Abstract
About 2.6 million third-trimester stillbirths occur annually worldwide, mostly in low- and middle-income countries. However, the causes of stillbirths are rarely investigated. We performed a retrospective, hospital-based study in Zhejiang Province, southern China, of the causes of third-trimester stillbirths. Causes of stillbirths were classified using the Relevant Condition at Death classification system. From January 1, 2013, to December 31, 2018, we enrolled 341 stillbirths (born to 338 women) from 111,275 perinatal fetuses (born to 107,142 women), as well as 293 control cases (born to 291 women). The total incidence of third-trimester stillbirths was 3.06/1000 (341/111,275). There were higher proportions of women with a high body mass index, twins, pregnancy-induced hypertension, assisted reproduction and other risk factors among the antepartum than the control cases. The antepartum stillbirth fetuses were of lower median birth weight and gestational age and had a smaller portion of translucent amniotic fluid than the control cases. The antepartum stillbirth fetuses had a higher frequency of abnormalities detected prenatally and of fetal growth restriction than the control cases. Of 341 cases (born to 338 mothers), the most common causes of stillbirth were fetal conditions [117 (34.3%) cases], umbilical cord [88 (25.8%)], maternal conditions [34 (10.0%)], placental conditions [31 (9.1%)], and intrapartum [28 (8.2%)]. Only eight (2.3%), three (0.9%), and two (0.6%) stillbirths were attributed to amniotic fluid, trauma, and uterus, respectively. In 30 (8.8%) cases, the cause of death was unclassified. In conclusion, targeted investigation can ascertain the causes of most cases of third-trimester stillbirths.
Similar content being viewed by others
Introduction
Stillbirth refers to intrauterine death of the fetus during pregnancy or parturition, who was delivered without any vital signs. The rate of stillbirths is an important indicator of the obstetric quality and comprehensive medical strength of a country or region. Although the stillbirth rate decreased from 2000 to 2015, there were 4.8 million perinatal deaths worldwide in 2015, of which 2.6 million were third-trimester stillbirths and 98% occurred in low- and middle-income countries (LMICs). It was reported that 36% of third-trimester stillbirths occurred in south-Asian LMICs, and 41% in African LMICs1,2. More importantly, stillbirths have marked socioeconomic consequences, including impairment of the physical and mental health of the parents and the financial cost to family and to the healthcare system3. Therefore, the World Health Assembly-endorsed Every Newborn Action Plan acknowledged the need to reduce the number of stillbirths in LMICs, with a target of reducing the number of stillbirths from 18.4 per 1000 births in 2015 to 12 per 1000 births by 20304. As one of the largest LMICs, the total incidence of stillbirths in China is 1–4%, and its number of stillbirths is in the top five worldwide5,6. Therefore, China must improve monitoring and reduce the number of preventable stillbirths.
The most effective means of reducing the incidence of stillbirths is to identify risk factors and provide targeted treatment. Pregnancy complications, such as pre-eclampsia and placental abruption, can lead to stillbirth, as can maternal infection7. However, 25–60% of stillbirths are unexplained8, possibly because of inadequate evaluation9. A systematic review of stillbirths from 2009 to 2016 in LMICs and high-income countries highlighted the poor quality of the data10, which hampers the development of strategies to reduce the incidence of stillbirths. The use of 34 classification systems for the causes of stillbirth undermines our understanding of stillbirth epidemiology. In addition, placental examination was performed, in some cases, in two studies from middle-income countries, but not in 28 studies from low-income countries; that method is useful for identifying risk factors11,12. Few high-quality biological investigations of the risk factors for stillbirths in LMICs have been performed.
The aim of this retrospective study was to investigate the incidence of third-trimester stillbirths and the risk factors thereof among women who attended the Women’s Hospital, Zhejiang University School of Medicine, China, from 2013 to 2018. We wish to provide reliable data that will enable the incidence of preventable stillbirths to be reduced, particularly in LMICs.
Results
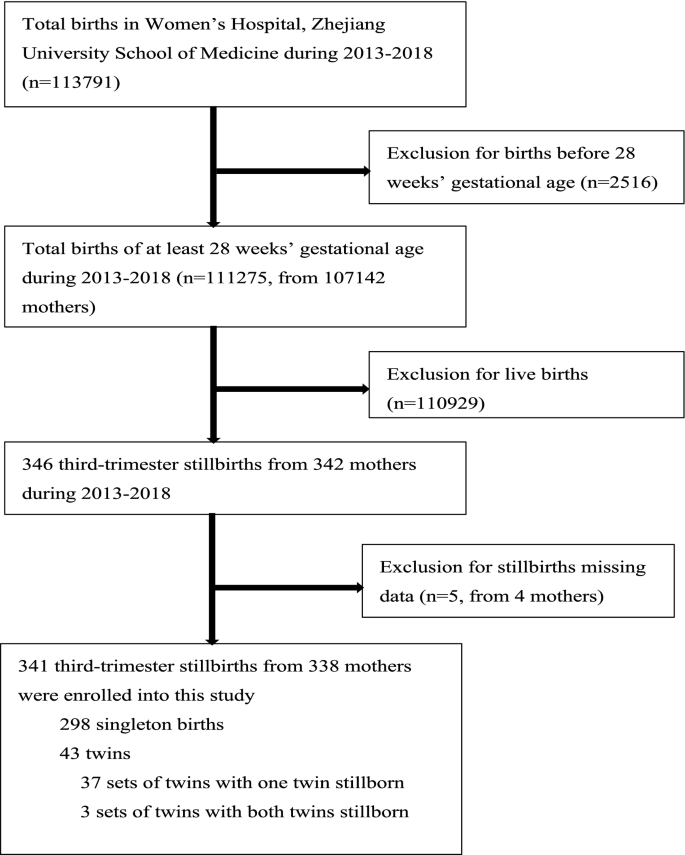
Incidence of third-trimester stillbirths
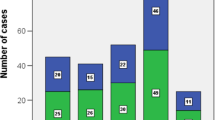
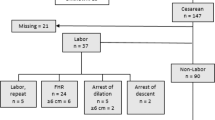
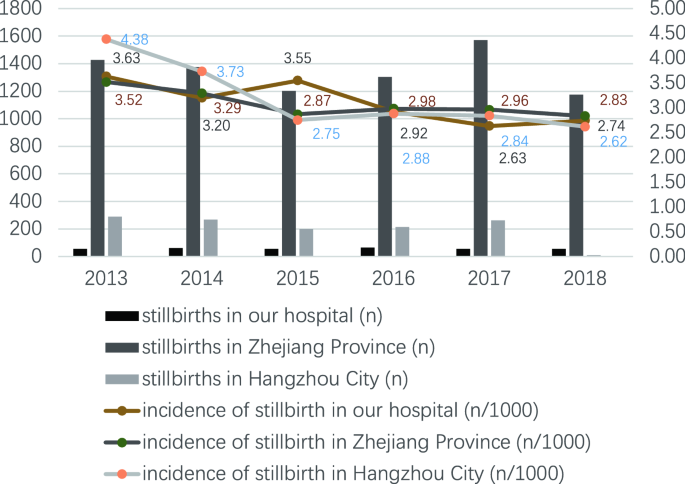
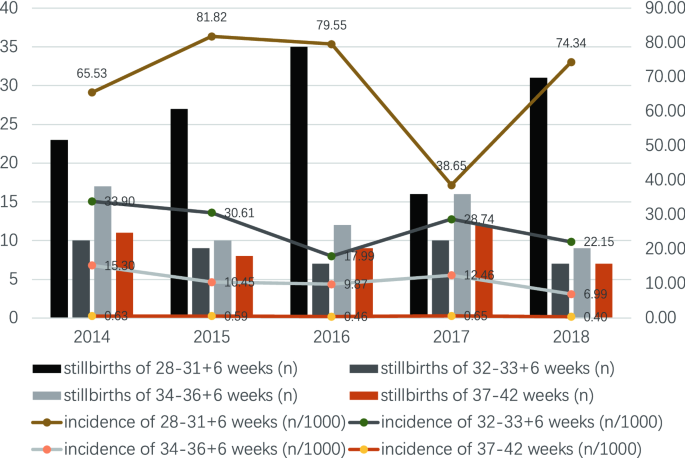
From January 1, 2013, to December 31, 2018, the total number of perinatal fetuses delivered in the Women’s Hospital, Zhejiang University School of Medicine was 111,275 (from 107,142 mothers), of which 341 were third-trimester stillbirths from 338 mothers (Fig. 1). The incidence of third-trimester stillbirths was 3.06/1000 (341/111,275). The lowest incidence was in 2017 (2.63/1000, 54/20,533) and the highest was in 2013 (3.63/1000, 55/15,134) (Fig. 2). The incidence of third-trimester stillbirths was 3.07/1000 in Zhejiang Province and 3.16/1000 in Hangzhou City. Figure 2 also presented the specific incidence from 2013 to 2018. The overall incidence of third-trimester stillbirths decreased with increasing gestational age in the previous 5 years: the highest incidence was 81.82/1000 (27/330) at 28–31 + 6 weeks of gestational age in 2015, and the lowest was 0.4/1000 (7/17,675) at 37–42 weeks of gestation in 2018 (Fig. 3). Moreover, the incidence of third-trimester stillbirths varied according to demographic features (Supplement: Incidence of third-trimester stillbirths in women and fetuses with different demographic features). These features may be risk factors for stillbirth (Table S1). We next analyzed 341 third-trimester stillbirths (338 mothers) and the corresponding controls.
Baseline demographic and clinical features of women who had stillbirths
Of the 338 women who had third-trimester stillbirths from January 1, 2013, to December 31, 2018, 310 were categorized as antepartum cases and the remaining 28 as intrapartum cases; 291 control cases were also analyzed. There were higher proportions of women with a high body mass index (BMI), minority nationality, primary education level, unemployed occupation, and previous inevitable abortion among the antepartum than the control cases. Only three (0.9%) of 338 women had a history of stillbirth (Table 1).
Clinical features during the current pregnancy of women who had stillbirths
There were higher proportions of women with twins, no antenatal care visit, pregnancy-induced hypertension, assisted reproduction, vaginal delivery, and history of preventing miscarriage among the antepartum than the control cases. Pregnancy-induced hypertension included hypertension (12, 3.6%), preeclampsia (10, 3.0%), and severe preeclampsia (32, 9.5%). Of the 338 women, 168 had abnormal fetal movement before diagnosis of stillbirth (Table 2).
Baseline demographic and clinical features of the stillbirths
Of the 341 third-trimester stillbirths (338 mothers), 313 were antepartum cases and 28 were intrapartum cases; 327 control cases were also analyzed. The antepartum cases were of lower median birth weight and gestational age and had a lower frequency of translucent amniotic fluid than the control cases. The antepartum cases also had a higher frequency of abnormalities detected prenatally and FGR than the control cases. Among the 341 stillbirths, there were 37 deaths of one twin and six of both twins. Of 298 singleton stillbirths, 97 (32.6%) had FGR (z-score for birthweight for gestational age, < − 2). Thirty-six stillbirths were autopsied, of which eight had abnormal findings. Eleven stillbirths underwent array chip testing, of which two had abnormal findings (Table 3).
Macroscopic and histological placental observations in stillbirths
The cord abnormalities comprised cord knots, cord hyper helix, cord torsion, cord entanglement, cord rupture, rupture of cord vessels, and others. Chorioamnionitis was histologically confirmed in 26 (40.6%) of 64 placentas tested. Among 24 of those cases (24/26, 92.3%) four were grade I, eight were grade II, and 12 were grade III according to the extent of inflammatory cellular infiltration of the placenta (Table 4).
Risk factors for third-trimester stillbirth
Using the ReCoDe system, in 311 (91.2%) of 341 cases, the third-trimester stillbirth was attributed to a single underlying condition, whereas no cause was evident in 30 (8.8%) cases (Table 5). Overall, third-trimester stillbirths were most commonly attributed to the fetus [117 (34.3%) cases; 51 (15.0%) with FGR and 42 (12.3%) with lethal congenital anomaly], umbilical cord [88 (25.8%) cases; 58 (17.0%) with other conditions (e.g., cord hyper helix/torsion and short cord)], mother [34 (10.0%) cases; 16 (4.7%) with hypertensive diseases in pregnancy and eight (2.3%) with diabetes], placenta [31 (9.1%) cases; 18 (5.3%) with placental abruption and eight (2.3%) with placental insufficiency], and intrapartum [28 (8.2%) cases; 25 (7.3%) with asphyxia and three (0.9%) with birth trauma]. Only eight (2.3%), three (0.9%), and two (0.6%) stillbirths were attributed to amniotic fluid, trauma and uterus, respectively.
The 51 cases of FGR comprised 35 cases of singleton FGR, eight cases of SIUGR (selective intrauterine growth restriction), and eight cases of DCDA (dichorionic diamniotic). Among the B-umbilical cord causes, B4 (umbilical cord-other) were most common [58 (17.0%) cases], comprising 50 cases of cord hyper helix/torsion, three of short umbilical cord, two of single umbilical artery, one of cord entangled by the amniotic band, one of cord atresia, and one case of cord cyst. Of the intrapartum causes, 25 stillbirths were attributed to acute asphyxia because of sudden rupture of cord vessels (four cases), hypertensive diseases in pregnancy (five cases), lethal congenital anomaly (four cases), cord prolapse (three cases), FGR (three cases), placental abruption (two cases), placental insufficiency (two cases), hyper helix of the umbilical cord (one case), and non-immune hydrops (one case).
Distribution of stillbirth causes in different gestational weeks
Most of the third-trimester stillbirths caused by fetal conditions occurred at 28–31 + 6 weeks of gestation, accounting for 43.4% (66/152), which was significant (P = 0.002). Most third-trimester stillbirths caused by umbilical cord occurred at 37–42 weeks of gestation, accounting for 47.4% (27/57), which was also significant (P = 0.000). The lowest frequency of third-trimester stillbirths caused by maternal conditions was at 37–42 weeks of gestation, accounting for 3.5% (2/57), but this was not significant. Similar results were obtained for other factors. The lowest frequency of third-trimester stillbirths caused by placental factors occurred at 32–33 + 6 weeks of gestation, accounting for 3.7% (2/54), and a trend toward a higher incidence of third-trimester stillbirths of intrapartum causes at 37–42 weeks of gestational age was observed, accounting for 12.3% (7/57), but this was not significant (Table 5).
Discussion
The incidence of stillbirth in the Women’s Hospital, Zhejiang University School of Medicine from January 1, 2013, to December 31, 2018, was 3.06/1000 (2.63–3.63/1000), lower than the national rate in previous reports5,6. Stillbirth was considered in relation to maternal age, education level, social status, and antenatal care of pregnant women13,14. We found that 78.8% of mothers were of an appropriate age (20–34 years) and 58.6% had a college or postgraduate degree. Furthermore, 13.0% of the pregnant women did not have regular antenatal care, and 4.1% of the mothers with stillbirth were engaged in physical labor. The mature obstetric techniques and extensive experience of prenatal care in our hospital may explain the low rate of stillbirths.
Collecting high-quality data and applying a reliable classification system constitute the first step in understanding the causes of stillbirth. Our understanding of stillbirth causes in LMICs is based on analysis of registration data, not investigation of the placenta or autopsy of the fetus. A systematic review of stillbirths from 2009 to 2016 highlighted the poor-quality data to determine the cause of stillbirths10. Although placental examination is highly informative, it was not performed in studies from low-income settings, and in only two small-scale studies in middle-income settings. An investigation of 2847 stillbirths in seven low-income countries using a computer-based hierarchal algorithm based on medical records15 and did not include a biological investigation of the placenta or autopsy of the fetus. Notably, the underlying causes of stillbirths were not fully characterized because biological investigations were not conducted. In this retrospective study, we reviewed available maternal and fetal medical records during pregnancy and delivery, and undertook macroscopic and histological examination of the placenta, and autopsy and array chip testing of the fetus. Unfortunately, only 64 of 341 stillbirths were subjected to placental examination. The recommended fetal autopsy rate is > 75%. However, the reported autopsy rate is 5.8–58% for various reasons, including religion, cognition of stillbirths, and the educational level of pregnant women16. In this study, only 36 autopsy cases (10.6%) were reported. In addition, two abnormal results were found among 11 stillbirths subjected to array chip testing, but the abnormality was not directly related to the clinical phenotype. The cause of stillbirth in one case was classified as B2 (constricting loop of umbilical cord), and the other as I1 (no relevant condition identified).
The aforementioned systematic review of stillbirths published in 2018 also highlighted the inconsistent use of classification systems for causes of stillbirths. A variety of classification systems are available17,18. The decline in the stillbirth rate in high-income countries has slowed or stopped during the last few decades after decreasing by two-thirds from 1950 to 197519. Standardization of classification systems is required to improve our understanding of stillbirth. In 2011 the authors of the Lancet Stillbirths Series suggested that classification should be the primary focus of epidemiological measurement research20. For each stillbirth, many possible causative conditions are present, and integrating the information is challenging. The ReCoDe classification organizes clinical information related to stillbirth rather than the cause of death21. The purpose of ReCoDe is to avoid a case-by-case analysis and it enables retrospective classification using databases. Although ReCoDe is less clinically effective than a case-by-case perinatal review22, it is less time-consuming, can be performed retrospectively, and accounts for inconsistencies among researchers, countries, and periods. Another advantage of the ReCoDe system is its ICD-code-based structural hierarchy, resulting in 85% of stillbirth cases meeting relevant conditions. However, it follows a pre-established hierarchy, irrespective of whether another condition made a greater contribution. In 2009, among the six stillbirth classification systems evaluated by the International Stillbirth Alliance23, RECODE ranked third. The optimum classification system should collect as much relevant information as possible, using a hierarchical method as a guide but still rely on expert advice24.
We evaluated the RECODE classification in a retrospective analysis of third-trimester stillbirths. The rate of unexplained cases (30/341, 8.8%) was slightly lower than that in a West Midlands cohort of 2625 stillbirths, an Italian sample of 154 stillbirths, a Dutch sample of 485 antepartum singleton stillbirths, and a French sample of 969 stillbirths (16.0, 14.3, 14.2, and 13.9%, respectively)20,21,25,26. We reported a 12.3% (42/341) rate of lethal congenital anomalies, similar to the finding of Gardosi, but the rate of stillbirths classified as FGR (A7) was significantly lower (15.0% versus 43.0%). In the three other case series, the rate of FGR was 30.3%, 16.9%, and 38.2%20,25,26. The differences may be a result of population enrollment and different definitions of FGR. The rate of FGR stillbirths may have been slightly underestimated in this study.
FGR is a common obstetrics complication. It is typically associated with adverse outcomes such as premature birth, stillbirth, and neonatal death. The incidence in the United States and Europe is 5–15%27, while that in China is similar to that of developed countries. Of the above-mentioned six stillbirth classification systems, only the ReCoDe system classifies FGR separately23. Of the 341 cases of third-trimester stillbirths, there were 97 cases of FGR in single fetuses [32.6% (97/298)], and 27 cases of FGR in twin fetuses [62.3% (27/43)]. Among them, 73 stillbirths had other conditions that were greater contributors than FGR, such as maternal status (including F4-severe pre-eclampsia, F1-gestational diabetes with poor glycemic control), fetal status (including A1-fetal congenital anomaly, A3-fetal non-immune hydrops), placental status (including C4-severe placental insufficiency, C1-placental abruption), umbilical factors (including B1-umbilical cord prolapse, B4-umbilical vascular rupture) and intrapartum (G), while the remaining 51 cases were classified as fetal growth restriction (A7). Termination of pregnancy according to the fetal condition is the mainstay of treatment for FGR. FGR pregnant women with abnormal doppler measurement of blood flow in the ductus venosus (DV) have a significantly increased incidence of stillbirth. The combination of fetal movement and ultrasound monitoring of blood flow parameters can reduce the incidence of FGR28.
A meta-analysis concluded that stillbirths in low-income countries were attributable to infection (15.8%), hypoxic peripartum death (11.6%), antepartum hemorrhage (9.5%), and other unspecified conditions (13.8%); 41–44% were unexplained10. In a study in seven low-income countries15, the main causes of stillbirth were asphyxia (46.6%), infection (20.8%), congenital anomalies (8.4%), prematurity (6.6%), and unidentified (11.8%). Infection was the leading cause of stillbirth in all of the above studies. In this work, the rate of chorioamnionitis (D1) was 2.1% (7/341), significantly lower than reported by others. The differences could be caused by inconsistent use of classification systems. In particular, the overall incidence of stillbirths in China has reached the level of high-income countries, and so the classification of causes of stillbirths has become similar to that in high-income countries. Among the seven cases of chorioamnionitis, two were clinically diagnosed, and the other five had pathological findings upon placental examination. In this study, among 64 cases in which placental pathology was evaluated, 26 cases of chorioamnionitis were histologically confirmed. Excluding the five cases mentioned above (D1), those 21 cases were classified as follows: 10 cases as umbilical cord-other (B4), two as constricting loop of umbilical cord (B2), two as lethal congenital anomaly (A1), two as hypertensive diseases in pregnancy (F4), two as diabetes (F1), one as placental insufficiency (C4), one as infection of fetus (A2) and one as intrapartum asphyxia (G1).
Although this study was conducted in an HBV-endemic area, no stillbirth was attributed to HBV. The incidence of third-trimester stillbirths was similar in HBV-negative (0.317%, 317/99,879) and HBV-positive (0.289%, 21/7263) pregnant women. Furthermore, five women were seropositive for syphilis, and four stillbirths were attributed to syphilis (A2-infection of fetus); the other was attributed to other conditions (A7-fetal growth restriction). The four syphilis-seropositive women classified as A2 (infection of fetus) did not attend routine antenatal care in our hospital. Three of them had stillbirths at the time of diagnosis of syphilis, and one had been treated with benzylpenicillin for 4 weeks in another hospital but had a titer of 1:16. The syphilis-seropositive woman classified as A7 (fetal growth restriction) was treated with two courses of benzylpenicillin in a foreign hospital for 5 weeks, and had a titer of 1:1. Otherwise, the incidence of third-trimester stillbirth in syphilis-seropositive pregnant women (2.793%, 5/179) was significantly higher than that in syphilis-seronegative pregnant women (0.311%, 333/106,963). This emphasizes the importance of syphilis screening and treatment.
The above-mentioned studies reported a 46.6% rate of asphyxia and 11.6% of hypoxic peripartum death10,15, an important cause of stillbirth. Abnormal conditions of the mother, placenta, and umbilical cord (e.g., preeclampsia, placental abruption, and umbilical cord prolapse) may cause fetal hypoxia, asphyxia, and death. In this study, the rate of asphyxia (G1) was 7.3% (25/341), significantly lower than reported previously. In the ReCoDe classification system, asphyxia is in the G1 subcategory of the G category (intrapartum). Among the 28 (8.2%) cases of G category (intrapartum), 25 stillbirths were attributed to acute asphyxia (G1) and the other three to birth trauma (G2), all of which were breech deliveries prior to 34 weeks. In fact, other conditions made greater contributions to stillbirths in these three cases of birth trauma but were classified as G2 because the direct cause was breech delivery. The same is true of 25 cases of acute asphyxia (G1), which were classified as sudden rupture of cord vessels (four cases), hypertensive diseases in pregnancy (five cases), lethal congenital anomaly (four cases), cord prolapse (three cases), FGR (three cases), placenta abruption (two cases), placenta insufficiency (two cases), hyper helix of umbilical cord (one case), and non-immune hydrops (one case). Early detection and treatment of complications during pregnancy (e.g., preeclampsia, FGR), enhanced fetal monitoring during birth (fetal heart rate monitoring, ultrasound monitoring), and rational use of midwifery technology (cesarean section, forceps, head-up attraction, perineal side cut), can reduce the incidence of intrapartum stillbirths by 45%29.
Placental investigation showed that 9.1% (31/341) of stillbirths were attributed to placenta (C), and 2.3% (8/341) to placental insufficiency (C4). The Stillbirth Collaborative Research Network study11 showed that placental examination can diagnose 64.6% of stillbirths. A prospective, observational study in South Africa30 involved macroscopic and histological examination of the placenta and culture of fetal blood. These examinations should be considered for future studies in LMIC settings. Our findings highlight the need for systematic investigation of stillbirth, including investigation of the placenta and medical records.
This study had several limitations. First, we did not use methods of determining the causes of stillbirth, such as antiphospholipid antibody testing (useful in 1.1% of cases), fetal-maternal hemorrhage testing (6.4%), and testing for bacteria (such as group B Streptococcus)31. We tested a small number of women for viruses (such as parvovirus B), which have been implicated as causes of stillbirths32. In addition, a complete autopsy (36/341) and karyotyping (11/341) were performed in a few cases, although those enabled identification of the cause of stillbirth in 42.3% and 11.9% of cases. The limited placental investigation may attribute to limited placental cause. Second, we retrospectively abstracted maternal and fetal clinical information from available medical records. Therefore, incomplete medical records may have contributed to unclassified (I) stillbirths (8.8%). Third, this was a single-center study. Although our research center is the largest in Hangzhou, cooperation with other research centers would make our findings more generalizable. Fourth, a larger control group may have been better.
Targeted investigation can ascertain the causes of most third-trimester stillbirths, reducing the incidence of stillbirths globally. We performed this study to obtain reliable medical evidence that could be used to reduce the rate of preventable stillbirths. Although our findings provide important insight into the causes of third-trimester stillbirth, the results may not be generalizable to other resource-poor areas. For example, in areas where interventions such as caesarean section are difficult to obtain, the rate of intrapartum causes of stillbirth may be higher. Further studies in diverse LMIC settings are needed to improve our understanding of the strategies, interventions, and research priorities necessary for achieving the goals of the ‘Every Newborn Action Plan’ by 2030.
Methods
Definition of stillbirth
The gestational weeks definition of stillbirth varies among countries and is ≥ 20 gestational weeks in high-income countries because of their advanced neonatal care2. The World Health Organization (WHO) defines stillbirth as fetal death at ≥ 28 weeks of gestation, 1000 g birth weight, or 35 cm birth length—the International Classification of Diseases definitions of third-trimester stillbirth33. Several factors affect the incidence of stillbirths, and the risk factors vary according to gestational weeks. In this study, we defined third-trimester stillbirths as fetal death at ≥ 28 gestational weeks.
Procedures
This retrospective study was conducted at the Women’s Hospital, Zhejiang University School of Medicine, where 111,275 perinatal fetuses were delivered from January 1, 2013, to December 31, 2018. We recruited only fetuses with a gestational age of at least 28 weeks. Gestational age staging was based on the last menstrual period date and obstetric ultrasound in the first trimester. Excluding those without complete information, a total of 338 women who had third-trimester stillbirths were enrolled, and 291 women with live births formed the control group, which were randomly selected from within the same period as the stillbirths, matched on date.
The maternal and fetal clinical information of the cases was abstracted from the medical records. The information was collected by a member of the study staff and was reviewed by a physician researcher using a standard data-collection form.
The information collected included: (1) General information: age of delivery, nationality, education level, domicile, stable occupation, weight, height, and body mass index of pregnant women; (2) antenatal care visit, gestational weeks, parity, mode of conception, multiple gestation, chorionic properties of twins, history of adverse contact in early pregnancy, history of preventing miscarriage; (3) history of maternal diseases, history of uterine surgery, complications of previous pregnancy, complications of current pregnancy; (4) previous inevitable abortion, spontaneous abortion, recurrent abortion or stillbirth; (5) genetic or structural abnormality of the fetus, fetal growth restriction (FGR); (6) pathological conditions of the umbilical cord; (7) pathological conditions of the placenta; (8) laboratory indicators: TORCH virus, parvovirus, genital tract pathogens, prenatal screening, ABO blood group, Rh blood group, maternal syphilis, hepatitis B virus (HBV) and human immunodeficiency virus test, alpha-fetoprotein, oral glucose tolerance test, glycated hemoglobin, thyroid function, triglyceride, total cholesterol, glycocholic acid, total bile acids, hemoglobin, coagulation function; (9) clinical manifestations; (10) timing of stillbirth (antepartum/intrapartum); (11) delivery conditions: mode of delivery, neonatal weight, neonatal sex, amniotic fluid, neonatal appearance, macroscopic observation of umbilical cord and placenta; (12) macroscopic observation of umbilical cord and placenta, array test, and autopsy; and (13) maternal adverse outcomes.
The study was approved by the Human Research Ethics Committee of the Women’s Hospital, Zhejiang University School of Medicine. The Human Research Ethics Committee agreed that this study is exempt from informed consent because there will be no additional adverse effects on participants, and the investigator will strictly observe the principle of confidentiality, and the relevant study information will only be accessible to the investigator. The methods were performed in accordance with the relevant guidelines and regulations.
Laboratory procedures
The placenta was retrieved and examined macroscopically after delivery. The placenta, membranes, and umbilical cord were immersed in 10% buffered formalin and transported to the Pathology Department of the Women’s Hospital, Zhejiang University School of Medicine. Portions of placenta selected by the histopathologist were embedded in paraffin and processed for routine hematoxylin and eosin staining, using the standard protocols for placental and umbilical cord assessment.
After delivery, a strip of muscle tissue (1 cm) was resected from the thigh and placed in a sterile container for testing using the CytoScan HD Array Chip (Affymetrix Company) by the Department of Reproductive Genetics of our hospital. The CytoScan HD Array Chip contains 75,000 single nucleotide polymorphism markers and 19,000 copy number variation markers. They focus on chromosomal microdeletions, duplications, and abnormalities, as well as subtendyme deletions, of known clinical significance.
After delivery, the dead fetus was transported to the Pathology Department for autopsy for assessment of general congenital defects, morphological deformities, and subtle abnormalities. Autopsy can also identify infection, anemia, hypoxia, and metabolic abnormalities.
Determination the single cause of stillbirths
Individual cases were reviewed by at least two obstetricians and the causes of third-trimester stillbirths were categorized by the Relevant Condition at Death (ReCoDe) classification system. The ReCoDe classification includes nine categories from A (fetal conditions) to I (unclassified), each of which is divided into several subgroups, for a total of 37 subcategories. Although multiple medical conditions may be associated with third-trimester stillbirth, each third-trimester stillbirth was assigned a single cause.
Each case of third-trimester stillbirths was discussed by the expert group in our hospital based on all available information (including clinical, pathological, genetic, autopsy, etc.), confirmed the single cause and recorded.
Statistical analysis
Categorical variables are presented as frequencies (%). The demographic and clinical features of mothers and fetuses were compared by χ2 test, as were risk factors for stillbirth according to number of gestational weeks. Statistical analysis was performed using SPSS 20.0 software. A value of P < 0.05 was regarded as indicative of statistical significance.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Blencowe, H. et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob. Health. 4, e98–e108 (2016).
Lawn, J. E. et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 387, 587–603 (2016).
Heazell, A. E. et al. Stillbirths: economic and psychosocial consequences. Lancet 387, 604–616 (2016).
WHO & UNICEF. Every newborn: an action plan to end preventable newborn deaths. June 30, 2014. http://www.everynewborn.org/Documents/Every_Newborn_Action_Plan-ENGLISH_updated_July2014.pdf. Accessed 29 March 2018.
Chen, D., Cui, S., Liu, C., Qi, H. & Zhong, N. Stillbirth in China. Lancet 387, 1995–1996 (2016).
Zhu, J. et al. Sociodemographic and obstetric characteristics of stillbirths in China: a census of nearly 4 million health facility births between 2012 and 2014. Lancet Glob. Healt. 4, e109–e118 (2016).
McClure, E. M., Nalubamba-Phiri, M. & Goldenberg, R. L. Stillbirth in developing countries. Int. J. Gynaecol. Obstet. 94, 82–90 (2006).
Stillbirth Collaborative Research Network Writing Group. Causes of death among stillbirths. JAMA. 306, 2459-68 (2011).
Man, J. et al. Stillbirth and intrauterine fetal death: factors affecting determination of cause of death at autopsy. Ultrasound Obstet. Gynecol. 48, 566–573 (2016).
Reinebrant, H. E. Making stillbirths visible: a systematic review of globally reported causes of stillbirth. BJOG 125, 212–224 (2018).
Page, J. M. Diagnostic tests for evaluation of stillbirth: results from the Stillbirth Collaborative Research Network. Obstet. Gynecol. 129, 699–706 (2017).
Aminu, M. et al. Causes of and factors associated with stillbirth in low-and middle-income countries: a systematic literature review. BJOG 121, 141–153 (2014).
GBD 2015 Child Mortality Collaborators. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under 5 mortality, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 388, 1725–1774 (2016).
Lawn, J. E. et al. Stillbirths: Where? When? Why? How to make the data count?. Lancet 377, 1448–1463 (2011).
McClure, E. M. et al. Global Network for Women’s and Children’s Health Research: probable causes of stillbirth in low- and middle-income countries using a prospectively defined classification system. BJOG 125, 131–138 (2018).
Auger, N., Tiandrazana, R. C., Healy-Profitós, J. & Costopoulos, A. Inequality in fetal autopsy in Canada. J. Health Care Poor Underserved. 27, 1384–1396 (2016).
Gordijn, S. J. et al. A multilayered approach for the analysis of perinatal mortality using different classification systems. Eur. J. Obstet. Gynecol. Reprod. Biol. 144, 99–104 (2009).
Reddy, U. M. et al. Stillbirth classification—developing an international consensus for research: executive summary of a National Institute of Child Health and Human Development workshop. Obstet. Gynecol. 114, 901–914 (2009).
Flenady, V. et al. Stillbirths: the way forward in high-income countries. Lancet 377, 1703–1717 (2011).
Ego, A. et al. Stillbirth classification in population-based data and role of fetal growth restriction: the example of RECODE. BMC Pregnancy Childbirth 13, 182 (2013).
Gardosi, J., Kady, S. M., McGeown, P., Francis, A. & Tonks, A. Classification of stillbirth by relevant condition at death (ReCoDe): population based cohort study. BMJ 331, 1113–1117 (2005).
Frøen, J. F. et al. Causes of death and associated conditions (Codac): a utilitarian approach to the classification of perinatal deaths. BMC Pregnancy Childbirth 9, 22 (2009).
Flenady, V. et al. An evaluation of classification systems for stillbirth. BMC Pregnancy Childbirth. 9, 24 (2009).
Dudley, D. J. et al. A new system for determining the causes of stillbirth. Obstet. Gynecol. 116, 254–260 (2010).
Korteweg, F. J. et al. A placental cause of intra-uterine fetal death depends on the perinatal mortality classification system used. Placenta 29, 71–80 (2008).
Vergani, P. et al. Identifying the causes of stillbirth: a comparison of four classification systems. Am. J. Obstet. Gynecol. 199, e311-314 (2008).
Gaccioli, F. & Lager, S. Placental Nutrient transport and intrauterine growth restriction. Front. Physiol. 7, 40 (2016).
Malacova, E. et al. Risk of stillbirth, preterm delivery, and fetal growth restriction following exposure in a previous birth: systematic review and meta-analysis. BJOG 125, 183–192 (2018).
Warland, J., Mitchell, E. A. & O’Brien, L. M. Novel strategies to prevent stillbirth. Semin. Fetal Neonatal. Med. 22, 146–152 (2017).
Madhi, S. A. et al. Causes of stillbirths among women from South Africa: a prospective, observational study. Lancet Glob. Health 7, e503–e512 (2019).
Nan, C. et al. Maternal group B streptococcus-related stillbirth: a systematic review. BJOG 122, 1437–1445 (2015).
Goldenberg, R. L. & Thompson, C. The infectious origins of stillbirth. Am. J. Obstet. Gynecol. 189, 861–873 (2003).
World Health Organization (WHO). International Classifications of Diseases (ICD). Available at: http://www.who.int/classifications/icd/en/. Accessed 7 March 2014.
Author information
Authors and Affiliations
Contributions
Y.H. and Z.L. conceived and designed this project; Y.H. and Q.W. did the analysis and wrote the manuscript; D.C., L.Q. and Z.L. supervised this project; J.L. and D.H. helped analyzing the data; Y.Z., J.L. and Y.W. helped to collect data. All authors have contributed to read and agreed the final content of manuscript for submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, Y., Wu, Q., Liu, J. et al. Risk factors and incidence of third trimester stillbirths in China. Sci Rep 11, 12701 (2021). https://doi.org/10.1038/s41598-021-92106-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-92106-1
This article is cited by
-
Exposure-lag response of fine particulate matter on intrauterine fetal death: an analysis using a distributed lag non-linear model in Linxia Hui Autonomous Prefecture, China
Environmental Science and Pollution Research (2023)
-
Temporal trends and adverse perinatal outcomes of twin pregnancies at differing gestational ages: an observational study from China between 2012–2020
BMC Pregnancy and Childbirth (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.