Abstract
To trace the linkage between Japanese healthcare-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) strains in the early 1980s and the 2000s onward, we performed molecular characterizations using mainly whole-genome sequencing. Among the 194 S. aureus strains isolated, 20 mecA-positive MRSA (10.3%), 8 mecA-negative MRSA (4.1%) and 3 mecA-positive methicillin-susceptible S. aureus (MSSA) (1.5%) strains were identified. The most frequent sequence type (ST) was ST30 (n = 11), followed by ST5 (n = 8), ST81 (n = 4), and ST247 (n = 3). Rates of staphylococcal cassette chromosome mec (SCCmec) types I, II, and IV composed 65.2%, 13.0%, and 17.4% of isolates, respectively. Notably, 73.3% of SCCmec type I strains were susceptible to imipenem unlike SCCmec type II strains (0%). ST30-SCCmec I (n = 7) and ST5-SCCmec I (n = 5) predominated, whereas only two strains exhibited imipenem-resistance and were tst-positive ST5-SCCmec II, which is the current Japanese HA-MRSA genotype. All ST30 strains shared the common ancestor strain 55/2053, which caused the global pandemic of Panton-Valentine leukocidin-positive MSSA in Europe and the United States in the 1950s. Conspicuously more heterogeneous, the population of HA-MRSA clones observed in the 1980s, including the ST30-SCCmec I clone, has shifted to the current homogeneous population of imipenem-resistant ST5-SCCmec II clones, probably due to the introduction of new antimicrobials.
Similar content being viewed by others
Introduction
Staphylococcus aureus (S. aureus) is a major opportunistic pathogen that can cause various life-threatening infections, and approximately 20% of healthy human individuals are persistent carriers of this bacterial species1. The first case of methicillin-resistant S. aureus (MRSA) was identified in the United Kingdom in 1961, only one year after the introduction of methicillin2,3. Since then, MRSA has remained a major clinical concern with both hospital-associated and community-associated MRSA (HA-MRSA and CA-MRSA, respectively) infections worldwide4,5,6. The number of deaths related to MRSA infection remains high, and rivals HIV/AIDS infections in its public health impact7.
MRSA is generated when methicillin-susceptible S. aureus (MSSA) acquires the exogenous mecA gene encoding the penicillin-binding protein 2′ (PBP2′), which is carried on a mobile genetic element designated staphylococcal cassette chromosome mec (SCCmec)8. According to the International Working Group on the Classification of Staphylococcal Cassette Chromosome Elements, strains can be classified by SCCmec types (I–XIV) based on their combination of mec and ccr gene complexes6,9,10,11. Each MRSA clone has been categorized by the combination of the chromosomal genotype of the recipient MSSA strain and the genotype of the integrated SCCmec. Therefore, multilocus sequence typing (MLST) and SCCmec typing by PCR and/or sequencing methods have been widely used as the gold standard methods in molecular epidemiological studies of MRSA4,12,13,14,15. In addition, whole-genome sequencing (WGS) of bacterial isolates by next-generation sequencing (NGS) technologies has recently become a promising tool for molecular typing, which together with advancing data processing systems, ever-larger NGS datasets and decreased costs has allowed remarkable advances for microbiologists16. During the 1970s and 1980s the MRSA epidemic was occurring not only in Japan, but throughout the world17,18. However, the molecular typing tools for MRSA isolates were not established until the 2000s. Thus, there have been few reports on molecular epidemiology of MRSA isolates collected before then.
Epidemiological tracking of drug-resistant bacteria using molecular typing tools over time can provide crucial insights into infection control and appropriate use of antimicrobials in clinical practice19. Therefore, the aims of this study were to retrospectively review the population structure of Japanese HA-MRSA strains isolated in the early 1980s using MLST, SCCmec typing and phylogenetic analysis based on whole-genome single nucleotide polymorphisms (SNPs), and to compare the population structure with that of strains isolated in recent years. Our data shows that in the 1980s, the population structure of Japanese HA-MRSA was remarkably polyclonal, including representative clones that are now rarely found.
Results
Prevalence and antimicrobial susceptibilities of MRSA and MSSA isolates in Japanese hospitals during the early 1980s
In total, 194 isolates were identified as S. aureus. One hundred and seventy-four patients yielded one strain per patient, whereas ten patients yielded two strains. According to phenotypic and genotypic determination of methicillin-resistance, we identified 20 mecA-positive MRSA (10.3%), 8 mecA-negative MRSA (4.1%), 3 mecA-positive MSSA (1.5%) and 163 mecA-negative MSSA (84.0%) strains. Consequently, the phenotypic methicillin-resistant rate of the strains described in this study was 14.4% (28 of 194 strains).
As shown in Table 1, all MRSA strains described in this study were susceptible to levofloxacin, which had not yet entered clinical use in Japan in the 1980s. None of the S. aureus strains was resistant to the anti-MRSA agents vancomycin, teicoplanin, linezolid, or arbekacin, irrespective of methicillin resistance. Moreover, 32.1% of MRSA strains (9 of 28 strains) showed resistance to imipenem, which was unavailable in Japan during the period under study, whereas all MSSA strains were susceptible to imipenem.
Detailed genetic characterizations of MRSA and mecA-positive MSSA strains
The results of MLST, SCCmec typing, spa-typing, toxin profiling, and acquired antimicrobial resistance gene profiling are shown in Table 2.
Among the 31 strains that included phenotypically-identified MRSA and mecA-positive MSSA, the most frequent sequence type (ST) was ST30 (n = 11, 35.5%), followed by ST5 (n = 8, 25.8%), ST81 (n = 4, 12.9%) and ST247 (n = 3, 9.7%). SCCmec types I, II, and IV were found in 15, 3, and 4 of 23 mecA-positive strains, respectively. ST30-SCCmec I (n = 7) was the most predominant genotype, followed by ST5-SCCmec I (n = 5), ST30-SCCmec IV (n = 3), ST247-SCCmec I (n = 3), and ST5-SCCmec II (n = 2). The current predominant HA-MRSA genotype, tst-positive ST5-SCCmec II, was identified in only two strains, N106 and N315. Eight PVL-positive strains were identified, all of which were ST30.
Among the acquired antimicrobial resistance genes detected in this study, mecA was the most frequent (n = 23), followed by blaZ (n = 22), ermA (n = 19), ant(9)-Ia (n = 19), and aac(6′)-aph(2′’) (n = 18). All mecA-positive strains had aminoglycoside resistance genes, and multiple strains carried genes related to resistance to macrolide (82.6%), tetracycline (39.1%), and phenicol (13.0%).
Overall, a diversity of MRSA isolates representing separate clones were found to be present during the early 1980s, and diverse genotypes were detected even among MRSA strains exhibiting the same ST.
Antimicrobial susceptibilities of the strains across SCCmec types
In order to consider the mechanisms for the shift in population structure of HA-MRSA strains from polyclonal to monoclonal in recent years, we compared the antimicrobial susceptibilities of MRSA strains across SCCmec types (Table 3).
Strains that carried SCCmec types I and II were highly resistant to β-lactams including oxacillin, but those that carried SCCmec type IV were more susceptible to β-lactams despite being mecA-positive. Among the 15 strains carrying SCCmec type I, the rate of erythromycin resistance was the highest (80.0%), followed by resistance to gentamicin (66.7%), clindamycin (40.0%), and minocycline (26.7%), which were commonly used antimicrobials at that time. The imipenem susceptibility rate in SCCmec type I strains was 73.3% (11 of 15 strains) as compared with 0% in SCCmec type II strains (0 of 3 strains) (p = 0.043).
The mecA-negative MRSA strains (n = 8) were more susceptible to β-lactams, and notably, all strains were susceptible to imipenem except the isolate N89. Also, these strains showed lower MICs for aminoglycosides, minocycline, erythromycin and clindamycin, when compared with mecA-positive strains.
Population structure of MRSA and mecA-positive MSSA strains in Japan during the early 1980s
The result of phylogenetic analysis based on whole-genome SNPs of 20 mecA-positive MRSA, 8 mecA-negative MRSA, 3 mecA-positive MSSA, and 125 reference S. aureus strains, is shown in Fig. 1.
Phylogenetic tree based on whole-genome SNPs in strains in the present study and 125 reference strains. mecA-positive MRSA, mecA-negative MRSA, mecA-positive MSSA isolated in this study and reference strains were indicated in red, blue, green and black letters, respectively. NJ tree was constructed by alignment of 41,910 SNP sites. S. argenteus MSHR1132 was used as the outgroup. CC clonal complex, MRSA methicillin-resistant Staphylococcus aureus, MSSA methicillin-susceptible Staphylococcus aureus, NJ neighbor-joining, SNPs single nucleotide polymorphisms, ST sequence type.
A neighbor-joining (NJ) tree was constructed by the alignment of 41,910 SNP sites. The percentage of the reference genome (S. argenteus MSHR1132) covered by all isolates was 62.95% (1,739,038 of 2,762,785 positions). Strains belonging to the CC30 cluster were most abundant (n = 11), followed by clonal complexes (CC) 5 (n = 9), CC1 (n = 4), and CC8 (n = 4), indicating that the population structure of MRSA strains during the early 1980s was composed of diverse clones.
Whole-genome SNP analysis of CC30 and CC5 strains
Detailed pairwise SNPs analysis of 11 ST30 strains described in this study and 6 CC30 reference strains was performed (Fig. 2a). The percentage of the reference genome (SJTUF_J27, ST433) covered by all strains was 89.16% (2,500,756 of 2,804,761 positions) in the SNPs analysis. SNP differences ranged from 28 to 1008. All CC30 strains described in this study clustered into a single clade and were most closely related to the MSSA strain 55/2053 isolated in the United Kingdom in 195520. Strains N83 and N86, which were isolated in Kumamoto in the same year and exhibited the same spa-type t1504, showed 28 SNP differences, suggesting a direct horizontal spread within the hospital. However, the SCCmec type and antimicrobial resistance gene profiles differed between these two strains, suggesting that these strains were independently acquired by each inpatient from different infectious sources. Similarly, the ST30 strains isolated in this study could be recognized as branches of a clone endemic to Japan, with only small numbers of SNPs ranging from 28 to 16421,22.
The phylogenetic inter-strain relationships within the same clonal complex based on pairwise SNP differences. (a) Phylogenetic tree based on whole-genome SNPs in CC30 strains. Staphylococcus aureus strain SJTUF_J27 was used as the outgroup. NJ tree was constructed based on the alignment of 2353 SNP sites. (b) Phylogenetic tree based on whole-genome SNPs in CC5 strains. S. aureus strain ED98 was used as the outgroup. NJ tree was constructed based on the alignment of 3684 SNP sites. mecA-positive MRSA, mecA-negative MRSA, mecA-positive MSSA isolated in this study and reference strains were indicated in red, blue, green and black letters, respectively. The numbers of inter-strain SNP differences were visualized in a red-yellow-green gradient with red indicating the top score (> 600) and green indicating the bottom score (0). CC clonal complex, MRSA methicillin-resistant Staphylococcus aureus, MSSA methicillin-susceptible Staphylococcus aureus, NJ neighbor-joining, SNPs single nucleotide polymorphisms.
Next, we performed SNP analysis among 9 CC5 MRSA strains in this study and 32 reference strains (Fig. 2b). The percentage of the reference genome (ED98) covered by all strains was 89.13% (2,517,393 of 2,824,404 positions) in the SNP analysis. SNP differences ranged from 0 to 621. ST5 MRSA strains described in this study clustered into five different clades. Strains N366, N98, N345, N279, and N283 harboring SCCmec type I belonged to a single cluster, with the number of SNP differences within the cluster ranging from 30 to 84. Strains N279 and N283, which were isolated in Miyagi in the same year, showed only 30 SNP differences and similar profiles regarding spa type, toxin and antimicrobial resistance genes, suggesting transmission events within a short period. Although strains N366 and N98 strains exhibited only 41 SNP differences, these strains were isolated in locations separated by over 750 km of mostly ocean, Okinawa and Nagasaki (Table 2). According to these results, strains exhibiting ST5-SCCmec I belonging to this clade could be recognized as part of another endemic clone in Japan, as contrasted with strains 16,125, 18,412, 18,341, 10,388, 15,532, 18,583, 16,035, and 10,497, all ST228 and all isolated at a hospital during the outbreaks in Switzerland23, and distinguished from each other pairwise by only 0 to 7 SNPs (Fig. 2b). In contrast, only the strains N315 and N106 exhibiting ST5-SCCmec II belong to the same clade with Mu3 and Mu50, which were isolated as HA-MRSA in the 1990s24.
These results suggest that MRSA clones exhibiting ST30- and ST5-SCCmec I may have already spread as major endemic clones throughout Japan by the early 1980s, whereas ST5-SCCmec II had achieved only a minor presence at that time.
Discussion
Our results suggest that the population structure of Japanese HA-MRSA strains during the early 1980s was notably different from that in recent years. The early 1980s polyclonal structure included ST5- and ST30-SCCmec I clones, both of which have become uncommon recently. The recent monoclonal population structure of HA-MRSA strains in Japan, which is composed of imipenem-resistant ST5-SCCmec II clone, likely formed over the past several decades, possibly in response to the release of various new antimicrobial agents including imipenem and changes in MRSA treatment strategies from the 1980s onward.
PVL-positive ST30-SCCmec I was the most frequent genotype among Japanese HA-MRSA strains in the early 1980s. According to a previous report, nosocomial outbreaks of MRSA exhibiting PVL-positive ST30-SCCmec IV occurred frequently in the late 1980s and early 1990s in Japanese hospitals25, whereas this genotype comprised only a minor population in the early 1980s as represented in this study. Our results suggest that the population structure of Japanese HA-MRSA strains underwent dynamic replacement through the 1980s. This replacement, largely due to ST30 MRSA clones, has probably resulted from high genetic and phenotypic diversity among ST30 MRSA strains. Indeed, in addition to mecA-positive MRSA, ST30 strains rarely isolated today such as mecA-negative MRSA and mecA-positive MSSA, were also found among the ST30 strains analyzed here. Differences in observed SCCmec types and the presence or absence of PVL genes were also noted among these strains.
As previously reported, the CC30 S. aureus lineage can be divided into three clusters: Clade 1 (prototype strain 55/2053; PVL-positive and penicillin-resistant MSSA), Clade 2 (prototype strain TCH60; PVL-positive CA-MRSA harboring SCCmec type IV), and Clade 3 (prototype strain MRSA252/EMRSA-16; PVL-negative HA-MRSA harboring SCCmec type II or IV)20. Clade 1 strains cause severe infections and were the epidemic strain type in Europe, the United States, and Australia in the 1950s26,27,28,29,30. The percent of S. aureus infections caused by Clade 1 strains had dramatically decreased by the mid-1960s, due to methicillin use for the treatment of penicillin-resistant strains31. However, according to our results, this clone had re-emerged as HA-MRSA in Japanese hospitals in the early 1980s. Our phylogenetic analysis based on whole-genome SNPs demonstrated that all Japanese ST30 isolates clustered into a single clade including strain 55/2053, suggesting that a Clade 1 strain imported from overseas had acquired SCCmec type I, SCCmec type IV, or unknown genetic factors and had already undergone diversification in Japanese hospitals by the early 1980s. Consequently, the ST30 strains had likely spread throughout Japan as a nosocomial clone causing a regional outbreak at that time.
This study shows that ST5-SCCmec I was the second-most frequent genotype among Japanese HA-MRSA strains in the early 1980s. This genotype is shared by EMRSA-3, which was the most common MRSA clone in the United Kingdom in 1987–1988 along with EMRSA-15 (ST22-SCCmec IV) and EMRSA-16 (ST36-SCCmec II)4. Studies conducted in South America in the late 1990s have identified the Cordobes/Chilean clone, which is genetically related to EMRSA-3 but presents differences in its pulsed-field gel electrophoresis (PFGE) pattern and spa type32,33,34. This MRSA clone was also detected at a high rate in hospitals in South Brazil in 2008, suggesting the potential for re-dissemination in Brazil35,36. Although this MRSA clone exhibiting ST5-SCCmec I has remained uncommon in regions outside of South America in recent years, continuous monitoring is needed to prevent future outbreaks.
Surprisingly, the clones of MRSA resistant to imipenem, such as strain N315, existed before imipenem entered clinical use. We previously reported strain N315, which was imipenem-resistant, tst-positive ST5-SCCmec II, as a representative strain of the New York/Japan HA-MRSA clone37. We reported that strains harboring SCCmec type II accounted for a large portion of MRSA in Japanese hospitals in the late 1990s12,38. In this study, our results show that a Japanese HA-MRSA lineage exhibiting the same genotype as strain N315 was already circulating as one of the diverse clones in the early 1980s. The phenotypic characteristics of strain N315 was multidrug-resistant, especially to imipenem. In the 1980s, multiple broad-spectrum antimicrobials entered clinical use in Japan, while imipenem/cilastatin was launched in 1987 and was being used as an anti-MRSA agent before the clinical introduction of vancomycin in 1991 in Japan. By contrast with SCCmec II strains, strains harboring SCCmec type I, which was the predominant genotype in this study and some countries including the United Kingdom in the early 1980s12,39, displayed a high rate of imipenem-susceptibility. It was also reported that in vitro exposure to imipenem can select for conversions of heterogeneous-to-homogeneous and Eagle type-to-homogeneous methicillin resistance in S. aureus strains via mutations to such chromosomal genes as vraSR and rpoB6,13,24,40,41,42,43. Thus, the frequent use of imipenem to treat MRSA infections may have contributed to the selective pressure for imipenem-resistant ST5-SCCmec II MRSA between 1980 and 2000, and caused the dynamic population shift in Japanese hospitals from diverse imipenem-susceptible MRSA clones to the monoclonal imipenem-resistant ST5-SCCmec II MRSA. The reason why imipenem-resistant clones other than ST5-SCCmec II MRSA disappeared in the 1990s is unclear, but some not-yet-understood factors may exist that boost the survival rate of ST5-SCCmec II MRSA.
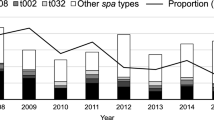
Our results show that the heterogeneous population of diverse clones observed in the 1980s shifted to the homogeneous population of ST5-SCCmec II clones from the 2000s onward among Japanese HA-MRSA isolates. However, entering the 2010s, further changes have been occurring in the population structural. It was reported that the population of Japanese HA-MRSA was shifting again in the 2010s from N315-like CC5-SCCmec II to CC8- SCCmec IV and CC1- SCCmec IV, both of which had higher susceptibility to cefotaxime, levofloxacin, clarithromycin and clindamycin44. The recovery of antimicrobial susceptibilities, and the history of clonal evolution of HA-MRSA strains from the 1980s to the 2010s, seems to reflect improved recent awareness of appropriate antimicrobial usage.
In this study, multiple MRSA strains exhibiting ST247-SCCmec I were isolated in the northeast area of Japan. This genotype is known as the Iberian clone, which was one of the major pandemic MRSA clones until the 2000s45,46,47,48. Our results show the local existence of the Iberian clone in Japan during the early 1980s. Interestingly, all ST247-SCCmec I strains in this study were resistant to imipenem. During the early clinical use of imipenem around the world, the Iberian clone may have undergone spread from the 1990s to the early 2000s. However, the Iberian clone has already been supplanted by the current major epidemic clones49.
Intriguingly, multiple mecA-negative MRSA and mecA-positive MSSA strains, though rarely observed today, were identified in this study, suggesting that methicillin-resistance in S. aureus strains of that time had both genetic and phenotypic diversity. These atypical S. aureus strains are known as oxacillin-susceptible MRSA (OS-MRSA) or borderline oxacillin-resistant S. aureus (BORSA) with oxacillin MICs typically equal to 1–8 μg/mL, which have been reported from various geographic locations for over a decade50,51. Although the clinical instances are not frequent compared with typical MRSA, OS-MRSA could have been underestimated because of the discrepancy between the phenotypes and genotypes in clinical laboratories50. BORSA can appear as community-acquired infections related to previous antimicrobial drug usage52. Our results suggest that OS-MRSA and BORSA strains were already circulating in the early 1980s. All OS-MRSA strains in the present study were ST30 strains isolated in geographically separated regions, and accounted for 30.0% (3 of 10) of mecA-positive ST30 strains. Even though S. aureus strains with intermediate methicillin-resistance such as OS-MRSA and BORSA were frequently isolated from hospital inpatients in the early 1980s, enhanced selective pressures due to new drug developments may have eliminated them from hospital environments over the past several decades. The intrinsic mechanisms of methicillin-resistance vary from isolate to isolate. The presence or hyper-production of beta-lactamase53,54,55, or the quantity of native PBP proteins and their β-lactam binding affinities54,55,56,57,58,59,60,61,62, or mutations in several chromosomal genes (e.g., femA, femB, gdpP, yjbH, and acrB) have been presumed to mediate β-lactam resistance58,59,60,61,62. Further systematic characterization of these atypical phenotypes will be indispensable in identifying undiscovered genetic traits of methicillin resistance.
In conclusion, this study reveals the alteration in population structure of HA-MRSA strains from the early 1980s onward, probably due to the survival of highly drug-resistant clones that may have arisen in response to new drugs introduced over the past several decades. Our findings clarify the role of diagnostic microbiology for tracking the epidemiology of MRSA, giving important evidence for a close correlation between spread of drug-resistance and appropriate/inappropriate use of antimicrobials. These findings will aid efforts to prevent escalating antimicrobial resistance.
Methods
Bacterial strains collection
This study examined a collection of 194 S. aureus strains (designated as “N” strains) that were isolated from 184 Japanese inpatients in 22 prefectures between January 1982 and December 1983. A subset of these N strains was previously reported63. The isolates were mainly from Fukushima (19, 9.8%), Miyagi (18, 9.3%), Okinawa (18, 9.3%), and Osaka (18, 9.3%) prefectures. Specimen types were as follows: pus (88, 45%), sputum (43, 22%), blood (20, 10%), urine (15, 8%), pharynx (10, 5%), other (7, 4%), and unknown (12, 6%), suggesting that skin and soft tissue infection and respiratory tract infection were major infectious diseases in the study population.
The originally stored isolates were inoculated on BBL Trypticase Soy Agar (TSA) (Beckton Dickinson Japan, Co., Ltd., Tokyo, Japan) and incubated at 37 °C for 24 h. Catalase-positive, Gram-positive cocci that were presumptively identified as staphylococci by colony morphology, were subcultured on TSA. Tube coagulase tests with rabbit plasma (Denka Seiken Co., Ltd., Tokyo, Japan) were performed, and only coagulase-positive staphylococcal strains were selected for further investigation. S. aureus was confirmed by a PCR method targeting the thermonuclease (nuc) gene after DNA extraction64. The S. aureus isolates were stored again in sterilized 10% skim milk (Difco Skim Milk, Becton, Dickinson and Co., Franklin Lakes, NJ, USA) at − 80 °C.
DNA extraction
Chromosomal DNA was extracted from bacterial cultures after single colony isolation on TSA, using the QIAamp DNA Mini Kit (QIAGEN, Hilden, Germany). Purified genomic DNA was used for PCRs and sequencing-based methods.
Determination of methicillin resistance
We determined phenotypic methicillin resistance in all S. aureus strains by evaluating oxacillin and cefoxitin susceptibilities according to Clinical and Laboratory Standards Institute (CLSI) M100-S22 performance standards. In addition, all strains were genetically assessed by two different PCRs for the presence of the mecA gene65,66. We also confirmed the presence or absence of the mecA gene by whole-genome sequencing for phenotypically-identified MRSA strains.
Antimicrobial susceptibility testing
Minimum inhibitory concentration (MIC) tests for other antimicrobial agents were performed by the broth microdilution method by BBL Mueller–Hinton II Broth (Cation-Adjusted) (CAMHB) (Beckton Dickinson Japan, Co., Ltd., Tokyo, Japan) using the Dry Plate “Eiken” DP32 (Eiken Chemical Co., Tokyo, Japan), containing oxacillin, cefoxitin, ampicillin, cefazolin, cefmetazole, flomoxef, imipenem, gentamicin, arbekacin, minocycline, erythromycin, clindamycin, levofloxacin, vancomycin, teicoplanin, linezolid, fosfomycin and trimethoprim-sulfamethoxazole. For oxacillin and cefoxitin, agar dilution method was also performed using BBL Mueller Hinton II Agar (Beckton Dickinson Japan, Co., Ltd., Tokyo, Japan), with 2% NaCl for oxacillin, in order to measure the detailed MIC values. MICs were examined by visual observation and interpreted according to CLSI M100-S22 performance standards.
The differences in the rates of imipenem susceptibility by SCCmec types were evaluated using Fisher's exact test utilizing the fisher. test function in R version 3.5.1 (R Development Core Team). Differences with p values < 0.05 were considered significant.
Molecular typing of MRSA strains
spa-typing and multilocus sequence typing (MLST) were carried out as previously reported67,68,69. Direct sequencing of PCR products was performed for spa typing and MLST for the S. aureus strains. Sequencing reactions were performed using a Big Dye Terminator (version 3.1) Cycle Sequencing Kit with an ABI Prism 3100 genetic analyzer (Applied Biosystems, Thermo Fisher Scientific Inc., Waltham, MA, USA). After assembling both forward and reverse consensus sequences, the spa type and MLST were assigned using the RIDOM web server (http://spaserver.ridom.de/) and the PubMLST (https://pubmlst.org/organisms/staphylococcus-aureus), respectively.
SCCmec typing (I–V) was performed by a multiplex PCR method reported previously14. Thirteen exotoxin genes, encoding staphylococcal enterotoxins SEA (sea), SEB (seb), SEC (sec), SED (sed), SEE (see), SEG (seg), SEH (seh), SEI (sei), SEJ (sej); exfoliative toxin A, B (ETA; eta, ETB; etb, respectively); toxic shock syndrome toxin (TSST-1; tst); and Panton-Valentine leukocidin (PVL; lukS and lukF) were detected by PCRs as reported previously70,71,72. Using 5 μL of PCR sample, DNA fragments were analyzed by electrophoresis on a 1% agarose gel stained with ethidium bromide.
WGS and additional molecular phylogenetic analysis
The Nextera XT DNA sample preparation kit (Illumina Inc., San Diego, CA, USA) was used for sample preparation for WGS. The DNA libraries were then purified using AMPure beads (Beckman Coulter, Inc., CA), according to the manufacturer’s protocol. Sequencing was performed using a paired-end 2 × 250 or 300-bp cycle runs on the Illumina MiSeq sequencing system using MiSeq reagent kit v2 or v3 (Illumina Inc.).
After sequencing, the obtained reads were filtered and trimmed by removing bases with quality value scores of 20 or less, de novo assembly was performed using the CLC Genomics Workbench version 9 (Qiagen N.V., Venlo, The Netherlands) with the default parameters.
Assembled contigs were submitted to spaTyper 1.0 for spa-typing, ResFinder 3.0 for detection of acquired drug-resistant genes, and MLST 1.8 for MLST, which are all housed at the Center for Genomic Epidemiology (CGE) website (http://www.genomicepidemiology.org//)16,73,74,75.
To infer the phylogenetic relationship based on whole-genome SNPs among strains in this study and 125 reference strains, assembled contigs were also submitted to CSI phylogeny 1.4 on the CGE website76. The complete sequences of the reference strains were accessed from the National Center for Biochemistry Information (NCBI) database. In addition, pairwise SNP analyses were performed focusing on CC5 and CC30 strains in order to elucidate relatedness with and preservation among the recent MRSA strains. Using a Newick file output from SNP analysis by CSI phylogeny, a neighbor-joining (NJ) tree was visualized using Figtree v1.4.3 (http://tree.bio.ed.ac.uk/software/figtree/). The numbers of inter-strain SNP differences were constructed in a red-yellow-green gradient with red indicating the top score (> 600) and green indicating the bottom score (0).
Data availability
The read data for whole-genome sequencing analysis of strains in this study have been deposited in GenBank under accession number DRA010146.
References
Kluytmans, J., van Belkum, A. & Verbrugh, H. Nasal carriage of Staphylococcus aureus: Epidemiology, underlying mechanisms, and associated risks. Clin. Microbiol. Rev. 10, 505–520. https://doi.org/10.1128/CMR.10.3.505 (1997).
Jevons, M. P., Coe, A. W. & Parker, M. T. Methicillin resistance in staphylococci. Lancet 1, 904–907. https://doi.org/10.1016/s0140-6736(63)91687-8 (1963).
Barber, M. Methicillin-resistant staphylococci. J. Clin. Pathol. 14, 385–393. https://doi.org/10.1136/jcp.14.4.385 (1961).
Enright, M. C. et al. The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA). Proc. Natl. Acad. Sci. USA 99, 7687–7692. https://doi.org/10.1073/pnas.122108599 (2002).
Gorak, E. J., Yamada, S. M. & Brown, J. D. Community-acquired methicillin-resistant Staphylococcus aureus in hospitalized adults and children without known risk factors. Clin. Infect. Dis. 29, 797–800. https://doi.org/10.1086/520437 (1999).
Hiramatsu, K. et al. Genomic basis for methicillin resistance in Staphylococcus aureus. Infect. Chemother. 45, 117–136. https://doi.org/10.3947/ic.2013.45.2.117 (2013).
Boucher, H. W. & Corey, G. R. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 46(Suppl 5), S344-349. https://doi.org/10.1086/533590 (2008).
Ito, T., Katayama, Y. & Hiramatsu, K. Cloning and nucleotide sequence determination of the entire mec DNA of pre-methicillin-resistant Staphylococcus aureus N315. Antimicrob. Agents Chemother. 43, 1449–1458. https://doi.org/10.1128/AAC.43.6.1449 (1999).
Wu, Z., Li, F., Liu, D., Xue, H. & Zhao, X. Novel Type XII Staphylococcal Cassette Chromosome mec Harboring a New Cassette Chromosome Recombinase, CcrC2. Antimicrob. Agents Chemother. 59, 7597–7601. https://doi.org/10.1128/aac.01692-15 (2015).
Baig, S. et al. Novel SCCmec type XIII (9A) identified in an ST152 methicillin-resistant Staphylococcus aureus. Infect. Genet. Evol. 61, 74–76. https://doi.org/10.1016/j.meegid.2018.03.013 (2018).
Urushibara, N., Aung, M. S., Kawaguchiya, M. & Kobayashi, N. Novel staphylococcal cassette chromosome mec (SCCmec) type XIV (5A) and a truncated SCCmec element in SCC composite islands carrying speG in ST5 MRSA in Japan. J. Antimicrob. Chemother. 75, 46–50. https://doi.org/10.1093/jac/dkz406 (2020).
Hiramatsu, K., Kondo, N. & Ito, T. Genetic basis for molecular epidemiology of MRSA. J. Infect. Chemother. 2, 117–129. https://doi.org/10.1007/BF02351563 (1996).
Hiramatsu, K., Cui, L., Kuroda, M. & Ito, T. The emergence and evolution of methicillin-resistant Staphylococcus aureus. Trends Microbiol. 9, 486–493. https://doi.org/10.1016/s0966-842x(01)02175-8 (2001).
Kondo, Y. et al. Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob. Agents Chemother. 51, 264–274. https://doi.org/10.1128/AAC.00165-06 (2007).
Oliveira, D. C. & de Lencastre, H. Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 46, 2155–2161. https://doi.org/10.1128/aac.46.7.2155-2161.2002 (2002).
Larsen, M. V. et al. Multilocus sequence typing of total-genome-sequenced bacteria. J. Clin. Microbiol. 50, 1355–1361. https://doi.org/10.1128/jcm.06094-11 (2012).
Nielsen, K. L. et al. Fitness cost: A bacteriological explanation for the demise of the first international methicillin-resistant Staphylococcus aureus epidemic. J. Antimicrob. Chemother. 67, 1325–1332. https://doi.org/10.1093/jac/dks051 (2012).
Campanile, F., Bongiorno, D., Borbone, S. & Stefani, S. Hospital-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) in Italy. Ann. Clin. Microbiol. Antimicrob. 8, 22. https://doi.org/10.1186/1476-0711-8-22 (2009).
Li, S. et al. The changing pattern of population structure of Staphylococcus aureus from Bacteremia in China from 2013 to 2016: ST239-030-MRSA Replaced by ST59-t437. Front. Microbiol. 9, 332. https://doi.org/10.3389/fmicb.2018.00332 (2018).
McGavin, M. J., Arsic, B. & Nickerson, N. N. Evolutionary blueprint for host- and niche-adaptation in Staphylococcus aureus clonal complex CC30. Front Cell Infect. Microbiol. 2, 48. https://doi.org/10.3389/fcimb.2012.00048 (2012).
Tewhey, R. et al. Genetic structure of community acquired methicillin-resistant Staphylococcus aureus USA300. BMC Genomics 13, 508. https://doi.org/10.1186/1471-2164-13-508 (2012).
Alam, M. T. et al. Transmission and microevolution of USA300 MRSA in U.S. households: Evidence from whole-genome sequencing. mBio 6, e00054–00015. https://doi.org/10.1128/mBio.00054-15 (2015).
Vogel, V., Falquet, L., Calderon-Copete, S. P., Basset, P. & Blanc, D. S. Short term evolution of a highly transmissible methicillin-resistant Staphylococcus aureus clone (ST228) in a tertiary care hospital. PLoS ONE 7, e38969. https://doi.org/10.1371/journal.pone.0038969 (2012).
Kuroda, M., Kuwahara-Arai, K. & Hiramatsu, K. Identification of the up- and down-regulated genes in vancomycin-resistant Staphylococcus aureus strains Mu3 and Mu50 by cDNA differential hybridization method. Biochem. Biophys. Res. Commun. 269, 485–490. https://doi.org/10.1006/bbrc.2000.2277 (2000).
Taneike, I. et al. Molecular nature of methicillin-resistant Staphylococcus aureus derived from explosive nosocomial outbreaks of the 1980s in Japan. FEBS Lett. 580, 2323–2334. https://doi.org/10.1016/j.febslet.2006.03.049 (2006).
Gillespie, W. A. & Alder, V. G. Control of an outbreak of staphylococcal infection in a hospital. Lancet 272, 632–634. https://doi.org/10.1016/s0140-6736(57)91091-7 (1957).
Rountree, P. M. & Rheuben, J. Penicillin-resistant Staphylococci in the general population. Med. J. Aust. 43, 399–402. https://doi.org/10.5694/j.1326-5377.1956.tb35408.x (1956).
Rountree, P. M. & Beard, M. A. Further observations on infection with phage type 80 staphylococci in Australia. Med. J. Aust. 45, 789–795. https://doi.org/10.5694/j.1326-5377.1958.tb36519.x (1958).
Shaffer, T. E., Sylvester, R. F., Jr., Baldwin, J. N. & Rheins, M. S. Staphylococcal infections in newborn infants. II. Report of 19 epidemics caused by an identical strain of staphylococcus pyogenes. Am. J. Public Health Nations Health 47, 990–994. https://doi.org/10.2105/ajph.47.8.990 (1957).
Bynoe, E. T., Elder, R. H. & Comtois, R. D. Phage-typing and antibiotic-resistance of staphylococci isolated in a general hospital. Can. J. Microbiol. 2, 346–358. https://doi.org/10.1139/m56-041 (1956).
Jessen, O., Rosendal, K., Bülow, P., Faber, V. & Eriksen, K. R. Changing Staphylococci and Staphylococcal Infections. N. Engl. J. Med. 281, 627–635. https://doi.org/10.1056/nejm196909182811201 (1969).
Rodriguez-Noriega, E. et al. Evolution of methicillin-resistant Staphylococcus aureus clones in Latin America. Int. J. Infect. Dis. 14, e560-566. https://doi.org/10.1016/j.ijid.2009.08.018 (2010).
Aires De Sousa, M. et al. Three-year assessment of methicillin-resistant Staphylococcus aureus clones in Latin America from 1996 to 1998. J. Clin. Microbiol. 39, 2197–2205. https://doi.org/10.1128/JCM.39.6.2197-2205.2001 (2001).
Sola, C., Cortes, P., Saka, H. A., Vindel, A. & Bocco, J. L. Evolution and molecular characterization of methicillin-resistant Staphylococcus aureus epidemic and sporadic clones in Cordoba Argentina. J. Clin. Microbiol. 44, 192–200. https://doi.org/10.1128/JCM.44.1.192-200.2006 (2006).
Becker, A. P., Santos, O., Castrucci, F. M., Dias, C. & D’Azevedo, P. A. First report of methicillin-resistant Staphylococcus aureus Cordobes/Chilean clone involved in nosocomial infections in Brazil. Epidemiol. Infect. 140, 1372–1375. https://doi.org/10.1017/S095026881100210X (2012).
Teixeira, M. M. et al. Emergence of clonal complex 5 (CC5) methicillin-resistant Staphylococcus aureus (MRSA) isolates susceptible to trimethoprim-sulfamethoxazole in a Brazilian hospital. Braz. J. Med. Biol. Res. 45, 637–643. https://doi.org/10.1590/s0100-879x2012007500065 (2012).
Kuroda, M. et al. Whole genome sequencing of meticillin-resistant Staphylococcus aureus. Lancet 357, 1225–1240. https://doi.org/10.1016/s0140-6736(00)04403-2 (2001).
Imai D. Characteristics of MRSA strains isolated in Japan in 1999. Juntendo Med. J. 49. https://doi.org/10.14789/pjmj.49.343 (2003).
Ito, T. et al. Structural comparison of three types of staphylococcal cassette chromosome mec integrated in the chromosome in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 45, 1323–1336. https://doi.org/10.1128/aac.45.5.1323-1336.2001 (2001).
Aiba, Y. et al. Mutation of RNA polymerase beta-subunit gene promotes heterogeneous-to-homogeneous conversion of beta-lactam resistance in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 57, 4861–4871. https://doi.org/10.1128/AAC.00720-13 (2013).
Kondo, N., Kuwahara-Arai, K., Kuroda-Murakami, H., Tateda-Suzuki, E. & Hiramatsu, K. Eagle-type methicillin resistance: New phenotype of high methicillin resistance under mec regulator gene control. Antimicrob. Agents Chemother. 45, 815–824. https://doi.org/10.1128/aac.45.3.815-824.2001 (2001).
Kuroda, M. et al. Two-component system VraSR positively modulates the regulation of cell-wall biosynthesis pathway in Staphylococcus aureus. Mol. Microbiol. 49, 807–821. https://doi.org/10.1046/j.1365-2958.2003.03599.x (2003).
Yamakawa, J. et al. Heterogeneously vancomycin-intermediate Staphylococcus aureus (hVISA) emerged before the clinical introduction of vancomycin in Japan: A retrospective study. J. Infect. Chemother. 18, 406–409. https://doi.org/10.1007/s10156-011-0330-2 (2012).
Harada, D. et al. Change in genotype of methicillin-resistant Staphylococcus aureus (MRSA) affects the antibiogram of hospital-acquired MRSA. J. Infect. Chemother. 24, 563–569. https://doi.org/10.1016/j.jiac.2018.03.004 (2018).
Dominguez, M. A., de Lencastre, H., Linares, J. & Tomasz, A. Spread and maintenance of a dominant methicillin-resistant Staphylococcus aureus (MRSA) clone during an outbreak of MRSA disease in a Spanish hospital. J. Clin. Microbiol. 32, 2081–2087. https://doi.org/10.1128/JCM.32.9.2081-2087.1994 (1994).
Mato, R. et al. Spread of the multiresistant Iberian clone of methicillin-resistant Staphylococcus aureus (MRSA) to Italy and Scotland. Microb. Drug Resist. 4, 107–112. https://doi.org/10.1089/mdr.1998.4.107 (1998).
Roberts, R. B. et al. Outbreak in a New York City teaching hospital burn center caused by the Iberian epidemic clone of MRSA. Microb. Drug Resist. 4, 175–183. https://doi.org/10.1089/mdr.1998.4.175 (1998).
Sanches, I. S. et al. Evidence for the geographic spread of a methicillin-resistant Staphylococcus aureus clone between Portugal and Spain. J. Clin. Microbiol. 33, 1243–1246. https://doi.org/10.1128/JCM.33.5.1243-1246.1995 (1995).
Lakhundi, S. & Zhang, K. Methicillin-Resistant Staphylococcus aureus: Molecular characterization, evolution, and epidemiology. Clin. Microbiol. Rev. 31. https://doi.org/10.1128/CMR.00020-18 (2018).
Hryniewicz, M. M. & Garbacz, K. Borderline oxacillin-resistant Staphylococcus aureus (BORSA): A more common problem than expected?. J. Med. Microbiol. 66, 1367–1373. https://doi.org/10.1099/jmm.0.000585 (2017).
Goering, R. V., Swartzendruber, E. A., Obradovich, A. E., Tickler, I. A. & Tenover, F. C. Emergence of oxacillin resistance in stealth methicillin-resistant Staphylococcus aureus due to mecA sequence instability. Antimicrob. Agents Chemother. 63, e00558-e619. https://doi.org/10.1128/AAC.00558-19 (2019).
Nelson, L. et al. Community case of methicillin-resistant Staphylococcus aureus Infection. Emerg. Infect. Dis. 12, 172–174. https://doi.org/10.3201/eid1201.050279 (2006).
McDougal, L. K. & Thornsberry, C. The role of beta-lactamase in staphylococcal resistance to penicillinase-resistant penicillins and cephalosporins. J. Clin. Microbiol. 23, 832–839. https://doi.org/10.1128/JCM.23.5.832-839.1986 (1986).
Tomasz, A. et al. New mechanism for methicillin resistance in Staphylococcus aureus: clinical isolates that lack the PBP 2a gene and contain normal penicillin-binding proteins with modified penicillin-binding capacity. Antimicrob. Agents Chemother. 33, 1869–1874. https://doi.org/10.1128/aac.33.11.1869 (1989).
Yoshida, R. et al. Physiological and molecular analysis of a mecA-negative Staphylococcus aureus clinical strain that expresses heterogeneous methicillin resistance. J. Antimicrob. Chemother. 51, 247–255. https://doi.org/10.1093/jac/dkg036 (2003).
Hackbarth, C. J., Kocagoz, T., Kocagoz, S. & Chambers, H. F. Point mutations in Staphylococcus aureus PBP 2 gene affect penicillin-binding kinetics and are associated with resistance. Antimicrob. Agents Chemother. 39, 103–106. https://doi.org/10.1128/aac.39.1.103 (1995).
Nadarajah, J. et al. Identification of different clonal complexes and diverse amino acid substitutions in penicillin-binding protein 2 (PBP2) associated with borderline oxacillin resistance in Canadian Staphylococcus aureus isolates. J. Med. Microbiol. 55, 1675–1683. https://doi.org/10.1099/jmm.0.46700-0 (2006).
Berger-Bachi, B. & Rohrer, S. Factors influencing methicillin resistance in staphylococci. Arch. Microbiol. 178, 165–171. https://doi.org/10.1007/s00203-002-0436-0 (2002).
Roemer, T., Schneider, T. & Pinho, M. G. Auxiliary factors: a chink in the armor of MRSA resistance to beta-lactam antibiotics. Curr. Opin. Microbiol. 16, 538–548. https://doi.org/10.1016/j.mib.2013.06.012 (2013).
Ba, X. et al. Truncation of GdpP mediates beta-lactam resistance in clinical isolates of Staphylococcus aureus. J. Antimicrob. Chemother. 74, 1182–1191. https://doi.org/10.1093/jac/dkz013 (2019).
Banerjee, R., Gretes, M., Harlem, C., Basuino, L. & Chambers, H. F. A mecA-negative strain of methicillin-resistant Staphylococcus aureus with high-level beta-lactam resistance contains mutations in three genes. Antimicrob. Agents Chemother. 54, 4900–4902. https://doi.org/10.1128/AAC.00594-10 (2010).
Argudin, M. A. et al. Genetic diversity among Staphylococcus aureus isolates showing oxacillin and/or cefoxitin resistance not linked to the presence of mec genes. Antimicrob. Agents Chemother. 62. https://doi.org/10.1128/aac.00091-18 (2018).
Matsumoto K et al. The pathogenic strains of Staphylococcus aureus lately isolated in Japan. Chemotherapy 32. https://doi.org/10.11250/chemotherapy1953.32.527 (1984).
Sasaki, T. et al. Multiplex-PCR method for species identification of coagulase-positive staphylococci. J. Clin. Microbiol. 48, 765–769. https://doi.org/10.1128/JCM.01232-09 (2010).
Hiramatsu, K., Kihara, H. & Yokota, T. Analysis of borderline-resistant strains of methicillin-resistant Staphylococcus aureus using polymerase chain reaction. Microbiol. Immunol. 36, 445–453. https://doi.org/10.1111/j.1348-0421.1992.tb02043.x (1992).
Murakami, K. et al. Identification of methicillin-resistant strains of staphylococci by polymerase chain reaction. J. Clin. Microbiol. 29, 2240–2244. https://doi.org/10.1128/JCM.29.10.2240-2244.1991 (1991).
Enright, M. C., Day, N. P., Davies, C. E., Peacock, S. J. & Spratt, B. G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 38, 1008–1015. https://doi.org/10.1128/JCM.38.3.1008-1015.2000 (2000).
Harmsen, D. et al. Typing of methicillin-resistant Staphylococcus aureus in a university hospital setting by using novel software for spa repeat determination and database management. J. Clin. Microbiol. 41, 5442–5448. https://doi.org/10.1128/jcm.41.12.5442-5448.2003 (2003).
Strommenger, B. et al. spa Typing of Staphylococcus aureus as a frontline tool in epidemiological typing. J. Clin. Microbiol. 46, 574–581. https://doi.org/10.1128/JCM.01599-07 (2008).
Becker, K., Roth, R. & Peters, G. Rapid and specific detection of toxigenic Staphylococcus aureus: use of two multiplex PCR enzyme immunoassays for amplification and hybridization of staphylococcal enterotoxin genes, exfoliative toxin genes, and toxic shock syndrome toxin 1 gene. J. Clin. Microbiol. 36, 2548–2553. https://doi.org/10.1128/JCM.36.9.2548-2553.1998 (1998).
Lina, G. et al. Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin. Infect. Dis. 29, 1128–1132. https://doi.org/10.1086/313461 (1999).
Monday, S. R. & Bohach, G. A. Use of multiplex PCR to detect classical and newly described pyrogenic toxin genes in staphylococcal isolates. J. Clin. Microbiol. 37, 3411–3414. https://doi.org/10.1128/JCM.37.10.3411-3414.1999 (1999).
Joensen, K. G. et al. Real-time whole-genome sequencing for routine typing, surveillance, and outbreak detection of verotoxigenic Escherichia coli. J. Clin. Microbiol. 52, 1501–1510. https://doi.org/10.1128/jcm.03617-13 (2014).
Zankari, E. et al. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 67, 2640–2644. https://doi.org/10.1093/jac/dks261 (2012).
Bartels, M. D. et al. Comparing whole-genome sequencing with Sanger sequencing for spa typing of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 52, 4305–4308. https://doi.org/10.1128/jcm.01979-14 (2014).
Kaas, R. S., Leekitcharoenphon, P., Aarestrup, F. M. & Lund, O. Solving the problem of comparing whole bacterial genomes across different sequencing platforms. PLoS ONE 9, e104984. https://doi.org/10.1371/journal.pone.0104984 (2014).
Acknowledgements
This study was supported by a Grant-in-Aid (S1201013) from the Ministry of Education, Culture, Sports, Science, and Technology Supported Program for the Strategic Research Foundation at Private Universities (2012–2016). We appreciate Professor Robert F. Whittier worked at Faculty of Medicine, Juntendo University, for native English proofreading of the final revised manuscript.
Author information
Authors and Affiliations
Contributions
H.Z., Y.U. and K.H. participated in the study design, H.Z., Y.U. and K.H. collected and analyzed clinical information, H.Z., Y.U., Y.L., T.S. and K.H. carried out all microbiological experiments and data analysis, H.Z., Y.U., T.S. and K.H. drafted and revised the manuscript. All authors read and approved the final manuscript. K. H. passed away on June 5, 2020, but he had already read and approved this manuscript before his passing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zuo, H., Uehara, Y., Lu, Y. et al. Genetic and phenotypic diversity of methicillin-resistant Staphylococcus aureus among Japanese inpatients in the early 1980s. Sci Rep 11, 5447 (2021). https://doi.org/10.1038/s41598-021-84481-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84481-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.