Abstract
We analyzed database from the Taiwan National Health Insurance to investigate whether primary aldosteronism (PA) increases the risk of bladder stones. This retrospective nationwide population-based cohort study during the period of 1998–2011 compared patients with and without PA extracted by propensity score matching. Cox proportional hazard models and competing death risk model were used to estimate the hazard ratios (HRs), sub-hazard ratios (SHRs) and corresponding 95% confidence intervals (CIs). There were 3442 patients with PA and 3442 patients without PA. The incidence rate of bladder stones was 5.36 and 3.76 per 1000 person-years for both groups, respectively. In adjusted Cox hazard proportional regression models, the HR of bladder stones was 1.68 (95% CI 1.20–2.34) for patients with PA compared to individuals without PA. Considering the competing risk of death, the SHR of bladder stones still indicates a higher risk for PA than a comparison cohort (SHR, 1.79; 95% CI 1.30–2.44). PA, age, sex, and fracture number were the variables significantly contributing to the formation of bladder stones. In conclusion, PA is significantly associated with risk of bladder stones.
Similar content being viewed by others
Introduction
Primary aldosteronism (PA), with aldosterone hypersecretion, was found in 5–13% of patients with resistant hypertension1. In addition to its detrimental effect on the cardiovascular system, it is suggested that PA could adversely affect the process of mineral bone homeostasis. For example, an increased risk of osteoporosis and bone fractures was demonstrated in PA by the following mechanism: enhanced calcium excretion through renal tubules in urinary and intestinal cells. Meanwhile, a remarkably higher secondary secretion of parathyroid hormone is occasionally observed concomitantly with PA2. Additionally, other systemic effects that result from PA were reported previously, such as increased incidence of new-onset diabetes mellitus and metabolic syndrome3,4.
There is a 7–13% lifetime risk of developing nephrolithiasis; this results in not only significant morbidity but also substantial economic costs5. The stones in urolithiasis are comprised of calcium oxalate or phosphate compounds. In addition to traditional risk factors such as age, sex, race, geography, and high body mass index, other factors, including hyperparathyroidism, osteoporosis, and diabetes mellitus are highly likely to be associated with the development of nephrolithiasis6.
A previous study suggests that recurrent calcium nephrolithiasis was likely associated with PA through increased hypercalciuria and hypocitraturia and that the status of hypersecretion of urinary calcium can be attenuated after adrenalectomy7,8. In addition, excretion of acidic urine resulting from higher aldosterone levels might also promote formation of urate stones9.
Although bladder stones are uncommon in nephrolithiasis (estimated at 5%), such calculi are reported to result in multiple major complications such as acute urinary retention, dysuria, and even acute renal failure10. Bladder stones are not only the cause of several upper urinary tract stone diseases, but also urinary stasis caused by bladder outlet obstruction or benign prostate hyperplasia11,12. Some evidence suggests that aldosterone plays a key role in urinary bladder function. Aldosterone could affect calcium-activated potassium (BK) channels, which are essential in regulating the function of urinary bladder smooth muscle13 by potassium depletion. Therefore, it is reasonable to suppose that PA is likely to be associated with urinary stone risk.
To the present, data regarding the risk of developing bladder stones in PA are still lacking. The present study is devoted to investigating the association of bladder stones and PA in a national cohort with a long observational period.
Results
Table 1 shows the PA and comparison cohort characteristics. Median age was 49.4 and 52.6 years for the PA and comparison cohorts, respectively (SMD, 0.04). In the PA and comparison cohorts, 46.5% and 58.3% of the patients were men, respectively (SMD, 0.24). The median frequency of medical visits was 0.54 and 0.62 for the PA and comparison cohorts, respectively (SMD, 0.08). Except for fracture, there was no difference in comorbidity percentage between the PA and comparison cohort.
Table 2 demonstrated the incidence, HRs, and SHRs of bladder stones between the PA and comparison cohort. The overall bladder stone incidences were 5.36 and 3.76 per 1000 person-years for the PA and comparison cohorts, respectively. Figure 1 shows the incidence rate of bladder stones was greater for the PA cohort than the comparison cohort (log-rank test, P = 0.02). After adjusting for age, sex, and comorbidities, the HR of bladder stones was 1.68 (95% CI 1.20–2.34) for patients with PA compared to individuals without PA. Relative to individuals without PA, the HRs for bladder stones was 1.86 (95% CI 1.11–3.10), 1.18 (95% CI 0.64–2.16), and 2.07 (95% CI 1.05–4.07) for patients with PA who were 20–49 years of age, 50–64 years of age, and ≥ 65 years of age, respectively. Only in men, patients with PA were significantly associated with a higher risk of bladder stone development than those of the comparison cohort (HR 1.65; 95% CI 1.09–2.49).
Table 2 also included the competing risk of death; the SHR of bladder stones still indicated a higher risk for the PA and comparison cohorts (SHR, 1.79; 95% CI 1.30–2.44). In study subjects aged ≥ 65 years, the PA cohort was associated with a 2.38-fold higher risk of bladder stone development than the comparison cohort (SHR, 2.38; 95% CI 1.20–4.72). Compared to patients without PA, the SHRs of bladder stones were 1.83 (95% CI 1.07–3.14) and 1.65 (95% CI 1.09–2.49) for patients with PA in women and in men, respectively. The risk of bladder stones was significantly higher for PA patients than comparisons (SHR = 2.12, 95% CI 1.27–3.57) to individuals without any comorbidity.
Table 3 shows the results of univariable and multivariable competing risk between the PA and comparison cohorts. The significant results for single variable analysis were PA (SHR, 1.56; 95% CI 1.15–2.13), sex (women vs men SHR, 1.89; 95% CI 1.37–2.59), age (SHR, 1.02; 95% CI 1.02–1.03), and fracture (SHR, 1.65; 95% CI 1.09–2.48). The multivariable model, which involved PA, age, sex, and fracture, showed that all variables were significantly at higher risk of developing bladder stones.
A sensitivity analysis was performed with PA versus a non-PA cohort by 1:4 frequency matching based on age, sex, and all comorbidities (Supplementary Table 1). Supplementary Table 2 demonstrated the incidence, HRs, and SHRs of bladder stones between the PA and comparison cohort. After adjusting for age, sex, and comorbidities, the HR of bladder stones was 1.63 (95% CI 1.28–2.08) for patients with PA compared to individuals without PA. In this sensitivity analysis, outcome was also consistent with the primary analysis.
Discussion
To the present, this is the first large-scale study to discover that PA is significantly associated with a higher bladder stones risk which was unrecognized previously. The findings disclosed an incidence rate of 5.36 per 1000 person-years of bladder stones in our PA cohort (cumulative incidence around 0.06% even after 10 years follow up) compared with that was 3.76 per 1000 person-years in control group and suggest that bladder stone was very easily ignored in daily practice because of a relative rare condition14. In our study, the bladder stone risk is high in patients with PA; particularly in those without any underlying disease which reached a 2.12-fold increased risk and that indicates a potential linkage between hyperaldosteronism and bladder stone formation.
In addition, in multivariable analysis of Cox regression model with adjusting associated confounders including gender, age, co-morbidities showed that fracture was significantly associated with a 1.77-fold increased risk of bladder stone which may seem a predictive factor for urinary stone. Of note, a lower proportion of cases with fracture were observed in patients with PA while compared to control group; nevertheless, our findings remained to exhibit a significantly higher risk of bladder stone in patients with PA. The findings implicate that PA may likely attribute to urinary stone directly independent of fracture. At last, in the sensitive analysis with frequency matching PA and non-PA group with sex, age and all comorbidities (including fracture), the findings were consistent. Taken together, the findings suggest that PA contributed to bladder stone formation by the disease per se rather than other factors.
Accumulating biologic evidence suggests that PA may play an important role in the development of nephrolithiasis. First, PA likely induces hypercalciuria through body volume expansion, which decreases both proximal tubule sodium and calcium absorption15. Second, PA induces hypocitraturia7. Potassium depletion in PA may induce proximal tubule intracellular acidosis and also cause hypocitraturia. These electrolyte disorders caused by PA itself could lead to the tubular abnormality which indirectly increases the formation of bladder stones. Moreover, PA might cause urinary bladder dysfunction because of hypokalemia. Hypokalemia is known as a cause of hypotonic bladder16,17. Several families of potassium channels, especially large-conductance voltage and calcium-activated BK channels, are essential to control urinary bladder smooth muscle contraction13,18.
PA was also suggested to be associated with new-onset diabetes mellitus and metabolic syndrome3,4. Both diabetes mellitus and metabolic syndrome induce more acidic urine to enhance urate crystallization and promote urate stone formation. Next, PA is accompanied by sympathetic overactivity19 and likely to aggravate urinary stasis20. At last, PA might be associated with benign prostatic hypertrophy (BPH), through elevated serum aldosterone21 and increased level of oxidative stress22,23.
Taken together, our findings provide clinical evidence that patients with chronically persistent hyperaldosteronism eventually develop bladder stones. This is supported by experimental data previously reported. Our findings showed that fracture history or female sex was also among the risk factors contributing to bladder stone formation. Previous study has suggested that bone fracture is significantly associated urinary tract stone24,25. Fracture, as a risk factor for bladder stones, suggests a role of metabolic abnormalities in the formation of bladder stones. Generally speaking, male sex is considered a traditional risk factor in the development of bladder stones, but this was not seen in our PA study cohort. This may be the result of the differences in the sexes that already exist in PA. For example, compared to male patients, female patients are more vulnerable to PA and associated with a higher risk of bilateral PA26, fractures2, depression mood, and even worse physical conditions27, all of which could partly explain why the female sex is a risk factor for the formation of bladder stones. The detailed mechanisms involved in the differences in bladder stone formation among the sexes in patients with PA need to be further clarified.
Some limitations to our study should be addressed. First, laboratory data could not be obtained from the database. Hence, metabolic factors associated with stone formation, such as serum glucose and electrolyte profiles, could not be further evaluated and may bias the findings. Proximity for these confounders, such as diabetes mellitus and hyperlipidemia, were adjusted as best we could in the study. Second, any occurrence of stone formation before the index date were excluded from our study; therefore, the case numbers could be underestimated. Third, influence of medication such as diuretics and potassium or calcium supplements could not be evaluated in our study. Forth, we could not distinguish patients with PA and unilateral hyperplasia from those with bilateral adenomas. Last, one limitation was inherent in the national inpatient database, which included only five diagnoses at discharge28, and some comorbidities might be under-estimated. Therefore, a relative lower incidence rates of hypertension either case group or control group was found after matching process.
In conclusion, the present study shows that patients with PA are at a significantly higher risk for the development of bladder stones which has never been reported previously. In addition to the adverse outcomes of cardiovascular disease and metabolic disorders in patients with PA, they have increased risk of bladder stones as well. Whether or not the suppression effect of mineralocorticoid receptor antagonists could decrease the risk of bladder stones should be further analyzed in the future.
Materials and methods
The NHIRD encrypts patient personal information to protect privacy and provides researchers with anonymous identification numbers associated with relevant claims information. Patient consent is not required to access the NHIRD. This study was approved to fulfill the condition for exemption from the Institutional Review Board (IRB) of China Medical University (CMUH-104-REC2-115). The IRB of China Medical University (CMUH-104-REC2-115) waived the informed consent requirement. Our research was performed in accordance with relevant guidelines/regulations.
Data sources
We used the National Health Insurance Research Database (NHIRD) to construct the study. The NHIRD contains the health insurance claim data from those insured through the Taiwan National Health Insurance program (Taiwan NHI). The Taiwan NHI is a national-based single payer health insurance program that has been in existence since 1995 and covered over 99% of 23 million Taiwan citizens in 1998. The health insurance claims data contains information including a registry of beneficiaries, disease record files (listed by the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]), and other medical services. In this study, all disease records were collected from inpatient files. Before the government released the disease records, patient personal identification information was obscured for purposes of this research.
Study population
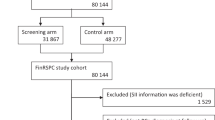
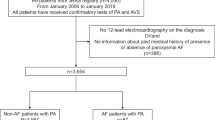
We designed a retrospective, population-based, matched cohort study. We planned to build a cohort of patients with PA (ICD-9-CM 255.1) and a comparison cohort. The PA cohort involved patients with new-onset PA ˃18 years of age and initially diagnosed between the years 1998 and 2011. The index date for patients with PA was the day of first diagnosis. We excluded any patients with PA who also had a history of bladder stones (ICD-9-CM 592.0, 592.1, 592.9) before the index date. The candidate comparison sample included patients from the NHIRD who were not diagnosed with PA. The propensity score matching method was used in this study. We assigned equivalent index dates for candidate comparisons and PA cases. The propensity score of the PA and candidate comparisons was calculated using logistic regression models which involved the variables age, sex, frequency of medical visits, hypertension (ICD-9-CM 401-405), diabetes mellitus (ICD-9-CM 250), hyperlipidemia (ICD-9-CM 272), gout (ICD-9-CM 274), urinary tract infection (ICD-9-CM 599.0), obesity (ICD-9-CM 278.0), chronic kidney disease (CKD, ICD-9-CM 585), fracture (ICD-9-CM 800-829), and hematuria (ICD-9-CM 599.7). For each PA case, the matched comparison subjects were selected using the nearest propensity score by algorithm (http://www2.sas.com/proceedings/sugi29/165-29.pdf). The comparisons also excluded patients with a diagnosis of bladder stones before the index date. The main outcome of this study is that patients with PA have a higher risk for the development of bladder stones. Follow-up visits for these patients began on the index date and terminated when the patients either (1) lost their health insurance; (2) died; (3) were diagnosed with bladder stones; or (4) until December 31, 2013.
Statistical analysis
Age distribution was expressed as mean ± SD; sex and comorbidities were expressed as number and percentage between the PA and comparison cohorts. The standardized mean difference (SMD), a test for distribution differences between the PA and comparison cohorts, was calculated from a difference in means or proportions of a variable divided by a pooled estimate of the SD of that variable. The significance level of SMD was set at a value over 0.1. The incidence density of bladder stones for the PA and comparison cohorts was calculated from the total number of bladder stone events divided by the sum of person time (per 1000 person-years). The cumulative bladder stone incidence curves for individuals with and without PA were drawn using the Kaplan–Meier method; the log-rank test was used to assess the difference in curves. To ascertain the risk of bladder stones between the PA and comparison cohorts, we used the single variable and multivariable Cox proportional hazard models to estimate the hazard ratios (HRs) and corresponding 95% confidence intervals (CIs). Because a death event could bias the estimation of bladder stone occurrence, we also used the competing risk model, a model developed from a standard Cox model29. We included the effect of competing death, shown as the sub-hazard ratios (SHRs) and 95% CIs of the bladder stone incidence in the PA and comparison cohorts. The data management and statistical analysis was performed using SAS 9.4 software (SAS Institute, Cary, NC, United States) and the incidence curve was created using R software30. The significance level was set at less than 0.05 for 2-sided testing.
References
Rossi, G. P. et al. A prospective study of the prevalence of primary aldosteronism in 1125 hypertensive patients. J. Am. Coll. Cardiol. 48, 2293–2300. https://doi.org/10.1016/j.jacc.2006.07.059 (2006).
Wu, V. C. et al. Risk of fracture in primary aldosteronism: A population-based cohort study. J. Bone Mineral Res. 32, 743–752. https://doi.org/10.1002/jbmr.3033 (2017).
Wu, V. C. et al. Risk of new-onset diabetes mellitus in primary aldosteronism: A population study over 5 years. J. Hypertens. 35, 1698–1708. https://doi.org/10.1097/HJH.0000000000001361 (2017).
Hanslik, G. et al. Increased prevalence of diabetes mellitus and the metabolic syndrome in patients with primary aldosteronism of the German Conn’s Registry. Eur. J. Endocrinol. 173, 665–675. https://doi.org/10.1530/EJE-15-0450 (2015).
Stamatelou, K. K., Francis, M. E., Jones, C. A., Nyberg, L. M. & Curhan, G. C. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 63, 1817–1823. https://doi.org/10.1046/j.1523-1755.2003.00917.x (2003).
Bagga, H. S., Chi, T., Miller, J. & Stoller, M. L. New insights into the pathogenesis of renal calculi. Urol. Clin. N. Am. 40, 1–12. https://doi.org/10.1016/j.ucl.2012.09.006 (2013).
Shey, J., Cameron, M. A., Sakhaee, K. & Moe, O. W. Recurrent calcium nephrolithiasis associated with primary aldosteronism. Am. J. Kidney Dis. 44, e7-12 (2004).
Kabadi, U. M. Renal calculi in primary hyperaldosteronism. Postgrad. Med. J. 71, 561–562 (1995).
Wagner, C. A. Effect of mineralocorticoids on acid-base balance. Nephron Physiol. 128, 26–34. https://doi.org/10.1159/000368266 (2014).
Schwartz, B. F. & Stoller, M. L. The vesical calculus. Urol. Clin. N. Am. 27, 333–346 (2000).
Childs, M. A. et al. Pathogenesis of bladder calculi in the presence of urinary stasis. J. Urol. 189, 1347–1351. https://doi.org/10.1016/j.juro.2012.11.079 (2013).
Hammad, F. T., Kaya, M. & Kazim, E. Bladder calculi: Did the clinical picture change?. Urology 67, 1154–1158. https://doi.org/10.1016/j.urology.2005.12.038 (2006).
Petkov, G. V. Central role of the BK channel in urinary bladder smooth muscle physiology and pathophysiology. Am. J. Physiol. 307, R571-584. https://doi.org/10.1152/ajpregu.00142.2014 (2014).
Kittanamongkolchai, W. et al. The changing incidence and presentation of urinary stones over 3 decades. Mayo Clin. Proc. 93, 291–299. https://doi.org/10.1016/j.mayocp.2017.11.018 (2018).
Friedman, P. A. Codependence of renal calcium and sodium transport. Annu. Rev. Physiol. 60, 179–197. https://doi.org/10.1146/annurev.physiol.60.1.179 (1998).
Asmar, A., Mohandas, R. & Wingo, C. S. A physiologic-based approach to the treatment of a patient with hypokalemia. Am. J. Kidney Dis. 60, 492–497. https://doi.org/10.1053/j.ajkd.2012.01.031 (2012).
Matthews, E. et al. Voltage sensor charge loss accounts for most cases of hypokalemic periodic paralysis. Neurology 72, 1544–1547. https://doi.org/10.1212/01.wnl.0000342387.65477.46 (2009).
Petkov, G. V. Role of potassium ion channels in detrusor smooth muscle function and dysfunction. Nat. Rev. Urol. 9, 30–40. https://doi.org/10.1038/nrurol.2011.194 (2011).
Kontak, A. C. et al. Reversible sympathetic overactivity in hypertensive patients with primary aldosteronism. J. Clin. Endocrinol. Metab. 95, 4756–4761. https://doi.org/10.1210/jc.2010-0823 (2010).
Michel, M. C. & Vrydag, W. Alpha1-, alpha2- and beta-adrenoceptors in the urinary bladder, urethra and prostate. Br. J. Pharmacol. 147(Suppl 2), S88-119. https://doi.org/10.1038/sj.bjp.0706619 (2006).
Yalcinkaya, S., Eren, E., Eroglu, M., Aydin, O. & Yilmaz, N. Deficiency of vitamin D and elevated aldosterone in prostate hyperplasia. Adv. Clin. Exp. Med. 23, 441–446 (2014).
Stehr, C. B. et al. Increased levels of oxidative stress, subclinical inflammation, and myocardial fibrosis markers in primary aldosteronism patients. J. Hypertens. 28, 2120–2126. https://doi.org/10.1097/HJH.0b013e32833d0177 (2010).
Bostanci, Y., Kazzazi, A., Momtahen, S., Laze, J. & Djavan, B. Correlation between benign prostatic hyperplasia and inflammation. Curr. Opin. Urol. 23, 5–10. https://doi.org/10.1097/MOU.0b013e32835abd4a (2013).
Caudarella, R., Vescini, F., Buffa, A., La Manna, G. & Stefoni, S. Osteoporosis and urolithiasis. Urol. Int. 72(Suppl 1), 17–19. https://doi.org/10.1159/000076585 (2004).
Han, S. G. et al. Kidney stones and risk of osteoporotic fracture in chronic kidney disease. Sci. Rep. 9, 1929. https://doi.org/10.1038/s41598-018-38191-1 (2019).
Akasaka, H. et al. Sex difference in the association between subtype distribution and age at diagnosis in patients with primary aldosteronism. Hypertension 74, 368–374. https://doi.org/10.1161/HYPERTENSIONAHA.119.13006 (2019).
Kunzel, H. E. et al. Quality of life in patients with primary aldosteronism: Gender differences in untreated and long-term treated patients and associations with treatment and aldosterone. J. Psychiatr. Res. 46, 1650–1654. https://doi.org/10.1016/j.jpsychires.2012.08.025 (2012).
Cheng, C. L. et al. Validation of acute myocardial infarction cases in the national health insurance research database in taiwan. J. Epidemiol. 24, 500–507. https://doi.org/10.2188/jea.je20140076 (2014).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509 (1999).
Team, R. C. A language and environment for statistical computing (R Foundation for Statistical Computing, 2020).
Acknowledgements
This study is supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW108-TDU-B-212-133004); China Medical University Hospital; Academia Sinica Stroke Biosignature Project (BM10701010021); MOST Clinical Trial Consortium for Stroke (MOST 107-2321-B-039-004); Tseng-Lien Lin Foundation, Taichung, Taiwan; and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. The interpretations and conclusions herein do not represent those of the Bureau of National Health Insurance, Department of Health, or the National Health Research Institutes. The funders performed no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
M.C.C., T.M.Y., M.J.W., C.H.C., S.J.J., and C.J.C. designed the research. M.C.C., C.L.L., C.Y.L., and T.M.Y. analyzed and interpreted the data. M.C.C. and T.M.Y. wrote the first draft of the paper. All authors participated in revising the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, MC., Lin, CL., Wu, MJ. et al. Primary aldosteronism is associated with risk of urinary bladder stones in a nationwide cohort study. Sci Rep 11, 7684 (2021). https://doi.org/10.1038/s41598-021-86749-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-86749-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.