Abstract
To investigate whether the optimal time to tracheal intubation (TTI) during cardiopulmonary resuscitation would differ by different blood gas phenotypes. Adult patients experiencing in-hospital cardiac arrest (IHCA) from 2006 to 2015 were retrospectively screened. Early intra-arrest blood gas analysis, performed within 10 min of resuscitation, was used to define different phenotypes. In total, 567 patients were included. Non-severe acidosis (pH≧7.15) was associated with favourable neurological outcome (odds ratio [OR]: 4.60, 95% confidence interval [CI] 1.63–12.95; p value = 0.004) and survival (OR: 3.25, 95% CI 1.72–6.15; p value < 0.001) in the multivariable logistic regression analyses. In the interaction analysis, normal blood gas phenotype (pH: 7.35–7.45, PCO2: 35–45 mm Hg, HCO3− level: 22–26 mmol/L) × TTI ≦ 6.3 min (OR: 20.40, 95% CI 2.53–164.75; p value = 0.005) and non-severe acidosis × TTI ≦ 6.3 min (OR: 3.35, 95% CI 1.00–11.23; p value = 0.05) were associated with neurological recovery while metabolic acidosis × TTI ≦ 5.7 min (OR: 3.63, 95% CI 1.36–9.67; p value = 0.01) and hypercapnic acidosis × TTI ≦ 10.4 min (OR: 2.27, 95% CI 1.20–4.28; p value = 0.01) were associated with survival. Intra-arrest blood gas analysis may help guide TTI during for patients with IHCA.
Similar content being viewed by others
Introduction
Approximately 209,000 patients experience in-hospital cardiac arrest (IHCA) in the United States annually1. Twenty-four percent of patients with IHCA survive to hospital discharge; among these patients, 14% sustain significant neurological disability1.
When treating cardiac arrest, point-of-care blood testing may yield important diagnostic information and guide therapeutic management during cardiopulmonary resuscitation (CPR). For example, the diagnosis of hyperkalaemia could enable the clinicians to rapidly administer potassium-reducing agents to reverse this life-threatening electrolyte abnormality during CPR2. However, clinical data on point-of-care blood gas analysis during CPR are limited.
For epidemiological and research purposes, aetiologies of out-of-hospital cardiac arrest are usually categorised into medical and non-medical causes based solely on contextual data without the incorporation of diagnostic testing3. Thus, substantial heterogeneity exists between patients even if they are classified within the same category. In scenarios such as prehospital CPR, this crude classification system may be necessary; nonetheless, for IHCA resuscitation, a more elaborate categorization may facilitate the application of appropriate therapeutics. For example, studies4,5 indicated that tracheal intubation during CPR may cause harm for patients without respiratory failure prior to IHCA but may not do so for patients with prior respiratory failure.
In this study, we first attempted to investigate whether intra-arrest blood gas analysis could help classify IHCA patients into distinct phenotypes with different prognoses; second, we attempted to investigate whether the optimal timing of tracheal intubation would differ according to different phenotypes. Besides traditionally defined blood gas phenotypes, we would also attempt to identify new phenotypes which may influence the optimal timing of tracheal intubation.
Materials and methods
Setting
We used previously established IHCA database for analysis6,7. Briefly, the patient data were collected retrospectively at the National Taiwan University Hospital (NTUH). As a tertiary medical centre, NTUH has 2600 beds, including 220 beds in intensive care units (ICUs). This study was performed in accordance with the Declaration of Helsinki amendments. The NTUH Research Ethics Committee approved this study (reference number: 201805098RINC) and waived the requirement for informed consent because of the retrospective and non-interventional nature. In NTUH, a code team is activated whenever an IHCA event occurs in the general wards. A code team consists of a senior resident, several junior residents, a respiratory therapist, a head nurse and several ICU nurses. For IHCA occurring in the ICUs, CPR is performed by the ICU staff without activating a code team. Resuscitation was performed according to recommendations of CPR guidelines8,9. In NTUH, point-of-care blood gas analysers were deployed in every ward floor, including floor of general wards and ICUs. Physicians were instructed to obtain blood samples as soon as possible for blood gas analysis in order to identify potential causes leading to IHCA. There were no supra-glottic airways available for IHCA resuscitation in NTUH.
Participants
Patients experiencing IHCA at NTUH between 2006 and 2015 were screened. Patients fulfilling the following criteria were included for analysis: (1) age above 18 years, (2) chest compressions performed for ≥ 2 min, (3) absence of a do-not-resuscitate order before CPR, (4) early intra-arrest blood gas analysis with available blood pH, partial pressure of carbon dioxide (PCO2), and bicarbonate (HCO3-) level data and (5) tracheal intubation during CPR. Tracheal intubation included endotracheal intubation, tracheostomy and cricothyroidotomy. If a single patient experienced IHCA events more than once during the hospitalisation, only the first event was analysed. Trauma-related arrest was excluded. The number of patients fulfilling the above criteria during the study period determined the sample size.
Data collection and outcome measures
The following information was extracted for each patient: age, sex, comorbidities, variables recommended by the Utstein template10, early intra-arrest blood gas analysis data and interventions performed at the time of IHCA and after sustained return of spontaneous circulation (ROSC). Sustained ROSC was defined as ROSC lasting consecutively for at least 20 min. Time to intubation was defined as the time interval between the initiation of chest compression to the completion of tracheal intubation. Duration of CPR was recorded as the time interval between the initiation of chest compression until termination of CPR, either due to sustained ROSC or due to declaration of death.
Early intra-arrest blood gas analysis was defined as the first available blood gas data measured within 10 min of initiating CPR, which was usually obtained in the beginning of CPR. The sample for blood gas analysis could be obtained from arterial or venous sources, which could not be verified retrospectively. Blood pH, PCO2 and HCO3- were measured using point-of-care blood gas analysers. Patients were classified into 5 traditionally defined blood gas phenotypes based on a combination of pH, PCO2 and HCO3− levels11,12: (1) normal (pH: 7.35–7.45, PCO2: 35–45 mm Hg, HCO3- level: 22–26 mmol/L), (2) non-acidosis, except normal (pH≧7.35, but not belonging to normal), (3) hypercapnic acidosis (pH < 7.35, PCO2 > 45 mm Hg, HCO3− level > 22 mmol/L), (4) metabolic acidosis (pH < 7.35, PCO2 ≦ 45 mm Hg, HCO3− level ≦ 22 mmol/L), (5) mixed acidosis (pH < 7.35, but not belonging to hypercapnic or metabolic acidosis).
Favourable neurological status at hospital discharge was selected as the primary outcome, which was defined as one or two points on the Cerebral Performance Category scale13. Survival at hospital discharge was selected as the secondary outcome.
Statistical analysis
We used R 3.3.1 software (R Foundation for Statistical Computing, Vienna, Austria) to analyse data. Categorical variables are presented as counts with proportions, and continuous variables are presented as medians with interquartile ranges. Categorical variables were examined by Chi-squared test while continuous variables were compared by Wilcoxon’s rank-sum test. A two-tailed p value < 0.05 was considered significant.
We calculated the odds ratio (OR) as the outcome measure. We conducted univariate and multivariable logistic regression analyses to investigate the associations between variables of interest and outcomes. We placed all available independent variables in the regression model for selection, irrespective of whether they were considered as significant in univariate analyses. We employed generalised additive models (GAMs)14 to explore non-linear effects of all continuous variables on outcomes and to identify the optimal cut-off points to transform these continuous variables into binary ones, which would also be tested in the regression analyses. Furthermore, the cut-off points identified for pH, PCO2 and HCO3- would be used to define new phenotypes. Because the blood gas analysis data, including pH, PCO2 and HCO3-, were used to define different phenotypes, they were not included as independent variables during the model-fitting process. We developed the final regression model by stepwise variable selection procedure with iterations between the forward and backward steps. We defined the significance levels for entry and to stay at 0.15 to avoid exclusion of potential variables. We determined the final regression model by excluding non-significant variables sequentially until all regression coefficients were significant.
In the primary or secondary model, the multivariable analysis was intended to identify the phenotypes associated with primary or secondary outcome, respectively. In the interaction analysis, the interaction between each phenotype and time to intubation was assessed during the model-fitting process. We assessed the goodness-of-fit of the regression models by c statistics, the adjusted generalised R2 and the Hosmer–Lemeshow goodness-of-fit test.
We performed a sensitivity analysis to assess the influence of patients with missing blood gas analysis data. We performed the multiple imputation procedure to impute the missing data. The packages of Amelia and Zelig were employed. We used predictors altogether to impute the missing values. Ten datasets were imputed, and each dataset was used individually to fit the final regression model obtained in the primary analysis. The ten fitted results were then pooled into a single coefficient in the regression model.
Results
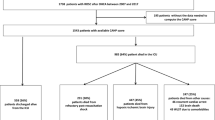
As shown in Supplemental Figure 1, there were 1698 adult non-trauma patients of IHCA who received CPR for ≥ 2 min at NTUH between 2006 and 2015. Of these, 599 patients were excluded because of the lack of early intra-arrest blood gas analysis, including 573 patients not having blood gas analysis and 26 patients having missing blood gas analysis data. In the remaining 1099 patients, 311 patients received intubation before IHCA and 221 patients did not receive intubation during CPR; therefore, a total of 567 patients were included in the analysis. The comparisons between patients with and without blood gas analysis data and among patients stratified by the timing of tracheal intubation were demonstrated in Supplemental Tables 1–4.
The features of included patients are presented in Tables 1 and 2. Median patient age was 69.9 years. Median CPR duration was 31.0 min and median time to intubation was 7.0 min. Median pH, PCO2, and HCO3− levels were 7.2, 54.3 mmHg and 19.6 mmol/L, respectively. Hypercapnic acidosis was the most dominant traditional blood gas phenotypes (214 patients, 37.7%). Only 66 patients (11.6%) survived to hospital discharge; of these, 30 patients (5.3%) demonstrated favourable neurological status.
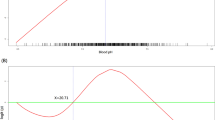
The GAM plots illustrated the association of logit (p), where p represented the probability for the primary outcome, with pH, PCO2, and HCO3− levels, respectively (Fig. 1). If logit (p) was greater than zero, the odds for achieving favourable neurological outcome would be greater than one. Therefore, pH of 7.15, PCO2 of 60 mmHg and HCO3- level of 16 mmol/L were selected as cut-off points to define new blood gas phenotypes, as follows: (1) non-severe acidosis (pH ≧ 7.15), (2) severe hypercapnic acidosis (pH < 7.15, PCO2 > 60 mm Hg, HCO3− level > 16 mmol/L), (3) severe metabolic acidosis (pH < 7.15, PCO2 ≦ 60 mm Hg, HCO3− level ≦ 16 mmol/L), (4) severe mixed acidosis (pH < 7.15, but not belonging to severe hypercapnic or metabolic acidosis). Both the new and traditional blood gas phenotypes were placed in the variable list for variable selection during the process of building primary and secondary models. Similarly, time to intubation was transformed into a binary variable based on GAM plots (Supplemental Figs. 2–5) and tested in the analysis.
Generalised additive model plots for nonparametric modelling of the respective effect of (A) blood pH, (B) PCO2, and (C) HCO3− on the logit of probability for favourable neurological outcome at hospital discharge. R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/.
For the primary outcome (Table 3), in the primary model, non-severe acidosis was positively associated with favourable neurological outcome (OR: 4.60, 95% confidence interval [CI] 1.63–12.95; p value = 0.004). The baseline characteristics and IHCA features stratified by severe acidosis are presented in Supplemental Tables 5–6. In the interaction analysis, both normal blood gas phenotype × time to intubation ≦ 6.3 min (OR: 20.40, 95% CI 2.53–164.75; p value = 0.005) and non-severe acidosis × time to intubation ≦ 6.3 min (OR: 3.35, 95% CI 1.00–11.23; p value = 0.05) were positively associated with favourable neurological outcome.
For the secondary outcome (Table 4), in the secondary model, non-severe acidosis was positively associated with survival (OR: 3.25, 95% CI 1.72–6.15; p value < 0.001). In the interaction analysis, both metabolic acidosis × time to intubation ≦ 5.7 min (OR: 3.63, 95% CI 1.36–9.67; p value = 0.01) and hypercapnic acidosis × time to intubation ≦ 10.4 min (OR: 2.27, 95% CI 1.20–4.28; p value = 0.01) were positively associated with survival.
In the sensitivity analysis, we imputed the data for the 26 patients who had missing blood gas analysis data and were excluded from the primary analysis. As shown in Supplemental Table 7, when imputed data were used to fit the primary model with interaction terms, the effect estimates of the included variables were similar to those of the original model (Table 3).
Discussion
Main findings
The results suggest that intra-arrest blood gas analysis might be used to classify IHCA patients into distinct phenotypes with different prognoses and responses to intervention. Non-severe acidosis, one of the phenotypes, was found to be positively associated with better neurological and survival outcomes. In the interaction analysis, for patients with non-severe acidosis, shorter time to intubation was associated with favourable neurological outcome, while for patients with metabolic or hypercapnic acidosis, shorter time to intubation was associated with improved survival. The results of interaction analysis suggested that the effects of time to intubation may differ between different phenotypes. Phenotyping by blood gas analysis may enable patient-tailored intervention during CPR.
Phenotyping by blood gas analysis and tracheal intubation
The most common feature used to phenotype patients during CPR may be the initial arrest rhythm, i.e. shockable versus non-shockable rhythm8,9, which significantly influences outcomes and necessitates prompt defibrillation for the former. However, beyond this, there are few reported features able to phenotype patients and essentially, all patients receive universal or one-size-fits-all managements8,9. The inability to phenotype patients may weaken the benefits of a certain intervention in some subgroups, or even cause harm, which might explain the abundant neutral results from clinical trials on cardiac arrest15. Point-of-care blood gas analysis had the potential to phenotype patients during CPR and guide corresponding treatment. Our results demonstrated a significant benefit of shorter time to intubation for patients with non-severe acidosis and normal blood gas phenotype regarding favourable neurological recovery. The normal blood gas phenotype was actually a subgroup of non-severe acidosis. Because the effects of shorter time to intubation were substantially greater for normal blood gas phenotype than non-severe acidosis (OR: 20.40 versus 3.35), the variables of shorter time to intubation with respective phenotypes were present in the primary model with interaction terms simultaneously. Earlier intubation during CPR may facilitate better control of ventilation and oxygenation16, resulting in better outcomes.
In our study, the benefits of shorter time to intubation were only observed in patients of non-severe acidosis, suggesting that the tracheal intubation may only be effective for patients with higher “resuscitability,” i.e. patients with higher chances of achieving favourable neurological or survival outcomes. Spindelboeck et al17 once reported that as high as 98% of OHCA patients had intra-arrest pH < 7.35. The mix of patients with high or low “resuscitability” may have thus nullified the potential benefits of intubation on long-term neurological and survival outcomes in previous studies18. In contrast to OHCA resuscitated in the out-of-hospital environment, IHCA patients usually could be attended earlier with more healthcare personnel involved. Therefore, it may be more likely for in-hospital code teams to conduct point-of-care blood gas analysis in determining whether early tracheal intubation should be performed during CPR for IHCA patients.
Most studies4,5,19 used large registry data to investigate the effect of tracheal intubation. Despite the increased statistical power with the larger study population4,5,19, the patients could only be classified under broad medical categories, such as shockable or non-shockable rhythm. In contrast, the phenotypes classified by blood gas analysis might be more reflective of the real-time pathophysiological states and be more appropriate to guide the corresponding treatment. The confounding effects of the different blood gas phenotypes, such as non-severe acidosis, could not accounted for in these studies4,5,19, which might lead to the heterogeneous results.
Clinical applications
Because our study was based on a highly selected cohort (approximately 33% [567/1698] of screened patients underwent blood gas analysis and intubation), the results should be further examined before clinical use. For example, the blood pH value used to define severe acidosis may need more patients to be validated. However, in the secondary model, we did find that for patients with traditionally defined hypercapnic or metabolic acidosis, shorter time to intubation was associated with better survival, which may be more clinically relevant. In most previous studies, point-of-care intra-arrest blood gas analysis data, such as pH20,21,22, PCO223, base excess24, and lactate25 levels, were used as single prognosticators to predict outcomes following CPR. For clinicians, it may be difficult to remember these individually identified predictors and relevant cut-off points in predicting poor outcomes. The use of common phenotypes, such as hypercapnic or metabolic acidosis, may be more familiar and intuitive for clinicians to react with corresponding interventions.
Study limitations
First, because of the nature of a retrospective study design, we could only establish an association, rather than a causal relationship, between independent variables and outcomes. Additionally, the effects of unmeasured confounding factors may also introduce bias into the analysis. For example, the indications for blood gas analysis and tracheal intubation could not be retrospectively obtained and adjusted for in the multivariable analysis. Second, blood sampling during CPR was technically difficult and therefore, it was difficult to verify whether blood sample was drawn from an artery or a vein source. Although venous pH may be consistent with arterial pH26,27, discrepancies between arterial and venous PCO2 levels have been reported28. This could only be resolved by a prospective study adopting a certified method to obtain arterial blood gas. Third, we did not record the timing and the amount of sodium bicarbonate administered during CPR. The changes in blood pH, PCO2 or HCO3- caused by administration of sodium bicarbonate29 may lead to misclassification bias, which may nullify the association between some blood gas phenotypes and outcomes. However, since the administration of sodium bicarbonate may not significantly improve or worsen the resuscitation outcomes29, the effect of misclassification bias could probably be mitigated to some extent. For example, the significant association between non-severe acidosis and neurological outcomes was still identified in the regression analysis. Fourth, despite that we had accounted for the confounding effects of CPR duration and time to intubation, the resuscitation time bias30 may still be concerning since those patients without intubation during CPR were excluded from the analysis. Fifth, the exact timing of obtaining blood gas samples was not recorded in the previously established IHCA database6,7 and therefore, we could not verify whether the timing of obtaining blood gas samples was prior to the timing of intubation or administration of sodium bicarbonate. Nonetheless, since the clinicians in NTUH were instructed to obtain blood gas analysis as soon as possible in the beginning of CPR, the interval between the timing of blood gas analysis and intubation or administration of sodium bicarbonate may be quite small (maximum: 10 min), which may not cause significant changes in blood gas analysis data. Finally, during the study period between 2006 and 2015, the guidelines31,32 did not recommend the optimal timing of tracheal intubation. The timing of tracheal intubation might be influenced by other unmeasured confounders, such as clinicians’ experience in tracheal intubation. While early tracheal intubation was associated with better outcomes in some phenotypes, the generalizability of this practice should be further examined in a prospective study since this study was based on a highly selected cohort. What was emphasized in the current study was that blood gas analysis could help classify patients into different phenotypes that were associated with outcome and with the effect of a certain intervention. However, the phenotypes may be simplified, and the cut-off points used may not be accurate. Therefore, results of the current investigation are best viewed as a proof-of-concept rather than a definite conclusion, which should be further examined in a prospective study.
Conclusions
Intra-arrest blood gas analysis may assist in phenotyping patients with IHCA. Non-severe acidosis was associated with better neurological and survival outcomes. For patients with non-severe acidosis, early tracheal intubation was associated with favourable neurological outcome, while for patients with metabolic or hypercapnic acidosis, early tracheal intubation was associated with improved survival.
Data availability
The data that support the findings of this study are available on request from the corresponding author, Wen-Jone Chen.
References
Benjamin, E. J. et al. Heart disease and stroke statistics-2017 update: A report from the American heart association. Circulation 135, e146–e603 (2017).
Wang, C. H. et al. The effects of calcium and sodium bicarbonate on severe hyperkalaemia during cardiopulmonary resuscitation: A retrospective cohort study of adult in-hospital cardiac arrest. Resuscitation 98, 105–111 (2015).
Perkins, G. D. et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 132, 1286–1300 (2015).
Bradley, S. M. et al. Retrospective cohort study of hospital variation in airway management during in-hospital cardiac arrest and the association with patient survival: Insights from Get With The Guidelines-Resuscitation. Crit Care 23, 158 (2019).
Andersen, L. W. et al. Association between tracheal intubation during adult in-hospital cardiac arrest and survival. JAMA 317, 494–506 (2017).
Wang, C. H. et al. Associations between body size and outcomes of adult in-hospital cardiac arrest: A retrospective cohort study. Resuscitation 130, 67–72 (2018).
Wang, C. H. et al. The association between long-term glycaemic control, glycaemic gap and neurological outcome of in-hospital cardiac arrest in diabetics: A retrospective cohort study. Resuscitation 133, 18–24 (2018).
ECC Committee, Subcommittees and Task Forces of the American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 112, IV1–203 (2005).
Field, J. M. et al. Part 1: Executive summary: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122, S640–S656 (2010).
Jacobs, I. et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 110, 3385–3397 (2004).
Tiruvoipati, R. et al. Association of hypercapnia and hypercapnic acidosis with clinical outcomes in mechanically ventilated patients with cerebral injury. JAMA Neurol. 75, 818–826 (2018).
Jaber, S. et al. Sodium bicarbonate therapy for patients with severe metabolic acidaemia in the intensive care unit (BICAR-ICU): A multicentre, open-label, randomised controlled, phase 3 trial. Lancet 392, 31–40 (2018).
Becker, L. B. et al. Primary outcomes for resuscitation science studies: A consensus statement from the American Heart Association. Circulation 124, 2158–2177 (2011).
Hastie, T. J. & Tibshirani, R. J. Generalized Additive Models (Chapman & Hall, 1990).
Callaway, C. W. Targeted temperature management after cardiac arrest: Finding the right dose for critical care interventions. JAMA 318, 334–336 (2017).
Benoit, J. L., Prince, D. K. & Wang, H. E. Mechanisms linking advanced airway management and cardiac arrest outcomes. Resuscitation 93, 124–127 (2015).
Spindelboeck, W. et al. Arterial blood gases during and their dynamic changes after cardiopulmonary resuscitation: A prospective clinical study. Resuscitation 106, 24–29 (2016).
Wang, C. H. et al. Comparing effectiveness of initial airway interventions for out-of-hospital cardiac arrest: A systematic review and network meta-analysis of clinical controlled trials. Ann Emerg Med 75, 627–636 (2020).
Izawa, J. et al. Pre-hospital advanced airway management for adults with out-of-hospital cardiac arrest: nationwide cohort study. BMJ 364, l430 (2019).
Lin, C. C. et al. Association between acidosis and outcome in out-of-hospital cardiac arrest patients. Am J Emerg Med 36, 2309–2310 (2018).
Shin, J. et al. Initial blood pH during cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients: A multicenter observational registry-based study. Crit Care 21, 322 (2017).
Wang, C. H. et al. Associations between early intra-arrest blood acidaemia and outcomes of adult in-hospital cardiac arrest: A retrospective cohort study. J Formos Med Assoc 119, 644–651 (2020).
Kim, Y. J. et al. Role of blood gas analysis during cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients. Medicine 95, e3960 (2016).
Farzi, S. et al. Prehospital measurement of arterial base excess and its role as a possible predictor of outcome after out-of-hospital cardiac arrest. Emergencias 25, 47–50 (2013).
Wang, C. H. et al. Monitoring of serum lactate level during cardiopulmonary resuscitation in adult in-hospital cardiac arrest. Crit Care 19, 344 (2015).
Rang, L. C., Murray, H. E., Wells, G. A. & Macgougan, C. K. Can peripheral venous blood gases replace arterial blood gases in emergency department patients?. CJEM 4, 7–15 (2002).
Zeserson, E. et al. Correlation of venous blood gas and pulse oximetry with arterial blood gas in the undifferentiated critically Ill patient. J Intensive Care Med 33, 176–181 (2018).
Steedman, D. J. & Robertson, C. E. Acid base changes in arterial and central venous blood during cardiopulmonary resuscitation. Arch Emerg Med 9, 169–176 (1992).
Ahn, S. et al. Sodium bicarbonate on severe metabolic acidosis during prolonged cardiopulmonary resuscitation: A double-blind, randomized, placebo-controlled pilot study. J Thorac Dis 10, 2295–2302 (2018).
Andersen, L. W., Grossestreuer, A. V. & Donnino, M. W. “Resuscitation time bias”—A unique challenge for observational cardiac arrest research. Resuscitation 125, 79–82 (2018).
Part 7.1: Adjuncts for airway control and ventilation. Circulation 112, IV-51-IV-57 (2005).
Neumar, R. W. et al. Part 8: Adult advanced cardiovascular life support. Circulation 122, S729–S767 (2010).
Acknowledgements
We thank Centre of Quality Management of National Taiwan University Hospital for providing the list of patients sustaining in-hospital cardiac arrest. We thank the staff of the 3rd Core Lab, Department of Medical Research, National Taiwan University Hospital for technical support. Author Chih-Hung Wang recieved a Grant (110-S4808) from the National Taiwan University Hospital. Author Wen-Jone Chen received a Grant (110-S4935) from the National Taiwan University Hospital. National Taiwan University Hospital had no involvement in designing the study, collecting, analysing or interpreting the data, writing the manuscript, or deciding whether to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
C.H.W., W.T.C., and C.H.H. conceived the idea, performed the analysis, and drafted the manuscript. M.S.T., T.C.L., E.C., and Y.W.W. interpreted the results and helped to revise the manuscript. W.J.C. helped to frame the idea of the study and helped to analyse the data. M.C.W. and C.Y.W. contributed to critical revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, CH., Wu, MC., Wu, CY. et al. Blood gas phenotyping and tracheal intubation timing in adult in-hospital cardiac arrest: a retrospective cohort study. Sci Rep 11, 10480 (2021). https://doi.org/10.1038/s41598-021-89920-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89920-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.