Abstract
Prognostic implications of therapeutic response of metastatic lymph nodes (LNs) to neoadjuvant chemotherapy (NAC) remain unclear in patients with breast cancer. We aimed to evaluate the prognostic value of axillary LN regression after NAC in locally-advanced breast cancer patients. Therapeutic response of the LNs was evaluated in 563 breast cancer patients and classified into four grades according to the regression pattern. Initial pathologic N stage was estimated from the sum of the metastatic LNs and those with complete regression. In survival analyses, LN regression grade, pathologic N stage after NAC, and presumed initial pathologic N stage stratified clinical outcome of the patients in the whole group, in both ER-positive and ER-negative subgroups, and in those with residual breast disease. On multivariate analysis, LN regression grade and presumed initial pathologic N stage were revealed as independent prognostic factors. The number of completely-responsive LNs and the ratio of non-responsive LNs also revealed a prognostic value. In conclusion, regression grade of axillary LNs and presumed initial pathologic N stage have prognostic values in breast cancer patients who receive NAC. Thus, regression of axillary LNs should be evaluated and included in pathologic reporting of post-NAC resection specimens.
Similar content being viewed by others
Introduction
Neoadjuvant chemotherapy (NAC) is regarded a standard therapy in patients with locally advanced breast cancer. Advantages of NAC include downstaging which allows inoperable tumors surgically-removable, reducing the extent of surgery, preventing systemic metastasis, and obtaining information on chemo-responsiveness1.
Pathologic complete response (pCR), defined as no residual invasive disease in both the breast and axilla after NAC, is a well-established prognostic factor in patients with breast cancer2. However, a significant proportion of patients who receive NAC does not reach pCR, and those who do not reach pCR include a broad range of patients with different responses to NAC. Thus, more detailed indices including Miller-Payne grading system which reflect cellularity difference between pre- and post-treatment tumors and the Residual Cancer Burden (RCB) classification that incorporates both primary and axillary tumor burden have been devised3,4. These systems not only reflect chemo-responsiveness of a tumor but also predict patients’ clinical outcome4,5.
Axillary status after NAC has been consistently reported as a robust prognostic factor for patient survival independent of primary tumor response6,7. In addition to the absolute number of residual metastatic LNs, some have reported the prognostic significance of the LN ratio (number of metastatic LNs divided by number of dissected LNs) in NAC setting8,9,10,11,12. However, the prognostic value of LN regression grade has not been studied widely in breast cancer.
In this study, we evaluated the regression of metastatic LNs, estimated initial pathologic N stage, and finally assessed their prognostic value in predicting survival of the patients with locally advanced breast cancer treated with NAC.
Results
Clinicopathologic characteristics
This study included either clinical stage II (n = 285) or III (n = 278) breast cancer patients treated with NAC. As for estrogen receptor (ER) status, 352 patients (62.5%) were ER-positive while the remaining 211 patients (37.5%) were ER-negative. For progesterone receptor (PR) status, 293 patients (52.0%) were PR-positive, and 270 (48.0%) were PR-negative. As for human epidermal growth receptor 2 (HER 2), 167 patients (29.7%) were HER2-positive while 396 patients (70.3%) were HER2-negative. The AC regimen consisting of doxorubicin and cyclophophamide for 4 to 6 cycles was given to 142 patients (25.2%), sequential AC-T comprising 4 cycles of AC followed by 4 cycles of docetaxel was administered in 271 patients (48.1%), and sequential AC-TH comprising 4 cycles of AC followed by 4 cycles of docetaxel and trastuzumab was given to 54 patients (9.6%). The AD regimen consisting of doxorubicin and docetaxel for 3 to 6 cycles was administered in 70 patients (12.4%), and the remaining 26 patients (4.6%) received various other regimens. The patients received breast surgery 3–4 weeks after the last chemotherapy cycle. Table 1 summarizes the clinicopathological features prior to NAC.
Chemotherapeutic response of LNs after NAC
Prior to NAC, 95 (16.9%) of the 563 patients showed no evidence of nodal metastases (cN0) while 468 (83.1%) patients were suspected of having nodal metastases by imaging studies (cN1–N3). After NAC, axillary LN metastasis was found in 298 patients (52.9%), and the mean number of metastatic LNs was 2.87 (standard deviation, 5.35). The mean ratio of non-responsive lymph nodes to the total number of estimated metastatic LNs was 0.61 (standard deviation, 0.45). As for LN regression grade, 136 (24.2%) patients had no metastatic LNs without regression (grade 0), 129 (22.9%) patients had no metastatic LNs with complete regression (grade 1; Fig. 1), 78 (13.9%) patients had metastatic LNs but complete regression in some LNs (grade 2), and 220 (39.1%) patients had metastatic LNs with no regression (grade 3). Initial pathologic N (ipN) stage was estimated from the sum of the number of metastatic LNs and those with a complete regressive change. There were 136 (24.2%) cases with ipN0, 232 (41.2%) cases with ipN1, 136 (24.2%) cases with ipN2, and 59 (10.5%) cases with ipN3. Table 2 summarizes the clinicopathological characteristics of tumor after NAC including response of LNs.
Representative images of complete tumor regression in axillary lymph nodes. (A) A large area of intranodal fibrosis is noted in the center of lymph node. (B) Magnification of A reveals depletion of lymphocytes and replacement with dense fibrous tissue. (C) Nodal architecture is obliterated with infiltration of foamy histiocytes and intranodal fibrosis. Thickened lymph node capsule is also found. (D) Magnification of (C) shows heavy infiltration of foamy histiocytes.
Clinicopathologic characteristics of tumors in relation to chemo-responsiveness of LNs
The clinicopathologic characteristics of the tumors according to chemo-responsiveness of the LNs are shown in Table 3. Briefly, grade 1 (complete regression) was significantly associated with high histologic grade, negative ER and PR status, and high Ki-67 index prior to NAC compared to grade 2 (partial regression) or grade 3 (no regression) (all P < 0.05). In addition, ypT0-T1, Miller-Payne grades 4–5, RCB classes 0-I, and absence of lymphovascular invasion after NAC were also associated with complete LN response to NAC (all P < 0.05). Conversely, in the LN non-responsive tumors encompassing grades 2 and 3, low to intermediate histologic grade, positive ER and PR status, low Ki-67 index, ypT2-T4, Miller-Payne grades 1–3, RCB classes II-III, and presence of lymphovascular invasion were more common as compared to completely node-responsive tumors (all P < 0.05). Grade 2 and grade 3 also showed difference in clinicopathologic characteristics with negative ER and PR status, positive HER2 status, high Ki-67 index, ypT0-T1, Miller-Payne grades 4–5, and RCB classes 0-I being more frequent in grade 2 than in grade 3 (all P < 0.05). As for breast cancer subtype, luminal A and luminal B subtypes were most prevalent in grade 3, and HER2 + and triple-negative subtypes were most frequent in grade 1.
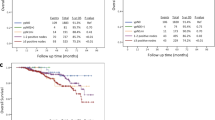
Prognostic significance of chemo-responsiveness of LNs
Survival analysis of the 563 patients revealed an association between four LN regression grades and disease-free survival of the patients, with grade 0 having the most favorable survival and grade 3 displaying the worst survival (p < 0.001, as a whole; p = 0.049, grade 0 vs. grade 1; p = 0.061, grade 1 vs. grade 2; p = 0.377, grade 2 vs. grade 3; Fig. 2). Pathologic N stage after NAC (ypN) also showed an association with disease-free survival (p < 0.001, as a whole; p = 0.003, ypN0 vs. ypN1; p = 0.157, ypN1 vs. ypN2; p = 0.146, ypN2 vs. ypN3; Fig. 2). As for ipN stage before NAC, we observed that ipN0 had the longest survival, and there was an almost stepwise decline in survival with each increase in ipN stage (p < 0.001, as a whole; p = 0.013, ipN0 vs. ipN1; p = 0.012, ypN1 vs. ypN2; p = 0.096, ypN2 vs. ypN3; Fig. 2).
Next, we performed the same set of analyses according to ER status. In ER-negative group (n = 211), there was a significant difference in disease-free survival among the four regression grades as a whole (p < 0.001; Fig. 3). However, grades 0 and 1 showed similar favorable survival while grades 2 and 3 revealed poor survival alike (p = 0.524, grade 0 vs. grade 1; p = 0.001, grade 1 vs. grade 2; p = 0.604, grade 2 vs. grade 3). As for pathologic N stage after NAC, there was a stepwise decrease in survival with increased ypN stage (p < 0.001, as a whole; p = 0.043, ypN0 vs. ypN1; p = 0.001, ypN1 vs. ypN2; p = 0.006, ypN2 vs. ypN3; Fig. 3). Presumed initial pathologic pN stage also showed an association with disease-free survival as a whole (p < 0.001; Fig. 3), but there was no survival difference between ipN0 and ipN1 (p = 0.361, ipN0 vs. ipN1; p = 0.001, ypN1 vs. ypN2; p = 0.003, ypN2 vs. ypN3).
Disease-free survival based on lymph node (LN) status after neoadjuvant chemotherapy by estrogen receptor (ER) status. In ER-negative subgroup, significant survival difference is observed based on LN regression grade (A), ypN stage (B), and initial pathologic N (ipN) stage (C), while in ER-positive subgroup, LN regression grade (D), ypN stage (E), and ipN stage (F) show less significant associations with patients’ survival.
In ER-positive group (n = 352), LN regression grade, ypN stage, and ipN stage were associated with disease-free survival of the patients as a whole (p = 0.002, p = 0.029, p = 0.023; Fig. 3), but there was no survival difference between LN regression grades 1 and 2, between ypN1, ypN2, and ypN3 or between ipN1, ipN2, and ipN3.
When we analyzed the association between LN status and survival in the patient group with residual breast disease, we also observed a difference in survival with respect to LN regression grade, ypN stage, and ipN stage (p = 0.005, p = 0.001, p < 0.001, respectively).
Multivariate analyses including chemo-responsiveness of LNs
We performed multivariate analyses to evaluate whether nodal response to NAC had an independent prognostic value. In the whole group, ypT stage (p < 0.001), Miller-Payne regression grade (p < 0.001), and RCB class (p < 0.001) were associated with disease-free survival as well as LN regression grades, ypN stage, and ipN stage. As LN regression grades, ypN stage, and ipN stage were highly correlated with each other (LN regression grades and ypN stage, r = 0.775; LN regression grades and ipN stage, r = 0.663; ypN stage and ipN stage, r = 0.801), multivariate analyses were conducted in different modes. In multivariate analysis, LN regression grade and ipN stage, but not ypN stage were revealed as independent prognostic factors (p = 0.016, p = 0.006, p = 0.097, respectively; Table 4).
In the patient group with residual breast cancer, ypT stage, post-NAC ER status, post-NAC Ki-67 index, LN regression grade, ypN stage, and ipN stage were found to be independent prognostic factors for disease-free survival (all p < 0.05; Table 5).
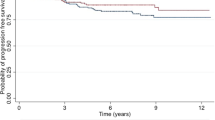
Prognostic value of number of LNs with complete regression
In patients with no metastatic LNs after NAC (ypN0), those belonging to LN regression grade 0 had a longer disease-free survival compared to those in LN regression grade 1 (p = 0.049). We performed a receiver operating characteristic (ROC) curve analysis to find the cutoff value for the number of LNs with complete response that maximized the sum of sensitivity and specificity in predicting tumor recurrence (AUC = 0.736; Fig. 4). Using a cutoff value of 2.5, comparison of patients with a number of completely-responsive LNs less than 3 with those having a completely-responsive LN number greater than or equal to 3 revealed a more favorable clinical outcome of the former compared to the latter (p < 0.001; Fig. 4).
Disease-free survival based on the number of completely-responsive lymph nodes (LNs). (A) A receiver operating characteristic curve analysis yields the highest area under curve (AUC) at a value of 2.5 as the cutoff for the number of completely-responsive LNs. (B) In ypN0 subgroup, patients with a number of completely-responsive LNs less than 3 show longer disease-free survival compared to those having a completely-responsive LN number greater than or equal to 3.
Prognostic value of ratio of non-responsive LNs
We also performed a ROC curve analysis to find the cutoff value of the ratio of non-responsive LNs to the total number of estimated metastatic LNs before treatment that maximized the sum of sensitivity and specificity in predicting tumor recurrence in patients with presumed metastatic LNs prior to NAC (AUC = 0.608; Fig. 5). As a result, 0.348 was identified as the cutoff value. Survival analysis revealed that patients with a ratio of non-responsive LNs to the total number of metastatic nodes less than 0.348 had a significantly longer disease-free survival compared to those with a ratio over 0.348 (p < 0.001; Fig. 5).
Disease-free survival based on the ratio of non-responsive lymph nodes (LNs) to the estimated total metastatic LNs. (A) A receiver operating characteristic curve analysis yields the highest area under curve (AUC) at a value of 0.348 as the cutoff for the ratio of non-responsive LNs to the estimated total initial metastatic LNs. (B) Patients with a ratio of non-responsive LNs to the total initial metastatic LNs less than 0.348 show a significantly longer disease-free survival compared to those with a ratio over 0.348.
Discussion
Prognosis of breast cancer patients receiving NAC is associated with two factors at large: tumor biology and tumor response to chemotherapy in the breast and/or axilla. In this study, we focused on the second factor, that is, nodal response to NAC as a potential prognostic factor. Researchers have evaluated the axillary status using several different parameters: absolute number of metastatic LNs after NAC (reflected in pathologic N stage, ypN), size of metastasis, LN ratio (ratio of metastatic LNs among total number of excised LNs), clinical N stage, and extracapsular extension9,12,13,14,15. However, among the factors related to LN status post-NAC, the prognostic value of LN regression pattern has not been studied widely in breast cancer. In as early as 2003, Newman et al.16 reported that detection of treatment effect in axillary LNs could identify patients with an outcome intermediate between node-positive and node-negative patients. However, this study had included only 71 cases to deduce statistically-significant conclusions. Also, in their survival analysis, all patients who showed nodal regression were grouped into the same group regardless of presence or absence of metastasis. In this study, we observed that patient survival was associated with LN regression grade with the best outcome belonging to grade 0 and the worst outcome belonging to grade 3.
It has been reported that NAC downstages the axillary nodal status, and the rate of negative conversion ranges as widely as 20 to 60%17,18,19. Studies have shown that patients who undergo a negative conversion of the axillary nodes have excellent survival regardless of residual breast disease7,18,20,21,22. On a similar note, Newman et al. reported that patient survival was dependent on not only node positivity vs. negativity but also on whether the nodes were downstaged16. In the present study, 129 (22.9%) patients underwent a negative nodal conversion (ypN0 with regression, LN regression grade 1). Fayanju et al. reported that patients with a node-positive disease at presentation who achieve a pCR have a prognosis comparable to those who are clinically node-negative at presentation23. However, we observed a significant difference in survival between LN regression grade 0 (node-negative at presentation) and LN regression grade 1 (negative nodal conversion) with grade 0 having a longer disease-free survival as a whole. Such discrepancy in results might be due to the difference in study population since Fayanju’s study included only those with clinical N0 and N1 patients and excluded those who showed a discordant or partial response in the breast and axilla. Furthermore, in further analyses, we found that prognostic significance of negative nodal conversion differed according to ER status. While LN regression grade 1 revealed poorer disease-free survival compared to LN regression grade 0 in ER-positive subset, LN regression grades 0 and 1 showed similar favorable prognosis in ER-negative subset. Furthermore, ER-negative breast cancer showed significant difference in survival between regression grade 1 and 2, whereas ER-positive tumors revealed no survival difference between them. Although the reason for this discrepant result by ER status remains unclear, it may be partly explained by the fact that in previous studies, pCR has been consistently reported to be associated with improved survival in ER-negative breast cancers including HER2-positive and triple-negative subtypes, but not in luminal A subtype24,25. Further studies are warranted to see if the prognostic significance of LN regression pattern does depend on ER status or breast cancer subtype.
In the ypN0 group, we compared patient survival according to the number of completely-responsive LNs and observed that patients with a completely-responsive LN number less than 3 had a more favorable outcome than those with a completely-responsive LN number greater than or equal to 3. It would be reasonable to infer that those with a smaller number of completely-responsive LNs had a smaller number of LN metastasis before NAC, which in turn, would mean less systemic tumor burden that led to improved survival.
In those patients with initial nodal involvement assessed by chemotherapeutic effect in the LNs, we investigated whether the ratio of non-responsive LNs to the total number of estimated metastatic LNs would have a prognostic value. After obtaining the cutoff ratio of 0.348 from ROC curve analysis, we observed that those patients with a non-responsive nodal ratio over 0.348 had poorer outcome compared to those less than 0.348. Such result suggests that in addition to evaluating LN regression pattern after NAC, evaluating the non-responsive LN ratio may provide additional prognostic information in patients who receive NAC.
Our multivariate analysis revealed the following post-NAC factors to be independently prognostic in the NAC setting: ypT stage, RCB class, LN regression grade, and ipN stage. In those with residual cancer in the breast, ypT stage, post-NAC ER status, post-NAC Ki-67 index, LN regression grade, ypN stage, and ipN stage were independent prognostic factors. From the above factors, ypT stage, pN stage, RCB class, Ki-67 index, and ER status have already been reported to be prognostic of patient outcome in breast cancer after NAC12,15,26,27. A novel finding worth noting is the prognostic significance of LN regression grade determined by presence or absence of complete LN regression and residual nodal metastasis, and ipN stage determined by adding the number of metastatic LNs and those with a complete regressive change; we believe this study to be the first one to have evaluated such parameters. Our results may support the idea that axillary status represents systemic micrometastatic burden. Initial pathologic N stage may be a more accurate assessment of a person’s systemic micrometastatic burden rather than ypN stage. Noting chemotherapeutic effects in the post-operative LNs and assessing ipN stage may help stratify patient outcome more accurately. Currently, RCB is the most widely-used index that takes into account both the primary tumor bed response and lymph node status. While it may not be feasible to incorporate the categorical lymph node regression grade into the RCB index, adding numerical parameters such as the number of completely-responsive lymph nodes or the ratio of non-responsive lymph node over total initial metastatic lymph nodes to the RCB index may be useful in making a new prognostic index after further investigations.
On a final note, while axillary nodal dissection has the advantage of accurate assessment of lymph node status in breast cancer patients, it can result in unwanted morbidities such as numbness and debilitating lymphedema; this is the rationale for sentinel node biopsy and the more recent targeted axillary dissection where only the pre-marked lymph nodes suspected of having metastasis are excised in addition to the sentinel nodes. It would be interesting to evaluate the prognostic value of the lymph node regression grade in such less extensive lymph node surgery in further studies.
This study has some limitations. First, we evaluated nodal treatment response using a representative hematoxylin & eosin-stained section rather than serial sections in non-sentinel lymph nodes; thus, we may have missed hidden metastatic foci which could have been present in deeper sections. Therefore, ipN stage estimated by adding the number of LNs with complete chemotherapeutic effect and metastatic nodes may not be exactly the same as the true ipN stage. Secondly, while we included only intranodal fibrosis and foamy histiocyte infiltration as representative of treatment effect, other subtle changes such as a thickened LN capsule can also be a treatment response28. Third, the follow-up period was relatively short with a median of 40 months to assess overall survival. Lastly, NAC regimen was not homogeneous, and trastuzumab treatment was given as part of NAC regimen in only some HER2-positive breast cancer patients due to reimbursement issues in Korea in the past.
In summary, we investigated the prognostic significance of axillary LN response in breast cancer patients who received NAC. LN regression grade, presumed ipN stage, number of completely-responsive LNs, and ratio of non-responsive LNs stratified clinical outcome of the patients. In multivariate analysis, LN regression grade and presumed ipN stage were revealed as independent prognostic factors. Further large, prospective studies are warranted to confirm whether LN regression and presumed ipN stage should be routinely evaluated and reported in breast cancer patients who receive NAC.
Methods
Patients and samples
We used clinicopathological data of 571 consecutive patients with primary breast cancer who underwent breast-conserving surgery or mastectomy after NAC at Seoul National University Bundang Hospital from October 2004 to December 2015, that had been collected in our previous study29. After excluding 8 patients who received sentinel node biopsy prior to NAC, 563 patients were finally included in this study. All patients were diagnosed with invasive carcinoma of the breast via core needle biopsy.
Medical records were reviewed to acquire clinical information of the patients including age, sex, initial clinical T and N stage, chemotherapeutic regimen, cycle of NAC, tumor recurrence, and patient survival. Pathologic information was collected from the pathology reports and the following information was recorded: histologic subtype, histologic grade, pathologic T and N stage after NAC, lymphovascular invasion, and pre- and post-NAC biomarker status.
Pathologic response to NAC was evaluated with the Miller-Payne regression grading4 and Residual Cancer Burden class3. Pathologic complete response (pCR) was defined as the complete disappearance of all invasive tumor cells from the breast and regional LNs regardless of the presence of residual ductal carcinoma in situ in the breast30.
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (Protocol # B-1601/332-304), and it was conducted in accordance with the Declaration of Helsinki. Informed consent was waived by the same IRB who approved this study.
Pathologic evaluation of LNs and definition of response
Of the 563 patients, 488 patients (86.7%) received axillary LN dissection with or without sentinel node biopsy, and the remaining 75 patients (13.3%) received sentinel node biopsy only after NAC. The median number of harvested LNs was 20 (range, 1–65). The sentinel nodes were cut in 2 mm intervals and examined in serial sections. LNs other than sentinel nodes were examined in a single representative section.
For this study, LN status after NAC was carefully evaluated. Histologic signs of tumor regression in LNs were defined as intranodal fibrosis and/or foamy histiocyte infiltration obliterating the nodal architecture, similar to previous studies16,28,31. On the other hand, the presence of hemosiderin-laden macrophages only was not regarded as a therapeutic effect since a prior procedure such as large core biopsy of breast or fine needle aspiration of LNs can result in similar histology. We counted the number of LNs with complete tumor regression, and using this data, we estimated the initial number of metastatic LNs before NAC. In addition, the ratio of LNs with residual disease to the total number of estimated metastatic LNs before NAC was calculated.
Regression of LNs was graded as follows: grade 0, no metastasis without regression; grade 1, no metastasis with complete regression (complete response); grade 2, metastasis, but complete regression in some LNs (partial response); grade 3, metastasis and no complete regression in LNs (no response). Initial pathologic N stage was estimated by the sum of the number of metastatic LNs and LNs with a complete regressive change.
Biomarker status and determination of breast cancer subtype
Immunohistochemical results for standard biomarkers including ER, PR, HER2, p53, and Ki-67 had been collected during the previous study29. ER and PR were regarded as positive if there were at least 1% positive tumor nuclei32. HER2 expression was scored according to 2013 ASCO/CAP guidelines33. HER2 status was determined by HER2 in situ hybridization (ISH) for cases that were equivocal on HER2 immunohistochemistry, and HER2 equivocal cases in ISH were regarded as HER2-non-amplified for statistical analysis. For Ki-67 proliferation index, tumors with 20% or more positive cells were regarded as having high indices34.
Standard biomarker status was used to determine the breast cancer subtype of the tumors according to the 2011 St. Gallen Expert Consensus as follows: luminal A (ER + and/or PR + , HER2-, Ki-67 < 14%), luminal B (ER + and/or PR + , HER2-, Ki-67 ≥ 14%; ER + and/or PR + , HER2 +), HER2 + (ER-, PR-, HER2 +), and triple-negative subtype (ER-, PR-, HER2-)35.
Statistical analysis
Pearson’s chi-square test or Fisher’s exact test was used to compare clinicopathological features of tumors according to chemo-responsiveness of LNs and corrections for multiple testing were made by Bonferroni method. A receiver operating characteristic (ROC) curve analysis was performed to identify cutoff values for the number of LNs with a complete pathologic response and ratio of LNs with residual disease to estimated total metastatic LNs before treatment that maximized the sum of sensitivity and specificity in predicting tumor recurrence. Disease-free survivals were estimated by Kaplan–Meier survival curves and statistical significances were determined with the log-rank test. Pearson correlation tests were used to assess the associations between LN regression grade, pathologic N stage after NAC, and estimated initial pathologic N stage. Multivariate analysis was performed by Cox proportional hazards regression model with backward stepwise selection method, using covariates that were associated with survival of the patient in the univariate analyses. Hazard ratios (HR) and their 95% confidence intervals (CI) were calculated for each variable. P values less than 0.05 were considered statistically significant, and all reported p values were two-sided. All statistical analyses were performed using Statistical Package, SPSS version 25.0 for Windows (IBM Corp., ARMONK, NY).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Thompson, A. M. & Moulder-Thompson, S. L. Neoadjuvant treatment of breast cancer. Ann. Oncol. 23(Suppl 10), x231-236 (2012).
Cortazar, P. et al. Pathological complete response and long-term clinical benefit in breast cancer: The CTNeoBC pooled analysis. Lancet 384, 164–172 (2014).
Symmans, W. F. et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J. Clin. Oncol. 25, 4414–4422 (2007).
Ogston, K. N. et al. A new histological grading system to assess response of breast cancers to primary chemotherapy: Prognostic significance and survival. Breast 12, 320–327 (2003).
Symmans, W. F. et al. Long-term prognostic risk after neoadjuvant chemotherapy associated with residual cancer burden and breast cancer subtype. J. Clin. Oncol. 35, 1049–1060 (2017).
Mamounas, E. P. et al. Predictors of locoregional recurrence after neoadjuvant chemotherapy: Results from combined analysis of National Surgical Adjuvant Breast and Bowel Project B-18 and B-27. J. Clin. Oncol. 30, 3960–3966 (2012).
Hennessy, B. T. et al. Outcome after pathologic complete eradication of cytologically proven breast cancer axillary node metastases following primary chemotherapy. J. Clin. Oncol. 23, 9304–9311 (2005).
Kim, J. Y. et al. The prognostic significance of the lymph node ratio in axillary lymph node positive breast cancer. J. Breast Cancer 14, 204–212 (2011).
Tsai, J., Bertoni, D., Hernandez-Boussard, T., Telli, M. L. & Wapnir, I. L. Lymph node ratio analysis after neoadjuvant chemotherapy is prognostic in hormone receptor-positive and triple-negative breast cancer. Ann. Surg. Oncol. 23, 3310–3316 (2016).
Kim, S. H. et al. Prognostic value of axillary nodal ratio after neoadjuvant chemotherapy of doxorubicin/cyclophosphamide followed by docetaxel in breast cancer: A multicenter retrospective cohort study. Cancer Res. Treat. 48, 1373–1381 (2016).
Cho, D. H. et al. Lymph node ratio as an alternative to pN staging for predicting prognosis after neoadjuvant chemotherapy in breast cancer. Kaohsiung J. Med. Sci. 34, 341–347 (2018).
Yang, S.-J. et al. Prognostic factors of axillary lymph node-positive patients in clinical stage II and III breast cancer after neoadjuvant chemotherapy. Ther. Radiol. Oncol. 2, 37–37 (2018).
Klauber-DeMore, N. et al. Size of residual lymph node metastasis after neoadjuvant chemotherapy in locally advanced breast cancer patients is prognostic. Ann. Surg. Oncol. 13, 685–691 (2006).
Huang, E. H. et al. Predictors of locoregional recurrence in patients with locally advanced breast cancer treated with neoadjuvant chemotherapy, mastectomy, and radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 62, 351–357 (2005).
Pierga, J. Y. et al. Prognostic value of persistent node involvement after neoadjuvant chemotherapy in patients with operable breast cancer. Br. J. Cancer 83, 1480–1487 (2000).
Newman, L. A. et al. Histopathologic evidence of tumor regression in the axillary lymph nodes of patients treated with preoperative chemotherapy correlates with breast cancer outcome. Ann. Surg. Oncol. 10, 734–739 (2003).
Kilbride, K. E. et al. Axillary staging prior to neoadjuvant chemotherapy for breast cancer: Predictors of recurrence. Ann. Surg. Oncol. 15, 3252–3258 (2008).
Kuerer, H. M. et al. Incidence and impact of documented eradication of breast cancer axillary lymph node metastases before surgery in patients treated with neoadjuvant chemotherapy. Ann. Surg. 230, 72–78 (1999).
McCready, D. R. et al. The prognostic significance of lymph node metastases after preoperative chemotherapy for locally advanced breast cancer. Arch. Surg. 124, 21–25 (1989).
Al-Hilli, Z., Hoskin, T. L., Day, C. N., Habermann, E. B. & Boughey, J. C. Impact of neoadjuvant chemotherapy on nodal disease and nodal surgery by tumor subtype. Ann. Surg. Oncol. 25, 482–493 (2018).
Rouzier, R. et al. Incidence and prognostic significance of complete axillary downstaging after primary chemotherapy in breast cancer patients with T1 to T3 tumors and cytologically proven axillary metastatic lymph nodes. J. Clin. Oncol. 20, 1304–1310 (2002).
Hayashi, N. et al. The prognostic effect of changes in tumor stage and nodal status after neoadjuvant chemotherapy in each primary breast cancer subtype. Clin. Breast Cancer 18, e219–e229 (2018).
Fayanju, O. M. et al. The clinical significance of breast-only and node-only pathologic complete response (pCR) after neoadjuvant chemotherapy (NACT): A review of 20,000 breast cancer patients in the national cancer data base (NCDB). Ann. Surg. 268, 591–601 (2018).
von Minckwitz, G. et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J. Clin. Oncol. 30, 1796–1804 (2012).
Haque, W. et al. Response rates and pathologic complete response by breast cancer molecular subtype following neoadjuvant chemotherapy. Breast Cancer Res. Treat. 170, 559–567 (2018).
Sheri, A. et al. Residual proliferative cancer burden to predict long-term outcome following neoadjuvant chemotherapy. Ann. Oncol. 26, 75–80 (2015).
Resende, U., Cabello, C., Ramalho, S. O. B. & Zeferino, L. C. Prognostic assessment of breast carcinoma submitted to neoadjuvant chemotherapy with pathological non-complete response. BMC Cancer 19, 601 (2019).
Barrio, A. V. et al. How often is treatment effect identified in axillary nodes with a pathologic complete response after neoadjuvant chemotherapy?. Ann. Surg. Oncol. 23, 3475–3480 (2016).
Ahn, S. et al. Negative conversion of progesterone receptor status after primary systemic therapy is associated with poor clinical outcome in patients with breast cancer. Cancer Res. Treat. 50, 1418–1432 (2018).
Kuerer, H. M. et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J. Clin. Oncol. 17, 460–469 (1999).
Glaeser, A. et al. Heterogeneous responses of axillary lymph node metastases to neoadjuvant chemotherapy are common and depend on breast cancer subtype. Ann. Surg. Oncol. 26, 4381–4389 (2019).
Hammond, M. E. et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J. Clin. Oncol. 28, 2784–2795 (2010).
Wolff, A. C. et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J. Clin. Oncol. 31, 3997–4013 (2013).
Denkert, C. & von Minckwitz, G. Reply to Ki67 in breast cancer: A useful prognostic marker!. Ann. Oncol. 25, 542–543 (2014).
Goldhirsch, A. et al. Strategies for subtypes-dealing with the diversity of breast cancer: Highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann. Oncol. 22, 1736–1747 (2011).
Acknowledgements
This study was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (Grant No. NRF-2015R1A2A2A01007907) to Park SY.
Author information
Authors and Affiliations
Contributions
Y.R.C. participated in the interpretation and analysis of data and drafted the manuscript. J.W.W. participated in the analysis of the data. S.A. participated in the acquisition and interpretation of pathologic data. E.K., E.K.K., M.J., S.M.K., S.H.K. and J.H.K. participated in the acquisition of clinical data. S.Y.P. conceived of the study, participated in its design, and was responsible for preparation of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, Y.R., Woo, J.W., Ahn, S. et al. Prognostic implications of regression of metastatic axillary lymph nodes after neoadjuvant chemotherapy in patients with breast cancer. Sci Rep 11, 12128 (2021). https://doi.org/10.1038/s41598-021-91643-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91643-z
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.