Abstract
The sensitivity of electrocardiogram (ECG) criteria to detect left ventricular hypertrophy (LVH) is low, especially in women. We determined sex-specific sensitivities of ECG-LVH criteria, and developed new criteria, using cardiovascular magnetic resonance imaging (CMR). Sensitivities of ECG-LVH criteria were determined in participants of the UK Biobank (N = 3632). LVH was defined when left ventricular mass was > 95% confidence interval (CI) according to age and sex. In a training cohort (75%, N = 2724), sex-specific ECG-LVH criteria were developed by investigating all possible sums of QRS-amplitudes in all 12 leads, and selecting the sum with the highest pseudo-R2 and area under the curve to detect LVH. Performance was assessed in a validation cohort (25%, N = 908), and association with blood pressure change was investigated in an independent cohort. Sensitivities of ECG-LVH criteria were low, especially in women. Newly developed Groningen-LVH criterion for women (QV2 + RI + RV5 + RV6 + SV2 + SV4 + SV5 + SV6) outperformed all ECG-LVH criteria with a sensitivity of 42% (95% CI 35–49%). In men, newly developed criterion ((RI + RV5 + SII + SV2 + SV6) × QRS duration) was equally sensitive as 12-lead sum with a sensitivity of 44% (95% CI 37–51%) and outperformed the other criteria. In an independent cohort, the Groningen-LVH criteria were strongest associated with change in systolic blood pressure. Our proposed CMR sex-specific Groningen-LVH criteria improve the sensitivity to detect LVH, especially in women. Further validation and its association with clinical outcomes is warranted.
Similar content being viewed by others
Introduction
Left ventricular (LV) hypertrophy (LVH) is a marker of the pathophysiologic response of the myocardium to chronic pressure or volume overload and is associated with cardiovascular events1,2. The electrocardiogram (ECG) is an inexpensive, widely available but imperfect tool to detect LVH3. Numerous ECG criteria have been developed to aid in the detection of LVH4,5,6,7. The accuracy of the ECG for diagnosing LVH has been described to be lower in women compared to men8. However, LVH on the ECG is a stronger risk factor for incident cardiovascular events in women than in men9.
In 1949, Sokolow and Lyon developed ECG-LVH criteria based on 147 patients with LVH measured by echocardiography4. The average blood pressure of the individuals with LVH in this study was 197/117 mmHg, values that are rarely seen in contemporary clinical practice. Also, no distinction was made between sexes. Later on, sex differences of ECG parameters were precisely described10,11. Major novelty of the Cornell criteria5, published in 1987, was the stratification for sex and age and increased the sensitivity to detect LVH in women. Most recently developed is the Peguero-Lo Presti criterion with sex-specific thresholds for diagnosing LVH7. So far, all ECG-LVH criteria have been developed in cohorts that used echocardiography to measure LV mass. Cardiovascular magnetic resonance imaging (CMR) provides more accurate and reproducible estimates of LV mass12.
In this study, we aim to determine the accuracy of existing ECG-LVH criteria in 1670 men and 1962 women of the UK Biobank with available CMR and ECG data. LVH was defined based on reference values of LV mass indexed for body surface area (LVMi), measured by CMR13. In addition, we aim to develop the first ECG-LVH criteria, the Groningen-LVH criteria, for both men and women based on CMR data.
Methods
Study design and population
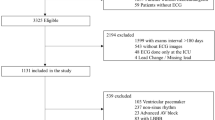
For this study, individuals participating in the CMR substudy of the UK Biobank study with previously determined LV mass on short axis cine series and available 12-lead ECG data were included (N = 4671, Fig. 1)13. The study design of the UK Biobank has been described in detail elsewhere14. This study was covered by the general ethical approval for UK Biobank studies from the NHS National Research Ethics Service (Ref 11/NW/0382). All methods were performed in accordance with the relevant guidelines and regulations. In brief, the UK Biobank is a population based prospective study established for investigating genetic and non-genetic determinants of diseases. Between 2006 and 2010, 502,664 participants aged between 40–69 years were recruited and signed informed consent. Imaging visits of the UK Biobank were initiated in 2015 in which CMR was performed. In addition, participants underwent a 12-lead resting ECG assessment.
Flowchart of the study population. Al individuals of the UK Biobank CMR substudy with available 12-lead ECG data were included in this study. Individuals with another ethnicity than Caucasian, poor ECG quality or with a history of cardiac disease were excluded from analyses. After exclusion, data of 1670 men and 1962 women was available for analyses. AF Atrial fibrillation, BBB bundle branch block, CMR cardiac magnetic resonance imaging, ECG electrocardiogram, LVH left ventricular hypertrophy, PM pacemaker, WPW Wolff-Parkinson-White.
Cardiovascular magnetic resonance
The UK Biobank’s CMR protocol has been described in detail elsewhere15. Long and short axis cine images were acquired on a 1.5 T scanner (MAGNETOM Aera, Syngo Platform VD13A, Siemens Healthcare, Erlangen, Germany). LVH by CMR was defined based on reference values as described by Petersen et al.13, using cutoff values of LVMi > 55 g/m2 in women, LVMi > 72 g/m2 in men aged under 65 years, and LVMi > 70 g/m2 in men aged 65 or older13.
Electrocardiography
12-lead ECG data were provided by the UK Biobank in XML format. The ECGs were made using CASE, CardioSoft Version 6 system by a trained research assistant. Amplitudes of the Q wave, R wave and S wave in all 12 leads, as well as QRS duration were predetermined and extracted from the XML files. ECGs automatically evaluated as poor quality (N = 700) were excluded from analyses, as well as ECGs with left or right bundle branch block, atrial fibrillation or flutter, Wolf Parkinson White, or a pacemaker rhythm. Several widely-used ECG-LVH criteria were calculated and examined (Table 1). Additionally, for the Sokolow-Lyon, Cornell, and 12-lead sum criteria, the products with QRS duration were calculated16.
Analytical approach
The first aim of our study was to determine the sex-specific sensitivity and specificity of existing ECG-LVH criteria. Second aim was to develop the first, sex-specific ECG-LVH criteria using CMR data: the Groningen-LVH criteria. We randomly divided the study population into a training cohort (75%, N = 2724) and a validation cohort (25%, N = 908). Third, we aimed to test the performance of the Groningen-LVH criteria in an independent cohort. All statistical analyses were performed using STATA/SE version 15.1 (StataCorp LLC, College Station, Texas, USA). P-values < 0.05 were considered statistically significant.
Accuracy of established ECG-LVH criteria
Dichotomous baseline characteristics are presented as frequencies and percentages. Continuous variables are summarized by means and standard deviation (SD). Differences between baseline characteristics of men and women with and without LVH were reported; the Chi-square test was used to compare dichotomous variables and differences of continuous variables between groups were evaluated through independent samples t-tests. Sex-specific sensitivity and specificity were reported with related 95% confidence interval (CI). Area under the curve (AUC) analyses, with 95% CI were used to estimate the predicted performance of the existing ECG-LVH criteria.
Development of sex-specific ECG criteria for diagnosing LVH
Performed steps of the data-driven approach used for the development of our sex-specific ECG-LVH criteria are displayed in Supplementary Fig. 1. First, correlations of LVMi with the Q, R and S wave amplitudes in all 12 leads (36 amplitudes in total) were determined in the training population, separately in men and women. Subsequently, for both men and women, all 36 amplitudes were ranked from the amplitude that was highest correlated with LVMi to the amplitude that was lowest correlated. A simple logistic regression analysis was performed with CMR determined LVH as dependent variable and the highest ranked amplitude (the one which was strongest correlated to LVMi) as independent variable, separately for men and women. Next, we added iteratively one extra amplitude, which was next highest ranked, to our model and generated all possible sums of amplitudes (for example, with two amplitudes, three combinations were generated: Amplitude 1, Amplitude 2 and Amplitude 1 + Amplitude 2 etc.). We performed simple logistic regression analyses on LVH with one of the possible sums as independent variable and determined whether one of these models improved the prediction of LVH based on pseudo R2 and AUC. Subsequently, the next highest ranked amplitude was added to the model and all possible sums were generated (3 amplitudes give 7 possible combinations, n amplitudes give 2n-1 possible combinations). The final model was selected when subsequently adding two amplitudes to the model did not show an improvement in both sexes based on pseudo R2 and AUC.
Finally, all possible generated sums of amplitudes were multiplied with QRS duration to assess whether this further improved the model, based on pseudo R2. Threshold of the Groningen-LVH criteria were determined using specificities of 90%. AUC analyses were used to estimate the predicted performance of the new ECG-LVH criteria and receiver operating characteristic (ROC) curves were plotted. Statistical significance of the differences in AUC between the proposed criteria and existing criteria was assessed using the Chi-squared and Hanley McNeil tests.
In the validation cohort, sensitivity, specificity and AUC were calculated for the proposed ECG-LVH criteria in both men and women and ROC curves were plotted.
Performance of the developed ECG-LVH criteria in an independent cohort
An increase in systolic blood pressure (SBP) is causally related to an increase in QRS amplitudes17. For testing the performance of the Groningen-LVH criteria, we examined the association between SBP change (ΔSBP) and QRS amplitudes defined by ECG-LVH criteria for men and women in the independent Lifelines cohort study. The Lifelines cohort study included more than 150.000 individuals of the northern part of the Netherlands18. All participants underwent blood pressure measurements and 12-lead ECGs during the baseline and follow-up visit (median follow-up time 3.8 years, interquartile range 3.0–4.6). Linear regression analyses were performed on QRS amplitudes (ECG-LVH criteria during follow-up) with ΔSBP; age, sex and the concordant baseline ECG-LVH criteria as independent variables. Standardized betas of ΔSBP (making both ΔSBP and ECG-LVH criteria unitless) for all models were obtained and compared for all ECG-LVH criteria to determine which ECG-LVH criteria best correlated with a change in blood pressure.
Results
Study population
A flow chart for selection of the study population (N = 3632) is shown in Fig. 1. Based on the used cutoff values, 79 men and 101 women with LVH were identified. Supplementary Table 1 shows characteristics of the study population, stratified by the presence of LVH and sex. Values of continuous ECG-LVH criteria as well as LVMi were higher in men compared to women in both the LVH as control group. Among the group with LVH, men and women had comparable age and body mass index and a similar prevalence of hypertension and diabetes.
Accuracy of ECG-LVH criteria
Several widely-used ECG-LVH criteria were calculated and examined (Table 1). Sensitivity and specificity of ECG-LVH criteria are displayed in Table 2. In men, 12-lead sum had nominally the highest sensitivity (44% (95% CI 37–51%)) followed by the Peguero-Lo Presti criteria (33% (95% CI 26–40%)). In women, the Peguero-Lo Presti criteria showed the highest sensitivity (31% (95% CI 24–38%)), followed by the Cornell criteria (21% (95% CI 15–27%)). Sensitivities of Sokolow-Lyon, Cornell product, 12-lead sum, 12-lead product and Peguero-Lo Presti were nominally lower in women compared to men (Table 2). Sensitivities of the Sokolow-Lyon product and Cornell criteria were higher in women compared to men. Specificity was above 90% for all ECG-LVH criteria and similar in men and women. Accuracy, as measured by the AUC, was nominally highest for the 12-lead product in men (0.77 (95% CI 0.72–0.82)), followed by the 12-lead sum (0.75 (95% CI 0.69–0.81, Supplementary Table 2)). For women, the Peguero-Lo Presti criteria had nominally the highest accuracy with an AUC of 0.75 (95% CI 0.70–0.80), followed by Sokolow-Lyon product (AUC 0.74 (95% CI 0.69–0.79), Supplementary Table 2).
Development of improved ECG criteria for diagnosing LVH.
Training cohort
In the training cohort (N = 2724), 79 women and 56 men had LVH based on CMR criteria (Supplementary Table 3). In both men and women, R amplitudes in the lateral leads (V4-V6) showed the strongest correlations to LVMi (Fig. 2). Pseudo R2 and AUC of a simple logistic regression analysis with the highest correlated amplitudes as independent variables are displayed in Fig. 3. Iteratively adding the next ranked amplitude and generating all possible sums of these amplitudes improved the accuracy of the model based on pseudo R2 and AUC (Fig. 3). Adding the 15th and 16th amplitude did not improve the association with LVH anymore in either sex (for women reaching a pseudo R2 of 0.177 and AUC of 0.79, for men reaching a pseudo R2 of 0.136 and AUC of 0.76, Fig. 3). Supplementary Tables 4 and 5 provide the R2 and generated sums of the 16 highest correlated amplitudes. Multiplying the amplitudes with QRS duration improved the prediction in men (pseudo R2 of 0.145, AUC 0.78, Supplementary Table 6), but not in women (pseudo R2 of 0.168, AUC 0.79, Supplementary Table 7). For women, the model with best prediction for LVH was:
Heatmap of the correlation of Q, R and S waves with LVMi in the training cohort. Correlations are displayed separately for men and women and the difference between men and women. The darker the color in the heatmap, the stronger the correlation of Q, R and S waves with LVMi. Correlation coefficients between − 0.05 (yellow in women, light purple in men) and 0.30 (brown in women, dark blue in men) were observed in women and men. In both men and women, R and S waves are more often highly correlated to LVMi than Q waves. QRSd QRS duration.
Pseudo R2s (orange square for women, blue round for men) and AUCs (pink triangle for women, green triangle for men) of the generated models including all possible sums of amplitudes in logistic regression analyses on LVH. On the X-axis the number of amplitudes added in each model is displayed. On the left Y-axis, the pseudo R2s of these models in a logistic regression analyses on CMR determined LVH are reported. The right Y-axis displays the concordant AUCs. AUC area under the curve.
For men, the following model reached the best prediction:
AUC was 0.79 (0.75–0.84) for Groningen-LVH criteria in women, which was nominally the most accurate model compared to existing ECG-LVH criteria (Table 3, Fig. 4). Also, AUC for the Groningen-LVH criteria in men was nominally the highest: 0.78 (95% CI 0.71–0.84, Table 3, Fig. 4). Sensitivities of the Groningen-LVH criteria were 39% (95% CI 31–47%, with a threshold of 49.5 mm using a specificity of 90%) in women and 43% (95% CI 35–51%, threshold of 4500 mm*milliseconds, specificity of 90%) in men, and were nominally the highest (Table 4). Applying the sex-specific Groningen-LVH criteria in the opposite sex, a lower accuracy to detect LVH was identified (pseudo R2 of 0.102 and AUC of 0.74 in men; pseudo R2 of 0.135 and AUC of 0.77 in women).
ROC curves for the existing and new developed ECG-LVH criteria in the training cohort. The different colors are ROC curves for each individual ECH-LVH criteria. The left graph shows the ROC curves in women and the right graph the ROC curves in men. The AUC of the Groningen-LVH criteria showed the largest AUC for both men and women. In parentheses the AUC is displayed. LVH left ventricular hypertrophy.
Validation cohort
The validation cohort of 908 individuals, consisted 22 women and 23 men with LVH based on CMR criteria (Supplementary Table 8). Individuals with LVH in the validation cohort were similar to individuals in the training cohort (Supplementary Table 9). Correlation analyses of ECG amplitudes with LVMi showed similar patterns as in the training cohort (Supplementary Fig. 2). For women, the sensitivity of the Groningen-LVH criteria was nominally the best (50% (95%CI 35–64%)), followed by the Peguero-Lo Presti criteria (27% (95% CI 14–40%), Table 5). For men, only 12-lead sum had nominally, but not significantly, a higher sensitivity (52% (95% CI 37–67%)), compared to the Groningen-LVH criteria with a sensitivity of 48% (95% CI 33–63%), Table 5. Applying the new criteria to the validation cohort, the diagnostic accuracy was nominally higher compared to the accuracy in the training cohort (AUC 0.84 (95% CI 0.76–0.93) in women and 0.82 (95% CI 0.74–0.91%) in men, Table 6 and Supplementary Fig. 3). Combining the training and validation cohort, accuracy of the Groningen-LVH criteria for women outperformed all other criteria (Supplementary Table 2), using the Chi-squared test. Using the Hanley McNeil test, accuracy of the Groningen-LVH criteria for women was similar to Peguero-Lo Presti criterium. For men, the Groningen-LVH criteria had nominally the same sensitivity as 12-lead sum (Table 2). AUC was nominally the largest for the Groningen-LVH criteria in men but did not differ significantly from 12-lead sum and 12-lead product (Supplementary Table 2, using Chi-squared test). Using Hanley McNeil test, the Groningen-LVH criteria for men did not differ significantly from 12-lead sum, 12-lead product and Sokolow-Lyon product.
Performance of the new ECG-LVH criteria in an independent cohort
Standardized betas of ΔSBP on ECG-LVH criteria assessed by linear regression analyses are displayed in Supplementary Table 10. An increase of one SD in ΔSBP increases the Groningen-LVH criteria with 0.095 SDs in women and with 0.068 SDs in men, which were nominally the largest effects of ΔSBP as compared to other ECG-LVH criteria.
Discussion
In this study, accuracies of existing ECG-LVH criteria were determined in 1,670 men and 1,962 women participating in the UK Biobank with available CMR-derived LVM measurements and 12-lead ECG data. Sensitivity of established ECG-LVH criteria is low, especially in women. The lower sensitivity of ECG-LVH criteria in women has been reported earlier19. Antihypertensive treatment can decrease LVH and improve left ventricular dysfunction20. The higher chance of false negative findings of LVH in women may therefore lead to undertreatment of LVH in women and the incidence of preventable cardiovascular events21. In the current study, we therefore developed the sex-specific Groningen-LVH criteria, which performed significantly better than the previously established criteria in women.
Women have lower ECG signal amplitudes than men10, which may be one of the explanations of the lower sensitivity of ECG-LVH criteria in women. Intuitively, the relatively lower QRS voltages in women could be due to the presence of breast tissue. However, it has been reported that breast tissue accounts for less that 1% of the total variation of QRS voltages22; a variation that may not be different from the normal day to day variation of ECG voltages23. Women with LVH in our study did not have a higher BMI compared to men, another factor that has been described to be inversely associated with sensitivity19. In addition to female sex, one study has reported age, blood pressure, relative wall thickness and the use of antihypertensive medication as predictors of this discrepancy24. In our study population, there was no difference in age or the presence of hypertension between men and women with LVH. Also, there was no sex interaction for mass to volume ratio between individuals with and without LVH in our study (sex interaction P-value 0.32 in the training cohort). Our findings therefore suggest that the sex differences in sensitivity may largely be explained by the lower absolute LVMi in women compared to men and the absence of sex-specific cut off points for most established ECG-LVH criteria.
Most of the ECG-LVH criteria were developed between 1940 and 1990. Since then, major changes have occurred in lifestyle, prevention and treatment of cardiovascular disease. Study populations in whom these criteria are developed may therefore differ from the contemporary population. Furthermore, the established ECG-LVH criteria were developed and validated using echocardiography as reference4,5,6,7. CMR provides more accurate, precise and reproducible estimates of LV mass12. Our reported sensitivities and specificities may therefore be a more precise measure of the performance of ECG criteria in the current general population.
For most of the existing ECG-LVH criteria, no distinction has been made between men and women. Sex differences of ECG amplitudes and durations are nowadays precisely described10,11 and suggest different cut off points and/or other criteria for men and women to detect LVH using ECG. Thus, the most important finding of the present study is the development of sex-specific ECG-LVH criteria, of which the accuracy is similar in men and women.
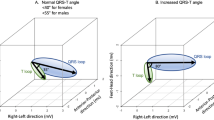
The development of our new sex-specific ECG criteria using CMR data, started with determining the correlation of Q, R and S amplitudes of all 12 leads with LVMi for both men and women. In both sexes, Q waves were less often highly correlated to LVMi than R or S waves. The Q wave is a reflection of the depolarization of the septum, conduction system and endomyocardial fibers of the left ventricle. The R and S wave are related to the depolarization of the myocardial and epicardial wall of the left ventricle25. Changes in voltages due to LVH may therefore be better represented in these waves. For both men and women, the most accurate combination of amplitudes was generated with a large proportion of amplitudes of the lateral leads (I, V5 and V6), which represent the electrical activity from the vantage point of the lateral wall of left ventricle. Since the electrical vector of the left ventricle is enhanced in LVH, R-waves in lateral leads and S waves in right sided chest leads (V1, V2) will increase as a result as well. As described by Peguero et al. it is plausible that changes in voltage that occur in patients with mild to moderate LVH are better represented by the latter part of the QRS complex, which corresponds to the S wave7. Our proposed criteria suggest that both R and S waves are important predictors of LVH and that the sum of a combination of R and S waves is most accurate.
Multiplying the sum of amplitudes with QRS duration improved the accuracy of the model for men, but not the model for women. Molloy et al. described the improvement of detecting LVH by the product of QRS duration with voltage16. However, the majority of the individuals in the study of Molloy et al. were men and no subgroup analyses was performed to see whether the product of QRS duration improved the prediction in both sexes. In a population with LVH due to underlying valvular regurgitation (volume overload which mainly leads to eccentric hypertrophy), accuracy of ECG-LVH criteria improved by multiplying the sum of amplitudes with QRS duration in both men and women26. In our study population, the majority (60%) of the individuals with LVH had hypertension and therefore pressure overload of the heart. It has been reported that male and female hearts under pressure overload respond primarily with concentric hypertrophy. However, women stay more in concentric hypertrophy, whereas men more often develop eccentric hypertrophy27. This sex difference in remodeling may be an explanation of the improvement of the ECG-LVH criteria multiplied by QRS duration in men, but not in women. Future studies, investigating ECG-LVH criteria separately for eccentric and concentric hypertrophy, are needed to validate this hypothesis.
Limitations
For the development of our sex-specific Groningen-LVH criteria we generated the most predictive models instead of the simplest. We are aware that calculation of our developed criteria by hand may be more time consuming than calculating the existing, simple criteria. However, for computer based algorithms used by ECG software, this complexity does not matter and will therefore give the best risk prediction for LVH.
Our proposed LVH criteria for women improved the accuracy for diagnosing LVH in both the training and validation cohort. For men, our proposed criteria had nominally the highest sensitivity in the training cohort, but 12-leadsum had nominally the highest sensitivity in the validation cohort. In the complete cohort, the sensitivity and AUC of our proposed criteria in men was as high as the 12-lead sum. Further validation in a larger population is therefore warranted for our proposed male criterion.
As we excluded individuals with a non-Caucasian ethnicity, and individuals with previous cardiovascular disease, the accuracy of our proposed criteria might not be generalizable and needs to be validated in these populations.
Conclusion
The sensitivity of existing ECG criteria to detect LVH measured by CMR is low, especially in women. Our proposed sex-specific Groningen-LVH criteria are the first criteria generated with CMR as reference, and improve the accuracy to detect LVH, especially in women. Further validation of our criteria in independent cohorts is warranted.
Data availability
The data that support the findings of this study are available from UK Biobank, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the UK Biobank.
Abbreviations
- AUC:
-
Area under the curve
- ECG:
-
Electrocardiogram
- CI:
-
Confidence interval
- CMR:
-
Cardiovascular magnetic resonance
- LV:
-
Left ventricle
- LVH:
-
Left ventricular hypertrophy
- LVMi:
-
Left ventricular mass indexed to body surface area
- ROC:
-
Receiver operating characteristic
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
References
Porthan, K. et al. ECG left ventricular hypertrophy as a risk predictor of sudden cardiac death. Int. J. Cardiol. 276, 125–129 (2019).
Antikainen, R. L. et al. Left ventricular hypertrophy is a predictor of cardiovascular events in elderly hypertensive patients: Hypertension in the very elderly trial. J. Hypertens. 34, 2280–2286 (2016).
Bacharova, L. & Estes, E. H. Left ventricular hypertrophy by the surface ECG. J. Electrocardiol. 50, 906–908 (2017).
Sokolow, M. & Lyon, T. P. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am. Heart J. 37, 161–186 (1949).
Casale, P. N., Devereux, R. B., Alonso, D. R., Campo, E. & Kligfield, P. Improved sex-specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocardiograms: Validation with autopsy findings. Circulation 75, 565–572 (1987).
Dollar, A. L. & Roberts, W. C. Usefulness of total 12-lead QRS voltage compared with other criteria for determining left ventricular hypertrophy in hypertrophic cardiomyopathy: Analysis of 57 patients studied at necropsy. Am. J. Med. 87, 377–381 (1989).
Peguero, J. G. et al. Electrocardiographic criteria for the diagnosis of left ventricular hypertrophy. J. Am. Coll. Cardiol. 69, 1694–1703 (2017).
Okin, P. M., Roman, M. J., Devereux, R. B. & Kligfield, P. Gender differences and the electrocardiogram in left ventricular hypertrophy. Hypertension 25, 242–249 (1995).
Porthan, K. et al. ECG left ventricular hypertrophy is a stronger risk factor for incident cardiovascular events in women than in men in the general population. J. Hypertens. 33, 1284–1290 (1995).
Simonson, E. et al. Sex Differences in the electrocardiogram. Circulation 22, 598–601 (1960).
van der Ende, M. Y., Siland, J. E., Snieder, H., van der Harst, P. & Rienstra, M. Population-based values and abnormalities of the electrocardiogram in the general Dutch population: The LifeLines cohort study. Clin. Cardiol. 40, 865–872 (2017).
Katz, J. et al. Estimation of human myocardial mass with MR imaging. Radiology 169, 495–498 (1988).
Petersen, S. E. et al. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J. Cardiovasc. Magn. Reson. 19, 18–017 (2017).
Sudlow, C. et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Petersen, S. E. et al. UK Biobank’s cardiovascular magnetic resonance protocol. J. Cardiovasc. Magn. Reson. 18, 8–016 (2016).
Molloy, T. J., Okin, P. M., Devereux, R. B. & Kligfield, P. Electrocardiographic detection of left ventricular hypertrophy by the simple QRS voltage-duration product. J. Am. Coll. Cardiol. 20, 1180–1186 (1992).
Van Der Ende, M. Y. et al. Causal pathways from blood pressure to larger QRS amplitudes: A mendelian randomization study. Sci. Rep. 8, 10290–11018 (2018).
van der Ende, M. Y. et al. The LifeLines Cohort Study: Prevalence and treatment of cardiovascular disease and risk factors. Int. J. Cardiol. 228, 495–500 (2017).
Levy, D. et al. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation 81, 815–820 (1990).
Wachtell, K. et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment: The losartan intervention for endpoint reduction in hypertension (LIFE) study. Circulation 105, 1071–1076 (2002).
Ghali, J. K. et al. The prognostic role of left ventricular hypertrophy in patients with or without coronary artery disease. Ann. Intern. Med. 117, 831–836 (1992).
Rautaharju, P. M., Park, L., Rautaharju, F. S. & Crow, R. A standardized procedure for locating and documenting ECG chest electrode positions: Consideration of the effect of breast tissue on ECG amplitudes in women. J. Electrocardiol. 31, 17–29 (1998).
Angeli, F. et al. Day-to-day variability of electrocardiographic diagnosis of left ventricular hypertrophy in hypertensive patients Influence of electrode placement. J. Cardiovasc. Med. 7, 812–816 (2006).
Petersen, S. S. et al. Factors associated with diagnostic discrepancy for left ventricular hypertrophy between electrocardiography and echocardiography. Blood Press. 26, 54–63 (2017).
Ramanathan, C., Jia, P., Ghanem, R., Ryu, K. & Rudy, Y. Activation and repolarization of the normal human heart under complete physiological conditions. Proc. Natl. Acad. Sci. U.S.A. 103, 6309–6314 (2006).
Okin, P. M., Roman, M. J., Devereux, R. B. & Kligfield, P. Time-voltage area of the QRS for the identification of left ventricular hypertrophy. Hypertension 27, 251–258 (1996).
Regitz-Zagrosek, V. & Kararigas, G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol. Rev. 97, 1–37 (2017).
Author information
Authors and Affiliations
Contributions
This research has been conducted using the UK Biobank resource under application number 12010. We would like to thank N.V., PhD, R.N.E., MD, PhD, M.A.S., BSc, Y.H., MSc, H.G., MD, and J.-W.B., BEng (Department of Cardiology, University of Groningen, University Medical Center Groningen, Groningen, the Netherlands), for their contributions to the extraction and processing of data in the UK Biobank. None of the contributors received compensation except for their employment at the University Medical Center Groningen.
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Ende, M.Y., Hendriks, T., van de Vegte, Y. et al. The Groningen electrocardiographic criteria for left ventricular hypertrophy: a sex-specific analysis. Sci Rep 11, 6662 (2021). https://doi.org/10.1038/s41598-021-83137-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-83137-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.