Abstract
Obesity and associated dyslipidemia may contribute to increased cardiovascular disease. Obesity has also been associated with neuropathy. We have investigated presence of peripheral nerve damage in patients with severe obesity without type 2 diabetes and the status of metabolic syndrome and lipoprotein abnormalities. 47participants with severe obesity and 30 age-matched healthy controls underwent detailed phenotyping of neuropathy and an assessment of lipoproteins and HDL-functionality. Participants with severe obesity had a higher neuropathy symptom profile, lower sural and peroneal nerve amplitudes, abnormal thermal thresholds, heart rate variability with deep breathing and corneal nerve parameters compared to healthy controls. Circulating apolipoprotein A1 (P = 0.009), HDL cholesterol (HDL-C) (P < 0.0001), cholesterol efflux (P = 0.002) and paroxonase-1 (PON-1) activity (P < 0.0001) were lower, and serum amyloid A (SAA) (P < 0.0001) was higher in participants with obesity compared to controls. Obese participants with small nerve fibre damage had higher serum triglycerides (P = 0.02), lower PON-1 activity (P = 0.002) and higher prevalence of metabolic syndrome (58% vs. 23%, P = 0.02) compared to those without. However, HDL-C (P = 0.8), cholesterol efflux (P = 0.08), apoA1 (P = 0.8) and SAA (P = 0.8) did not differ significantly between obese participants with and without small nerve fibre damage. Small nerve fibre damage occurs in people with severe obesity. Patients with obesity have deranged lipoproteins and compromised HDL functionality compared to controls. Obese patients with evidence of small nerve fibre damage, compared to those without, had significantly higher serum triglycerides, lower PON-1 activity and a higher prevalence of metabolic syndrome.
Similar content being viewed by others
Introduction
Obesity is a worldwide epidemic conferring a major public health challenge, placing increased economic burden on health care systems, and is the fifth leading global cause of death from cardiovascular disease and cancer1.
Type 2 diabetes (T2DM) is the commonest cause of peripheral neuropathy (PN), but impaired glucose tolerance (IGT), hypertriglyceridemia and increased waist circumference are also associated with PN2,3,4,5. The Monica/Kora Augsburg study showed an increased prevalence of painful neuropathy in people with IGT, which was associated independently with weight and waist circumference5. The Cooperative Health Research in the Region of Augsburg (KORA) F4 study also showed that the prevalence of PN in elderly people with IGT and T2D was comparable6 and that abdominal obesity was associated with the development of diabetic polyneuropathy (DPN)7. The mechanisms that drive obesity-related neuropathy have received limited attention.
Small fibre neuropathy and cardiac autonomic neuropathy occur in obese individuals with and without T2DM8,9,10,11. Hypertriglyceridemia and obesity have been associated with reduced intraepidermal nerve fibres and elevated HbA1c has been related to reduced nerve conduction velocity12. We have previously shown small fibre pathology in people with IGT13, especially those who progress to diabetes14. Intraepidermal nerve fibre density increases after diet and exercise in people with IGT15, particularly those with the metabolic syndrome16 and small nerve fibres regenerate after bariatric surgery17.
Dyslipidaemia has previously been implicated in the pathogenesis of diabetic neuropathy18. Serum paraoxonase-1 (PON-1), an antioxidant and antiatherogenic component of HDL reduces the susceptibility of LDL to lipid peroxidation19 and is lower in people with diabetes and microvascular complications20. Short-term improvements in serum triglycerides improve diabetic neuropathy21. High-fat fed mice with peripheral nerve and dorsal root ganglion overexpression of 12/15-lipoxygenase develop small nerve fibre damage22. A loss of HDL’s antioxidant function and systemic and adipose tissue inflammation may also contribute to obesity-mediated neuropathy23,24.
We hypothesised that neuropathy and small nerve fibre damage in particular, is associated with abnormalities in circulating lipoproteins, HDL-functionality and metabolic syndrome in people with severe obesity.
Materials and methods
Participants with obesity were recruited from a regional tier 3 specialist weight management service at Salford Royal Hospital and were not previously diagnosed with T2D or prediabetes, confirmed by an HbA1c < 42 mmol/mol (6.0%). The control group were healthy volunteers recruited from Manchester University Foundation Trust, Salford Royal Hospital and the University of Manchester. Exclusion criteria were history of cancer, previous chemotherapy or radiotherapy, diabetes mellitus, prediabetes, anaemia, hereditary neuropathies, inborn errors of metabolism, untreated vitamin and mineral deficiencies, low vitamin B12 or folate levels, history of corneal trauma or surgery or a history of ocular or systemic disease that may affect the cornea. This study was approved by the Central Manchester Research and Ethics Committee. This research adhered to the tenant of declaration of Helsinki and was carried out in accordance with the relevant guidelines and regulations. All subjects provided written informed consent prior to the participation.
Demographics and assessment of neuropathy
All study participants underwent assessment of body mass index (BMI (kg/m2)) , blood pressure (Dinamap pro 100v2, GE Medical Systems, Freiburg, Germany) and neuropathy symptoms using the Neuropathy symptom profile (NSP). Neurological deficits were evaluated using the modified neuropathy disability score (NDS), which is comprised of an assessment of vibration perception, pin-prick, temperature sensation and presence or absence of ankle reflexes25. A Neurothesiometer (Horwell, Scientific Laboratory Supplies, Wilfrod, Nottingham, UK) was used for the assessment of vibration perception threshold (VPT) and TSA-II NeuroSensory Analyser (Medoc Ltd., Ramat-Yishai, Israel) for the assessment of cold (CPT) and warm (WPT) perception thresholds14.
Electro-diagnostic studies were undertaken using a Dantec “Keypoint” system (Dantec Dynamics Ltd, Bristol, UK) equipped with a DISA temperature regulator to keep limb temperature constantly between 32 and 35 °C. Sural sensory nerve amplitude, conduction velocity and latency and peroneal motor nerve amplitude, conduction velocity and latency were assessed by a consultant neurophysiologist using a Dantec “Keypoint” system (Dantec Dynamics Ltd, Bristol, UK)14.
Heart rate variability with deep breathing (HRV-DB) was assessed with an ANX 3.0 autonomic nervous system monitoring device (ANSAR Medical Technologies Inc., Philadelphia, PA, USA).
Patients underwent examination with a corneal confocal microscope (CCM; Heidelberg Retinal Tomograph III Rostock Cornea Module, Heidelberg Engineering GmbH, Heidelberg, Germany) as per our previously established protocol26. Six non-overlapping images/patient (3 per eye) were selected from the central cornea following an established protocol27. Manual corneal nerve quantification was undertaken using CCMetrics (University of Manchester, UK) in a masked fashion. Corneal nerve fiber density (CNFD)—the total number of major nerves/mm2 of corneal tissue, corneal nerve branch density (CNBD)—the number of branches emanating from the major nerve trunks/mm2 of corneal tissue and corneal nerve fiber length (CNFL)—the total length of all nerve fibers and branches (mm/mm2) within the area of corneal tissue were assessed. Subjects with obesity were divided into those with and without small fibre damage based on a CNFL < 2SD of the control mean.
Blood sampling
Blood samples were collected after a 10 h overnight fast, serum and EDTA-plasma were isolated by centrifugation at 2000 g for 15 min at 4° C within 2 h of collection and stored at -700C.
Lipid Profile
Total cholesterol was measured using the cholesterol oxidase phenol 4-aminoantipyrine peroxidase method, serum triglycerides by the glycerol phosphate oxidase phenol 4-aminoantipyrine peroxidase method, and apolipoprotein A1 (apoA1) was assayed using immunoturbidimetric assays. HDL-C was assayed using the direct clearance method. All these tests were performed on a Randox daytona analyzer (Randox Laboratories Ltd, Crumlin, County Antrim, UK). The laboratory participates in RIQAS (Randox International Quality Assessment Scheme; Randox Laboratories, Dublin, Ireland), which is CRC calibrated. LDL was estimated using the Friedewald formula.
Paraoxonase-1 (PON-1) activity
Serum PON-1 activity was determined by a semi-automated micro-titer plate method using paraoxon (O,O-Diethyl O-4-nitrophenyl phosphate28. Plates were read at 405 nm using a multiskan multisoft plate reader (Labsystems, Hampshire, UK). Intra-assay and inter-assay CVs were 3% and 3.5%, respectively.
Serum amyloid A (SAA)
SAA was measured using the human SAA solid-phase sandwich ELISA (ThermoFisher Scientific, Loughborough, UK). Intra-assay and inter-assay CVs were 6.1% and 7.4%, respectively.
Capacity of HDL to promote cholesterol efflux in vitro
Cholesterol efflux of HDL was determined in an assay that has been previously validated29. ApoB depleted serum was prepared after removal of apolipoprotein B (apoB) containing lipoproteins with polyethylene glycol (MW 8000; Sigma),diluted to 2.8%30 and J774A.1 cells were incubated with radiolabelled cholesterol and incubated with apoB-depleted serum for 4 h. After incubation, the cell media was collected, and cells were washed with PBS and dissolved in 0.5 ml 0.2 N NaOH to determine radioactivity. Cellular cholesterol efflux was expressed as the percentage of radioactivity in the medium from the radioactivity in the cells and medium. Cholesterol efflux was linear over 4 h and was calculated using the following formula:
To calculate cholesterol efflux at any time point, we subtracted efflux to serum free media (control) from that of apolipoprotein B depleted serum. Intra-assay and inter-assay coefficient of variance (CV) were 3.9% and 7.3%, respectively.
Statistical analysis
Analysis was carried out on SPSS for Mac (Version 19.0, IBM Corporation, New York, USA). All data are expressed as mean ± standard deviation (SD). The data were assessed for normality and appropriate statistical analyses conducted. To assess within and between group differences we used one-way analysis of variance (ANOVA) or a non-parametric counterpart (Kruskal–Wallis). A significant p value was considered to be < 0.05.
Results
Clinical variables
We studied 47 participants with severe obesity compared to 30 age-matched healthy controls (P = 0.5) (Table 1). The obese group had a significantly higher weight (P < 0.0001), waist circumference (P < 0.0001) and BMI (P < 0.0001), but no statistically significant difference in HbA1c, blood pressure or eGFR compared to controls (Table 1). Nineteen (40%) of the participants with obesity fulfilled the criteria for metabolic syndrome31.
Neuropathy assessment in obese compared to control subjects
Participants with obesity had a significantly higher NSP (P < 0.0001) and lower sural (P < 0.0001) and peroneal (P = 0.006) nerve amplitudes, but no difference in sural and peroneal nerve conduction velocity and latency compared to controls (Table 1). VPT (P < 0.0001) and WPT (P < 0.0001) were significantly higher, whilst CPT (P = 0.003) and HRV-DB (P < 0.0001) were significantly lower in participants with obesity compared to controls. CNFD (P < 0.0001), CNBD (P < 0.0001) and CNFL (P < 0.0001) were significantly lower in obese participants compared to controls.
Obese participants with and without small nerve fibre damage
Based on a CNFL cut-off greater than 2 standard deviations below the mean of healthy controls, 51% of participants with obesity had significant small nerve fibre damage. More participants with small nerve fibre damage (58%) had metabolic syndrome compared to those without small fibre damage (23%; P = 0.02). CNFD (P < 0.0001), CNBD (P < 0.0001) and CNFL (P < 0.0001) were significantly lower in obese patients with small nerve fibre damage compared to those without. Other measures of neuropathy did not differ significantly between obese subjects with and without small nerve fibre damage, except for a higher sural nerve conduction velocity (P = 0.03) (Table 2).
Lipoproteins and HDL functionality markers
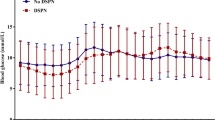
Eleven (23%) of the participants with severe obesity were treated with statins, but their lipid profile, apoA1, apoB and HDL functionality markers did not differ from participants not on statins. Total cholesterol was significantly lower (P = 0.002), but there was no significant difference in LDL-C or serum triglycerides in participants with severe obesity compared to controls. HDL-C (P < 0.0001), PON-1 (P < 0.0001), apoA1 (P = 0.009) and cholesterol efflux (P = 0.002) were lower, and SAA (P < 0.0001) was higher in obese participants compared to controls (Fig. 1). Serum triglycerides (P = 0.02) were higher and PON-1 activity (P = 0.005) was lower in obese patients with small nerve fibre damage; however, HDL-C (P = 0.8), cholesterol efflux (P = 0.08), apoA1 (P = 0.8) and SAA (P = 0.8) did not differ between obese participants with and without small nerve fibre damage (Table 3).
Discussion
We have shown significant small nerve fibre damage in participants with severe obesity which was associated with reduced PON-1 activity, higher serum triglycerides and metabolic syndrome. Experimental studies have shown that high-fat fed mice develop neuropathy22. We and others have previously demonstrated significant small fibre damage in people with metabolic syndrome and IGT3,5,12. A study has shown that 11% of women with severe obesity have peripheral neuropathy32 and we have recently reported small nerve fibre regeneration after bariatric surgery33 .
The exact mechanisms underlying small nerve fibre damage in obesity are not understood; but appear to be different to the hyperglycemia-mediated large fibre neuropathy in patients with diabetes34. Patients with severe obesity have small fibre dysfunction8 and a reduction in tibial and peroneal nerve amplitudes9, which correlates with BMI35. Participants with moderate obesity showed reduced sensory nerve amplitudes and normal nerve conduction velocity which was attributed to impaired percutaneous stimulation due to thicker subcutaneous tissue36. In the present study we show that individuals with obesity without diabetes have evidence of small nerve fibre damage, evidenced by corneal nerve loss. These observations are consistent with the Utah Diabetic Neuropathy Study which reported that obesity and hypertriglyceridemia were related to a loss of intraepidermal nerve fibres12. In the present study we also identify cardiac autonomic dysfunction in individuals with obesity. Central obesity has been associated with cardiac autonomic neuropathy in participants with impaired glucose tolerance37, and Valensi et al. have previously shown that deep breathing heart rate variability correlates with BMI in type 2 diabetes10. Furthermore, in a series of 121 participants with obesity, 50% had at least one abnormal cardiac autonomic function test38. In individuals with obesity, waist-to-hip ratio was associated with reduced parasympathetic and increased sympathetic activation39 and obesity predicts the development of autonomic neuropathy in type 2 diabetes40.
The EURODIAB study reported a significant association between total cholesterol and serum triglyceride levels with incident diabetic peripheral and cardiac autonomic neuropathy in patients with type 1 diabetes18. Wiggin et al.4 showed that elevated serum triglycerides predicted a loss of myelinated nerve fibres in sural nerve biopsies from people with diabetes41; and the DISTANCE study showed that serum triglycerides were an independent risk factor for non-traumatic lower extremity amputation42. Indeed, in the present study we report a significantly higher level of serum triglycerides and prevalence of metabolic syndrome in people with obesity and small nerve fibre damage.
HDL is the most abundant lipoprotein in human tissue and provides protection to cell membranes from oxidative stress43. Intracellular and membrane cholesterol distribution are important for neuronal integrity, but excess cholesterol is detrimental and can promote amyloid precursor protein cleavage and the generation of toxic amyloid peptides44. Maintaining a physiologic cholesterol balance is vital for neuronal function and synaptic transmission45. Cholesterol efflux and the capacity of HDL to accept cholesterol is partly regulated by ATP-binding cassette subfamily A1 (ABCA1) and ATP-binding cassette subfamily G1 (ABCG1) proteins46. Tangier disease is a rare inherited metabolic neuropathy due to a mutation in the ABCA1 gene which results in a marked reduction in circulating HDL particles and serum HDL-C level and accumulation of cholesterol esters in peripheral nerves47. HDL is not only involved in reverse cholesterol transport, but also impedes lipid peroxidation and has anti-inflammatory properties43. ApoA1, the main protein component in HDL, is known to have an anti-inflammatory effect and inhibit dendritic cell differentiation48. We demonstrate significantly reduced PON-1 activity in people with obesity and small nerve fibre damage. PON-1 is an HDL associated enzyme with anti-oxidant/glycation properties, and certain PON-1 genotypes increase the risk of developing microalbuminuria and retinopathy49. PON-1 activity also correlates with the capacity of HDL to protect LDL against oxidation in vitro19, hence decreased PON-1 activity may lead to neuropathy through a mechanism involving increased lipid peroxidation. Low PON-1 activity has been implicated in the development of retinopathy50 and macrovascular disease51 in patients with diabetes; and Abbott et al.52 demonstrated lower PON-1 activity in patients with diabetic neuropathy. Fenofibrate increases PON-1 activity53, which may account for its benefit in reducing amputations54.
SAA is an acute phase protein, which correlates with BMI and decreases with weight loss55. There is increasing evidence for its role in adipose tissue inflammation, insulin resistance, diabetes and cardiovascular disease56. During an acute phase reaction, SAA displaces apoA1, compromising HDL’s capacity to protect against oxidation and promote cholesterol efflux56. Recent studies have shown that the association between obesity and incident diabetic neuropathy may be partially mediated by inflammation7. We show that patients with obesity have a significantly higher SAA and lower capacity of HDL to promote cholesterol efflux; however, this did not differ between subjects with and without small nerve fibre damage. We also report abnormalities in multiple markers of HDL functionality in people with obesity perse which have been reported in patients with cardiovascular disease57 and patients with rheumatoid arthritis58, suggesting a common pathway for inflammation and enhanced vascular disease risk in these patients.
In conclusion we show there is evidence of small nerve fibre damage in people with severe obesity. Patients with obesity had elevated serum triglycerides and SAA and lower HDL-C, PON-1 activity and cholesterol efflux. Furthermore, obese subjects with small nerve fibre damage, compared to those without, had higher serum triglycerides and prevalence of metabolic syndrome and lower PON1 activity. These factors may represent therapeutic targets to prevent or reverse small nerve fibre damage in obesity.
Data availability
The data is available from the corresponding author with reasonable request.
Abbreviations
- apoA1:
-
Apolipoprotein AI
- apoB:
-
Apolipoprotein B
- ABCA1 and ABCG1:
-
ATP-binding cassette subfamily A
- CV:
-
Coefficient of variation
- CPT:
-
Cold perception threshold
- CNBD:
-
Corneal nerve branch density
- CNFD:
-
Corneal nerve fiber density
- CNFL:
-
Corneal nerve fiber length
- HRV-DB:
-
Heart rate variability with deep breathing
- IGT:
-
Impaired glucose tolerance
- IL:
-
Interleukin
- IENFD:
-
Intra-epidermal nerve fibre density
- LOX1:
-
Lectin-like oxLDL receptor-1
- NDS:
-
Neuropathy disability score
- MPO:
-
Myeloperoxidase
- NSP:
-
Neuropathy symptom profile
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- oxLDL:
-
Oxidised LDL
- PON-1:
-
Paraoxonase-1
- PN:
-
Peripheral neuropathy
- SFN:
-
Small fibre neuropathy
- SAA:
-
Serum Amyloid A
- VPT:
-
Vibration perception threshold
- WPT:
-
Warm perception threshold
References
Bhakta, S. K. & Sarker, A. Effect of serum lipoprotein (a) [Lp(a)] in menopausal women. Mymensingh Med. J. MMJ. 25(2), 255–260 (2016).
Straub, R. H., Thum, M., Hollerbach, C., Palitzsch, K.-D. & Schölmerich, J. Impact of obesity on neuropathic late complications in NIDDM. Diabetes Care 17(11), 1290–1294 (1994).
Asghar, O. et al. Corneal confocal microscopy detects neuropathy in subjects with impaired glucose tolerance. Diabetes Care 37(9), 2643–2646 (2014).
Wiggin, T. D. et al. Elevated triglycerides correlate with progression of diabetic neuropathy. Diabetes 58(7), 1634–1640 (2009).
Ziegler, D., Rathmann, W., Dickhaus, T., Meisinger, C. & Mielck, A. Prevalence of Polyneuropathy in pre-diabetes and diabetes is associated with abdominal obesity and macroangiopathy the MONICA/KORA augsburg surveys S2 and S3. Diabetes Care 31(3), 464–469 (2008).
Bongaerts, B. W. et al. Older subjects with diabetes and prediabetes are frequently unaware of having distal sensorimotor polyneuropathy: the KORA F4 study. Diabetes Care 36(5), 1141–1146 (2013).
Schlesinger S, Herder C. General and abdominal obesity and incident distal sensorimotor polyneuropathy: insights into inflammatory biomarkers as potential mediators in the KORA F4/FF4 Cohort. 2019;42(2):240–7.
Herman, R. M. et al. Prevalence of somatic small fiber neuropathy in obesity. Int J Obes (Lond). 31(2), 226–235 (2007).
Miscio, G. et al. Obesity and peripheral neuropathy risk: a dangerous liaison. J Peripher Nerv Syst. 10(4), 354–358 (2005).
Valensi P, Paries J, Attali JR, French Group for R, Study of Diabetic N. Cardiac autonomic neuropathy in diabetic patients: influence of diabetes duration, obesity, and microangiopathic complications--the French multicenter study. Metabolism. 2003;52(7):815–20.
Pop-Busui, R. et al. Effects of cardiac autonomic dysfunction on mortality risk in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care 33(7), 1578–1584 (2010).
Smith, A. G. & Singleton, J. R. Obesity and hyperlipidemia are risk factors for early diabetic neuropathy. J Diabetes Complicat. 27(5), 436–442 (2013).
Asghar, O. et al. Individuals with impaired glucose tolerance demonstrate normal cardiac sympathetic innervation using I-123 mIBG scintigraphy. J. Nuclear Cardiol. Official Publ. Am. Soc. Nuclear Cardiol. 22(6), 1262–1268 (2015).
Azmi, S. et al. Corneal confocal microscopy identifies small-fiber neuropathy in subjects with impaired glucose tolerance who develop type 2 diabetes. Diabetes Care 38(8), 1502–1508 (2015).
Smith, A. G. et al. Lifestyle intervention for pre-diabetic neuropathy. Diabetes Care 29(6), 1294–1299 (2006).
Singleton, J. R., Marcus, R. L., Lessard, M. K., Jackson, J. E. & Smith, A. G. Supervised exercise improves cutaneous reinnervation capacity in metabolic syndrome patients. Ann. Neurol. 77(1), 146–153 (2015).
Iqbal, Z. et al. Metabolic and cardiovascular outcomes of bariatric surgery. Curr Opin Lipidol. 31(4), 246–256 (2020).
Tesfaye, S. et al. Vascular risk factors and diabetic neuropathy. N Engl. J. Med. 352(4), 341–350 (2005).
Davidson, W. S. et al. Proteomic analysis of defined HDL subpopulations reveals particle-specific protein clusters: relevance to antioxidative function. Arterioscler. Thromb. Vasc. Biol. 29(6), 870–876 (2009).
Kota, S. K. et al. Implications of serum paraoxonase activity in obesity, diabetes mellitus, and dyslipidemia. Indian J. Endocrinol. Metabolism. 17(3), 402–412 (2013).
Perkins, B. A., Dholasania, A., Buchanan, R. A. & Bril, V. Short-term metabolic change is associated with improvement in measures of diabetic neuropathy: a 1-year placebo cohort analysis. Diabet. Med. 27(11), 1271–1279 (2010).
Obrosova, I. G. et al. High-fat diet induced neuropathy of pre-diabetes and obesity: effects of “healthy” diet and aldose reductase inhibition. Diabetes 56(10), 2598–2608 (2007).
Yadav, R. et al. Impairment of high-density lipoprotein resistance to lipid peroxidation and adipose tissue inflammation in obesity complicated by obstructive sleep apnea. J Clin Endocrinol Metab. 99(9), 3390–3398 (2014).
Aghamohammadzadeh, R. et al. Effects of bariatric surgery on human small artery function: evidence for reduction in perivascular adipocyte inflammation, and the restoration of normal anticontractile activity despite persistent obesity. J. Am. Coll Cardiol. 62(2), 128–135 (2013).
Young, M., Boulton, A., MacLeod, A., Williams, D. & Sonksen, P. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia 36(2), 150–154 (1993).
Tavakoli M, Malik RA. Corneal confocal microscopy: a novel non-invasive technique to quantify small fibre pathology in peripheral neuropathies. J Vis Exp. 2011(47).
Kalteniece, A. et al. Corneal confocal microscopy is a rapid reproducible ophthalmic technique for quantifying corneal nerve abnormalities. PLoS ONE 12(8), 0183040 (2017).
Charlton-Menys, V., Liu, Y. & Durrington, P. N. Semiautomated method for determination of serum paraoxonase activity using paraoxon as substrate. Clin Chem. 52(3), 453–457 (2006).
de la Llera-Moya, M. et al. The ability to promote efflux via ABCA1 determines the capacity of serum specimens with similar high-density lipoprotein cholesterol to remove cholesterol from macrophages. Arterioscler. Thromb. Vasc. Biol. 30(4), 796–801 (2010).
Asztalos, B. F. et al. Differential effects of HDL subpopulations on cellular ABCA1- and SR-BI-mediated cholesterol efflux. J. Lipid Res. 46(10), 2246–2253 (2005).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16), 1640–1645 (2009).
Dias LS, Nienov OH, Machado FD, Ramos CP, Rodrigues D, Menguer RK, et al. Polyneuropathy in Severely Obese Women Without Diabetes: Prevalence and Associated Factors. Diabetes Care. 2018.
Adam, S. et al. Improvements in diabetic neuropathy and nephropathy after bariatric surgery: a prospective cohort study. Obes. Surg. 31(2), 554–563 (2021).
Breiner, A., Lovblom, L. E., Perkins, B. A. & Bril, V. Does the prevailing hypothesis that small-fiber dysfunction precedes large-fiber dysfunction apply to type 1 diabetic patients?. Diabetes Care 37(5), 1418–1424 (2014).
Buschbacher, R. M. Body mass index effect on common nerve conduction study measurements. Muscle Nerve. 21(11), 1398–1404 (1998).
Yadav, R. L. et al. Somatic neural alterations in non-diabetic obesity: a cross-sectional study. BMC Obes. 3, 50 (2016).
Laitinen, T. et al. Cardiovascular autonomic dysfunction is associated with central obesity in persons with impaired glucose tolerance. Diabet Med. 28(6), 699–704 (2011).
Valensi, P., Thi, B. N., Lormeau, B., Paries, J. & Attali, J. R. Cardiac autonomic function in obese patients. Int. J. Obes. Relat. Metab. Disord. 19(2), 113–118 (1995).
Yadav, R. L. et al. Association between obesity and heart rate variability indices: an intuition toward cardiac autonomic alteration - a risk of CVD. Diabetes Metab. Syndr Obes. 10, 57–64 (2017).
Andersen, S. T. Risk factors for the presence and progression of cardiovascular autonomic neuropathy in type 2 diabetes: ADDITION-denmark. Obes. Surg. 41(12), 2586–2594 (2018).
Vincent, A. M., Hinder, L. M., Pop-Busui, R. & Feldman, E. L. Hyperlipidemia: a new therapeutic target for diabetic neuropathy. J. Peripher. Nerv. Syst. 14(4), 257–267 (2009).
Callaghan, B. C. et al. Triglycerides and amputation risk in patients with diabetes: ten-year follow-up in the DISTANCE study. Diabetes Care 34(3), 635–640 (2011).
Soran, H., Hama, S., Yadav, R. & Durrington, P. N. HDL functionality. Curr Opin Lipidol. 23(4), 353–366 (2012).
Runz, H. et al. Inhibition of intracellular cholesterol transport alters presenilin localization and amyloid precursor protein processing in neuronal cells. J. Neurosci. 22(5), 1679–1689 (2002).
Mauch, D. H. et al. CNS synaptogenesis promoted by glia-derived cholesterol. Science 294(5545), 1354–1357 (2001).
Jessup, W., Gelissen, I. C., Gaus, K. & Kritharides, L. Roles of ATP binding cassette transporters A1 and G1, scavenger receptor BI and membrane lipid domains in cholesterol export from macrophages. Curr. Opin. Lipidol. 17(3), 247–257 (2006).
Brunham, L. R. et al. Clinical, biochemical, and molecular characterization of novel mutations in ABCA1 in families with tangier disease. JIMD Rep. 18, 51–62 (2015).
Kim, K. D. et al. Apolipoprotein A-I induces IL-10 and PGE2 production in human monocytes and inhibits dendritic cell differentiation and maturation. Biochem. Biophys. Res. Commun. 338(2), 1126–1136 (2005).
Ikeda, Y. et al. Serum paraoxonase activity and its relationship to diabetic complications in patients with non—insulin-dependent diabetes mellitus. Metabolism 47(5), 598–602 (1998).
Mackness, B., Durrington, P. N., Abuashia, B., Boulton, A. J. & Mackness, M. I. Low paraoxonase activity in type II diabetes mellitus complicated by retinopathy. Clin. Sci (Lond). 98(3), 355–363 (2000).
Mackness, B., Durrington, P. N., Boulton, A. J., Hine, D. & Mackness, M. I. Serum paraoxonase activity in patients with type 1 diabetes compared to healthy controls. Eur. J. Clin. Invest. 32(4), 259–264 (2002).
Abbott, C. A., Mackness, M. I., Kumar, S., Boulton, A. J. & Durrington, P. N. Serum paraoxonase activity, concentration, and phenotype distribution in diabetes mellitus and its relationship to serum lipids and lipoproteins. Arterioscler. Thromb. Vasc. Biol. 15(11), 1812–1818 (1995).
Phuntuwate, W. et al. Effect of fenofibrate therapy on paraoxonase1 status in patients with low HDL-C levels. Atherosclerosis 196(1), 122–128 (2008).
Rajamani, K. et al. Effect of fenofibrate on amputation events in people with type 2 diabetes mellitus (FIELD study): a prespecified analysis of a randomised controlled trial. Lancet 373(9677), 1780–1788 (2009).
Zhao, Y. et al. Association between serum amyloid a and obesity: a meta-analysis and systematic review. Inflamm. Res. 59(5), 323–334 (2010).
King, V. L., Thompson, J. & Tannock, L. R. Serum amyloid a in atherosclerosis. Curr Opin Lipidol. 22(4), 302–307 (2011).
Khera, A. V. et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl. J. Med. 364(2), 127–135 (2011).
Kim, J. Y. et al. Patients with rheumatoid arthritis show altered lipoprotein profiles with dysfunctional high-density lipoproteins that can exacerbate inflammatory and atherogenic process. PLoS ONE 11(10), e0164564 (2016).
Acknowledgements
We acknowledge support from the Manchester Comprehensive Local Research Network and the National Institute for Health Research/Wellcome Trust Clinical Research Facility in Manchester, lipid disease fund and an unrestricted research donation from AMGEN.
Author information
Authors and Affiliations
Contributions
All authors were involved in revising the manuscript critically for important intellectual content and for final approval of the version to be published. S. Azmi was involved in acquisition of data, analysis and interpretation of data and wrote the manuscript. H.S., S. Adam, A.S. and J.H.H. recruited patients and controls. M.F., Y.L., T.S., S. Azmi, G.P., A.M., I.N.P., J.H.H., A.S., B.A. and H.S. contributed to acquisition and analysis of the data. Y.L., T.S., J.H.H. and S. Adam performed biochemical analysis. P.N.D. was involved in interpretation of the data. R.A.M. contributed to conception and design of the study, wrote and revised the manuscript. H.S. designed the study and contributed to interpretation of the data, wrote and revised the manuscript, and is principal investigator of the study. H.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Azmi, S., Ferdousi, M., Liu, Y. et al. The role of abnormalities of lipoproteins and HDL functionality in small fibre dysfunction in people with severe obesity. Sci Rep 11, 12573 (2021). https://doi.org/10.1038/s41598-021-90346-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-90346-9
This article is cited by
-
92A Systematic Review of Proteomics in Obesity: Unpacking the Molecular Puzzle
Current Obesity Reports (2024)
-
In vivo corneal confocal microscopy as a non-invasive test to assess obesity induced small fibre nerve damage and inflammation
Eye (2023)
-
The Peripheral Neuropathy Prevalence and Characteristics Are Comparable in People with Obesity and Long-Duration Type 1 Diabetes
Advances in Therapy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.