Abstract
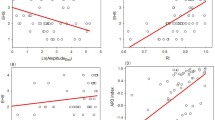
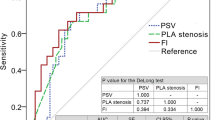
Measurement of blood flow velocity through the cavernosal arteries via penile color Doppler ultrasound (PDUS) is the most common objective method for the assessment of erectile function. However, in some clinical cases, this method needs to be augmented via the invasive intracavernosal pressure (ICP) measurement, which is arguably a more direct index for erectile function. The aim of this study is to develop a lumped parameter model (LPM) of the penile circulation mechanism integrated to a pulsatile, patient-specific, bi-ventricular circulation system to estimate ICP values non-invasively. PDUS data obtained from four random patients with erectile dysfunction are used to develop patient-specific LPMs. Cardiac output is estimated from the body surface area. Systemic pressure is obtained by a sphygmomanometer. Through the appropriate parameter set determined by optimization, patient-specific ICP values are predicted with only using PDUS data and validated by pre- and post-papaverine injection cavernosometry measurements. The developed model predicts the ICP with an average error value of 3 mmHg for both phases. Penile size change during erection is predicted with a ~15% error, according to the clinical size measurements. The developed mathematical model has the potential to be used as an effective non-invasive tool in erectile function evaluation, expanding the existing clinical decision parameters significantly.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Feldman H, Goldstein I, Hatzichristou DG, Krane R, J.B. M. Impotence and ıts medical and psychosocial correlates: results of the Massachusetts male aging study. J Urol. 1994;151:54–61.
Aytac IA, McKinlay JB, Krane R. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–6.
Kruyt R, AA G. Color Doppler analysis of penile arteries in impotence. Radiology. 1988;169:283.
Bookstein JJ, Valji K, Parsons L, Kessler W. Penile pharmacocavernosography and cavernosometry in the evaluation of impotence. J Urol. 1987;137:772–6.
Halls J, Bydawell G, Patel U. Erectile dysfunction: the role of penile Doppler ultrasound in diagnosis. Abdom Imaging. 2009;34:712–25.
Fuselier HA, Allen JM, Annaloro A, Morgan JO. Incidence and simple management of priapism following dynamic infusion cavernosometry cavernosography. South Med J. 1993;86:1261–3.
Kilic M, Serefoglu EC, Ozdemir AT, Balbay MD. The actual incidence of papaverine-induced priapism in patients with erectile dysfunction following penile colour Doppler ultrasonography. Andrologia. 2010;42:1–4.
Connolly JA, Borirakchanyavat S, Lue TF. Ultrasound Evaluation of the Penis for Assessment of Impotence. J Clin Ultrasound. 1996;24:481–6.
Sikka S, Hellstrom W, Brock G, Morales A. Standardization of Vascular Assessment of Erectile Dysfunction. J Sex Med. 2012;10:120–9.
Teloken PE, Park K, Parker M, Guhring P, Narus J, Mulhall JP. The false diagnosis of venous leak: Prevalence and predictors. J Sex Med. 2011;8:2344–9.
Borowitz E, Barnea O. Hemodynamic mechanisms of penile erection. IEEE Trans Biomed Eng. 2000;47:319–26.
Barnea O, Gillon G. Cavernosometry: A theoretical analysis. Int J Impot Res. 2004;16:154–9.
Gillon G, Barnea O. Erection mechanism of the penis: a model based analysis. J Urol. 2002;168:2711–5.
Barnea O, Hayun S, Gillon G. A mathematical model of penile vascular dysfunction and its application to a new diagnostic technique. Ann N. Y Acad Sci. 2007;1101:439–52.
Hoppensteadt FC, Peskin CS. The heart and circulation. In: Mathematics in medicine and the life sciences. New York: Springer Science; 1992. p. 105–39.
Sundareswaran KS, Pekkan K, Dasi LP, Whitehead K, Sharma S, Kanter KR, et al. The total cavopulmonary connection resistance: a significant impact on single ventricle hemodynamics at rest and exercise. Am J Physiol Hear Circ Physiol. 2008;295:2427–35.
Pekkan K, Frakes D, De Zelicourt D, Lucas CW, Parks WJ, Yoganathan AP. Coupling pediatric ventricle assist devices to the Fontan circulation: simulations with a lumped-parameter model. ASAIO J. 2005;51:618–28.
Yigit MB, Kowalski WJ, Hutchon DJR, Pekkan K. Transition from fetal to neonatal circulation: Modeling the effect of umbilical cord clamping. J Biomech. 2015;48:1662–70.
Sagawa K, Lie RK, Schaefer J. Translation of Otto frank’s paper ‘Die Grundform des Arteriellen Pulses’ Zeitschrift für Biologie 37: 483-526 (1899). J Mol Cell Cardiol. 1990;22:253–4.
Milišić V, Quarteroni A. Analysis of lumped parameter models for blood flow simulations and their relation with 1D models. ESAIM Math Model Numer Anal. 2004;38:613–32.
Juillet B, Bos C, Gaudichon C, Tomé D, Fouillet H. Parameter estimation for linear compartmental models-a sensitivity analysis approach. Ann Biomed Eng. 2009;37:1028–42.
Eberhart R, Kennedy J. A new optimizer using particle swarm theory. In: MHS’95 Proceedings of the Sixth International Symposium on Micro Machine and Human Science. p. 39–43.
Kennedy J, Eberhart R. Particle swarm optimization. Proc. IEEE Int Conf. 1995;4:1942–8.
Eberhart R, Shi Y. Particle swarm optimization: developments, applications and resources. Proc 2001 Congr Evol Comput (IEEE Cat No01TH8546). 2002;1:81–6.
MathWorks. Global Optimization Toolbox User’s Guide (R2018a). 2018.
Luenberger DG. Least-squares estimation. In: Optimization by vector space methods. John Wiley & Sons; 1970. p. 78–102.
Jegier W, Sekelj P, Auld PA, Simpson R, McGregor M. The relation between cardiac output and body size. Br Heart J. 1963;25:425–30.
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peñ BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26.
Turunc T, Deveci S, Guvel S, Peskircioglu L. The assesment of Turkish validation with 5 question version of Iinternational index of erectile function (IIEF-5). Turkish. J Urol. 2007;33:45–9.
Moons K, Altman D, Reitsma J, Ioannidis J, Macaskill P, Steyerberg E et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162:W1–73.
Chen J, Gefen A, Greenstein A, Matzkin H, Elad D. Predicting penile size during erection. Int J Impot Res. 2000;12:328–33.
Nelson RP, Lue TF. Determination of erectile penile volume by ultrasonography. J Urol. 1989;141:1123–6.
Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381:153–65.
Andersson K-E, Wagner G. Physiology of penile erection. Physiol Rev. 1995;75:191–218.
Lue TF, Takamura T, Schmidt RA, Palubinskas AJ, Tanagho EA. Hemodynamics of Erection in the Monkey. J Urol. 1983;130:1237–41.
McVeigh G, Allen P, Morgan D. Arterial compliance: a new measure of therapeutic efficacy. In: Kaplan NM, editor. Hypertension therapy annual. Taylor & Francis; 2002. p. 111–28.
Kuo Y, Liu S, Chen J, Chang H, Tsai VFS, Hsieh J. Feasability of a novel audio-video sexual stimulation system: an adjunct to the use of penile duplex Doppler. Ultrasonography 2009;7:3979–83.
Lee B, Sikka S, Randrup E, Villemarette P, Baum N, Hower J, et al. Standardization of penile blood flow parameters in normal men using intracavernous prostaglandin E1 and visual sexual stimulation. J Urol. 1993;149:49–52.
Mellinger B, Vaughan E Jr. Penile blood flow changes in the flaccid and erect state in potent young men measured by duplex scanning. J Urol. 1990;144:894–6.
Speel TGW, Van Langen H, Wijkstra H, Meuleman EJH. Penile duplex pharmaco-ultrasonography revisited: revalidation of the parameters of the cavernous arterial response. J Urol. 2003;169:216–20.
Chung E, De Young L, Brock GB. Penile duplex ultrasonography in men with Peyronie’s disease: is it veno-occlusive dysfunction or poor cavernosal arterial inflow that contributes to erectile dysfunction? J Sex Med. 2011;8:3446–51.
Serefoglu EC, Trost L, Sikka SC, Hellstrom WJG. The direction and severity of penile curvature does not have an impact on concomitant vasculogenic erectile dysfunction in patients with Peyronie’s disease. Int J Impot Res. 2015;27:6–8.
Serefoglu EC, Atmaca AF, Dogan B, Altinova S, Akbulut Z, Balbay MD. Problems in understanding the Turkish translation of the international index of erectile function. J Androl. 2008;29:369–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yildirim, C., Erturk, H., Pekkan, K. et al. A novel method for hemodynamic analysis of penile erection. Int J Impot Res 34, 55–63 (2022). https://doi.org/10.1038/s41443-020-00362-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-00362-y