Abstract
NUDT15 and TPMT variants are strong genetic determinants of thiopurine-induced hematological toxicity. Despite the impact of homozygous CRIM1 on thiopurine toxicity, several patients with wild-type NUDT15, TPMT, and CRIM1 experience thiopurine toxicity, therapeutic failure, and relapse of acute lymphoblastic leukemia (ALL). Novel pharmacogenetic interactions associated with thiopurine intolerance from hematological toxicities were investigated using whole-exome sequencing for last-cycle 6-mercaptopurine dose intensity percentages (DIP) tolerated by pediatric ALL patients (N = 320). IL6 rs13306435 carriers (N = 19) exhibited significantly lower DIP (48.0 ± 27.3%) than non-carriers (N = 209, 69.9 ± 29.0%; p = 0.0016 and 0.0028 by t test and multiple linear regression, respectively). Among 19 carriers, 7 with both heterozygous IL6 rs13306435 and CRIM1 rs3821169 showed significantly decreased DIP (24.7 ± 8.9%) than those with IL6 (N = 12, 61.6 ± 25.1%) or CRIM1 (N = 94, 68.1 ± 28.4%) variants. IL6 and CRIM1 variants showed marked inter-ethnic variability. Four-gene-interplay models revealed the best odds ratio (8.06) and potential population impact [relative risk (5.73), population attributable fraction (58%), number needed to treat (3.67), and number needed to genotype (12.50)]. Interplay between IL6 rs13306435 and CRIM1 rs3821169 was suggested as an independent and/or additive genetic determinant of thiopurine intolerance beyond NUDT15 and TPMT in pediatric ALL.
Similar content being viewed by others

Introduction
Despite improvements in combination drug therapy and risk stratification, approximately 20% of pediatric patients with acute lymphoblastic leukemia (ALL) still experience drug resistance and treatment failure due to drug toxicities. In European populations, about 50% of thiopurine-induced cytotoxic adverse reactions, such as severe neutropenia and leukopenia, are explained by NUDT15 and TPMT genetic variants1,2,3,4. The Clinical Pharmacogenetics Implementation Consortium (CPIC)5 publishes practical guidelines for the implementation of pharmacogenetic (PGx) testing of thiopurine by using traditional star (*) allele-based molecular phenotyping for NUDT15 and TPMT6,7.
According to the established guideline, the thiopurine dose is pharmacogenetically titrated based on the known risk variants of NUDT15 and TPMT. However, a substantial proportion of patients with leukemia presenting no genetic variation in NUDT15 or TPMT still experience life-threatening toxicities, which may result in dose reduction and/or discontinuation of thiopurine, resulting in therapeutic failure and relapse of leukemia. In an attempt to overcome the PGx gap, CRIM1 rs3821169 homozygote has been identified in East Asians as a novel risk variant of thiopurine-induced hematological toxicities8. Heterozygotes of the variant have revealed only mild effect on thiopurine toxicity with an unknown clinical impact. However, its high prevalence (T = 0.066, Phase 3 of the 1000 Genomes Project9) and remarkable inter-ethnic variability (Table 2) might have severely confounded previous PGx studies assessing thiopurine toxicity. Therefore, investigating PGx interactions of novel genes/variants, other than NUDT15 and TPMT variations, is urgently needed for preventing thiopurine intolerance due to hematological toxicities and improving pediatric ALL care.
The categorical nature of the traditional star allele haplotype-based method can complement the quantitative nature of gene-wise variant burden (GVB) method for evaluating the complex interplay of multiple genes/variants10. For instance, designating three categories [i.e., poor (PM), intermediate (IM), and normal (NM) metabolizers] per gene creates an exponentially increasing complexity of 3N for a drug with N-gene PGx interactions. NUDT15 and TPMT have been assigned nine PGx subgroups for thiopurine, which will increase exponentially following new PGx discoveries across different ethnic groups. GVB quantitates the cumulative variant burden of one or more genes into a single score with dimensionality reduction, thus providing a reliable frame for multiple gene-interaction analysis11,12,13.
In the present study, we aimed to identify novel PGx interactions associated with thiopurine toxicity in pediatric ALL patients carrying both wild-type (WT) NUDT15 and TPMT (and not carrying homozygous CRIM1 rs3821169) by using whole-exome sequencing (WES) technology. Our investigation of the effect of novel candidate PGx variants on the last-cycle 6-mercaptopurine (6-MP) dose intensity percentage (DIP) tolerated by pediatric patients with ALL, revealed clinically significant hematological toxicities and thiopurine intolerance. Our results provide not only the measures of clinical validity but also the measures of population impact (or clinical utility), including relative risk (RR), population attributable fraction (PAF), number needed to treat (NNT), and number needed to genotype (NNG)14, for preventing thiopurine toxicity.
Methods
Subjects
As described in our previous study, we recruited 320 Korean pediatric patients with ALL, who underwent maintenance therapy with 6-MP at three teaching hospitals, Seoul National University Hospital (SNUH), Asan Medical Center (AMC), and Samsung Seoul Medical Center (SMC), located in Seoul, South Korea. All subjects conformed with the exclusion criteria (i.e., relapse of the disease, stem cell transplantation, Burkitt’s lymphoma, mixed phenotype acute leukemia, infant ALL, or very high-risk of ALL)8. Patients were assigned to the standard-risk group if they were 1–9 years of age at the time of diagnosis with a white blood cell (WBC) count less than 50 × 109/L; all other patients were assigned to the high-risk group. Patients underwent hematopoietic stem cell transplantation if they met one or more of the following criteria: age younger than 1 year, hypodiploidy, the presence of t(9;22), a WBC count equal to or greater than 200 × 109/L, or the 11q23 rearrangement15. Patients allocated to the standard-risk group were treated with Children’s Cancer Group (CCG)-189116, CCG-195217 or Children’s Oncology Group (COG) AALL-0331 regimens18. In high-risk groups, CCG-188219, 0601, or 1501 protocols for Korean multicenter studies20 were employed. In Korea, the planned dose of 6-MP was modified from 75 to 50 mg/m2, as several patients who had been administered the same dose under the original Western protocol exhibited moderate to severe toxicities during 6-MP administration15,21. The 6-MP doses during maintenance therapy were adjusted to maintain a WBC count of 2.0–3.5 × 109/L, with an absolute neutrophil count (ANC) of over 500/μL. Hepatotoxicity-related dose modifications were primarily based on the COG guidelines; however, they were also performed at the discretion of the treating physician as this study was not undertaken per the uniform prospective protocols. Hematological toxicity as the clinical endpoint was estimated by the tolerated last-cycle 6-MP DIP (%). The percentage of the actual prescribed amount to the planned dose (50 mg/m2) was defined as the last-cycle 6-MP DIP using the recorded 6-MP dose per meter body surface area over the last-cycle (12-week) of maintenance. Doses employed for the last maintenance cycle were considered, as dose modification of 6-MP was mainly adopted during the early phase of maintenance. Further detailed descriptions of patients and measurements have been summarized in our previous study8,15,21. The present study was approved by the SNUH, AMC, and SMC Institutional Review Boards. Written informed consent was obtained from each participant. For the participants under the age of 18 years, informed consent was obtained from a parent and/or legal guardian. All experiments and methods were performed in accordance with the relevant guidelines and regulations.
Whole-exome sequencing and pharmacogenomic subgrouping
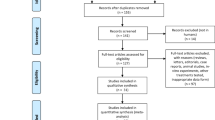
WES data were obtained for pediatric patients with ALL patients and analyzed in a bioinformatics pipeline as previously described8,10,11. CPIC provides major PGx genes with haplotype definitions and molecular function annotations based on star (*) nomenclature. We classified patients with ALL into PM, IM, and NM groups for each gene, NUDT15 and TPMT, according to CPIC classifications6,7. For both genes, we considered NMs as WTs. As in our previous study, data regarding DIP and the relative frequency of neutropenia (ANC < 500 μL) was available for the discovery cohort (N = 244)8. The relative frequency of neutropenia was defined by the ratio of frequencies of complete blood cell counts (CBC) with neutropenia from among the total tested CBCs. However, data regarding the frequency of neutropenia was not collected for the replication cohort (N = 76) at the time of this analysis. Therefore, we conducted a variant selection process using the discovery cohort. First, we performed multivariate linear regression, adjusting age, sex, and body surface area. Of 14,931 genes with GVB scores, 10 genes were identified with statistical significance at both DIP and the relative frequency of ANC < 500 μL. Next, we identified 45 variants with SIFT (sorting intolerant from tolerant) scores from among 156 variants of genes that passed multivariate linear regression with GVB score. Among the 45 variants, 3 variants passed the multivariate linear regression cutoff for SNPs22. Finally, we selected IL6 rs13306435 as a novel candidate, which was only a missense variant among 3 variants (Fig. 1, Supplementary Table S1). We observed that no star name had been designated to the novel (or candidate) PGx genes. Thus, for the purpose of the present study, we defined non-carriers of CRIM1 rs3821169 and IL6 rs13306435 as WT carriers (WTs) of CRIM1 and IL6, respectively (Table 2). Haplotypes were determined using PHASE 2.1.123,24.
Workflow schema of the discovery phase. Variants with SIFT score less than 0.7 were incorporated into the GVB score calculation. Gene-wise multiple covariate linear regression was performed, and filtered genes were defined as candidate genes. Next, variant-wise multiple covariate linear regression was performed, and variants with filtered thresholds were deemed candidate variants. SIFT sorting intolerant from tolerant, GVB gene-wise variant burden.
Gene-wise variant burden for evaluating single- and multi-gene effects
GVB analysis was performed to evaluate the aggregated impact of both common and rare variants10,11. For each individual, the GVB of a coding gene was defined as the geometric mean of the SIFT22 scores of the coding variants (with SIFT score < 0.7) in the coding gene, where GVBG denotes the GVB score of gene G [range 0.0–1.0]. The more deleterious the variant burden, the lower the score. First, we included NUDT15 and TPMT in GVB analysis because these genes are clinically recognized to be related to thiopurine-induced toxiticy and have clinical guidelines like CPIC guidelines. Additionally, we included CRIM1 rs3821169, which was identified in our previous study to define conditional GVB8. Finally, we included IL6 rs13306435 following the selection process stated above. The multi-gene effect was evaluated by defining GVBA,B,C as the geometric mean of GVBA, GVBB and GVBC [range 0.0–1.0]. Gene-variant interaction was considered by defining conditional GVBG^(variant) as the GVB score of gene G, depending on the presence or absence of the specified variant. For example, GVBCRIM1^(rs13306435) equals GVBCRIM1 when rs13306435 is present, vanishing to a WT score of 1.0 when absent.
Inter-ethnic variability of allele frequencies and molecular phenotypes
Using the 2504 whole-genome sequences with multiple ethnicities provided by the 1000 Genomes Project phase 39, we investigated inter-ethnic distributions of PGx alleles and haplotypes, along with their molecular phenotypes associated with thiopurine intolerance due to hematological toxicities (Table 2).
Statistical analysis
The last-cycle 6-MP DIPs (%) according to different PGx groups were assessed using Student’s t test or one-way ANOVA with posthoc Tukey test. Multiple linear regression was also applied to adjust for confounding clinical variables. The powers of GVBNUDT15, GVBTPMT, GVBCRIM1, and GVBIL6, and their combinations for predicting 6-MP DIPs, were systematically evaluated by analyzing ROC (receiver operating characteristic) curves across eight different DIP cutoffs (i.e., 10%, 15%, 25%, 35%, 45%, 60%, 80%, and 100%) in terms of AUCs (areas under the ROC curves) (Figs. 3, 4). An ROC curve is a two-dimensional depiction of classification performance integrating all sensitivity and specificity values at all cutoff levels25. All statistical analyses were performed using the R statistical package (version 3.5.1). R package ‘pROC’ was used for calculating AUC values26. The optimal cutoff for the GVB score was determined by maximizing Youden’s index27.
GVBCRIM1^(rs3821169*) was applied to control the potential confounding effect of the impressively high carrier frequency in East Asians [43.7% (= 220/504)], compared with other ethnicities (0.2–9.4%), and the mild effect of heterozygous expression on thiopurine intolerance attributed to hematological toxicities. GVBCRIM1^(rs3821169*) denotes a conditional GVB score of CRIM1 dependent on the presence or absence of homozygous rs3821169 variant (denoted as rs3821169*). It equals GVBCRIM1 when the subject carries homozygous rs3821169 variant and otherwise vanishes to 1.0.
Clinical validity parameters
We calculated and assessed clinical validity for each statistical parameter as follows.
Positive predictive value (PPV) implies the probability of an event when the genetic variant is present. In contrast, negative predictive value (NPV) means the probability of no event when the genetic variant is absent.
NNT is the inverse of the absolute of intervention, that is, the difference between the proportion of events in the control group and the proportion of events in the case group, which can be written as.
If NNT is 20, it implies that 20 patients are needed to prevent an event like death or an adverse effect. NNG is the number of patients who must be genotyped to avoid one patient from experiencing an adverse event, which can be predicted based on following formula
For example, an NNG of 33 means that one adverse event was avoided for every 33 patients genotyped.
RR is the relative ratio of the proportion of events in the control group and the proportion of events in the case group, which is calculated by following formula.
Odds ratio (OR) is calculated based on the comparison of the relative odds of an event in each group, which can be determined as
In the above Eqs. (1),(2),(3),(4), \({P}_{c}\) is the proportion of events in the control group and \({P}_{i}\) is the proportion of events in the case group. PAF is the proportion of events that would be eliminated from the population if exposure to the risk factor were eliminated, which can be assessed as
In Eq. (5), Y is an event development and X is a binary risk factor14.
Results
IL6 rs13306435 as a novel pharmacogenetic variant for thiopurine intolerance due to hematological toxicities
We classified patients into three groups according to the variant status of NUDT15 and TPMT to identify new variants not confounded by the two most critical PGx genes associated with thiopurine intolerance. Table 1 describes the clinical characteristics of 320 pediatric patients with ALL according to their PGx subgroups, presenting 80 patients who were non-WTs (i.e., IMs or PMs) of NUDT15 and/or TPMT (N = 80), 115 patients who were all WTs (WT carriers of all the four genes), and 125 who were WTs of both genes, NUDT15 and TPMT (both WTs) and carried CRIM1 rs3821169 and/or IL6 rs13306435 variants. Of the 125 patients with WT characterization for both NUDT15 and TPMT, 94, 12, 11, and 8 patients belonged to the heterozygous CRIM1, heterozygous IL6, homozygous CRIM1, and IL6 and CRIM1 variant groups, respectively (Table 1).We used patients with all WTs (N = 115) as a control group for the following analysis. The average of the tolerated 6-MP DIPs of non-WTs for NUDT15 (47.1 ± 30.5%, N = 72) and/or for TPMT (56.6 ± 33.6%, N = 9) were significantly lower than that of all WTs (71.3 ± 29.6%, N = 115) (p < 0.001, Table 1). The patients with homozygous CRIM1 (dark blue circle in Fig. 3) tolerated significantly lower 6-MP DIP than the patients with all WTs before (N = 16, 44.6 ± 35.2%) or after (N = 11, 42.3 ± 35.0%) controlling the five subjects with NUDT15 (59.76 ± 37.24%) or IL6 (9.77%) variants.
To rule out the PGx effect of NUDT15, TPMT, and homozygous CRIM1 on thiopurine intolerance, we extracted 228 samples of non-carriers for these variants for the further discovery of novel PGx variants. We observed that carriers of IL6 rs13306435 (N = 19, 48.0 ± 27.3%) exhibited significantly lower 6-MP DIPs than non-carriers (N = 209, 69.9 ± 29.0%), as evaluated by Student’s t test (p = 0.0016) and multiple covariate linear regression (p = 0.0028). Furthermore, of the 19 carriers, 7 patients with both IL6 rs13306435 and CRIM1 variants demonstrated significantly lower 6-MP intolerance, with a DIP of 24.7 ± 8.9% when compared with the DIP of 12 patients harboring only IL6 rs13306435 variant (61.6 ± 25.1%; orange circle in Fig. 3). The potential interplay between IL6 and CRIM1 variants was suggested, which was further supported by the finding that seven patients with both IL6 and CRIM1 variants showed significantly lower 6-MP DIPs (24.7 ± 8.9%) than 94 heterozygous CRIM1 carriers (68.1 ± 28.4%; light blue circle in Fig. 3).
Interplay of IL6 and CRIM1 variants in thiopurine toxicity
Figure 2 exhibits the distributions of the last-cycle 6-MP DIPs (%) of 115 all WTs (Fig. 2a), carriers of only heterozygous CRIM1 (N = 94, Fig. 2b), carriers of only heterozygous IL6 (N = 12, Fig. 2c), carriers of only homozygous CRIM1 (N = 11, Fig. 2d), and carriers of both IL6 and CRIM1 variants (N = 8, Fig. 2e). Homozygous CRIM1 and IL6 and CRIM1 groups showed significantly lower 6-MP DIPs (44.6 ± 35.2% and 24.7 ± 8.9%, respectively, Fig. 2d,e) than all WTs and heterozygous CRIM1 groups (71.3 ± 29.6% and 68.1 ± 28.4%, respectively, Figs 2a,b) by one-way ANOVA (p = 0.0001; adj. p < 0.05 posthoc Tukey). Furthermore, the IL6 and CRIM1 group showed significantly lower 6-MP DIPs (44.6 ± 35.2%) than the heterozygous IL6 group (61.6 ± 25.1%; adj. p < 0.05, posthoc Tukey) (Fig. 2c,e). All 10 patients with both IL6 and CRIM1 variants with any NUDT15 or TPMT status (red numbers in Fig. 3) exhibited the lowest DIPs (9.77–32.68%) among all subgroups of the whole PGx groups. Thus, a significant interplay between IL6 and CRIM1 in thiopurine intolerance was suggested.
Distribution of the average of the tolerated last-cycle 6-MP DIPs (%) of the CRIM1 rs3821169 and/or IL6 rs13306435 variant carrier vs. non-carrier subgroups among 240 pediatric patients with ALL presenting both NUDT15 and TPMT WT characterization. Of the 320 pediatric patients with ALL, we excluded 80 carriers presenting either NUDT15 or TPMT variants to obtain 240 subjects with both NUDT15 and TPMT WT. Both (a) non-carrier group of CRIM1 rs3821169 or IL6 rs13306435 (N = 115, 47.92%, i.e., “All WTs” in Table 2 and Fig. 3) and (b) carrier group of heterozygous CRIM1 rs3821169 only (N = 94, 39.17%) showed significantly higher thiopurine tolerance than the carrier groups of (d) homozygous CRIM1 rs3821169 (N = 11, 4.38%) (adj. p < 0.05, posthoc Tukey) and of (e) both IL6 rs13306435 and CRIM1 rs3821169 (N = 8, 3.33%) (adj. p < 0.0005, posthoc Tukey) by one-way ANOVA (p = 0.0001). (c) Carrier group of IL6 rs13306435 heterozygous variant only (N = 12, 5.00%) showed significantly higher thiopurine intolerance than (c) that of the hetero/homozygous variant of both IL6 and CRIM1 (adj. p < 0.05, posthoc Tukey). No carrier of homozygous IL6 was detected, and only one subject carried both heterozygous IL6 and homozygous CRIM1 variants (DIP = 9.7%). Thiopurine intolerance was measured by the last-cycle 6-MP DIP (%) among 240 pediatric patients with ALL presenting both NUDT15 and TPMT WT genes to control their effect on thiopurine intolerance. *p < 0.05 and **p < 0.01, posthoc Tukey test after one-way ANOVA. ALL acute lymphoblastic leukemia, WT wild-type, DIP (%) dose intensity percentage, 6-MP 6-mercaptopurine.
Distribution of the last-cycle 6-MP DIP for pediatric patients with ALL according to NUDT15, TPMT, CRIM1, and IL6 pharmacogenetic subgroups (N = 320). Green circles depict NUDT15 and TPMT metabolism phenotypes, and blue and orange circles represent CRIM1 rs3821169 and IL6 rs13306435 genotype subgroups, respectively. Of the 320 patients, 115 with no pharmacogenetic variants exhibited higher 6-MP DIPs (71.31%) than 72 NUDT15 (47.14%), 9 TPMT (56.56%), 147 CRIM1 (57.89%), and 25 IL6 (DIP = 44.47%) non-WTs. Subjects with both CRIM1 and IL6 variants (N = 10, 3.13%) exhibited the lowest DIPs (9.77–32.68%, in red numbers). Numbers are the number of subjects and 6-MP DIPs (mean ± SD). ALL acute lymphoblastic leukemia, WT wild-type, non-WT non-wild-type (i.e., poor- or intermediate thiopurine-metabolizing sub-groups of NUDT15 and TPMT carriers), DIP dose intensity percentage, SD standard deviation.
Notably, it was more clinically relevant to evaluate the magnitude of the actual decrease in 6-MP DIP (%) tolerated by patients than the mere statistical significance affected by the study sample size and biomarker prevalence. Table 1 shows that more than one-quarter of the patients with homozygous CRIM1 (36.4%) and IL6 and CRIM1 (50.0%) tolerated less than 25% of the planned DIP, increasing the risk of thiopurine therapeutic failure. The DIPs of our cohorts were comparable with those of the recommended 6-MP doses published in the current CPIC guideline when NUDT15 or TPMT variants were involved28. Furthermore, when we raised the DIP cutoff from 25 to 35%, the proportions of homozygous CRIM1 and IL6 and CRIM1 groups increased to 54.6% (6/11) and 87.5% (7/8), respectively, which far exceeded 38.9% and 33.3% of NUDT15 (28/72) and TPMT (3/9) non-WTs, respectively. Notably, only 6.1% (7/115) and 10.5% (12/115) of all WTs tolerated less than 25% and 35% of the planed DIP (Table 1).
Inter-ethnic variabilities in carrier frequencies and molecular phenotypes
Both NUDT15 and TPMT show wide inter-ethnic variabilities. Table 2 exhibits inter-ethnic variabilities of the PGx variants and molecular phenotypes of the four thiopurine pharmacogenes computed from among 2504 subjects of the 1000 Genomes Project9. NUDT15 non-WT (i.e., IM or PM) is common in East (22.6%) and South (13.9%) Asians but rare in Europeans and Africans (< 1%). In contrast, TPMT non-WT is common in Europeans (8.0%) and Americans (13.3%) but relatively rare in Asians (< 5.0%).
Novel PGx variant, CRIM1 rs3821169, demonstrates remarkably high minor allele frequency (T = 0.255) and carrier prevalence (43.7%, 220/504) in East Asians. Table 2 also shows that 6.5% of East Asians harbor homozygous CRIM1 rs3821169 variant, which can hardly be detected in other populations (< 1.0%). In contrast, IL6 rs13306435 is widely distributed with the highest carrier frequency of 15.0% in Americans and 3.0% among Asian and European populations; It is rare in South Asian and African populations (< 1.0%). The carrier frequencies of both IL6 and CRIM1 variants were 2.0% and 1.2% for East Asian and American populations, respectively.
Single- and multi-gene prediction performances of IL6 and CRIM1
We performed ROC analysis of GVB-based single- and multi-gene models to predict the last-cycle 6-MP DIPs (%) using 240 both WTs for NUDT15 and TPMT to control their long-known PGx effects. Figure 4 demonstrates that (b) GVBCRIM1 outperformed (a) GVBIL6 in predicting DIPs at all cutoff levels, probably due to the higher variant frequency of CRIM1 over IL6 in the study population. Two-gene model GVBIL6,CRIM1 (Fig. 4c) consistently outperformed each of the single-gene models (GVBIL6 and GVBCRIM1) at all cutoffs.
ROC analysis of IL6, CRIM1, and their combined prediction accuracies for thiopurine intolerance among pediatric patients with ALL presenting wild-type NUDT15 and TPMT genes (N = 240). Single-gene prediction models of (a) IL6 and (b) CRIM1 were highly outperformed by (c) the two-gene combined model for predicting thiopurine intolerance at all DIP levels. We excluded 80 subjects from among the total of 320 subjects to control the effects of the well-established NUDT15 and TPMT genes and performed ROC analysis for the 240 subjects with both wild-type NUDT15 or TPMT genes. Prediction accuracies were measured across 8 cutoff levels for the last-cycle 6-MP DIP (%) (≤ 10%, ≤ 15%, ≤ 25%, ≤ 35%, ≤ 45%, ≤ 60%, ≤ 80%, and ≤ 100%) in terms of AUC. ROC receiver operating characteristics, DIP (%) dose intensity percentage, AUC area under the ROC curve, GVB gene-wise variant burden; GVBCRIM1^(rs13306435, rs3821169*), GVB of CRIM1 dependent on IL6 rs13306435 or CRIM1 rs3821169 homozygote; 6-MP, 6-mercaptopurine.
For a comprehensive evaluation of all PGx interactions among NUDT15, TPMT, IL6, and CRIM1, we performed comprehensive ROC analysis using data of all 320 pediatric patients with ALL (Fig. 5). Among the four single-gene models in Fig. 5a,b,d), GVBNUDT15 outperformed others at all cutoffs, probably due to the high prevalence of NUDT15 variants and the strong metabolic impact of on thiopurine toxicity. Two-gene models (Fig. 5c,f) consistently outperformed each of the corresponding single-gene counterparts, i.e., the order of their AUCs was GVBNUDT15,TPMT > GVBNUT15 > GVBTPMT and of GVBIL6,CRIM1 > GVBCRIM1 > GVBIL6 at all cutoff levels. Three-gene models created by adding IL6 or CRIM1 to the traditional NUDT15 and TPMT model also consistently improved the prediction accuracy (Fig. 5g,h). The final four-gene model in Fig. 5(i) outperformed all other models in predicting DIPs at all cutoff levels. Moreover, it is worth noting that the ROC curves across eight DIP cutoffs in Fig. 5 exhibited ‘dose–response relationships’, i.e., GVB score’s prediction power (measured by AUC) increases as a function of the severity of thiopurine intolerance (measured by DIP). That is, the final four-gene model’s AUC increased as a function of decreasing DIP (%) (i.e., AUC<15% = 0.757, AUC<25% = 0.748, AUC<35% = 0.711, AUC<45% = 0.716, AUC<60% = 0.646, and AUC<80% = 0.592 in a descending order, Fig. 5i).
Prediction accuracy profile of single- and multi-gene models for thiopurine intolerance in pediatric patients with ALL (N = 320). Single-gene prediction models of (a) NUDT15 and (b) TPMT were outperformed by (c) the two-gene combined model and those of (d) IL6 and (e) CRIM by (f) the IL6-CRIM1 combined model. Three-gene models of NUDT15, TPMT, and (g) IL6 and (h) CRIM1 were outperformed by (i) all four-gene combined models. Overall the final (i) four-gene combined models outperformed other models for predicting thiopurine intolerance at all DIP levels in pediatric patients with ALL (N = 320). AUCs for predicting the last-cycle 6-MP DIP (%) were measured at 8 cutoff levels (≤ 10%, ≤ 15%, ≤ 25%, ≤ 35%, ≤ 45%, ≤ 60%, ≤ 80%, and ≤ 100%). ALL acute lymphoblastic leukemia, DIP dose intensity percentage, AUC area under the receiver operating characteristics curve, GVB gene-wise variant burden.
Evaluation of the clinical validity and utility of the star allele and GVB methods
We systematically compared the clinical utility as well as clinical validity of traditional star (*) allele-based and GVB-based methods for preventing thiopurine toxicity. Table 3 demonstrates the measures of clinical validity and potential population impact along with the pharmacogenetic association of the different prediction models14. Because the designated star alleles for IL6 or CRIM1 were not available, star allele-based molecular phenotyping was not applicable for these novel genes.
GVBNUDT15,TPMT slightly outperformed STARNUDT15,TPMT, the classical star (*) allele-based molecular phenotyping (Table 3a,b). Three-gene models (i.e., GVBNUDT15,TPMT,IL6 and GVBNUDT15,TPMT,CRIM1* also outperformed the two-gene models (Table 3c,d). The four-gene interplay model, GVBNUDT15,TPMT,IL6,CRIM1^(CRIM1,IL6), presented the best performance for all the eight measures of clinical validity and potential population impact (except specificity) (marked in bold numbers in Table 3g).
The addition of IL6 and CRIM1 to create the final four-gene model by integrating both common and rare alleles markedly improved PAF from 0.36 to 0.58 as well as RR (3.29–5.73) and OR (4.21–8.06). PAF is the proportion of events attributed to the PGx risk factor or the maximum percentage of cases that can be prevented if individuals who test positive for the PGx variants receive different treatments.
In the group of all the patients with 6-MP toxicities (DIP < 25%), we could expect eight patients more with the GVB-based model than with the traditional star (*) allele-based method [23 patients in Table 3a vs. 31 patients in Table 3f]. NNG is the number of patients that must be genotyped to prevent one patient from experiencing an adverse event. The NNG of 20 and an NNT of 5 of the traditional STARNUDT15,TPMT showed that 5 out of every 20 patients genotyped would be found to have positive test results for genotyping and would need alternative treatment to prevent toxicity related 6-MP intolerance in one patient (DIP < 25%). Adding IL6 and CRIM1 to the traditional NUDT15 and TPMT testing to create GVBNUDT15,TPMT,IL6,CRIM1^(CRIM1,IL6) may require only 12.5 patients (37.5% improvement of NNG) to be genotyped to return 3.7 test-positive patients (26.0% improvement of NNT) receiving alternative treatment to prevent adverse event in one patient (Table 3g).
Ethics approval and consent to participate
Informed written consent was obtained from all subjects, and the study was approved by the ethics committees of Asan Medical Center, Seoul National University Hospital, and Samsung Medical Center.
Discussion
In the present study, the interplay between IL6 and CRIM1 variants in thiopurine intolerance due to hematological toxicity was investigated in 320 pediatric patients with ALL.
IL6 has been known to modulate hematopoiesis and neutrophil trafficking, especially possessing a role in anti-apoptosis29. In patients with osteomyelitis, IL6 was correlated with longer neutrophil survival apart from other cytokines; this anti-apoptotic effect was blocked using anti-IL6 antibodies and reversed with anti-IL630. According to a recent study on chronic hepatitis C infection, the expression of anti-apoptotic genes was increased following in vitro IL6 treatment, with a considerable downregulation in T cell inhibitory receptors and caspase-3, thus indicating the promising nature of IL6 in enhancing lymphocyte effector functions31. These anti-apoptotic roles seemed to be secondary to the effects of IL6 trans-signaling, such as the inhibition of the chemokines CXCL1, CXCL8 and CX3CL1 and the promotion of the chemokines CXCL5, CXCL6, and CCL2; however, the suppression of IL6 might result in blood cytopenia. The occurrence of neutropenia as an adverse effect of the IL6 inhibitor, tocilizumab, could also demonstrate the relationship between IL6 and neutrophil survival. IL6 mobilizes neutrophils into the circulating pool from the marginated pool comprising the lymph nodes and the spleen. Therefore, neutropenia due to a lack of IL6 induced by tocilizumab may indicate that IL6 has a critical role in enriching circulating neutrophils32.
IL6 variant, rs13306435, is located in exon 5 of the IL6 gene. The T>A variation of rs13306435 has an altered amino acid, from Asp to Glu. The T allele of 13306435 is reportedly associated with increased expression and plasma levels of IL633. In this regard, patients with a heterozygous variant of rs13306435 might have decreased expression and plasma levels of IL6 compared with the patients with the WT characterization, resulting in reduced IL6 effects on neutrophils.
CRIM1 is a cell-surface transmembrane protein that resembles developmentally important proteins which are known to interact with bone morphogenetic proteins (BMPs). A role of CRIM1 in drug resistance has been suggested by previous studies34,35 revealing that the level of mRNA expression of CRIM1 is high in resistant leukemic cells. This affects the levels of BMPs, suggesting that CRIM1 regulates the growth and differentiation of hematopoietic cells. The rs3821169 heterozygous cases revealed lower mRNA expression levels than the WT cases, which indicated that subjects carrying this variant might display drug-sensitive responsiveness8. Although we could not clarify the detailed mechanism underlying the interplay between IL6 and the CRIM1 variant, the presence of a negative feedback loop between IL6 and the BMP pathway was reported, in which increased levels of IL6 induced BMP pathway activities resulting in the suppression of IL636. Based on our findings, it can be suggested that the interplay between IL6 and CRIM1 in thiopurine intolerance due to hematological toxicity may represent a pharmacodynamic effect leading to an adverse reaction, while the well-known NUDT15 and TPMT are pharmacokinetic enzymes for metabolizing thiopurines.
The present study presented several limitations that need to be acknowledged, including the possible confounding effects from concomitant medications (methotrexate or vincristine) and the absence of serum level measurements of drugs or metabolites. Moreover, not all patients with thiopurine toxicity were explained by pharmacogenetic analysis. Seven (6.1%) of the 115 all-WT patients experienced thiopurine toxicity. Supplementary Table S2 lists further candidate variants determined by analyzing the all WTs (N = 115, p < 0.05 by one-sided Student’s t test). Of the three carriers of FSIP2 rs191083003, two (66.7%) exhibited DIP < 25% (8.82, 21.88, and 48.54%, N = 3). We observed one more FSIP2 rs191083003 carrier in the homozygous-CRIM1 group, who exhibited the lowest DIP of 6.94% within the entire ALL cohort (N = 320). The low frequency (1.25%, 4/320) of FSIP2 rs191083003 prohibited any conclusion, necessitating further elucidation. Overall, the interplay between IL6 and CRIM1 and the well-known NUDT15 and TPMT improved PAF from 36.4 to 58.2% by considering PGx variants only in an East Asian cohort of pediatric ALL (N = 320). The quantitative analytical approach employed in the present study could be applied to other ethnic groups for further discover and evaluate thiopurine-related pharmacogenomics.
Reportedly, Americans present the highest allele frequency of IL6 rs13306435 (A = 0.078) among all ethnic groups (Global A = 0.020, the 1000 Genomes Project, Phase 39). This high inter-ethnic variability may partially explain why rs13306435 has not yet been identified as a biomarker for thopurine intolerance. Current research is mostly biased towards Europeans37. NUDT15 rs116855232 variant, which was recently discovered in the Korean population as a strong predictor of thopurine toxicity3, shows the highest allele frequency in East Asians (T = 0.095) among all ethnic groups (Global T = 0.040). Pharmacogenes, by definition, unlike pathogenic disease genes, do not have an overt phenotype unless exposed to drugs. The absence of detrimental phenotypic effect attributed to phrmacogenes may have permitted wide inter-ethnic variability and/or diversity across different ethnic groups under various evolutionary selection pressures.
For pediatric ALL, the CPIC guideline for thiopurine treatment is based on the star (*) allele-based haplotypes, with designated molecular phenotypes of NUDT15 and TPMT6,7. However, CPIC does not provide general standard rules for combining multi-gene interactions of the categorically classified star-alleles. Novel genes like IL6 and CRIM1 have no designated star alleles nor molecular phenotypes. The quantitative GVB method has benefits over categorical star allele-based approaches. GVB quantitates single- or multi-gene PGx burden of common, rare, and novel variants into a single score to provide a comprehensive framework for further PGx discovery and evaluation of many gene interactions. A conventional single variant-based association test of rare variants requires an infeasible magnitude of sample sizes38; however, approaches that aggregate common, rare, and novel variants jointly will substantially reduce the required effective sample sizes39. In contrast to a traditional haplotyping-based method, GVB assigns a gene-level score for each pharmacogene without using population data, enabling an unbiased PGx approach, especially for under-investigated subpopulations.
Conclusion
In summary, our results suggest an independent and/or additive effect of the interplay between IL6 rs13306435 and CRIM1 rs3821169 on thiopurine intolerance attributed to hematological toxicity in pediatric ALL.
Data availability
All data generated or analyzed during this study are included in this article. If any additional information is required, it may be obtained by request from the corresponding author.
Abbreviations
- ALL:
-
Acute lymphoblastic leukemia
- DIP:
-
Dose intensity percentage
- GVB:
-
Gene-wise Variant Burden
- CPIC:
-
Clinical Pharmacogenetics Implementation Consortium
- PGx:
-
Pharmacogenetic
- PM:
-
Poor metabolizer
- IM:
-
Intermediate metabolizer
- NM:
-
Normal metabolizer
- WT:
-
Wild-type
- WES:
-
Whole-exome sequencing
- RR:
-
Relative risk
- PAF:
-
Population attributable fraction
- NNT:
-
Number needed to treat
- NNG:
-
Number needed to genotype
- 6-MP:
-
6-Mercaptopurine
- SNUH:
-
Seoul National University Hospital
- AMC:
-
Asan Medical Center
- SMC:
-
Samsung Seoul Medical Center
- CCG:
-
Children’s Cancer Group
- ANC:
-
Absolute neutrophil count
- SIFT:
-
Sorting intolerant from tolerant
- AUCs:
-
Areas under the ROC curves
- OR:
-
Odds ratio
- IL-6R:
-
Interleukin 6 receptor
- CRIM1:
-
Cysteine-Rich Transmembrane BMP Regulator 1
- BMPs:
-
Bone morphogenetic proteins
References
Schaeffeler, E. et al. Impact of NUDT15 genetics on severe thiopurine-related hematotoxicity in patients with European ancestry. Genet. Med. 21(9), 2145–2150 (2019).
Yang, J. J. et al. Inherited NUDT15 variant is a genetic determinant of mercaptopurine intolerance in children with acute lymphoblastic leukemia. J. Clin. Oncol. 33(11), 1235 (2015).
Yang, S.-K. et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat. Genet. 46, 1017–1020 (2014).
Moriyama, T. et al. NUDT15 polymorphisms alter thiopurine metabolism and hematopoietic toxicity. Nat. Genet. 48(4), 367–373 (2016).
Relling, M. V. & Klein, T. E. CPIC: Clinical pharmacogenetics implementation consortium of the pharmacogenomics research network. Clin. Pharmacol. Ther. 89(3), 464–467 (2011).
Relling, M. V. et al. Clinical pharmacogenetics implementation consortium guidelines for thiopurine methyltransferase genotype and thiopurine dosing: 2013 update. Clin. Pharmacol. Ther. 93(4), 324–325 (2013).
Relling, M. V. et al. Clinical pharmacogenetics implementation consortium guideline for thiopurine dosing based on TPMT and NUDT15 genotypes: 2018 update. Clin. Pharmacol. Ther. 105(5), 1095–1105 (2019).
Park, Y. et al. A CRIM1 genetic variant is associated with thiopurine-induced neutropenia in leukemic patients with both wild-type NUDT15 and TPMT. J. Transl. Med. 18(1), 1–13 (2020).
Genomes, P. C. et al. A global reference for human genetic variation. Nature 526(7571), 68–74 (2015).
Lee, K. H. et al. Genome sequence variability predicts drug precautions and withdrawals from the market. PLoS One 11, e0162135-e1162115 (2016).
Park, Y. et al. Star allele-based haplotyping versus gene-wise variant burden scoring for predicting 6-mercaptopurine intolerance in pediatric acute lymphoblastic leukemia patients. Front Pharmacol. 10, 654 (2019).
Park, Y., Seo, H., Ryu, B. Y. & Kim, J. H. Gene-wise variant burden and genomic characterization of nearly every gene. Pharmacogenomics 21(12), 827–840 (2020).
Park, J. et al. Gene-wise burden of coding variants correlates to noncoding pharmacogenetic risk variants. Int. J. Mol. Sci. 21(9), 3091 (2020).
Tonk, E. C. M., Gurwitz, D., Maitland-van der Zee, A.-H. & Janssens, A. C. J. W. Assessment of pharmacogenetic tests: Presenting measures of clinical validity and potential population impact in association studies. Pharmacogenom. J. 17(4), 386–392 (2017).
Kim, H. et al. APEX1 polymorphism and mercaptopurine-related early onset neutropenia in pediatric acute lymphoblastic leukemia. Cancer Res Treat. 50(3), 823–834 (2018).
Lange, B. J. et al. Double-delayed intensification improves event-free survival for children with intermediate-risk acute lymphoblastic leukemia: A report from the Children’s Cancer Group. Blood 99(3), 825–833 (2002).
Matloub, Y. et al. Intrathecal triple therapy decreases central nervous system relapse but fails to improve event-free survival when compared with intrathecal methotrexate: Results of the Children’s Cancer Group (CCG) 1952 study for standard-risk acute lymphoblastic leukemia, reported by the Children’s Oncology Group. Blood 108(4), 1165–1173 (2006).
Maloney, K. W. et al. Outcome in children with standard-risk B-cell acute lymphoblastic leukemia: Results of children’s oncology group trial AALL0331. J. Clin. Oncol. 38(6), 602–612 (2020).
Nachman, J. et al. Response of children with high-risk acute lymphoblastic leukemia treated with and without cranial irradiation: A report from the Children’s Cancer Group. J. Clin. Oncol. 16(3), 920–930 (1998).
Rhee, E. S. et al. Outcome and prognostic factors in pediatric precursor T-cell acute lymphoblastic leukemia: A single-center experience. Clin. Pediatr. Hematol. Oncol. 25(2), 116–127 (2018).
Kim, H. et al. Pharmacogenetic analysis of pediatric patients with acute lymphoblastic leukemia: A possible association between survival rate and ITPA polymorphism. PLoS One 7(9), e45558 (2012).
Ng, P. C. SIFT: Predicting amino acid changes that affect protein function. Nucleic Acids Res. 31, 3812–3814 (2003).
Stephens, M. & Scheet, P. Accounting for decay of linkage disequilibrium in haplotype inference and missing-data imputation. Am. J. Human Genet. 76(3), 449–462 (2005).
Stephens, M., Smith, N. J. & Donnelly, P. A new statistical method for haplotype reconstruction from population data. Am. J. Human Genet. 68(4), 978–989 (2001).
Fawcett, T. An introduction to ROC analysis. Pattern Recogn. Lett. 27(8), 861–874 (2006).
Robin, X. et al. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 12(1), 77 (2011).
Youden, W. J. Index for rating diagnostic tests. Cancer 3(1), 32–35 (1950).
Relling, M. V. et al. Clinical pharmacogenetics implementation consortium guideline for thiopurine dosing based on TPMT and NUDT 15 genotypes: 2018 update. Clin. Pharmacol. Therap. 105(5), 1095–1105 (2019).
Hunter, C. A. & Simon, A. J. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 16(5), 448–457 (2015).
Asensi, V. et al. In vivo interleukin-6 protects neutrophils from apoptosis in osteomyelitis. Infect. Immunity 72(7), 3823–3828 (2004).
Naseem, S. et al. Interleukin-6 rescues lymphocyte from apoptosis and exhaustion induced by chronic hepatitis C virus infection. Viral Immunol. 31(9), 624–631 (2018).
Ogata, A. et al. IL-6 inhibitor for the treatment of rheumatoid arthritis: A comprehensive review. Mod. Rheumatol. 29(2), 258–267 (2019).
Fishman, D. et al. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J. Clin. Investig. 102(7), 1369–1376 (1998).
Renkert, M., Uggla, B., Tidefelt, U. & Strid, H. CRIM1 is expressed at higher levels in drug-resistant than in drug-sensitive myeloid leukemia HL60 cells. Anticancer Res. 30(10), 4157–4161 (2010).
Ziliak, D. et al. Genetic variation that predicts platinum sensitivity reveals the role of miR-193b* in chemotherapeutic susceptibility. Mol. Cancer Ther. 11(9), 2054–2061 (2012).
Hagen, M. et al. Interaction of interleukin-6 and the BMP pathway in pulmonary smooth muscle. Am. J. Physiol. Lung Cell. Mol. Physiol. 292(6), L1473–L1479 (2007).
Sirugo, G., Williams, S. M. & Tishkoff, S. A. The missing diversity in human genetic studies. Cell 177, 26–31 (2019).
Bansal, V., Libiger, O., Torkamani, A. & Schork, N. J. Statistical analysis strategies for association studies involving rare variants. Nat. Rev. Genet. 11(11), 773–785 (2010).
Witte,. Rare genetic variants and treatment response: Sample size and analysis issues. Stat. Med. 31(25), 3041–3050 (2012).
Funding
This research was supported by a Grant (16183MFDS541) from Ministry of Food and Drug Safety in 2019.
Author information
Authors and Affiliations
Contributions
H.K., S.Y., H.J.I., H.J.K., and J.H.K. designed the model and the framework. H.K., J.Y.C., Y.M., K.H.Y., H.J.I., and H.J.K. collected samples and clinical data. S.Y., Y.P., and S.Y. analyzed the data and carried out the implementation of the idea. S.Y. performed the calculations. S.Y. and J.H.K. wrote the manuscript. K.T.H, K.N.K., K.H.L., H.Y.S., and S.L. reviewed the manuscript. J.H.K., H.J.K, and H.J.I. conceived the study and were in charge of its overall direction and planning. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H., You, S., Park, Y. et al. Interplay between IL6 and CRIM1 in thiopurine intolerance due to hematological toxicity in leukemic patients with wild-type NUDT15 and TPMT. Sci Rep 11, 9676 (2021). https://doi.org/10.1038/s41598-021-88963-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88963-5
This article is cited by
-
An intron SNP rs2069837 in IL-6 is associated with osteonecrosis of the femoral head development
BMC Medical Genomics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.