Abstract
Strain elastography of the uterine cervix may be useful in the diagnosis and prediction of obstetric complications. The inability to obtain quantitative results, with only the possibility of visual semiquantitative evaluation of the obtained elastograms, has been the limitation of the method thus far. E-Cervix is a software program that uses intrinsic compression to excite tissue and allows the evaluation of quantitative parameters on the basis of pixel distribution in an elastogram. The aim of this study was to assess the repeatability and reproducibility of quantitative cervical strain elastography (E-Cervix) of the uterine cervix and to assess the correlation of the obtained parameters with selected clinical features of patients in the third trimester of pregnancy. In total, 222 patients participated in the study. We assessed 5 ultrasound parameters: elasticity index (ECI), hardness ratio (HR), internal os strain (IOS), external os strain (EOS) and IOS/EOS ratio. Each study was performed according to a predetermined standardized protocol. For all assessed elastographic parameters, we obtained good intra- and interobserver reproducibility. The interclass correlation coefficient (ICC) ranged from 0.77 to 0.838 for intraobserver variability and from 0.771 to 0.826 for interobserver variability. We demonstrated a significant correlation of some obtained elastographic parameters with the basic clinical features of patients, such as age, the number of previous caesarean sections, pregnancy weight and BMI. In each case, the correlation was very low. Quantitative elastographic assessment with the use of E-Cervix is characterized by good repeatability. Some clinical features may affect the value of the parameters obtained. The clinical relevance of this interference requires further investigation.
Similar content being viewed by others
Introduction
Ultrasound elastography (USE) of human organs has already found its use in many medical specializations. USE is used, among other applications, in the evaluation of the fibrosis process affecting the liver and transplanted kidneys. In the case of focal lesions in the breast, thyroid, liver and prostate, USE can be used as a supplement to other imaging techniques, allowing for better classification of radiological changes and a reduction in the percentage of organ biopsies1. In obstetrics, it seems natural to employ USE to evaluate the consistency of the cervix. Cervical hardness is a standard element assessed in the bimanual examination of the pelvis during pregnancy, and it is also an element of the Bishop scale assessment2. Consistency examination can be used in the prediction of preterm labour3,4, in the prediction of a spontaneous onset of labour and in evaluations of the effectiveness of the induction of labour (IOL)5,6. The two main techniques of USE are strain elastography (SE) and shear wave elastography (SWE), differing in terms of the stress type applied to tissue.
To date, SE has been limited by its presentation of results only in the form of an elastogram, i.e., a "colour map" of the organ, in which the intensity of the colour corresponds to the stiffness of the organ (qualitative assessment). The elastogram can then be visually assessed with the possible use of semiquantitative scales7. The E-Cervix (Samsung Medison), a semiautomatic system for the elastographic evaluation of the cervix, meets the expectations of the quantitative approach to the elastogram. In this method, the cervix is examined with the use of SE—in which the necessary vibrations of the tissue are excited by intrinsic factors—mainly due to the pulse wave of the pelvic vessels carried by the surrounding tissues8. As part of the test results, in addition to the colour elastogram, we also obtained measurable quantitative parameters calculated on the basis of the pixel colour distribution within the elastogram. The parameters obtained, together with their definitions, are listed in Table 1.
Objective
The study was intended to assess the repeatability and reproducibility of the parameters obtained in the E-Cervix examination.
The secondary aim was to correlate the obtained parameters with the basic demographic data of the female patients.
Methods
Female patients in their third trimester of pregnancy hospitalized in the Pregnancy Pathology Department of the Gynaecology and Obstetrics Clinic of the Provincial Combined Hospital in Kielce in 2020 (third degree of referentiality) participated in the study. We received approval to examine the patients for research purposes from the bioethics commission at Jan Kochanowski University in Kielce (approval number—55/2019). All methods were performed in accordance with the relevant local regulations and guidelines of the ethical commission. All participants gave informed consent for ultrasonographic diagnosis and participation in the study. In this study, we used a Samsung WS80A ultrasound device with a 6 MHz vaginal ultrasound transducer and E-Cervix software.
Sample image of the cervix obtained in the study. (a) The dashed white line represents the endocervical canal; (b) the internal and external cervical os are represented by the white circular sectors; and (c) the green 6-point sector represents the ROI. In the lower right corner, you can see the values of the E-Cervix parameters.
The demographic characteristics of the sample group are presented in Table 2. Since the study was intended to assess a diagnostic method, the patients were not selected according to the reason for hospitalization. Patients with cervical Naboth cysts, multiple pregnancies, cervical procedures (conization, loop electrosurgical excision procedure), ruptured membranes, cervical cerclage or obstetrical pessary placement, and no clear visualization of internal cervical os were excluded from the study. Two ultrasound specialists were involved in the study. For the assessment of interobserver variability, two specialists performed E-Cervix examination according to a standard protocol immediately after each other, each blinded to the other operator's result. Intraobserver variability was assessed by having the same ultrasound specialist perform the examination two times. The ultrasound transducer was removed from the vagina between the examinations. The protocol of the examination is presented in Table 5. To standardize and compare results from different centres, we used an examination protocol based on the method presented by Seol et al.10 An example of ultrasound images with elastograms and ROIs is shown in Fig. 1. We compared the quantitative E-Cervix parameters obtained (description in Table 1).
Statistical analysis
For the description of the group, we used the median as a measure of the central tendency for a distribution different from normal (p < 0.05 in the Shapiro–Wilk test) and the arithmetic mean for a distribution close to normal. As a measure of scatter, the interquartile range (IQR) and the standard deviation (SD) were employed. To evaluate the intra- and interobserver reproducibility of elastographic cervical parameters, the interclass correlation coefficient (ICC) was calculated. Based on the available literature, it was found that a certain level of interrater and intrarater agreement already exists (in none of the ICC studies found was it less than 0.5)9,12. We estimated a minimal sample size based on the table presented by Bujang et al.13 (with a prespecified null hypothesis set at 0.5 and a prespecified minimal alternative hypothesis set at 0.7, alpha = 0.05 and power = 0.9). Based on these calculations, the minimal sample size to properly assess the given ICC was 87 subjects. The ICC values were interpreted as follows: > 0.9—excellent reproducibility, 0.75–0.9—good reproducibility, 0.5–0.75—moderate reproducibility, and < 0.5—poor reproducibility. Baseline patient parameters were correlated with those assessed in the E-Cervix. In the correlation analysis, the arithmetic mean of two obtained measurements was used. Spearman's rank correlation coefficient (Spearman's rho) was used to assess the correlation. Statistical analysis was performed with SPSS 27.0.1.0 (IBM Company) and Statistica 13.1 (Tibco Software). A p value < 0.05 was considered to be statistically significant.
Results
A total of 222 Caucasian patients were enrolled in the study: 125 patients in the group assessing intraobserver variability (79 for rater A and 46 for rater B) and 97 patients in the group assessing interobserver variability (each patient assessed by raters A and B). The demographic characteristics of the patients and the correlation with the individual elastographic parameters are presented in Table 3. We found a very weak positive correlation between age, the number of previous caesarean sections (CSs) and HR (0.14 and 0.16, respectively); a very weak negative correlation between BMI and ECI (− 0.17); and a very weak positive correlation between BMI and IOS (0.15). Moreover, we observed a weak positive correlation between IOS/EOS and patient weight (0.21) and a very weak negative correlation between EOS and patient age (− 0.15). A moderate negative correlation between cervical length and gestational age (− 0.39) was also found. The remaining elastographic parameters did not significantly correlate with the baseline characteristics of the patients.
The repeatability and reproducibility of quantitative E-Cervix parameters are shown in Table 4. All ICCs received in the intra- and interobserver variability categories were in a good range of reproducibility. The cervical length measurement showed excellent reproducibility. The Bland–Altman plots are shown in Fig. 2. The lowest consistency in terms of repeatability was obtained in the IOS measurement, where 7 (5.6%) of the measurement pairs were outside the level of agreement (LoA—mean of difference ± 1.96 of standard deviation). The lowest agreement in reproducibility was obtained for the EOS measurement, where 4 (4.1%) pairs of measurements were outside the LoA (Table 4., Fig. 1).
Discussion
The results of our research show that the semiautomatic system for cervical elastography measurement is characterized by high repeatability. This is also confirmed by the data available in the literature. In none of the studies available in the literature was the ICC of any elastographic parameter lower than 0.63310,12,14. EOS was the parameter with the lowest repeatability in each of the available studies. This parameter has the greatest sensitivity to the measurement conditions due to the proximity of the external outlet of the external uterine os to the ultrasound transducer head. The influence of measurement conditions on the EOS value is confirmed by clinical trials with gradual compression of the ultrasound transducer head on the uterine cervix. The EOS value significantly decreases with increasing pressure of the transducer head12.
In the study conducted by the Korean Research Group of Cervical Elastography10, moderate to excellent reproducibility was achieved depending on the elastographic parameter tested. The intraobserver ICC ranged from 0.633 to 0.723, and the interobserver ICC ranged from 0.814 to 0.977. In our study, we used the same measurement protocol (measurement conditions, ROI determination), whereas the differences concerned the postprocessing method during the database creation. In our study, we wanted the conditions to be closer to real-world settings. We wanted to evaluate the reproducibility of the elastographic parameters directly obtained in research by operators using the same measurement protocol, performing the entire research procedure again.
Seul et al.10 used external quality control, rejecting measurements with inadequate images (9.8%), while in some cases, remeasurement was used by an expert using precaptured elastograms (10%). Similarly, for the interobserver variability assessment, the second operator used precaptured images to calculate elastographic parameters without retesting. Our study seems to be more adapted to clinical conditions. In each case, the second operator, blinded to the results of the first measurement, performed the examination from the beginning after removing and reinserting the ultrasound transducer into the vagina. In theory, the lack of external control of elastograms should result in less agreement among observers, but nevertheless, the repeatability obtained in our study is equally high. In our opinion, this is evidence of high repeatability when testing is performed according to strictly defined procedures included in a standardized protocol.
One of the variables having a considerable impact on the data obtained in elastography is the degree of pressure of the transducer head on the examined organ and vibrations of the operator's hand transmitted to the head, which results directly from the measurement method (free-hand ultrasound system). Direct pressure of the ultrasound transducer head against the uterine cervix affects both its length and the parameters of the elastogram12. The analysis of the pairs of measurements outside the level of agreement from our study shows differences in the distance between the transducer head and the uterine cervix canal. Excessive pressure on the transducer head, in addition to increasing the cervical length, also affects the increase in the HR value and the decrease in the EOS value and thus the increase in the IOS/EOS ratio12.
Therefore, it seems that the key to achieving high reproducibility is the unification of the rules for transducer head placement with the recommendations for cervical measurements in the second trimester of pregnancy15 and the standard protocol described in the literature (also used in our study)10. This procedure will allow for the comparison of the results of multicentre studies and research in the application of E-Cervix in clinical practice. The influence of the transducer head movements on the obtained values, in the case of the E-Cervix software, is limited by the reliability indicator. This indicator is a stack of colour blocks displaying acquisition reliability. In the autofreeze mode, the image freezes only when the ultrasound device obtains a sufficient number of steady frames to provide satisfactory data, which is symbolised by all the indicator blocks turning green8.
Strain elastography is a diagnostic method possessing some other technical limitations that may alter the results of the measurements. These limitations are particularly noticeable in methods employing an internal impulse to stimulate the tissue under study. In this case, the impulse power is difficult to control and standardize, and vectors of power from various sources (e.g., vibrations transmitted from the vessels, respiratory movements, and cardiac activity) may interfere with each other. In such cases, although physiological motion is required to perform the analysis, such motion also exhibits unpredictable variability, which may alter the outcome of the examination1. The impulse power may be influenced by the height of the pulse wave, the passage of the ultrasound wave through tissue barriers of various densities and the attenuation of the signal in the adipose tissue or amniotic fluid. In the literature on this subject, the results of the analysis of the correlation between the parameters obtained in the E-Cervix and baseline clinical factors are available. No correlation with the patient’s heart rate, mean arterial blood pressure, uterine artery pulsation or resistance index was found10. The variable significantly correlated with certain E-Cervix parameters in the quoted work was the patient's BMI, which was positively correlated with EOS and ECI readings and negatively correlated with HR. The correlation of BMI with several parameters (ECI and IOS) was also observed in our work. The correlation was very low (Spearman’s rho < 0.2) in both investigations10. In our study, we also demonstrated that several of the parameters may correlate with variables such as age (HR, EOS), number of previous CSs (HR) and patient weight (IOS/EOS). The observed relationship of HR with E-Cervix parameters may be the result of the degeneration of cervical connective tissue fibres under the influence of ageing and healing. The positive correlation of IOS/EOS parameters with weight may be a result of increased intra-abdominal pressure transferred to the internal cervical os in obese patients. In all cases, the correlation, although statistically significant, was very low (≤ 0.2), casting doubt on its clinical relevance; however, further research is required to assess the clinical implications. Similar relationships are observed in studies assessing the uterine cervix with SWE, and its stiffness measured with this method increases with age. In the cited study, no relationship was found between cervical stiffness and patient BMI16. Nevertheless, the analysis of correlation in our sample group may be subject to limitations due to the selection of the sample, which included patients hospitalized at the pregnancy pathology unit rather than a population of patients in physiological pregnancy.
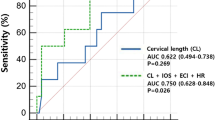
The reproducibility assessment of a diagnostic method is always the foundation for research with higher clinical relevance. The quantitative result obtained on the basis of the elastogram allows a less subjective assessment of the uterine cervix compared to the semiquantitative scales typically used in strain elastography and creates an opportunity to compare results across research centres. The uterine cervix undergoes a natural process of softening as pregnancy progresses. There are initial reports in the literature regarding the sensitivity of the obtained E-Cervix parameters to physiological changes in cervical consistency for repeated measurements performed on the same pregnant patient as the pregnancy progresses9 Further natural development of this diagnostic method would involve its application in the prediction of preterm labour and the effectiveness of labour induction. Research demonstrates the usefulness of semiquantitative scales for these indications7,17, and there are initial reports of the use of E-Cervix for this purpose. In one of the reports published in 2019, the inclusion of the ECI parameter in the logistic regression model containing three other parameters (CL, prepregnancy BMI and gestational age at examination) for patients in the second trimester of pregnancy with cervix length ≥ 1.5 cm significantly increased the overall diagnostic accuracy of the test compared to screening based solely on CL4. In the perinatal period, some of the E-Cervix parameters (HR, IOS) in combination with CL allowed for increasing the predictive capacity of the model evaluating the chance of vaginal delivery in the next 24 h during labour induction with the use of a dinporoston vaginal insert6. Perhaps further research in elastography will contribute to its wider use in obstetrics. We are confident that the possibility of quantitatively evaluating the elastogram by the method studied by us, as well as the high repeatability we have obtained, are the features that will allow the performance of broader research in various clinical situations.
Conclusion
All quantitative parameters in cervical elastography using the E-Cervix module are characterized by high repeatability and reproducibility. The obtained quantitative parameters correlate with some clinical features of the patients. The clinical relevance of this correlation requires further research.
Data availability
The dataset used for this study was uploaded to a public repository and is available at this URL: https://doi.org/10.17605/OSF.IO/6D9E7.
References
Sigrist, R. M. S., Liau, J., Kaffas, A. E., Chammas, M. C. & Willmann, J. K. Ultrasound elastography: review of techniques and clinical applications. Theranostics 7, 1303–1329 (2017).
Bishop, E. H. Pelvic scoring for elective induction. Obstet. Gynecol. 24, 266–268 (1964).
Baños, N. et al. Mid-trimester sonographic cervical consistency index to predict spontaneous preterm birth in a low-risk population. Ultrasound Obstet. Gynecol. 51, 629–636 (2018).
Park, H. S. et al. Addition of cervical elastography may increase preterm delivery prediction performance in pregnant women with short cervix: a prospective study. J. Korean Med. Sci. 34, e68 (2019).
Meier, K., Parrish, J. & D’Souza, R. Prediction models for determining the success of labor induction: a systematic review. Acta Obstet. Gynecol. Scand. 98, 1100–1112 (2019).
Zhou, Y. et al. Predictive value of cervical length by ultrasound and cervical strain elastography in labor induction at term. J. Int. Med. Res. 49, 300060520985338 (2021).
Swiatkowska-Feund, M., Traczyk-Łoś, A., Preis, K., Łukaszuk, M. & Zielińska, K. Prognostic value of elastography in predicting premature delivery. Ginekol. Pol. 85, 204–207 (2014).
R&D Samsung Medison. E-Cervix a tool for measuring the stiffness of cervix using elastographic images. https://www.samsungmedison.com (2018).
Du, L. et al. Quantitative elastography of cervical stiffness during the three trimesters of pregnancy with a semiautomatic measurement program: a longitudinal prospective pilot study. J. Obstet. Gynaecol. Res. 46, 237–248 (2020).
Seol, H. J. et al. Standardization of measurement of cervical elastography, its reproducibility, and analysis of baseline clinical factors affecting elastographic parameters. Obstet. Gynecol. Sci. 63, 42–54 (2020).
To, M. S., Skentou, C., Chan, C., Zagaliki, A. & Nicolaides, K. H. Cervical assessment at the routine 23-week scan: standardizing techniques. Ultrasound Obstet. Gynecol. 17, 217–219 (2001).
Zhang, L. et al. Quantitative cervical elastography: a new approach of cervical insufficiency prediction. Arch. Gynecol. Obstet. 301, 207–215 (2020).
Bujang, M. A. & Baharum, N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: a review. Arch. Orofac. Sci. 12, 1–11 (2017).
Rizzo, G. et al. Sonoelastographic assessment of the uterine cervix in the prediction of imminent delivery in singleton nulliparous women near term: a prospective cohort study. J. Ultrasound Med. 40, 559–568 (2021).
McIntosh, J., Feltovich, H., Berghella, V. & Manuck, T. The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. Am. J. Obstet. Gynecol. 215, B2-7 (2016).
Castro, L. et al. Influence of epidemiological characteristics (age, parity and other factors) in the assessment of healthy uterine cervical stiffness evaluated through shear wave elastography as a prior step to its use in uterine cervical pathology. Arch. Gynecol. Obstet. 302, 753–762 (2020).
Swiatkowska-Freund, M. & Preis, K. Elastography of the uterine cervix: implications for success of induction of labor. Ultrasound Obstet. Gynecol. 38, 52–56 (2011).
Acknowledgements
This project was financed under a Ministry of Science and Higher Education program called “Regional Initiative of Excellence” in the years 2019–2022, project no. 024/RID/2018/19, amount of financing: 11 999 000,00 zł.
Author information
Authors and Affiliations
Contributions
J.M.: ultrasonographic examinations, statistical analysis, interpretation of results, article draft. M.M.: article draft, interpretation of results, J.P. ultrasonographic examinations K.D.: data collection. A. M.: database research for literature. G.S.: result interpretation, article draft. M.S.: content supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mlodawski, J., Mlodawska, M., Plusajska, J. et al. Repeatability and reproducibility of quantitative cervical strain elastography (E-Cervix) in pregnancy. Sci Rep 11, 23689 (2021). https://doi.org/10.1038/s41598-021-02498-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-02498-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.