Abstract
Nutrient intake for adult cancer survivors is of clinical importance for managing metabolic health. Whether dietary fiber intake is associated with metabolic syndrome (MetS) or not in adult cancer survivors is uncertain. We aim to investigate the association between dietary fiber intake and MetS in adult cancer survivors using a population-based cross-sectional study. A study sample of 1301 adult cancer survivors aged more than 20 years from the sixth and seventh Korea Nutrition Examination Survey (KNHANES) from 2013 to 2018 was identified. Odds ratio (OR) and 95% confidence intervals (95% CI) were estimated from multiple logistic regression adjusted for sociodemographic factors, health behavior, and nutritional status. Among 1,301 adult cancer survivors identified from the KNHANES 2013–2018, the mean dietary fiber intake was 28.1 g/day (standard error, 0.54). Compared to the first quintile of dietary fiber intake, the adjusted ORs and 95% CIs for MetS in the second, third, fourth, and fifth quintiles of dietary fiber intake were 0.84 (0.27–2.61), 0.77 (0.16–3.74), 0.55 (0.14–2.22), and 0.26 (0.05–1.39), respectively (p value for trend = 0.0007). Our findings suggest that high dietary fiber intake is marginally associated with reduced odds of MetS in adult cancer survivors.
Similar content being viewed by others
Introduction
Nutrition and Physical Activity Guidelines for Cancer Survivors were released by the American Cancer Survivors (ACS) in 20121. The ACS recommends that cancer survivors take sufficient dietary fiber as a part of healthy and balanced diet such as lower proportion of dietary saturated fat with emphasis on vegetables and fruits intake for improved health outcomes2,3,4. Based on the most recent meta-analysis of cross-sectional and cohort studies reported in 2018, high dietary intake of fiber is inversely associated with metabolic syndrome (MetS) in the general population5,6. The accumulated evidence shows limited association and dose–response relationship between dietary fiber intake and MetS, potentially owning to the limited data from cohort studies. Furthermore, on the basis of the currently available guidelines and evidence, association between dietary fiber intake and MetS has not been clearly established, especially in the cancer survivors whose potential health benefits from dietary fiber is of public health importance for policy to support cancer survivors7,8,9,10.
High intake of dietary fiber has been inversely associated with MetS in some of the general and vulnerable populations at risk, but not all studies showed statistically significant associations despite the potential mechanisms supporting its benefit for metabolic health11,12,13,14. In addition, evidence from an observational study of non-metastatic colon cancer survivors in the United States showed some health benefits of dietary fiber intake including reduced mortality from cancer and any cause15. Yet, there is insufficient evidence for cancer survivors on the health benefits of dietary fiber intake in relation to MetS, which is an important clinical outcome for long-term health in cancer survivors16,17,18.
We therefore conducted the present study to evaluate the association between dietary fiber intake and MetS in adult cancer survivors from a nationally representative cross-sectional survey including sociodemographic, health behavior, health status, and dietary assessment.
Results
Characteristics of the study population
Sociodemographic, health behavior, clinical and nutritional status according to quintiles of dietary fiber intake in adult cancer survivors identified in the sixth and seventh KNHANES (2013–2018) are shown in Table 1. The mean dietary fiber intake was 28.1 g/day (standard error [SE], 0.54) and median (interquartile range, IQR) dietary fiber intake from the first quintile to the fifth quintile were 12.0 g/day (IQR: 9.0 to 14.0), 19.0 g/day (IQR: 17.0 to 20.0), 25.0 g/day (IQR: 23.0 to 27.0), 33.0 g/day (30.0 to 35.0), and 49.0 g/day (43.0 to 59.0), respectively. The adult cancer survivors in the highest quintile of dietary fiber intake were relatively young, with higher education attainment, and had healthy lifestyle (lower smoking and alcohol consumption rate and physically active). Across the quintiles of dietary fiber intake among adult cancer survivors, there was no statistically significant difference for metabolic risk profile. However, total energy intake was reported to be the highest in the adult cancer survivors of the fifth quintile of dietary fiber intake compared to the rest. Similar patterns were found for carbohydrate, fat, and protein intake.
Association between dietary fiber intake and MetS in adult cancer survivors
In this cross-sectional study, multivariable logistic regression analyses showed a marginally inverse association between dietary fiber intake and MetS in adult cancer survivors. Compared to the lowest category of dietary fiber intake (the first quintile), the adjusted OR and 95% CI for MetS in the second, third, and fifth quintile were 0.93 (0.31–2.79), 0.91 (0.25–3.37), 0.66 (0.20–2.21), and 0.30 (0.09–1.00) for Model 1 (adjusted for age, sex, and physical activity), 0.87 (0.28–2.68), 0.81 (0.19–3.46), 0.59 (0.17–2.03), and 0.29 (0.09–0.92) for Model 2 (adjusted for household income, education level, cigarette smoking, alcohol consumption in addition to the variables included in Model 1), 0.84 (0.27–2.61), 0.77 (0.16–3.74), 0.55 (0.14–2.22), and 0.26 (0.05–1.39) for Model 3 (adjusted for variables included in Model 2 and total energy intake), respectively. P-value for linear trend across the quintiles of the dietary fiber intake in association with MetS for Model 1, Model 2, and Model 3 were 0.0001, 0.0004, and 0.0007, respectively (Table 2). Similar to the analysis of the association between dietary fiber intake as categorical values and MetS, the restricted cubic splines showed the marginally protective association of dietary fiber intake with MetS with confidence intervals exceeding the statistical significance level in adult cancer survivors (Fig. 1). The association between dietary fiber intake and MetS in cancer survivors did not significantly vary by the sociodemographic (age, sex, household income, education level), health behavior (cigarette smoking, alcohol consumption, physical activity) and nutritional status (total energy intake) for the lowest (the first quintile) versus highest (the fifth quintile) analyses (p value for > 0.05 interaction for all comparisons) (Table 3).
Relation between dietary fiber intake and metabolic syndrome in adult cancer survivors in the Korea National Health and Nutrition Examination Survey VI and VII (2013–2018), fitted with restricted cubic splines. The curves above are adjusted for sociodemographic (age, sex, education level, household income), health behavior (physical activity, cigarette smoking, alcohol consumption) and nutritional status (total energy intake).
Discussion
In the current study, we found a marginally protective association between high dietary fiber intake with MetS in community-dwelling adult cancer survivors. Compared to the lowest dietary fiber intake, the highest dietary fiber intake was associated with 74% lower odds of MetS that did not reach statistical significance after adjusting for potential confounders. However, the overall linear trend across the quintiles of dietary fiber intake in relation to the odds of MetS was observed.
Our results from this study are similar to those cross-sectional and cohort studies showing relationship between dietary fiber and MetS in both general population and vulnerable population at risk. A recent meta-analysis based on 11 cross-sectional and 3 cohort studies comprised of 26,403 total study subjects have shown that dietary fiber intake was inversely associated with MetS with lower risk comparing the highest with the lowest intake5. Pooled together, cross-sectional studies showed 30% lower odds and cohort studies showed 14% decreased risk of MetS in the highest consumption of dietary fiber compared to the lowest category. However, high heterogeneity and publication bias were found in the cross-sectional studies and the pooled relative risk from the cohort studies did not reach statistical significance. One of the notable studies conducted in Asia included in this meta-analysis was the study based on the Fukuoka Diabetes Registry (FDR) with 4,399 participants, which showed an inverse relationship of dietary fiber with MetS (OR: 0.92; 95% CI: 0.89–0.96)19. While the findings from our study and the FDR study is comparable, the definition of MetS in the FDR was harmonizing the metabolic syndrome20, which excludes the impaired fasting glucose as the components compared to the NCEP-ATP III definition. In addition, the study subjects of the FDR were limited to the participants with diabetes mellitus. Our study was focused on the association of dietary fiber intake with MetS in adult cancer survivors with limited statistical evidence supporting the protective association.
Only a few previous studies have investigated the health benefits of fiber intake in the high risk population including cancer survivors. In the prospective study of health professionals after diagnosis of non-metastatic colorectal cancer (CRC) in the U.S cohort, the Nurses’ Health Study (NHS) and Health Professionals Follow-up Study (HPFS) showed that high fiber intake was associated with lower CRC-specific and all-cause mortality supporting evidence for improved health outcome for high fiber consumption15. In addition, two studies from the NHS and HPFS, high dietary fiber intake was inversely associated with mortality among the survivors of myocardial infarction (MI)21. Taken together, these findings provide evidence that high dietary fiber intake is associated with better health outcomes in the vulnerable populations such as patients diagnosed with CRC or MI. However, the endpoint of these studies from the two large U.S cohorts were mortality instead of MetS. Our study investigated the health benefits of dietary fiber intake for MetS and found that high dietary fiber intake is marginally associated with lower odds of MetS.
High dietary fiber intake has been linked to improving components of MetS with potential mechanisms that support the beneficial role albeit these do not fully suggest that exact mechanisms could be directly applied to adult cancer survivors. Consumption of high fiber may reduce abdominal obesity through regulating energy homeostasis and altering gut microbiota22,23. High fiber intake is also reported to have cholesterol-lowering effect potentially attributable to reducing glycemic response after food consumption along with appetite control (i.e. inducing satiation and satiety)24. Previous observational studies consistently reported that high dietary fiber intake is inversely associated with the risk of type 2 diabetes mellitus and suggested that consumption of high dietary fiber may modulate inflammatory cytokines (e.g. interleukin-1 (IL-1), IL-12, and IL-18, tumor necrosis factor alpha (TNF-α), interferon gamma (IFNγ), and granulocyte–macrophage colony stimulating factor (GM-CSF)) and substantially improve glucose hemostasis25,26,27. Unlike the possible mechanisms that may partially explain the protective role of dietary fiber on MetS, mechanism behind consumption of high dietary fiber intake and reduced systolic and diastolic blood pressure is poorly understood. While these mechanisms are widely used to support the previous studies that reported protective association of high dietary fiber intake with MetS, the findings of our study showed that the association was not substantial, but rather marginal, possibly due to the limited statistical power for the adult cancer survivors identified in the KNHANES.
The most notable strength in this study includes assessment of dietary fiber intake in relation to MetS using a population-based sample of adult cancer survivors, which was understudied yet an important issue for clinical nutrition in cancer survivors. However, there are some limitations in this study that should be addressed when interpreting the results from the perspective of public health policy and clinical practice for adult cancer survivors. First, information on dietary fiber intake was obtained from the self-administered 24-h recall questionnaire in the KNHANES, which were not validated through consistent dietary records of the study participants. Thus, under or over estimation of dietary fiber intake in this study was inevitable due to the limited source of the dietary assessment. Considering the inevitable recall bias and other limitations of the 24-h recall approach for dietary fiber intake assessment, the future studies validating the results of this study with different dietary assessment methods are needed28. Second, we were not able to extensively consider other confounding variables that were not included in the KNHANES. Third, we were only able to conduct cross-sectional data analysis due to the study design of the KNHANES. Therefore, we were not able to determine whether the adult cancer survivors with high dietary fiber intake already had less odds of MetS or were less likely to develop newly diagnosed MetS in the follow-up period. Finally, the generalizability of the results found in this study might be limited because the sampling weight of the KNHANES was not originally designed to represent the entire population of cancer survivors in the Republic of Korea. Therefore, the weighted analyses conducted in accordance with the sampling design of the KNHANES could not fully reflect the entire cancer survivors from a statistical standpoint.
Evidence-based dietary guidelines for adult cancer survivors for the adequate range of daily dietary fiber intake for improving metabolic health needs further investigation as our study had limited statistical power. A marginally protective trend was observed for high dietary fiber intake and MetS up to approximately 43.0 g/day of dietary fiber intake in the restricted cubic splines with wide confidence intervals.
In conclusion, among the community-dwelling adult cancer survivors in the Republic of Korea, we observed marginally protective association of dietary fiber intake with MetS. As a part of the nutritional approaches to reduce the odds of MetS for adult cancer survivors, beneficial effects of increase in dietary fiber intake from variety of food consumption such as fruit, leafy vegetables, beans and whole grains should be carefully reviewed. Future investigations on the association of dietary fiber intake and MetS in adult cancer survivors should include well-designed observational studies or randomized clinical trials to update and support the evidence on the current guidelines on clinical nutrition for cancer survivors.
Materials and methods
Study population, design, and data collection
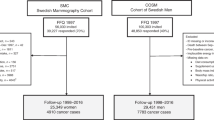
The study population in this study were community-dwelling cancer survivors who participated in the sixth and seventh Korea National Health and Nutrition Examination Survey (KNHANES VI-VII, 2013–2018), a nationally representative cross-sectional study consist of non-institutionalized individuals that initiated in 1998 by the Korea Disease Control and Prevention Agency (KDCA) in the Republic of Korea. Details of the KNHANES are available elsewhere29 and the KNHANES database had been used in various studies previously30,31,32,33,34. Among the participants of the sixth and seventh KNHANES, we identified 1632 adult (aged more than 20 years) cancer survivors from the self-reported questionnaire on the history of any type of cancer diagnosis. Of these adult cancer survivors in the dataset, we excluded those with missing information on dietary fiber intake information from the self-administered 24-h dietary recall (N = 101), missing information on the components of MetS (N = 78), and missing information on confounding variables (N = 152). The final study population included 1301 adult cancer survivors (Fig. 2).
Assessment of dietary fiber intake
The self-administered 24-h recall questionnaire for daily dietary intake in the KNHANES was used to assess the dietary fiber intake (grams per day, g/day) among cancer survivors. Based on this information, dietary fiber intake was divided into quintiles from the lowest (the first quintile) to the highest (the fifth quintile), and the median and interquartile ratio (IQR) were obtained for each quintile. The validity of the self-administered 24-h recall questionnaire for dietary assessment has been described previously35. In addition, a previous study reported that 24-h recall method in the KNHANES had high correlation with the Food Frequency Questionnaire for usual portion size and consumption-day intake36.
Definition of metabolic syndrome
Parts of the sixth and seventh KNHANES (2013–2018) consists of laboratory data, anthropometric measurements by trained medical staff and survey on clinical treatment for few diseases. Based on these data, we collected information on waist circumference (WC), systolic blood pressure (SBP), diastolic blood pressure (DBP), antihypertensive drug use, serum high density lipoprotein cholesterol (HDL-C), serum triglycerides (TG), lipid-lowering drug use, fasting serum glucose (FSG), and hypoglycemic agent or insulin treatment. We defined MetS according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATPIII) modified for the Asian population37,38,39. Therefore, cancer survivors in the KNHANES with at least three of the following components were defined as having MetS: (1) abdominal obesity (WC ≥ 90 cm for men and WC ≥ 85 cm for women, respectively); (2) elevated TG (serum TG ≥ 150 mg/dL or lipid-lowering drug use); (3) reduced HDL-C (serum HDL-C ≤ 40 mg/dL for men and ≤ 50 mg/dL for women, respectively); (4) elevated BP (SBP ≥ 130 mmHg or DBP ≥ 85 mmHg or with antihypertensive drug use); (5) elevated FSG (serum FSG ≥ 100 mg/dL or receiving hypoglycemic agent or insulin treatment). The modified definition of MetS in the KNHANES were used in the previous studies.
Assessment of confounding variables
We obtained information on sociodemographic (age, sex, household income, and education level), health behavior (cigarette smoking, physical activity, and alcohol consumption), and dietary intake (total energy intake, carbohydrate intake, fat intake, and protein intake) from self-reported survey in the KNHANES. The household income was calculated from the summation of total income among household members divided by the square root of the number of household members. Physical activity was categorized into engaging in aerobic exercise, muscle-strengthening exercise, and balance and flexibility exercise in accordance to the recommended types of physical activity listed in the Physical Activity Guidelines for Americans, 2nd edition released in 201840.
Statistical analysis
To take complex, multistage, and probability sampling design of the KNHANES into account in all of the statistical analyses in this study, we used the appropriate procedure in the statistical software (e.g. “PROC SURVEYFREQ” and “svy” commands in SAS and STATA, respectively) for the results to represent the entire population of the Republic of Korea. Characteristics of the cancer survivors according to quintiles of dietary fiber intake were assessed using numbers (percentages) for categorical variables and means (standard error [SD]) for continuous variables with survey weights of the KNHANES taken into consideration. We used chi-squared test to compare the categorical variables and survey-weighted linear regression model to compute linear trend of the continuous variables, respectively. To estimate the odds of MetS according to quintiles of dietary fiber intake among cancer survivors, we used multiple logistic regression models and computed odds ratio (OR) and 95% confidence intervals (95% CI) using the lowest dietary fiber intake (the first quintile) as reference. First, we developed a minimally adjusted model (Model 1 adjusted for age, sex, and physical activity). In addition to Model 1, Model 2 was further adjusted for household income, education level, cigarette smoking, and alcohol consumption. Finally, Model 3 was adjusted for total energy intake with all other variables included in Model 2. To further assess the relation between dietary fiber intake and MetS among cancer survivors, we used restricted cubic splines of dietary fiber intake with five knots using multiple logistic regression adjusted for all of the variables included in Model 3. All analyses in this study were conducted using SAS software version 9.4 (SAS Institute., NC, USA) and STATA 14 (STATA Corp., College Station, TX, USA). p values less than 0.05 were considered statistically significant.
Ethics statement
The protocols, conduct of the research, and data release for the sixth and seventh KNHANES (2013–2018) was approved by the KCDA Institutional Review Board (2013-12EXP-03-5C). All of the participants provided informed consent prior to participating in the KNHANES. This study was conducted in accordance to the guidelines of the Declaration of Helsinki-ethnical principles for medical research involving human subjects. The KNHANES dataset is publicly available for research purpose upon approval by the KDCA (www.kdca.go.kr).
References
Rock, C. L. et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J. Clin. 62, 242–274 (2012).
Lupton, J. R. et al. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids Vol. 5, 589–768 (National Academy Press, 2002).
Fradet, Y., Meyer, F., Bairati, I., Shadmani, R. & Moore, L. Dietary fat and prostate cancer progression and survival. Eur. Urol. 35, 388–391 (1999).
Kim, D. J. et al. Premorbid diet in relation to survival from prostate cancer (Canada). Cancer Causes Control 11, 65–77 (2000).
Chen, J.-P., Chen, G.-C., Wang, X.-P., Qin, L. & Bai, Y. Dietary fiber and metabolic syndrome: a meta-analysis and review of related mechanisms. Nutrients 10, 24 (2018).
Wei, B. et al. Dietary fiber intake and risk of metabolic syndrome: a meta-analysis of observational studies. Clin. Nutr. 37, 1935–1942 (2018).
Murphy, J. L. & Girot, E. A. The importance of nutrition, diet and lifestyle advice for cancer survivors—the role of nursing staff and interprofessional workers. J. Clin. Nurs. 22, 1539–1549 (2013).
Brown, J. et al. Nutrition during and after cancer treatment: A guide* for informed choices by cancer survivors. CA: A Cancer Journal for Clinicians 51, 153–181 (2001).
Keaver, L., Yiannakou, I., Folta, S. C. & Zhang, F. F. Perceptions of oncology providers and cancer survivors on the role of nutrition in cancer care and their views on the “nutricare” program. Nutrients 12, 1277 (2020).
Mohammadi, S., Sulaiman, S., Koon, P. B., Amani, R. & Hosseini, S. M. Association of nutritional status with quality of life in breast cancer survivors. Asian Pac. J. Cancer Prev. 14, 7749–7755 (2013).
Carlson, J. J., Eisenmann, J. C., Norman, G. J., Ortiz, K. A. & Young, P. C. Dietary fiber and nutrient density are inversely associated with the metabolic syndrome in US adolescents. J. Am. Diet. Assoc. 111, 1688–1695 (2011).
Galisteo, M., Duarte, J. & Zarzuelo, A. Effects of dietary fibers on disturbances clustered in the metabolic syndrome. J. Nutr. Biochem. 19, 71–84 (2008).
Hosseinpour Niazi, S., Mirmiran, P., Sohrab, G., Hosseini Esfahani, F. & Azizi, F. Association between dietary fiber intake and metabolic syndrome: Tehran lipid and glucose study. Iran. J. Epidemiol. 7, 19–28 (2012).
Ventura, E. E. et al. Dietary intake and the metabolic syndrome in overweight Latino children. J. Am. Diet. Assoc. 108, 1355–1359 (2008).
Song, M. et al. Fiber intake and survival after colorectal cancer diagnosis. JAMA Oncol. 4, 71–79 (2018).
De Haas, E. C. et al. The metabolic syndrome in cancer survivors. Lancet Oncol. 11, 193–203 (2010).
Nuver, J., Smit, A. J., Postma, A., Sleijfer, D. T. & Gietema, J. A. The metabolic syndrome in long-term cancer survivors, and important target for secondary preventive measures. Cancer Treat. Rev. 28, 195–214 (2002).
Kim, M., Kim, I.-H., Lim, M. K., Kim, Y. & Park, B. Increased prevalence of metabolic syndrome in adult cancer survivors: Asian first report in community setting. Cancer Epidemiol. 58, 130–136 (2019).
Fujii, H. et al. Impact of dietary fiber intake on glycemic control, cardiovascular risk factors and chronic kidney disease in Japanese patients with type 2 diabetes mellitus: the Fukuoka Diabetes Registry. Nutr. J. 12, 159 (2013).
Alberti, K. et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120, 1640–1645 (2009).
Li, S. et al. Dietary fiber intake and mortality among survivors of myocardial infarction: prospective cohort study. Bmj 348 (2014).
Byrne, C., Chambers, E., Morrison, D. & Frost, G. The role of short chain fatty acids in appetite regulation and energy homeostasis. Int. J. Obes. 39, 1331–1338 (2015).
Benítez-Páez, A. et al. Impact of dietary fiber and fat on gut microbiota re-modeling and metabolic health. Trends Food Sci. Technol. 57, 201–212 (2016).
van Bennekum, A. M., Nguyen, D. V., Schulthess, G., Hauser, H. & Phillips, M. C. Mechanisms of cholesterol-lowering effects of dietary insoluble fibres: relationships with intestinal and hepatic cholesterol parameters. Br. J. Nutr. 94, 331–337 (2005).
Sánchez, D., Miguel, M. & Aleixandre, A. Dietary fiber, gut peptides, and adipocytokines. J. Med. Food 15, 223–230 (2012).
Weickert, M. O. & Pfeiffer, A. F. Metabolic effects of dietary fiber consumption and prevention of diabetes. J. Nutr. 138, 439–442 (2008).
Dandona, P., Aljada, A., Chaudhuri, A., Mohanty, P. & Garg, R. Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation 111, 1448–1454 (2005).
Thompson, F. E. & Subar, A. F. Dietary assessment methodology. In Nutrition in the Prevention and Treatment of Disease, 5–48 (2017).
Kweon, S. et al. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). Int. J. Epidemiol. 43, 69–77 (2014).
Lee, M.-R., Jung, S. M., Bang, H., Kim, H. S. & Kim, Y. B. Association between muscle strength and type 2 diabetes mellitus in adults in Korea: data from the Korea national health and nutrition examination survey (KNHANES) VI. Medicine 97, e10984 (2018).
Han, E. et al. Association between dietary acid load and the risk of cardiovascular disease: nationwide surveys (KNHANES 2008–2011). Cardiovasc. Diabetol. 15, 122 (2016).
Jung, C.-H. et al. Association of meal frequency with metabolic syndrome in Korean adults: from the Korea National Health and Nutrition Examination Survey (KNHANES). Diabetol. Metab. Syndr. 9, 77 (2017).
Shin, D., Joh, H.-K., Kim, K. H. & Park, S. M. Benefits of potassium intake on metabolic syndrome: the fourth Korean National Health and Nutrition Examination Survey (KNHANES IV). Atherosclerosis 230, 80–85 (2013).
Park, S., Ahn, J., Kim, N.-S. & Lee, B.-K. High carbohydrate diets are positively associated with the risk of metabolic syndrome irrespective to fatty acid composition in women: the KNHANES 2007–2014. Int. J. Food Sci. Nutr. 68, 479–487 (2017).
Park, M. K. et al. Adapting a standardised international 24 h dietary recall methodology (GloboDiet software) for research and dietary surveillance in Korea. Br. J. Nutr. 113, 1810–1818 (2015).
Lee, J. Y. & Kim, D. W. Validation of food intake frequency from food frequency questionnaire for use as a covariate in a model to estimate usual food intake. Culin. Sci. Hosp. Res. 23, 64–73 (2017).
Heng, D. et al. Modification of the NCEP ATP III definitions of the metabolic syndrome for use in Asians identifies individuals at risk of ischemic heart disease. Atherosclerosis 186, 367–373 (2006).
Ramachandran, A., Snehalatha, C., Satyavani, K., Sivasankari, S. & Vijay, V. Metabolic syndrome in urban Asian Indian adults—a population study using modified ATP III criteria. Diabetes Res. Clin. Pract. 60, 199–204 (2003).
Thomas, G. N. et al. The US national cholesterol education programme adult treatment panel III (NCEP ATP III) prevalence of the metabolic syndrome in a Chinese population. Diabetes Res. Clin. Pract. 67, 251–257 (2005).
Piercy, K. L. et al. The physical activity guidelines for Americans. JAMA 320, 2020–2028 (2018).
Acknowledgements
This research was supported by a grant of the Korean Health Promotion R&D Project, funded by the Ministry of Health and Welfare, Republic of Korea (Grant No.: HS20C0093). We would like to thank Nayeon Kim (Division of Cancer Control and Policy, National Cancer Control Institute, National Cancer Center, Goyang, the Republic of Korea) for administrative support.
Author information
Authors and Affiliations
Contributions
K.K. conducted literature review and analyzed the data. K.K. conceived and designed the study under the supervision of Y.C. Both K.K. and Y.C. prepared the paper and critically revised the manuscript for important intellectual content upon submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, K., Chang, Y. Association of dietary fiber intake with metabolic syndrome among adult cancer survivors: a population-based cross-sectional study. Sci Rep 11, 11794 (2021). https://doi.org/10.1038/s41598-021-91312-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91312-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.