Abstract
Erectile dysfunction (ED) is mostly due to the lack of blood flow into the penis. In the past 20 years, near-infrared spectroscopy (NIRS) was used in measuring the concentrations and temporal dynamics of different hemoglobin types. However, the dynamics of the light absorption (photoplethysmography; PPG) have not been applied to survey penile hemodynamics and erection quality. This paper compared the use of photoplethysmography (PPG) to study vascular ED with standard penile Doppler ultrasonography. Men diagnosed with vascular ED for at least 6 months and nominated for penile ultrasonography were included. PPG signals were collected during the ultrasound examination. All beat-to-beat PPG waveforms were aligned with the peak and averaged to one representative template waveform for feature analysis, including amplitude differences (APD) index, reflection time index (RTI), augmentation index (AI), and perfusion index (PI). An inverse correlation was found between end-erection amplitude and both erection hardness score (EHS) and resistive index (RI). APD index and EHS as well as the international index of erectile function-5 (IIEF) and RI were positively correlated. RTI and AI were inversely correlated to IIEF and RI. PI was positively correlated to RI. PPG may therefore be useful as a noninvasive, convenient, technique for sexual function evaluation.
Similar content being viewed by others
Introduction
Erectile dysfunction (ED) is a condition that causes a negative impact on the quality of life, self-esteem, and partner relationship. It is defined as the inability to achieve and maintain an erection hard enough for intercourse to the mutual satisfaction of the man and his partner1. It influences a large population worldwide, with an estimated 320 million men affected with ED by 20252. The failure of sustaining penile rigidity is mostly due to the lack of blood flow into the penis. Thus, penile hemodynamic measurements are fundamental to erectile function evaluation. Doppler ultrasonography and the pudendal vessel angiography are currently used to evaluate penile hemodynamics3,4. Most examination methods are invasive and inconvenient, making patients uncomfortable.
Near-infrared spectroscopy (NIRS), which uses light in the 700- to 1,000-nm wavelength, has been used to continuously assess changes in hemoglobin concentrations in the blood with very low energy5. In the last 20 years, NIRS has been used in urological examinations, including the measurement of testicular and renal cortex oxygenation, bladder functional studies, and penile hemodynamics6,7,8,9,10. In addition to measuring the concentrations of oxy- and deoxy-hemoglobin, the temporal dynamics of light absorption (photoplethysmography; PPG) is proportional to the volume changes in the arterial blood after removing the constant term due to the light absorption of tissue and the venous hemoglobin11. The dynamics of arterial light absorption measured in a finger were used as an alternative to noninvasive hemodynamic parameters in assessing vascular stiffness and continuous blood pressure in many studies12,13. PPG is ideal for in-hospital or home monitoring because most modern portable pulse oximetry equipment can export PPG signals. However, potential PPG applications in penile hemodynamics had not been studied. This study hypothesized that the reduction in the blood flow of cavernous arteries due to high pressure inside the penis during erection causes a relatively lesser blood volume pumped into the penis and induces a decrease in PPG amplitude, representing the degree of hardness of penile erection. Furthermore, the penile PPG waveform, an alternative to the pressure waveform of cavernous arteries, may also advance the current understanding of penile hardness, penile Doppler parameters, and sexual ability. This study was undertaken to investigate penile hemodynamics and penile erection quality using PPG.
Results
Patient demographics
Table 1 shows the demographics of the current study cohort. The mean age was 57.14 ± 13.05 years, and the mean international index of erectile function-5 (IIEF-5) score was 11.89 ± 4.52. Most subjects in this study presented an erection hardness score (EHS) score 2 and inability to complete intercourse in the past 6 months. Most of the ED cases were observed in the mild to moderate groups. Significant differences exist in the amplitude differences (APD) index, reflection time index (RTI), augmentation index (AI), and resistive index (RI) when patients were grouped by ED severity (Table 2). The moderate and severe ED groups had smaller perfusion index (PI) values and lower peak systolic velocities, although the latter was not statistically significant.
Amplitude correlative series and sexual function
Penile erection was verified to correspond to decreased PPG signals. The amplitude in the end-erection period, as well as EHS and RI, had a significant inverse relationship (Table 3, Fig. 1). The relationship between RI and EHS in this study was also statistically significant (R = 0.670, P < 0.001). Conversely, the APD index is positively correlated with IIEF, EHS, and RI (Fig. 1, Table 3). A higher intracavernosal pressure (ICP) at the end of the erection, which represents the harder penis, causes less blood volume into the penis resulting in lower end-erection PPG amplitude and higher APD index (the difference between mid- and end-erection amplitudes). Nevertheless, the correlation between the PPG amplitude and peak systolic velocity of the cavernous artery was not statistically significant (p = 0.921).
The amplitude correlative series and sexual function. A: Amplitude in the end-erection period is negatively correlated with EHS (R = − 0.405, p < 0.05); B: APD index is positively correlated with EHS (R = 0.522, p < 0.05); C: RI is positively correlated with EHS (R = 0.670, P < 0.001); D: APD index is positively correlated with RI (R = 0.417, p < 0.05).
The waveform characteristics and sexual function
The cavernous arterial RTI and AI were negatively correlated with IIEF and RI (Table 3, Fig. 2). The PI was positively correlated with RI and inversely correlated with end-diastolic velocity. These findings support that the harder cavernous tissue (higher EHS or penile hardness) can stiffen the local cavernous artery and cause the PPG waveform changes. The main and the reflected wave are superimposed earlier, leading to a higher second peak and shorter reflection time resulting in lower AI and RTI, because the pulse wave travels faster in the stiffened artery. The perfusion index, considered as the dynamic acceleration of arterial vessel wall, was also observed to may be an indicator of RI and end-diastolic velocity.
Discussion
This study analyzed the dynamics of arterial PPG monitored via NIRS and derived several waveform characteristics. First, the PPG amplitude in the end-erection period can be an indicator for EHS, and the APD index of the cavernous artery is positively correlated with IIEF, EHS, and RI. The APD index was significantly lower in the severe ED group compared with the other groups. Second, during the mid-erection period, the RTI and AI derived from the systolic and diastolic peaks of the waveform and the stiffness indexes for the vascular system were negatively correlated with IIEF and EHS. Third, the PI value, a measurement of the dynamics of vessel wall changes, is positively correlated with RI and inversely correlated to end-diastolic velocity. All these findings can be translated to a higher ICP built at the end of the erection leading to lesser blood volume into the penis and hardens it. These physiological changes during erection can be assessed by the amplitude parameters (low amplitude at the end-erection period and high APD index) and waveform parameters (lower AI and lower RTI) derived from PPG.
ED is a problem in obtaining or maintaining an erection for sexual intercourse. The prevalence of ED increases with age and is becoming continuously frequent in young males in recent years14. Aside from PPG, clinicians use several noninvasive devices to gather erectile information, including strain gage (e.g., Erektor), pulse–volume–plethysmography, and laser Doppler imaging15,16,17,18. PPG use for penile hemodynamics has several distinct advantages over the other aforementioned devices. First, PPG can potentially measure not only changes in hemoglobin in oxygenated blood19 but also arterial volume changes (proportional to light absorption dynamics). Second, it is low cost, portable for natural settings (e.g., in actual human intercourse context instead of video stimulations), which makes long-term recording possible in a clinical friendly environment, and is more comfortable for patients. Recent urological studies using NIRS have included testicular ischemia, voiding dysfunction, and ED6,9,20,21,22,23,24,25,26,27,28. Kim et al. performed a NIRS experiment with six healthy men shown an adult video for 4 min28. The NIRS sensors for collecting signals were placed on the side and top of the penis. A significant increase of oxygenated hemoglobin (HbO) when the adult video started indicated the dilation of the cavernous arteries and the compression of the penile venous complex. A similar NIRS study was undertaken by Kudlow et al. to compare hemoglobin concentrations in healthy young men and prostate cancer patients after bilateral nerve-sparing radical prostatectomy27. They found that HbO increased up to 70% and 58.3% in the young, healthy group and in the prostate cancer groups, respectively. These studies suggest that NIRS can be a convenient method that is sensitive enough for detecting real-time hemoglobin concentration changes in the dilated arterial system in various locations of the penis during visual sexual stimulation with real-time results. However, the proponents did not address the relationship between the dynamic changes in oxygenated hemoglobin concentrations and erectile function or penile arterial profiles. Consequently, a study on penile saturation during flaccid and erection periods in men with and without ED was conducted in 2007 by Padmanabhan et al., who found that men with ED have significantly lower corporal and glandular penile saturation during the flaccid period26. The study explored the relationship between resting saturation and erectile function but did not discuss data on the erection period. None of the above studies analyzed the dynamics of chromophores associated with arterial volume changes (Supplementary material Table S1).
EHS was negatively associated with the PPG amplitude in the end-erection period and positively correlated with RI. The correlation between EHS and RI can be attributed mostly to end-diastolic velocity during the end-erection period but not to maximal systolic velocity although a significant increase in maximal systolic velocity and a significant decrease in end-diastolic velocity were observed. Thus, penile hardness needs cumulative pressure in the engorged corporal tissue during end-erection. Burnett et al. established a series of spectral changes correlated to the volume change of the in vitro model system and use the optical signal changes (light absorption) to predict the actual penile blood volume change. They found that the blood volume percentage increase is correlated with erection quality (P < 0.001), penile rigidity (P < 0.005), and penile circumference increase (P < 0.0001). Additionally, the positive correlation between APD index and EHS indicates that penile hardness can be attributed to the dilation of the cavernous arteries during mid-erection and high ICP during the end-erection period during which engorged corporal tissue prevents blood to pass through or return to the venous system.
Peripheral PPG waveform (e.g., finger PPG) can be regarded as an alternative to arterial pressure waveform12. The decreased AI and RTI during the resting state can be a result of reduced compliance of the elastic arteries, thus causing an earlier return of the reflected wave12,29,30. The harder cavernous tissue (higher EHS or penile rigidity) can stiffen the local cavernous artery and cause the reflected wave to return sooner. The earlier superimposed reflected peak leads to a higher second peak, resulting in lower AI and shorter reflection time and, thus, a lower RTI. Therefore, the lower cavernous arterial RTI and AI were associated with lower IIEF and RI. However, the AI and RTI during the end-erection period could not be determined because the differences between the systolic and diastolic volumes were minimal. Therefore, AI and RTI derived during the mid-erection period may not be a good predictor for penile hardness during end erection.
It is believed that this is the first study to analyze the dynamics of PPG light absorption waveform characteristics correlated with erectile function, penile hardness, and penile Doppler ultrasound profiles. These findings demonstrate that PPG may be useful as a noninvasive, potential technique to evaluate penile erection and men’s health given the advantages (e.g., low cost, transportability, continuous data acquisition, and safety). The findings of this study demonstrate that PPG signal dynamics can potentially be applied to clinical penile hardness and erectile function assessments. For example, the clinical use of PPG signal dynamics can extend to collect the nighttime erection status and hardness, i.e., nocturnal penile tumescence (NPT) test. Thus, conducting an NPT test at home is feasible and more convenient. Moreover, the penile erection status during intercourse may also be objectively evaluated. In combination with a self-reported questionnaire, the clinicians can better understand and judge the quality of sexual life. The application of PPG device might potentially be a new idea of at-home erection quality evaluation. However, this study has some limitations. Firstly, a relatively small sample size (n = 68) was studied. Nevertheless, this is the PPG study with the biggest sample size to date. Secondly, some correlations of the derived parameters were weak. Thirdly, a control group of normal, healthy subjects was not used for comparison because of the risks of alprostadil administration. More comprehensive studies in the future are warranted. Furthermore, split-new EHS was used instead of EHS score because of the following reasons. First, the split-new EHS score is determined by two urologists at the end of the penile ultrasound examination. Thus, the split-new EHS score is more detailed and accurate than the EHS score reported by the patients. Second, erection hardness is found between the two integers from time to time (e.g., EHS 1 and 2, EHS 2 and 3, or EHS 3 and 4). Giving an integer score was difficult. Thus, a score of 0.5 (e.g., EHS 1.5 and EHS 2.5 or 3.5) was given. Third, more groupings allow the understanding of the relationship between PPG and erection quality in more detail. Nonetheless, the current findings on PPG use in ED studies add insights to further understand erectile dysfunction, penile arterial stiffness, and men’s health.
In conclusion, this is the first study to explore penile hemodynamics, chromophore dynamics, and men’s health via PPG. This study demonstrated an inverse correlation between PPG amplitude at the end of erection and EHS. Positive correlations were found between the APD index and EHS as well as IIEF and RI. RTI and AI are inversely correlated to erectile function (IIEF). From a practical point of view, PPG has the potential to be a promising, convenient, noninvasive, and safe to evaluate penile erection and men’s health.
Methods
All methods were carried out following relevant guidelines and regulations.
Experimental subjects and paradigm
Men experiencing ED (IIEF < 22) for at least 6 months and nominated for penile Doppler ultrasonography were registered in this study. Patients were excluded with previous penile trauma, history of hormone replacement therapy, post-penile prosthesis, venous leak-type ED, and neurological ED. From November 2019 to June 2020, 68 men were enrolled at the National Taiwan University Hospital. Penile Doppler ultrasonography parameters, PPG data, and retrospective historical chart reviews were collected and approved by the National Taiwan University Hospital institutional review board (201907031RINA). All data were collected by two urologists with signed informed consent obtained from all participants in the study. Demographic data included age, height, body weight, BMI, endothelial risk factors (diabetes, hypertension, dyslipidemia, or medications), and personal medical and sexual histories.
Experimental setup
Patients were laid down in the supine position, and 20 μg alprostadil (Caverject) was given via intracavernosal injection. PPG and penile Doppler ultrasonography were conducted 3 min after injection as mid-erection period signals. The PPG signals were collected for 2 min. PPG and penile Doppler ultrasonography were performed again for the end-erection period signals, also 2 min, when patients reached full-rigid penis status (Fig. 3). Penile Doppler ultrasonography was performed using high-frequency linear probes with the patient in the supine position. The peak systolic velocity (PSV) of the cavernous artery indicated that the highest speed detected at end-erection status (usually 20 min postpharmacostimulation) and the end-diastolic velocity (EDV) was also detected at the same time. RI is defined as the difference in PSV and EDV divided by PSV. RI helps predict venous leakage ED, which is excluded in the current population (RI, < 0.75). After completing the examinations, two urologists determined the split-new EHS right at the end of the penile Doppler test (split-new EHS scoring: 1, penis is larger but not hard; 1.5, the hardness score is between 1 and 2 or the penis tip score is 1 but the penis root score is 2; 2: penis is hard but not hard enough for penetration; 2.5: the hardness score is between 2 and 3 or the penis tip score is 2 but the penis root score is 3; 3: penis is hard enough for penetration but not completely hard; 3.5: the hardness score is between 3 and 4 or the penis tip score is 3 but the penis root score is 4; and 4: penis is completely hard and fully rigid).
The experimental setup: The patients simultaneously receive penile Doppler ultrasound and transmittance-type PPG examination (700 and 840 nm, sampling 32 Hz) in the supine position. Penile Doppler ultrasonography is performed using high-frequency linear probes. The light-emitting diode (LED) and photodetector are included each in a separate sensor. They are both fixed to the penile root by stickers, leaving enough space for penile inflation. The LED and photodetector sensors are located on the skin of the front and back of the cavernous artery. The correct placement was guided by ultrasonography and confirmed by urologists.
The PPG system and PPG waveforms
The light-emitting diode (LED) and photodetector are included each in a separate sensor. They are both fixed to the penile root by stickers, leaving enough space for penile inflation. The source detector distance is approximately 1.7 cm and increases with the inflation of the penis to 2.7 cm. The LED and photodetector sensors are located on the skin of the front and back of the cavernous artery. The correct placement was guided by ultrasonography and confirmed by urologists. The PPG system was approved by the Taiwan Food and Drug Administration and provided local tissue oxygen saturation and light absorption measurements sampled at 32 Hz. The transmittance-type PPG system consists of two LEDs at 700 nm and 840 nm as source of light and a light-dependent resistor as a photodetector. The PPG includes an amplifier, filter, and analog-to-digital converter. The light energy is absorbed by chromophores, i.e. mainly the oxy- and deoxy-hemoglobin in the corpus cavernosum when the light passes through the penile tissue. Thus, changes in the chromophore concentrations associated with hemodynamics were measured and recorded in real-time after removing the constant term (constant light absorption by the tissue and the venous hemoglobin, which is not pulsating), extracting a pulsatile PPG waveform. The instrument measures the arterial pulse wave, which is based on a higher chromophore concentration during systole and a lower concentration during diastole, which leads to a lower light intensity at the detector during systole and a higher one during diastole. The artery is dilated when blood pressure is increased. Thus, the real-time light absorption detected by the PPG detectors is correlated with the penile arterial pulsation. A second-order Butterworth band-pass filter was applied with a passband from 0.5 to 6.0 Hz to remove the noise.
PPG signal preprocessing and features extraction
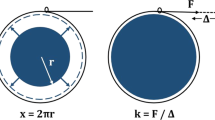
The noise using a second-order Butterworth filter at 0.5–6.0 Hz and detected beat-to-beat systolic pulsatile waveforms was suppressed after decoding the PPG signals. All beat-to-beat PPG waveforms were aligned with the peak and averaged to one representative template waveform for further feature analysis (Fig. 4a). The template waveform was used to calculate the parameters of the chromophore dynamics index. A first-order differential of the template waveform was made as a second derivative waveform to evaluate the vessel wall changes acceleration (Fig. 4b).
The calculation formula of reflection time index (RTI), augmentation index (AI), and perfusion index (PI). A: Template PPG waveform interpretation, A1 amplitude of systolic peak, A2 amplitude of diastolic peak, T1 time to reach the systolic peak, and T2 time to reach the diastolic peak B: Second derivative waveform transformed by the first-order differential of the template waveform for calculating PI.
The amplitudes (A1) of PPG signals (Fig. 4a) were calculated using template waveforms during the mid- and end-erection periods. APD is defined as the amplitude difference between the mid- and end-erection periods. The APD index is defined as the amplitude difference of the mid- and end-erection periods divided by the amplitude of the mid-erection period:
The fiducial points of the waveform are a consequence of a systolic pressure wave circulated forward to the peripheral vascular system being measured. In addition to the systolic pressure wave generated by the left ventricular contraction, the waveform also contains the second peak related to the reflected waves when the pressure wave reaches areas of turbulence or changes in lumen diameter (Fig. 4a)15,16,17. The RTI and AI of the arterial wave are widely used to assess vessel stiffness31,32. The RTI is defined as the time difference between the systolic and diastolic peaks in the arterial waveform (mid-erection period) divided by the total wave duration (Fig. 4a):
The AI is defined as the amplitude difference between the systolic and diastolic peaks divided by the systolic peak in the mid-erection period (Fig. 4a):
Otherwise, the first-order differential of the template waveform was considered as a second derivative waveform to evaluate the changes in vessel wall velocity. PI is defined as the amplitude above the baseline in the second derivative waveform divided by the amplitude of the total wave (Fig. 4b):
Statistical analysis
The baseline demographic characteristics are shown as the mean ± standard deviation for continuous variables and as proportions for categorical variables. Normality assumption was performed using the Shapiro–Wilk test in all the statistical tests. If the data present a normal distribution, the differences between groups were examined by one-way analysis of variance (ANOVA) with Tukey’s honestly significant difference post hoc comparison and Pearson’s correlation. Otherwise, the Kruskal–Wallis one-way ANOVA with pairwise post hoc comparison and Spearman’s rank correlation was applied for each of the measurements. All statistical analyses were performed using R software (version 3.5.0; R Foundation for Statistical Computing, Vienna, Austria) and IBM SPSS Statistics for Windows (version 22; IBM Corp., Armonk, NY, USA). A p value < 0.05 was considered statistically significant.
References
McCabe, M. P. et al. Definitions of sexual dysfunctions in women and men: a consensus statement from the fourth international consultation on sexual medicine 2015. J. Sex. Med. 13, 135–143. https://doi.org/10.1016/j.jsxm.2015.12.019 (2016).
Ayta, I. A., McKinlay, J. B. & Krane, R. J. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 84, 50–56. https://doi.org/10.1046/j.1464-410x.1999.00142.x (1999).
Sattar, A. A. et al. Correlation of nocturnal penile tumescence monitoring duplex ultrasonography and infusion cavernosometry for the diagnosis of erectile dysfunction. J. Urol. 155, 1274–1276 (1996).
Rosen, M. P. et al. Arteriogenic impotence: findings in 195 impotent men examined with selective internal pudendal angiography. Young Investigator’s Award. Radiology 174, 1043–1048. https://doi.org/10.1148/radiology.174.3.174-3-1043 (1990).
Beć, K. B. & Huck, C. W. Breakthrough potential in near-infrared spectroscopy: spectra simulation. A review of recent developments. Front. Chem. https://doi.org/10.3389/fchem.2019.00048 (2019).
Capraro, G. A. et al. Feasibility of using near-infrared spectroscopy to diagnose testicular torsion: an experimental study in sheep. Ann. Emerg. Med. 49, 520–525. https://doi.org/10.1016/j.annemergmed.2006.06.041 (2007).
Burnett, A. L. et al. Near infrared spectrophotometry for the diagnosis of vasculogenic erectile dysfunction. Int. J. Impot. Res. 12, 247–254 (2000).
Stothers, L., Guevara, R. & Macnab, A. Classification of male lower urinary tract symptoms using mathematical modelling and a regression tree algorithm of noninvasive near-infrared spectroscopy parameters. Eur. Urol. 57, 327–332. https://doi.org/10.1016/j.eururo.2009.05.004 (2010).
Macnab, A. J., Stothers, L. S. & Shadgan, B. Monitoring detrusor oxygenation and hemodynamics noninvasively during dysfunctional voiding. Adv. Urol. 2012, 676303. https://doi.org/10.1155/2012/676303 (2012).
Farag, F. F., Martens, F. M., D’Hauwers, K. W., Feitz, W. F. & Heesakkers, J. P. Near-infrared spectroscopy: a novel, noninvasive, diagnostic method for detrusor overactivity in patients with overactive bladder symptoms–a preliminary and experimental study. Eur. Urol. 59, 757–762. https://doi.org/10.1016/j.eururo.2010.12.032 (2011).
Akl, T. J., Wilson, M. A., Ericson, M. N. & Coté, G. L. Quantifying tissue mechanical properties using photoplethysmography. Biomed. Opt. Express 5, 2362–2375. https://doi.org/10.1364/boe.5.002362 (2014).
Reisner, A., Shaltis, P. A., McCombie, D. & Asada, H. H. Utility of the photoplethysmogram in circulatory monitoring. Anesthesiology 108, 950–958. https://doi.org/10.1097/ALN.0b013e31816c89e1 (2008).
Shelley, K. H. Photoplethysmography: beyond the calculation of arterial oxygen saturation and heart rate. Anesth. Analg. 105, S31–S36. https://doi.org/10.1213/01.ane.0000269512.82836.c9 (2007).
Rastrelli, G. & Maggi, M. Erectile dysfunction in fit and healthy young men: psychological or pathological?. Transl. Androl. Urol. 6, 79–90. https://doi.org/10.21037/tau.2016.09.06 (2017).
Stein, M. J., Lin, H. & Wang, R. New advances in erectile technology. Ther. Adv. Urol. 6, 15–24. https://doi.org/10.1177/1756287213505670 (2014).
Lavoisier, P., Barbe, R. & Gally, M. Validation of a continuous penile blood-flow measurement by pulse-volume-plethysmography. Int. J. Impot. Res. 14, 116–120. https://doi.org/10.1038/sj.ijir.3900840 (2002).
Lavoisier, P., Courtois, F., Proulx, J., Durand, L. G. & de Carufel, F. Validation of a non-invasive device to measure intracavernous pressure as an index of penile rigidity. Br. J. Urol. 65, 624–628. https://doi.org/10.1111/j.1464-410x.1990.tb14833.x (1990).
Waxman, S. E. & Pukall, C. F. Laser Doppler imaging of genital blood flow: a direct measure of female sexual arousal. J. Sex. Med. 6, 2278–2285. https://doi.org/10.1111/j.1743-6109.2009.01326.x (2009).
Wolf, M., Ferrari, M. & Quaresima, V. Progress of near-infrared spectroscopy and topography for brain and muscle clinical applications. J. Biomed. Opt. 12, 062104. https://doi.org/10.1117/1.2804899 (2007).
Colier, W. N., Froeling, F. M., de Vries, J. D. & Oeseburg, B. Measurement of the blood supply to the abdominal testis by means of near infrared spectroscopy. Eur. Urol. 27, 160–166. https://doi.org/10.1159/000475150 (1995).
Macnab, A., Stothers, L. & Shadgan, B. Dynamic topographic mapping of the human bladder during voiding using functional near-infrared spectroscopy. J. Biomed. Opt. 14, 020507. https://doi.org/10.1117/1.3122886 (2009).
Mastoroudes, H. et al. Use of near infrared spectroscopy as an alternative to videourodynamics to detect detrusor overactivity in women with the overactive bladder syndrome. Urology 80, 547–550. https://doi.org/10.1016/j.urology.2012.05.036 (2012).
Macnab, A. J. & Stothers, L. Near-infrared spectroscopy: validation of bladder-outlet obstruction assessment using non-invasive parameters. Can. J. Urol. 15, 4241–4248 (2008).
Macnab, A. J., Shadgan, B., Stothers, L. & Afshar, K. Ambulant monitoring of bladder oxygenation and hemodynamics using wireless near-infrared spectroscopy. Can. Urol. Assoc. J. 7, E98–E104. https://doi.org/10.5489/cuaj.271 (2013).
Macnab, A. J. & Stothers, L. Development of a near-infrared spectroscopy instrument for applications in urology. Can. J. Urol. 15, 4233–4240 (2008).
Padmanabhan, P. & McCullough, A. R. Penile oxygen saturation in the flaccid and erect penis in men with and without erectile dysfunction. J. Androl. 28, 223–228. https://doi.org/10.2164/jandrol.106.001313 (2007).
Paul Kudlow, B. R. Near-infrared spectroscopy to assess penile blood flow: a possible novel technique for the diagnosis of vasculogenic erectile dysfunction. Univ. West. Ont. Med. J. 80, 7–8 (2011).
Kim, E., Lee, S., Phillips, Z. T. & Kim, J. G. A discrepancy of penile hemodynamics during visual sexual stimulation observed by near-infrared spectroscopy. BMC Urol. 15, 11. https://doi.org/10.1186/s12894-015-0005-x (2015).
Elgendi, M. On the analysis of fingertip photoplethysmogram signals. Curr. Cardiol. Rev. 8, 14–25. https://doi.org/10.2174/157340312801215782 (2012).
Millasseau, S. C., Kelly, R. P., Ritter, J. M. & Chowienczyk, P. J. Determination of age-related increases in large artery stiffness by digital pulse contour analysis. Clin. Sci. (London, England: 1979) 103, 371–377. https://doi.org/10.1042/cs1030371 (2002).
Barodka, V. M., Joshi, B. L., Berkowitz, D. E., Hogue, C. W. Jr. & Nyhan, D. Review article: implications of vascular aging. Anesth. Analg. 112, 1048–1060. https://doi.org/10.1213/ANE.0b013e3182147e3c (2011).
Sharman, J. E. & Marwick, T. H. Arterial stiffness: measurement and significance in management of hypertension. Indian Heart J. 62, 378–383 (2010).
Acknowledgements
The authors would like to thank the staff at National Taiwan University Hospital for their assistance with patient recruitment and data collection.
Author information
Authors and Affiliations
Contributions
Y.H.P., Y.K.C., V.F.S.T., and C.L. designed the study. Y.H.P., Y.K.C., C.E.H., Y.C.L., and P.C.C. acquired the samples and clinical outcomes. Y.H.P., Y.K.C., and H.C.C. carried out the experimental work. C.E.H., M.Z.L., and C.L. carried out the analysis. Y.H.P. and Y.K.C. wrote the paper, which was edited by C.L. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pong, YH., Chang, YK., Hsu, CE. et al. Probing penile hemodynamics by using photoplethysmography as objective indicators for male erection quality and sexual function. Sci Rep 11, 12019 (2021). https://doi.org/10.1038/s41598-021-91582-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91582-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.