Abstract
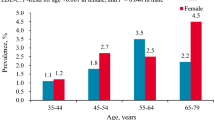
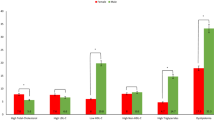
Dyslipidemia, a major risk factor for cardiovascular diseases, has become a global issue. Due to the variations in the prevalence of dyslipidemia, this study aimed to evaluate dyslipidemia and its associated factors in women of the Bandare-Kong Cohort Study (BKNCD). This study was conducted on women from the population-based BKNCD, as part of the Prospective Epidemiological Research Studies in IrAN (PERSIAN). Sociodemographic data, medical history, and anthropometric indices were collected. Dyslipidemia was defined as any lipid abnormality including low-density lipoprotein (LDL) ≥ 160, total cholesterol (TC) ≥ 240, high-density lipoprotein (HDL) < 40, or triglyceride > 200 mg/dl. From the 2223 women in this study (mean age: 48.28 ± 9.26 years), dyslipidemia was observed in 851 (38.3%). High TC was the most common lipid abnormality (18.5%) followed by high LDL (17.7%). Dyslipidemia was most prevalent among women aged 55–70 years, the married, those with < 6 years of education, the unemployed, the overweight or obese, with low socioeconomic status, diabetes, hypertension, and high waist circumference, those using the hookah and living in urban areas. Logistic regression revealed that women with high waist-to-hip ratio (WHR) (OR = 2.22, 95% CI 1.60–3.08), those aged 45–54 years (OR = 1.34, 95% CI 1.07–1.68) and 55–70 years (OR = 1.33, 95% CI 1.03–1.72), and those living in urban areas (OR = 1.35, 95% CI 1.05–1.73) were at significantly increased risk of dyslipidemia. In addition, the results were confirmed using deep neural network models. Dyslipidemia was highly prevalent in Iranian women in the southern coastal region. Central obesity, age over 45 years, and living in urban areas appear to be relatively significant risk factors for dyslipidemia among women.
Similar content being viewed by others
Introduction
Dyslipidemia, a disorder of lipid metabolism, is clinically defined as the presence of one of the following abnormalities: elevated plasma triglycerides (TG), elevated total cholesterol (TC), high levels of low-density lipoprotein (LDL), and decreased high-density lipoprotein (HDL)1. With the increasing prevalence of dyslipidemia, mostly due to adverse changes in lifestyle including dietary changes, the more sedentary lifestyle, and reduced physical activity, it has become a global public health issue2. There is substantial evidence that dyslipidemia is associated with an increased risk of cardiovascular disease (CVD)3. According to the World Health Organization (WHO) estimates, dyslipidemia, especially high TC, is responsible for 2.6 million deaths annually and 29.7 million disability-adjusted life years (DALYS) worldwide4.
The prevalence of dyslipidemia varies in different regions, with hypercholesterolemia ranging from 22.6% to 54% across Africa, South East Asia, Europe, and America4. Studies in Iran have also reported the prevalence of dyslipidemia: the prevalence of hypertriglyceridemia, hypercholesterolemia, high LDL, and low HDL ranged 14–40.6%, 14–61%, 13.4–45.5%, and 5–73%, respectively5,6,7,8. In addition, it has been demonstrated in many parts of the world including Iran, that dyslipidemia can be influenced by numerous factors including socio-economic status, level of fat intake, obesity, and gender9,10,11. Dyslipidemia is a modifiable risk factor for the development of type 2 diabetes, atherosclerosis, CVD, and stroke; early effective management of patients with dyslipidemia can decrease the incidence and the burden of the above-mentioned conditions12,13,14.
Metabolism in women can be affected by alterations in hormonal levels throughout their lives, in either the premenopausal or postmenopausal period15. It has been reported that serum TC levels in women increases with age; however, this occurs more gradually compared to men10. Yet, it increases at a higher rate after the age of 44 years, probably as a result of the loss of estrogen in the postmenopausal period and decreased activity of LDL receptors16.
With regard to regional differences in the prevalence of dyslipidemia and gender variations in this respect, and taken into consideration the modifiable nature of dyslipidemia for prevention and control of the disease burden, as well as specific hormonal effects in females, it would be extremely important to be aware of the prevalence and potential influencing factors of this condition in women. Indeed, there is no information about the women who live in the southern coastal of Iran, thus we aimed to evaluate dyslipidemia and its associated factors in women of the PERSIAN Bandare-Kong Cohort Study.
Methods
Participants
We evaluated the women of the PERSIAN Bandare Kong Cohort Study, a prospective, population-based cohort study in Bandare-Kong, Iran, which has been previously described in detail17. This cohort study includes 2334 women aged 35–70 years, recruited between November 17, 2016, and November 22, 2018, from Hormozgan province, southern Iran, as part of the Prospective Epidemiological Research Studies in IrAN (PERSIAN). Written informed consent was obtained from all the participants. After the exclusion of pregnant women, those taking lipid-lowering medications, and incomplete records, 2223 women were included in the final analysis. All methods were carried out in accordance with relevant guidelines and regulations.
Study design
The BKNCD cohort study is part of the PERSIAN (Prospective Epidemiological Research Studies in IrAN) Cohort. Sociodemographic data were collected using a face-to-face interview by trained interviewers. Age, education, marital status, place of residence, and hookah use were recorded. Data regarding occupation, type of residence ownership, home size/area, trips, and other possessions including cars, computers, dishwashers, etc. were used to determine the socioeconomic status (SES) by means of principal component analysis. Daily calorie intake was calculated using daily ingested foods reported by the participants and their calorie content. Daily and weekly energy expenditure were determined using the metabolic equivalent of tasks (METs).
Weight was measured with a digital scale (measurement accuracy of 0.5 kg), with subjects in minimum clothing and without shoes. Height was measured with subjects standing shoeless and with their shoulders set normally. Waist circumference (WC) was measured twice for each participant and the average was recorded. WC was measured at the end of several consecutive natural breaths, at a level parallel to the floor, the midpoint between the top of the iliac crest and the inferior margin of the last palpable rib in the midaxillary line. Hip circumference (HC) was measured at the largest circumference of the buttocks, at a parallel level to the floor. All measurements were done with the same stretch-resistant tape to the nearest 0.5 cm. Subjects were standing upright during the measurements, with arms relaxed at the side, feet evenly spread apart and body weight evenly distributed. Waist-to-hip ratio (WHR) was calculated as WC divided by HC to the nearest 0.01. WHO cut-off for substantially increased risk of metabolic complications in women are: WC > 88 cm and WHR ≥ 0.85. According to the study by Azizi et al. the cut-off value of WC for the Iranian population is WC ≥ 95 cm for both men and women18. No WHR cut-off has been established for the Iranian population; therefore, the WHO cut-off for WHR was used.
BMI was calculated as weight in kilograms divided by the square of the person’s height in meters to the nearest 0.01. Participants were categorized into two groups: BMI < 25 kg/m2 and BMI ≥ 25 kg/m2.
Blood pressure (BP) was measured using a standard mercury sphygmomanometer after 5 min of rest with an appropriate cuff size for the upper-arm circumference, in the seated position, with feet on the floor, and arm supported at heart level. The average of two measurements made at least 5 min apart was used for analysis. Hypertension was defined as sustained blood pressure ≥ 140/90 mmHg or treatment with anti-hypertensive medications. Elevated values (≥ 140/90 mmHg) were confirmed on a separate day.
Venous blood samples were collected following overnight 8-h fasting and fasting plasma glucose (FPG) was measured. Plasma glucose measurements were done using the glucose oxidase method. According to the American Diabetes Association (ADA) criteria, diabetes was defined as an FPG ≥ 126 mg/dl, confirmed in a repeat test, or treatment with glucose-lowering agents. Venous blood samples were collected on another day following overnight 12-h fasting and TC, TG, LDL, and HDL were measured for each participant using the enzymatic method. LDL < 100 mg/dl was considered optimal, 100–129 mg/dl near or above optimal, 130–159 borderline high, 160–189 high, and ≥ 190 very high. TC < 200 mg/dl was considered desirable, 200–239 borderline high, and ≥ 240 high. Low HDL was defined as HDL < 50 mg/dl in women and HDL ≥ 60 mg/dl was considered high. TG < 150 mg/dl was considered normal, 150–199 borderline high, 200–499 high, and ≥ 500 very high. Based on the following criteria, dyslipidemia was defined as the presence of one or more of the following disorders19:
-
1.
TC ≥ 240 mg/dl
-
2.
TG > 200 mg/dl
-
3.
LDL ≥ 160 mg/dl
-
4.
HDL < 40 mg/dl (in women)
Data analysis
The Statistical Package for the Social Sciences (SPSS) software (version 25.0, Armonk, NY: IBM Corp.) was used for data analysis. Mean, standard deviation, frequency, and percentages were used to describe the results. The binary logistic regression model was used to examine the correlation of dyslipidemia and its components with the associated factors. Qualitative variables with P-values ≤ 0.2 in single correlations by the logistic regression were included in the general model. Area under the receiver operating characteristic (AUROC) curve was calculated to determine the prediction performance of the logistic regression model20. Linear regression was used to determine the predictive power of associated factors on lipid profile components. All potential predictive variables of quantitative nature were included in the linear regression model. P-values of equal to or less than 0.05 were regarded as statistically significant.
The deep neural network model (deep learning) was used for complementary analysis. Currently, different types of deep learning analysis are widely used whether in image analysis or discrete value analysis such as patients’ information. The analysis of tumor detection and classification in Alzheimer’s disease are two example of MRI image analysis that use deep convolutional neural networks (CNN)21. Based on the information and desired analysis, different deep learning methods can be used in a model and deep feed forward neural network is used for our approach. The model consists of a deep feed forward neural network with 9 layers using Python programming. Based on common practice, we split the data into 70% as a training and 30% as a testing set. The methods of calculating the accuracy, precision, recall, and classification error are shown in equations. Precision = (TP)/(TP + FP). In this equation, true positive (TP) represents transactions that were positive and classified as positive. True negative (TN) represents the number of transactions that were negative and classified as positive. False positive (FP) also indicates the number of transactions that were positive and classified as negative. Finally, FN (False Negative) shows transactions that were negative and classified as negative. The equation to the validity and recall assessment is as follows: Recall = (TP)/(TP + FN)22. The F1 score is the harmonic mean of the precision and recall. The highest possible value of an F-score is 1.0, indicating perfect precision and recall, and the lowest possible value is zero, when either the precision or the recall is zero.
Ethics approval and consent to participate
The cohort study was given ethical approval by the Ethics Committee of Hormozgan University of Medical Sciences.
Results
From the 2223 women evaluated in this study (with the mean age of 48.28 ± 9.26), dyslipidemia was observed in 851 (38.3%). The mean values of TC, TG, HDL, and LDL were 204.72 ± 42.39 mg/dl, 127.19 ± 68.73 mg/dl, 50.37 ± 10.83 mg/dl, and 129.16 ± 35.52 mg/dl, respectively. High TC was the most common lipid abnormality (18.5%) followed by high LDL (17.7%), low HDL (14.8%), and high TG (10.8%). One, two, three, and four abnormal lipid components were observed in 18.4%, 16.5%, 3.1%, and 0.3%, respectively, while 61.7% of the participants had no lipid abnormalities. High TG (individually, with other components being normal), high TC, low HDL, and high LDL were exclusively seen in 3.5%, 1.9%, 10.8%, and 2.3%, respectively. In general, most participants were aged 35–44 years (31.5%). They were mostly married (96.8%), and had < 6 years of education (71.9%). Most of them lived in urban areas (84.3%), had low socioeconomic status (44%), and were unemployed (84.8%). Moreover, 13.5% used hookah. With regard to medical history and anthropometric indices, 20.9% had diabetes, 30% had hypertension, most participants had BMI ≥ 25 kg/m2 (69.5%), 87.4% had high WHR, 76.4% had high WC based on the WHO cut-off, and 53.6% based on the Iranian-specific cut-off.
The prevalence of dyslipidemia and individual lipid abnormalities are demonstrated in Table 1. The prevalence of dyslipidemia, high TC, and high LDL was the highest in women aged 55–70 years, while high TG and low HDL were most prevalent in those aged 45–54 and 35–44 years, respectively. Except for high TG which was more prevalent among single women, dyslipidemia and all other lipid abnormalities were highest in married participants. Aside from low HDL, which was the highest in those with ≥ 6 years of education, dyslipidemia and all other lipid abnormalities were the highest in those with < 6 years of education. Apart from high TG and high TC, most prevalent in those living in rural areas, dyslipidemia and other lipid abnormalities were most prevalent in those living in urban areas. Details of lipid abnormalities are shown in Table 2.
Logistic regression revealed that high WHR was consistently correlated with dyslipidemia and all of its components. Women living in urban areas were at significantly increased risk of dyslipidemia and low HDL compared to those living in rural areas, while ≥ 6 years of education was protective against high LDL. Age over 45 years was associated with dyslipidemia and high TC, while it was protective against low HDL. Women with diabetes and hypertension were at significantly increased risk of high TG; however, surprisingly hookah was protective against high TC and high LDL. Also, high socioeconomic status was protective regarding low HDL (Table 3).
The AUROC curve of the logistic regression model for prediction of dyslipidemia was 0.607 (95% CI 0.583–0.630) which shows the relatively acceptable performance of this model (61%) (Fig. 1).
Linear regression ("enter" method) showed that every 1 kg/m2 increase in BMI led to 2.51, 1.56, and 0.94 mg/dl increase in TG, TC, and LDL, respectively. Every 1 mg/dl increase in FPG and every 1 mmHg increase in systolic blood pressure (SBP) led to 0.22 and 0.41 mg/dl increase in TG, respectively. Every 1 year advance in age and 1 mmHg elevation in diastolic blood pressure (DBP) led to 0.59 and 0.31 mg/dl increase in TC, respectively. Weight, HC, and WHR were negatively correlated with HDL. Age was also positively associated with LDL. Besides, altogether age, years of education, weight, WC, HC, WHR, BMI, FPG, SBP, DBP, daily calorie intake, and weekly METs could predict 14%, 6%, 7%, and 3% of the variance of TG, TC, HDL, and LDL, respectively (Table 4).
The group correlation between independent and effective variables with dyslipidemia (dependent variable) was evaluated using deep learning. It is possible to completely assess the singular correlation between the mentioned variables through statistical analyses that have been performed previously. The model consists of a deep learning feed forward network with 9 layers as follows:
Model: "Sequential".
Layer (type) | Output shape | Parameters |
|---|---|---|
dense (Dense) | (None, 64) | 4032 |
dense_1 (Dense) | (None, 32) | 2080 |
dense_2 (Dense) | (None, 64) | 2112 |
dense_3 (Dense) | (None, 32) | 2080 |
dense_4 (Dense) | (None, 64) | 2112 |
dropout (Dropout) | (None, 64) | 0 |
batch_normalization | (None, 64) | 256 |
dense_5 (Dense) | (None, 2) | 130 |
Total parameters: 12,802, Trainable parameters: 12,674, Non-trainable parameters: 128.
As shown above, the model consists of 9 layers including the input layer, and 12,802 parameters, of which 12,674 parameters were trainable. In each layer, the number of neural network nodes and parameters of that layer has been expressed. The network with variety of variables was evaluated. We reached the best performance in accuracy and predictability for the following variables (age groups ≥ 45 years, urban residence, and high WHR). The resulting confusion table is based on 304 negative samples and 244 positive samples as follows:
Decision | |||
|---|---|---|---|
No dyslipidemia | Dyslipidemia | ||
Target | No dyslipidemia | 201 | 103 |
Dyslipidemia | 86 | 158 | |
The overall precision of the model is equal to 0.65% in the considered range.
Class | Precision | Recall | F1-score | Support |
|---|---|---|---|---|
No dyslipidemia | 0.7 | 0.66 | 0.68 | 304 |
Dyslipidemia | 0.61 | 0.65 | 0.63 | 244 |
The average performance of the model is:
Decision | |||
|---|---|---|---|
No dyslipidemia | Dyslipidemia | ||
Target | No dyslipidemia | 261 | 141 |
Dyslipidemia | 158 | 107 | |
and the mean's precision is 0.55%.
Class | Precision | Recall | F1-score | Support |
|---|---|---|---|---|
No dyslipidemia | 0.62 | 0.65 | 0.64 | 402 |
Dyslipidemia | 0.43 | 0.4 | 0.42 | 265 |
Therefore, the model confirmed 45% of the cases in the target range with 65% of precision. This means a definite confirmation of 35% of cases in the database. The model also confirms 40% of cases in the entire database with 55% precision. This means a definite confirmation of 22% of cases in the database. By comparing the two results, it could be concluded that the risk of dyslipidemia is higher in those older than 45 years, urban dwellers, and individuals with central obesity.
Discussion
The primary finding of the current study was the high prevalence of dyslipidemia in women aged 35–70 years of the PERSIAN Bandare Kong Cohort Study, with 38.3% of the study population having at least one lipid abnormality. High TC was the most common, (18.5%) followed by high LDL (17.7%), low HDL (14.8%), and high TG (10.8%).
Prevalence of dyslipidemia in women was 87.7% in Najafipour et al.'s study23, 61.3% in the study by Ebrahimi et al.24, 85.1% in Latifi et al.'s study25, and 37.6% among Chinese women2. In a systematic review and meta-analysis on the prevalence of dyslipidemia in published articles in Iran until September 2011, hypercholesterolemia, low HDL, and high LDL were more prevalent in women compared to men26. Another study showed that the prevalence of hypertriglyceridemia and hypercholesterolemia were 33.2% and 45.4% among females27. The corresponding percentages were 41% and 23% in Japanese women aged 25–64 years28, 25% and 37.2% in Turkish adults29, 24.1% and 30.6% in Najafipour et al.'s study23, and 65.1% and 47.5% in Latifi et al.'s study25. The variety of the prevalence of dyslipidemia and its individual components across different studies can be explained by demographic, socioeconomic, and anthropometric features of study populations which will be discussed in detail later on.
The results of this study showed that the prevalence of dyslipidemia steadily increased with age in women. A similar trend was observed in Ebrahimi et al.'s study24. Nonetheless, we found that the odds of dyslipidemia in women aged 45–54 and 55–70 years were similar based on the logistic regression analysis. Yet, other studies in different parts of the world have shown that the risk of different types of dyslipidemia increases with age in both men and women29,30,31.
We found no correlation between marital status and dyslipidemia or any of its components, which was in line with the findings of Ebrahimi et al.24. While high TG was more prevalent among single women, dyslipidemia and all other lipid abnormalities were highest in married participants in our study. Whereas, aside from low HDL, other lipid abnormalities were higher in married and widowed individuals compared to singles in the study by Erem et al.29.
According to the findings of the current study, ≥ 6 years of education was protective against high LDL; however, level of education was not associated with dyslipidemia and other lipid abnormalities. Quite similarly, dyslipidemia was not influenced by level of education in a study conducted in India11. In addition, this was partially consistent with the results of Ebrahimi et al.'s study, in which no relationship was found between the risk of developing different types of dyslipidemia and the level of education24. On the contrary, Erem et al. in their study to estimate the prevalence of dyslipidemia and associated factors among Turkish adults, demonstrated that the risk of dyslipidemia was higher in those with lower education level. They justified their findings by higher exposure to risk factors such as poor eating habits and working conditions, difficulty to access health services, and stress in those with low level of education29. Of note, the findings of the above-mentioned studies were with respect to both men and women. Results can be different when only women are concerned.
We found that women living in living in rural areas were at significantly increased risk of dyslipidemia and low HDL compared to those living in urban areas. On the contrary, the odds of hypertriglyceridemia and hypercholesterolemia, although insignificant, was lower in women living in urban areas. Similarly, Cui et al. demonstrated that the prevalence of hypercholesterolemia was higher in rural areas compared to urban areas for women28. Contrarily, Tripathy et al. demonstrated that living in rural areas increased the risk of dyslipidemia and high TC32. The reason for these inconsistencies may be the consumption of fat-rich foods such as high-fat dairy by individuals living in rural areas in the two studies.
Over the past decade, there has been a decline in consumption of traditional foods, while use of high-fat, high-calorie, low-fiber, and processed foods has increased. This unhealthy diet together with insufficient physical activity, are risk factors for obesity and hypertriglyceridemia33,34,35. Among the participants of the current study, 69.5% were overweight or obese. Overweight and obesity were not correlated with dyslipidemia or individual lipid abnormalities. Among the anthropometric indices, high WHR was the best predictor of dyslipidemia and all of its components. Obesity has been reported to be associated with hypertriglyceridemia in many studies8, 11, 29,30,31, 36, 37. It should be noted that contrary to our findings, obesity has been proposed as a risk for hypercholesterolemia in some studies8, 11, 29, 36.
The ROC curve predicted the logistic regression model's performance once with all the variables included in the model and then with the significant factors (high WHR, age over 45 years, and living in urban areas). The AUROC of the model for significant factors was 0.61. Besides, based on our findings in the deep learning models, the accuracy was 65%. The accuracy of the prediction model is lower than our expectation which might be explained by the effect of unknown variables that have not been measured in the cohort study.
The odds of hypertriglyceridemia was significantly higher in women with hypertension or diabetes in our study, while neither dyslipidemia nor any other components were associated with the two comorbidities. This was in agreement with the findings of Ebrahimi et al.; however, they also reported a significant correlation between high blood pressure and dyslipidemia24. Tabrizi et al. reported similar results38. Despite comparable findings regarding the association between hypertension and hypertriglyceridemia in a study in India, dyslipidemia and other lipid abnormalities were also significantly correlated in this study32. Lipids are the major components of atherosclerotic plaques which are associated with hypertension through a decrease in the vascular lumen diameter and an increase in the arterial wall resistance; moreover, dyslipidemia can cause endothelial damage leading to the disturbance of the physiological vasomotor activity39. As for the relationship between dyslipidemia and diabetes, the effect of insulin resistance on key enzymes involved in lipid metabolism has been established resulting in diabetic dyslipidemia consisting of a triad of increased LDL, decreased HDL, and raised triglycerides40.
One limitation of the current study was that although, lipid-lowering medications were taken into account, some women with diabetes may have failed to indicate that they were taking these agents, which resulted in contradictory findings regarding the relationship between dyslipidemia or its components with diabetes. Another limitation was the assessment of physical activity which was reported in METs. The positive effect of physical activity on serum lipids, plasma glucose, and many other CVD risk factors has been previously established; therefore, the increase in TC and LDL with higher weekly METs observed in the current study can in part be due to inaccurate evaluation of physical activity. One more limitation was the daily calorie intake that was not subdivided based on specific foods. Calorie content of fat-rich foods would have been more valuable in the assessment of the correlation between lipid abnormalities and daily calorie intake.
Conclusions
Dyslipidemia was highly prevalent in women of the PERSIAN Bandare Kong Cohort Study. High TC was the most common, and high TG the least common lipid abnormalities in this population. High WHR put women aged 35–70 years at high risk of dyslipidemia and all of its components and appears to be the best predictive anthropometric index with regard to lipid abnormalities. Women over 45 years were at highest risk of developing lipid abnormalities compared to other age groups. Living in urban areas positively influenced the lipid profile of women, while marital status and employment had no effect on it. Except for the positive effect of ≥ 6 years of education on high LDL, level of education did not affect lipid abnormalities. Although the odds of high TG was higher in those with hypertension or diabetes. The significance of hookah use for lipid abnormalities was paradoxical. These findings should be taken into consideration in the preparation of future management and prevention guidelines designated for this specific population. Future studies are needed to identify unknown variables in the prediction of dyslipidemia.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADA:
-
American Diabetes Association
- ATP III:
-
Adult Treatment Panel III
- AUROC:
-
Area under the receiver operating characteristic (curve)
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DALYS:
-
Disability-adjusted life years
- DBP:
-
Diastolic blood pressure
- FPG:
-
Fasting plasma glucose
- HC:
-
Hip circumference
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- MET:
-
Metabolic equivalent of task
- OR:
-
Odds ratio
- PERSIAN:
-
Prospective Epidemiological Research Studies in IrAN
- ROC:
-
Receiver operating characteristic
- SBP:
-
Systolic blood pressure
- SES:
-
Socioeconomic status
- SPSS:
-
Statistical Package for the Social Sciences
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- WC:
-
Waist circumference
- WHO:
-
World Health Organization
- WHR:
-
Waist-to-hip ratio
References
Stone, N. J. et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 63(25 Part B), 2889–934 (2014).
Qi, L. et al. Prevalence and risk factors associated with dyslipidemia in Chongqing, China. Int. J. Environ. Res. Public Health. 12(10), 13455–13465 (2015).
Stevens, W. et al. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv. Res. 16(1), 175 (2016).
World Health Organization. Global status report on noncommunicable diseases 2014 (World Health Organization, 2014).
Asgari, F., Mirzazadeh, A. & Heidaria, H. Iran-non-communicable diseases risk factors surveillance-Data book for 2007 1–82 (Chakameh Ava Group, 2009).
Hatmi, Z. N., Tahvildari, S., Motlag, A. G. & Kashani, A. S. Prevalence of coronary artery disease risk factors in Iran: a population based survey. BMC Cardiovasc. Disord. 7(1), 32 (2007).
Sharifi, F., Mousavinasab, S. N., Soruri, R., Saeini, M. & Dinmohammadi, M. High prevalence of low high-density lipoprotein cholesterol concentrations and other dyslipidemic phenotypes in an Iranian population. Metab. Syndr. Related Disord. 6(3), 187–195 (2008).
Yarahmadi, S. H., Etemad, K., Hazaveh, A. R. M. & Azhang, N. Urbanization and non-communicable risk factors in the capital city of 6 big provinces of Iran. Iran. J. Public Health 42(Supple1), 113 (2013).
Aguilar-Salinas, C. A. et al. Prevalence of dyslipidemias in the Mexican national health and nutrition survey 2006. Salud Publica Mex. 52, S44–S53 (2010).
Azizi, F. et al. Serum lipid levels in an Iranian adults population: Tehran Lipid and Glucose Study. Eur. J. Epidemiol. 18(4), 311–319 (2003).
Guptha, S. et al. Cholesterol lipoproteins and prevalence of dyslipidemias in urban Asian Indians: a cross sectional study. Indian Heart J. 66(3), 280–288 (2014).
Han, X., Fox, D. S., Chu, M., Dougherty, J. S. & McCombs, J. Primary prevention using cholesterol-lowering medications in patients meeting new treatment guidelines: a retrospective cohort analysis. J. Manag. Care Spec. Pharm. 24(11), 1078–1085 (2018).
Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in, 20, 536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360, 7–22 (2002).
Jayarama, N., Reddy, M. & Lakshmaiah, V. Prevalence and pattern of dyslipidemia in type 2 diabetes mellitus patients in a rural tertiary care centre, southern India. Glob. J. Med. Public Health 1, 24–28 (2012).
William, B. et al. Dyslipidemia as a risk factor for developing hypertension and cardiovascular disease in females of reproductive age. J. Nat. Appl. Sci. Pak. 1(2), 139–147 (2019).
Grundy, S. M. Multifactorial etiology of hypercholesterolemia: Implications for prevention of coronary heart disease. Arterioscler. Thromb. J. Vasc. Biol. 11(6), 1619–35 (1991).
Poustchi, H. et al. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): rationale, objectives, and design. Am. J. Epidemiol. 187(4), 647–655 (2018).
Azizi, F., Khalili, D., Aghajani, H., Esteghamati, A. R., Hosseinpanah, F., Delavari, A. R., et al. Appropriate waist circumference cut-off points among Iranian adults: the first report of the Iranian National Committee of Obesity. 2010.
Moradinazar, M. et al. Association between dyslipidemia and blood lipids concentration with smoking habits in the Kurdish population of Iran. BMC Public Health 20, 1–10 (2020).
Yu, H. et al. LEPR hypomethylation is significantly associated with gastric cancer in males. Exp. Mol. Pathol. 116, 104493 (2020).
Liu, M. et al. A multi-model deep convolutional neural network for automatic hippocampus segmentation and classification in Alzheimer’s disease. Neuroimage 208, 116459 (2020).
Farashah, M. V., Etebarian, A., Azmi, R. & Dastjerdi, R. E. An analytics model for TelecoVAS customers’ basket clustering using ensemble learning approach. J. Big Data 8, 1–24 (2020).
Najafipour, H. et al. Prevalence of dyslipidemia and its association with other coronary artery disease risk factors among urban population in Southeast of Iran: results of the Kerman coronary artery disease risk factors study (KERCADRS). J. Diabetes Metabol Disord. 15(1), 49 (2016).
Ebrahimi, H., Emamian, M. H., Hashemi, H. & Fotouhi, A. Dyslipidemia and its risk factors among urban middle-aged Iranians: a population-based study. Diabetes Metab. Syndr. Clin. Res. Rev. 10(3), 149–156 (2016).
Latifi, S. M., Moradi, L., Shahbazian, H. & Aleali, A. M. A study of the prevalence of dyslipidemia among the adult population of Ahvaz. Iran. Diabetes Metab. Syndr. Clin. Res. Rev. 10(4), 190–193 (2016).
Tabatabaei-Malazy, O. et al. Prevalence of dyslipidemia in Iran: a systematic review and meta-analysis study. Int. J. Prev. Med. 5(4), 373 (2014).
Esteghamati, A. et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health 9(1), 167 (2009).
Cui, M., Chiang, C., Cui, R., Honjo, K., Yatsuya, H., Watson, B. M., et al. Prevalence and correlates of dyslipidemia among men and women in Palau: findings of the Palau STEPS survey 2011–2013. J. Epidemiol. JE20170127 (2018).
Erem, C., Hacihasanoglu, A., Deger, O., Kocak, M. & Topbas, M. Prevalence of dyslipidemia and associated risk factors among Turkish adults: Trabzon lipid study. Endocrine 34(1–3), 36–51 (2008).
Khader, Y. S., Batieha, A., El-Khateeb, M., Al Omari, M. & Ajlouni, K. Prevalence of dyslipidemia and its associated factors among Jordanian adults. J. Clin. Lipidol. 4(1), 53–58 (2010).
Crawford, A. G. et al. Prevalence of obesity, type II diabetes mellitus, hyperlipidemia, and hypertension in the United States: findings from the GE Centricity Electronic Medical Record database. Popul. Health Manag. 13(3), 151–161 (2010).
Tripathy, J. P. et al. Burden and risk factors of dyslipidemia-results from a STEPS survey in Punjab India. Diabetes Metab. Synd. Clin. Res. Rev. 11, S21–S27 (2017).
World Health Organisation. Facts on obesity. Retrieved February 1:2016.
Mozaffarian, D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133(2), 187–225 (2016).
Hata, Y. & Nakajima, K. Life-style and serum lipids and lipoproteins. J. Atheroscler. Thromb. 7(4), 177–197 (2000).
Deng, B., Luo, T., Huang, Y., Shen, T. & Ma, J. Prevalence and determinants of hyperlipidemia in moderate altitude areas of the Yunnan-Kweichow plateau in Southwestern China. High Alt. Med. Biol. 13(1), 13–21 (2012).
Montano, G. T., Witherell, R., Mar, A., Szpunar, S. M. & Anne, P. Predictors of screening for hyperlipidemia in an urban pediatric tertiary care center. Clin. Pediatr. 54(3), 244–248 (2015).
Tabrizi, J. S. et al. Prevalence of dyslipidemia in urban and rural areas of the Northwest of Iran: the sociodemographic, dietary and psychological determinants. Iran. J. Public Health 48(5), 925 (2019).
Wong, N. D., Lopez, V., Tang, S. & Williams, G. R. Prevalence, treatment, and control of combined hypertension and hypercholesterolemia in the United States. Am. J. Cardiol. 98(2), 204–208 (2006).
Taskinen, M.-R. Diabetic dyslipidemia. Atheroscler. Suppl. 3(1), 47–51 (2002).
Acknowledgements
BKNCD is a part of PERSIAN national cohort and we would like to thank Professor Reza Malekzadeh, Deputy of Research and Technology at the Ministry of Health and Medical Education of Iran and Director of the PERSIAN cohort, and also Dr. Hossein Poustchi, Executive Director of the PERSIAN cohort and Azim Nejatizadeh Director of BKNCD for all their supports during design and running of BKNCD. The Iranian Ministry of Health and Medical Education has contributed to the funding used in the PERSIAN Cohort through Grant Number 700/534.
Funding
The Iranian Ministry of Health and Medical Education has contributed to the funding used in the PERSIAN Cohort through Grant Number 700/534.
Author information
Authors and Affiliations
Contributions
M.N. designed the study and was a major contributor in writing the manuscript. M.K.E. was consulted on the possible associated factors to be taken into account and wrote the manuscript. H.Y. performed the statistical analysis. M.V.F. & B.M. did the deep learning model analysis. M.K.A. interpreted the analyzed data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nikparvar, M., Khaladeh, M., Yousefi, H. et al. Dyslipidemia and its associated factors in southern Iranian women, Bandare-Kong Cohort study, a cross-sectional survey. Sci Rep 11, 9125 (2021). https://doi.org/10.1038/s41598-021-88680-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88680-z
This article is cited by
-
Association between serum vitamin D levels and lipid profiles: a cross-sectional analysis
Scientific Reports (2023)
-
Prevalence of dyslipidemia and its association with opium consumption in the Rafsanjan cohort study
Scientific Reports (2022)
-
Cross-sectional study of passive opiate smoking in relation to stroke and some of stroke attributable risk factors in women
Scientific Reports (2022)
-
Prediction of hypercholesterolemia using machine learning techniques
Journal of Diabetes & Metabolic Disorders (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.