Results
Of 150,924 infants, 94% had no COVID-related diagnosis or test; 247 (0.2%) infants tested positive for COVID-19 and were more likely to require mechanical ventilation. Infants with unknown maternal status and negative testing were more commonly premature, outborn, and had longer hospitalizations.
Conclusion
In this large cohort of hospitalized infants, most had no known exposure to COVID-19. Adverse outcomes and mortality were rare. Further studies are needed to evaluate the long-term effects of COVID-19 in this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Centers for Disease Control and Prevention. COVID Data Tracker. [Updated 2023 March 7] https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed 8 March 2023.
Lopez L 3rd, Hart LH 3rd, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325:719–20.
Jamieson DJ, Rasmussen SA. An update on COVID-19 and pregnancy. Am J Obstet Gynecol. 2022;226:177–86.
Walter K. COVID-19 and pregnancy. JAMA. 2022;327:790.
Sankaran D, Nakra N, Cheema R, Blumberg D, Lakshminrusimha S. Perinatal SARS-CoV-2 infection and neonatal COVID-19: a 2021 update. Neoreviews. 2021;22:e284–95.
Di Toro F, Gjoka M, Di Lorenzo G, De Santo D, De Seta F, Maso G, et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27:36–46.
Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID multinational cohort study. JAMA Pediatr. 2021;175:817–26.
Abu-Raya B. Vaccination of pregnant women against COVID-19. Neoreviews. 2021;22:e570–3.
Angelidou A, Sullivan K, Melvin PR, Shui JE, Goldfarb IT, Bartolome R, et al. Association of maternal perinatal SARS-CoV-2 infection with neonatal outcomes during the COVID-19 pandemic in Massachusetts. JAMA Netw Open. 2021;4:e217523.
Spitzer AR, Ellsbury DL, Handler D, Clark RH. The Pediatrix BabySteps Data Warehouse and the Pediatrix QualitySteps improvement project system–tools for "meaningful use" in continuous quality improvement. Clin Perinatol. 2010;37:49–70.
Athiraman NK, Patience A, Onwuneme C, Zalewski S, Skeath T. Impact of COVID-19 on maternity and neonatal services—three year-on-year review data from the North East of England. Acta Paediatr. 2022;111:1039–41.
Devin J, Marano R, Mikhael M, Feaster W, Sanger T, Ehwerhemuepha L. Epidemiology of neonatal COVID-19 in the United States. Pediatrics. 2022;150:e2022056297.
Smith V, Seo D, Warty R, Payne O, Salih M, Chin KL, et al. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PLoS One. 2020;15:e0234187.
Hudak ML, Flannery DD, Barnette K, Getzlaff T, Gautam S, Dhudasia MB, et al. Maternal and newborn hospital outcomes of perinatal SARS-CoV-2 infection: a national registry. Pediatrics. 2023;151:e2022059595.
Buonsenso D, Costa S, Giordano L, Priolo F, Colonna AT, Morini S, et al. Short- and mid-term multidisciplinary outcomes of newborns exposed to SARS-CoV-2 in utero or during the perinatal period: preliminary findings. Eur J Pediatr. 2022;181:1507–20.
Raman R, Patel KJ, Ranjan K. COVID-19: unmasking emerging SARS-CoV-2 variants, vaccines and therapeutic strategies. Biomolecules. 2021;11:993.
Funding
This work was supported by Duke Clinical Research Institute’s R25 Summer Training in Academic Research (STAR) Program (grant #5R25HD076475-09). This work was also funded by a COVID-19 Supplement (3U24TR001608-05S2), in part by the Duke University-Vanderbilt University Medical Center Trial Innovation Center (U24TR001608), and by the Vanderbilt University Medical Center Recruitment Innovation Center (U24TR001579), which is part of the National Center for Advancing Translational Sciences (NCATS) Trial Innovation Network. This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
EBH conceptualized and designed the study, and contributed to the data interpretation, the drafting of the initial manuscript, and reviewing and revising the manuscript. RHC contributed to the data interpretation and the critical revision of the manuscript for important intellectual content. PBS contributed to the data interpretation and the critical revision of the manuscript for important intellectual content. DKB contributed to the data interpretation and the critical revision of the manuscript for important intellectual content. KOZ contributed to the data interpretation and the critical revision of the manuscript for important intellectual content. KAA contributed to the data interpretation and the critical revision of the manuscript for important intellectual content. CKB contributed to the data interpretation and the critical revision of the manuscript for important intellectual content. HW contributed to the data interpretation and the manuscript drafting. RS contributed to the data interpretation and the manuscript drafting. AB contributed to the data interpretation and the manuscript drafting. CON contributed to the data interpretation and the manuscript drafting. JA contributed to the data interpretation and the manuscript drafting. ON contributed to the data interpretation and the manuscript drafting. RGG contributed to the conception and design of the study, supervised the drafting of the manuscript, interpreted the data analyses, and reviewed and revised the manuscript. RGGreenberg had full access to all the data and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
RGG has received support from industry for research services (https://dcri.org/about-us/conflict-of-interest/). The authors have no other conflicts of interest relevant to this article to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
High school or college student affiliated with the Duke Clinical Research Institute’s R25 Summer Training in Academic Research (STAR) Program: Hannah Won, Rachel Ssengonzi, Avi Belbase, Courage O. Ndalama, Jennifer An, Ogugua Nwaezeigwe.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heyward, E.B., Clark, R.H., Smith, P.B. et al. Trends in COVID-19 diagnoses and outcomes in infants hospitalized in the neonatal intensive care unit. J Perinatol 44, 35–39 (2024). https://doi.org/10.1038/s41372-023-01725-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01725-1