Abstract
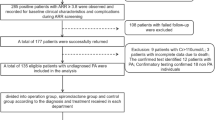
The incidence of atrial fibrillation (AF) and risk of cardiovascular events are reportedly higher in patients with primary aldosteronism (PA) than essential hypertension. However, associated factors of comorbid AF and cardiovascular events in PA patients after PA treatment remain unclear. This nationwide registration study included PA patients ≥20 years old. Incident cardiovascular events were observed with a mean follow-up of approximately 3 years. A total of 3654 patients with PA were included at the time of analysis. Prevalence of AF was 2.4%. PA patients with AF were older, more frequently male and had longer duration of hypertension than those without AF. No significant difference in basal plasma and adrenal venous aldosterone concentration, renin activity, potassium concentration, confirmatory tests of PA, laterality or surgery rate were seen between groups. Logistic regression analysis showed age, male sex, cardiothoracic ratio, past history of coronary artery disease and heart failure were independent factors associated with AF. PA patients with AF showed a higher frequency of cardiovascular events than those without AF (P < 0.001). Multivariate Cox analyses demonstrated AF in addition to older age, duration of hypertension, body mass index and chronic kidney disease as independent prognostic factors for cardiovascular events after PA treatment. Incidence of cardiovascular events were significantly lower in PA patients with AF than AF patients from the Fushimi registry during follow-up after adjusting age, sex and systolic blood pressure. Early diagnosis of PA may prevent AF and other cardiovascular events in PA patients by shortening the duration of hypertension and appropriate PA treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962.
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837–47.
Rienstra M, Lyass A, Murabito JM, Magnani JW, Lubitz SA, Massaro JM, et al. Reciprocal relations between physical disability, subjective health, and atrial fibrillation: the Framingham Heart Study. Am Heart J. 2013;166:171–8.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Rossi GP. Primary aldosteronism: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74:2799–811.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Umakoshi H, Tsuiki M, Takeda Y, Kurihara I, Itoh H, Katabami T, et al. Significance of computed tomography and serum Potassium in predicting subtype diagnosis of primary Aldosteronism. J Clin Endocrinol Metab. 2018;103:900–8.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary Aldosteronism: a multicenter study in Japan. Hypertension. 2018;71:530–7.
Akehi Y, Yanase T, Motonaga R, Umakoshi H, Tsuiki M, Takeda Y, et al. High prevalence of diabetes in patients with primary Aldosteronism (PA) associated with subclinical hypercortisolism and prediabetes more prevalent in Bilateral than Unilateral PA: a large, multicenter cohort study in Japan. Diabetes Care. 2019;42:938–45.
Kobayashi H, Nakamura Y, Abe M, Kurihara I, Itoh H, Ichijo T, et al. Effect of cosyntropin during adrenal venous sampling on subtype of primary aldosteronism: analysis of surgical outcome. Eur J Endocrinol. 2020;182:265–73.
Ohno Y, Sone M, Inagaki N, Kawashima A, Takeda Y, Yoneda T, et al. Nadir Aldosterone levels after Confirmatory Tests are correlated with left ventricular hypertrophy in Primary Aldosteronism. Hypertension. 2020:HYPERTENSIONAHA11914601.
Seccia TM, Caroccia B, Adler GK, Maiolino G, Cesari M, Rossi GP. Arterial hypertension, Atrial Fibrillation, and Hyperaldosteronism: the triple trouble. Hypertension. 2017;69:545–50.
Esato M, Chun YH, An Y, Ogawa H, Wada H, Hasegawa K, et al. Clinical impact of Asymptomatic presentation status in patients with Paroxysmal and Sustained Atrial Fibrillation: The Fushimi AF Registry. Chest. 2017;152:1266–75.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Okamoto R, Taniguchi M, Onishi Y, Kumagai N, Uraki J, Fujimoto N, et al. Predictors of confirmatory test results for the diagnosis of primary hyperaldosteronism in hypertensive patients with an aldosterone-to-renin ratio greater than 20. The SHRIMP study. Hypertens Res. 2019;42:40–51.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, et al. Recommendations on the use of Echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). J Am Soc Echocardiogr. 2015;28:727–54.
Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840–4.
Andersson T, Magnuson A, Bryngelsson IL, Frobert O, Henriksson KM, Edvardsson N, et al. All-cause mortality in 272,186 patients hospitalized with incident atrial fibrillation 1995-2008: a Swedish nationwide long-term case-control study. Eur Heart J. 2013;34:1061–7.
Chatterjee NA, Chae CU, Kim E, Moorthy MV, Conen D, Sandhu RK, et al. Modifiable Risk Factors for Incident Heart Failure in Atrial Fibrillation. JACC Heart Fail. 2017;5:552–60.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J Am Coll Cardiol. 2017;69:1811–20.
Watson T, Karthikeyan VJ, Lip GY, Beevers DG. Atrial fibrillation in primary aldosteronism. J Renin Angiotensin Aldosterone Syst. 2009;10:190–4.
Verdecchia P, Reboldi G, Gattobigio R, Bentivoglio M, Borgioni C, Angeli F, et al. Atrial fibrillation in hypertension: predictors and outcome. Hypertension. 2003;41:218–23.
Vaziri SM, Larson MG, Lauer MS, Benjamin EJ, Levy D. Influence of blood pressure on left atrial size. The Framingham Heart Study. Hypertension. 1995;25:1155–60.
Reil JC, Hohl M, Selejan S, Lipp P, Drautz F, Kazakow A, et al. Aldosterone promotes atrial fibrillation. Eur Heart J. 2012;33:2098–108.
Healey JS, Baranchuk A, Crystal E, Morillo CA, Garfinkle M, Yusuf S, et al. Prevention of atrial fibrillation with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: a meta-analysis. J Am Coll Cardiol. 2005;45:1832–9.
Alexandre J, Dolladille C, Douesnel L, Font J, Dabrowski R, Shavit L, et al. Effects of mineralocorticoid receptor antagonists on atrial fibrillation occurrence: a systematic review, meta-analysis, and meta-regression to identify modifying factors. J Am Heart Assoc. 2019;8:e013267.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Savard S, Amar L, Plouin PF, Steichen O. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2013;62:331–6.
Badheka AO, Patel NJ, Grover PM, Shah N, Patel N, Singh V, et al. Optimal blood pressure in patients with atrial fibrillation (from the AFFIRM Trial). Am J Cardiol. 2014;114:727–36.
Reincke M, Fischer E, Gerum S, Merkle K, Schulz S, Pallauf A, et al. Observational study mortality in treated primary aldosteronism: the German Conn’s registry. Hypertension. 2012;60:618–24.
Rossi GP, Maiolino G, Flego A, Belfiore A, Bernini G, Fabris B, et al. Adrenalectomy lowers incident Atrial Fibrillation in Primary Aldosteronism patients at long term. Hypertension. 2018;71:585–91.
Pan CT, Liao CW, Tsai CH, Chen ZW, Chen L, Hung CS, et al. Influence of different treatment strategies on New-Onset Atrial Fibrillation among patients with Primary Aldosteronism: a Nationwide Longitudinal Cohort-Based Study. J Am Heart Assoc. 2020;9:e013699.
Acknowledgements
We wish to thank the JPAS/JRAS study members for collecting the clinical data. We are grateful to Keiko Umegaki (Kyoto Medical Center) and Kazuho Ikedo (Mie University) for their excellent technical assistance and the Fushimi AF registry investigators for their great help in revising this paper.
Funding
This work was supported by the Japan Agency for Medical Research and Development (AMED) (grant numbers JP17ek0109112 and JP20ek0109352 to MN), Grants-in-Aid for Scientific Research from the Ministry of Education, Science, Technology, Sports and Culture, Japan, and the Mie Medical Foundation (grant number 19K08578 to RO and KD) and the National International Center for Health and Global Medicine, Japan (grant number 30–1008 to AT).
Author information
Authors and Affiliations
Consortia
Contributions
RO and SS designed this study and carried out the analyses; RO, SS and MN drafted and revised the manuscript; and CI, MA, KK, IK, YT, YO, TK, MT, SF collected the data; NI, HR, AT, KT, YY, KD managed and advised for the study and the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakaguchi, S., Okamoto, R., Inoue, C. et al. Associated factors and effects of comorbid atrial fibrillation in hypertensive patients due to primary aldosteronism. J Hum Hypertens 37, 757–766 (2023). https://doi.org/10.1038/s41371-022-00753-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00753-2