Abstract
Background
Pregnancies with prenatally diagnosed congenital heart disease (CHD) have increased cesarean delivery (CD) rates, with no outcome improvement.
Objective
We aim to examine indications for delivery, indications for CD and risk factors associated with CD.
Study design
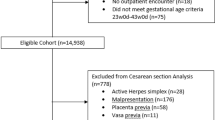
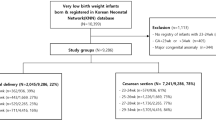
Retrospective cohort of 322 singleton pregnancies prenatally diagnosed with moderate to severe CHD. We compared maternal and fetal factors correlated with delivery route.
Results
CD rate was 46% (95% CI 40, 51%). Of all CD, 31.3% (95% CI 23.8, 38.7) were secondary to urgent fetal indications. However, 79.7% of inductions resulted in vaginal delivery (VD). Factors associated with CD include morbid obesity (RR 3.0, 95% CI 1.5, 6.1), diabetes (RR 3.9, 95% CI 2.0, 7.3) and severe pre-eclampsia (6.0, 95% CI 1.7, 21.4). Of the 10 most frequent CHD diagnoses, only hypoplastic-left-heart was associated with CD (OR 1.9, 95% CI 1.02, 3.4).
Conclusions
Although the CD rate is higher in fetal CHD, most indications for CD are maternal.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Hoffman JL, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–1900.
Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in Atlanta, 1998–2005. J Pediatr. 2008;153:807–13.
Ailes EC, Gilboa SM, Riehle-Colarusso T, Johnson CY, Hobbs CA, Correa A, et al. National birth defects prevention study. Prenatal diagnosis of nonsyndromic congenital heart defects. Prenat Diagn. 2014;34:214–22.
Bakker MK, Bergman JEH, Krikov S, Amar E, Cocchi G, Cragan J, et al. Prenatal diagnosis and prevalence of critical congenital heart defects: an international retrospective cohort study. BMJ Open. 2019;9:e028139.
Chakraborty A, Gorla SR, Swaminathan S. Impact of prenatal diagnosis of complex congenital heart disease on neonatal and infant morbidity and mortality. Prenat Diagn. 2018;38:958–63.
Holland BJ, Myers JA, Woods CR Jr. Prenatal diagnosis of critical congenital heart disease reduces risk of death from cardiovascular compromise prior to planned neonatal cardiac surgery: a meta-analysis. Ultrasound Obstet Gynecol. 2015;45:631–8.
Khoshnood B, Lelong N, Houyel L, Bonnet D, Ballon M, Jouannic JM, et al. EPICARD Study group. Impact of prenatal diagnosis on survival of newborns with four congenital heart defects: a prospective, population-based cohort study in France (the EPICARD Study). BMJ Open. 2017;7:e018285.
Landis BJ, Levey A, Levasseur SM, Glickstein JS, Kleinman CS, Simpson LL, et al. Prenatal diagnosis of congenital heart disease and birth outcomes. Pediatr Cardiol. 2013;34:597–605.
Özer Bekmez B, Alyamaç Dizdar E, Okur N, Büyüktiryaki M, Uraş N, Oğuz SS. Does prenatal diagnosis of critical congenital heart diseases influence the prereferral mortality in a center without surgical intervention? J Matern Fetal Neonatal Med. 2019;32:3431–4.
Li YF, Zhou KY, Fang J, Wang C, Hua YM, Mu DZ. Efficacy of prenatal diagnosis of major congenital heart disease on perinatal management and perioperative mortality: a meta-analysis. World J Pediatr. 2016;12:298–307.
Levey A, Glickstein JS, Kleinman CS. The impact of prenatal diagnosis of complex congenital heart disease on neonatal outcomes. Pediatr Cardiol. 2010;31:587–97.
Peyvandi S, Nguyen TA, Almeida-Jones M, Boe N, Rhee L, Anton T, et al. University of California Fetal Consortium (UCfC). Timing and mode of delivery in prenatally diagnosed congenital heart disease - an analysis of practices within the University of California Fetal Consortium (UCfC). Pediatr Cardiol. 2017;38:588–95.
Tworetzky W, McElhinney DB, Reddy VM. Improved surgical outcome after fetal diagnosis of hypoplastic left heart syndrome. Circulation. 2001;103:1269–73.
Mahle WT, Clancy RR, McGaurn SP. Impact of prenatal diagnosis on survival and early neurologic morbidity in neonates with the hypoplastic left heart syndrome. Pediatrics. 2001;107:1277–82.
Ueda K, Ikeda T, Iwanaga N, Katsuragi S, Yamanaka K, Neki R, et al. Intrapartum fetal heart rate monitoring in cases of congenital heart disease. Am J Obstet Gynecol. 2009;201:64.e1–6.
Morikawa M, Endo D, Yamada T, Cho K, Yamada T, Minakami H. Electronic fetal heart rate monitoring in five fetuses with Ebstein’s anomaly. J Obstet Gynaecol Res. 2014;40:424–8.
Cedergren MI, Källén BA. Obstetric outcome of 6346 pregnancies with infants affected by congenital heart defects. Eur J Obstet Gynecol Reprod Biol. 2006;125:211–6.
Rossi RM, Divanovic A, DeFranco EA. Obstetric outcomes associated with fetal cyanotic congenital heart disease. Am J Perinatol. 2019;36:701–8.
Cnota JF, Gupta R, Michelfelder EC, Ittenbach RF. Congenital heart disease infant death rates decrease as gestational age advances from 34 to 40 weeks. J Pediatr. 2011;159:761–5.
Dadlez NM, Brubaker SG, Simpson LL, Yilmaz B, Williams IA. Impact of change in delivery practice on neonatal and maternal outcomes in cases of significant congenital heart disease. Congenit Heart Dis. 2014;9:368–72.
Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118:29–38.
Boyle A, Reddy UM, Landy HJ, Huang CC, Driggers RW, Laughon SK. Primary cesarean delivery in the United States. Obstet Gynecol. 2013;122:33–40.
Walsh CA, MacTiernan A, Farrell S, Mulcahy C, McMahon CJ, Franklin O, et al. Mode of delivery in pregnancies complicated by major fetal congenital heart disease: a retrospective cohort study. J Perinatol. 2014;34:901–5.
Author information
Authors and Affiliations
Contributions
HM, EM, JC, ST and AD conceived the idea. HM, EM, and AD developed the idea. HM and AJ collected the data and wrote the manuscript. All authors participated in review of results and contributed to discussion. HM, EM, JC, ST, and AD developed additional questions to answer.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki. This study was approved by the institutional review board at Cincinnati Children’s Hospital Medical Center (IRB# 2019-0739) and University of Cincinnati Medical Center (IRB #2020-040).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Masters, H., Marcuccio, E., Jukic, A. et al. Maternal and neonatal factors associated with cesarean delivery in a cohort of pregnancies complicated by prenatally diagnosed congenital heart disease. J Perinatol 44, 360–365 (2024). https://doi.org/10.1038/s41372-023-01747-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01747-9