Abstract
Cervical elastography might be an objective method for evaluating cervical ripening during pregnancy, but its usefulness has not been fully investigated. We examined the significance of cervical elastography in the last trimester of pregnancy. Cervical elastography was performed at weekly checkups after 36 weeks of gestation in 238 cases delivered at our hospital from 2017 to 2018. The correlation with the onset time of natural labor, which is an index for judging maternal delivery preparation status, was examined. A total of 765 examinations were conducted, and cervical stiffness determined by cervical elastography was positively correlated with the Bishop score (r = 0.46, p < 0.0001). When examined separately for each week, only the examinations performed at 39 weeks were associated with the onset of spontaneous labor up to 7 days later (p = 0.0004). Furthermore, when stratified and analyzed by the Bishop score at 39 weeks of gestation, cervical elastography was associated with the occurrence of spontaneous labor pain for up to seven days in the groups with Bishop scores of 3–5 and 6–8 (p = 0.0007 and p = 0.03, respectively). In conclusion, cervical elastography at 39 weeks of pregnancy is useful for judging the delivery time.
Similar content being viewed by others
Introduction
Assessing maternal labor readiness is a basic matter of pregnancy and delivery management. Predicting the onset of spontaneous labor is important to encourage pregnant women to prepare for labor. The Bishop score1, as determined by pelvic examination, has been used to evaluate the preparatory state of delivery. However, this pelvic examination is subjective, and the error between examiners is large. Additionally, the pelvic examination fingers cannot reach in some cases, and pain and discomfort might occur, necessitating a more objective and less invasive evaluation method.
During pregnancy, in the mature cervical canal, neutrophil infiltration is observed, and local cytokines are produced. These processes cause the swollen cervical tissue to soften2,3. Cervix ripening results in ease of cervix opening and forms the birth canal. Moreover, cytokine production and decreased progesterone activity also cause uterine contractions and are associated with labor onset4.
Elastography is a technique that shows the hardness of the tissue in color and can be divided into strain elastography and shear wave elastography. Elastography has been useful for the diagnosis of breast cancer and liver cirrhosis and is used in daily practice. An elastographic evaluation of cervical softness using a transabdominal probe has also been reported5,6,7.
Furthermore, since 2007, cervical elastography has been performed using a transvaginal probe, and its clinical application is expected. Cervical elastography has been useful for predicting subsequent premature birth and vaginal delivery during the induction of labor. However, another report did not predict the success rate of transvaginal delivery8.
We consider that cervical elastography as an indicator of the preterm birth rate and success rate of labor induction is not a pure evaluation index because it is affected by the treatment, size of the bone production tract, fetal size, and fetal well-being, among others; it does not merely evaluate cervical ripening. This study examined the correlation between cervical elastography and pelvic examination findings in the third trimester. In addition, the significance of cervical elastography for predicting the onset of spontaneous labor was demonstrated.
Results
The relationship between the Bishop score and the number of days
First, we examined the relationship between the Bishop score and the number of days until the onset of spontaneous labor. The highest recorded Bishop score was 8 points. We divided the Bishop score into three groups: 0–2 points, 3–5 points, and 6–8 points. After examining the incidence of spontaneous labor within 7 days from the pelvic examination, we determined that those with a higher Bishop score tended to have a higher rate of spontaneous labor onset. There was a significant difference at 37 and 39 weeks of gestation (p = 0.01 and p = 0.02, respectively; Fig. 1). In addition, when examining the number of days from the pelvic examination to the onset of spontaneous labor, not limited to 7 days, higher Bishop scores tended to be associated with the onset of labor, particularly at the 39th week of pregnancy (p = 0.0007, Supplementary Figure S1).
Elastography and scoring of pelvic examination findings
The correlation between cervical elastography and its internal findings was examined by Spearman’s correlation. In the total 769 tests, the correlations between the Bishop score, stiffness, dilatation, effacement, and elastography were strong (r = 0.46, 0.30, 0.39, and 0.46, respectively), and the correlations between position and station with elastography were weak (r = 0.08, 0.10, respectively) (Table 1).
When examined by week, the cervical elastography findings were positively correlated with the Bishop score, stiffness, dilatation, and effacement (r = 0.24 ~ 0.51), but there was only a weak correlation with position and station at any week (r = − 0.07 ~ 0.11) (Table 1).
When examining each ultrasonic model separately for VOLUSONS6 (January 2017 to May 2018) and ARIETTA 60 (June 2018 to December 2018), both showed that the Bishop score, stiffness, dilatation, and effacement were strongly correlated with elastography (all r > 0.30), but position and station were only weakly correlated with elastography (all r < 0.20) (Table 1).
Comparison of the number of days from the examination date to the onset of natural labor
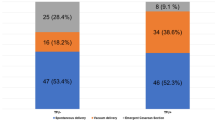
We investigated whether the Bishop score performed from 36 to 40 weeks of pregnancy (classified as scores of 0–2, 3–5, and 6–8) correlated with the onset of spontaneous labor within 7 days after the exam. Only at week 39, there was a significant difference between the three groups between the Bishop scores (p = 0.02, Fig. 2).
We also investigated which cervical elastography out of those performed from 36 to 40 weeks of pregnancy was correlated with the onset of spontaneous labor.
The relationship between cervical elastography and the incidence of spontaneous labor within 7 days of the examination showed that labor tended to occur earlier in the soft tissue group at 39 weeks of gestation, and a significant difference was noted among the three groups: the rate of labor onset was 80% in the soft tissue group and 40% in the medium-hard tissue and hard tissue groups at seven days after 39 gestational weeks (p = 0.0004, Fig. 3). At 40 weeks, the rate of spontaneous labor onset within 7 days also tended to be high, but there was no significant difference (p = 0.08, Fig. 3). Similarly, when examining the number of days from the exams to spontaneous labor onset, not limited to 7 days, labor onset occurred significantly earlier in the soft tissue group than in the medium-hard tissue or hard tissue groups, but this finding was only observed at 39 weeks gestation (p = 0.001, Supplementary Figure S2).
When analyzing the incidence of spontaneous labor onset within 7 days of the examination at the 39th week of pregnancy, divided into primiparas and multiparas, labor onset appeared early when the elastography findings were classified as soft tissue, regardless of primiparas and multiparas. A statistically significant difference was observed (p = 0.04 and p = 0.03, respectively, Fig. 4).
We analyzed the association between cervical elastography findings at 39 weeks and the rate of onset of labor within 1 week, stratified by the Bishop score. At Bishop scores of 3–5 and 6–8, soft tissue elastography displayed a significantly increased rate within 7 days (p = 0.0007 and p = 0.03, respectively, Fig. 5).
Association between cervical elastography at 39 weeks of gestation and the incidence of spontaneous labor within 7 days after the exam. (A) Bishop score 0–2, (B) Bishop score 3–5, (C) Bishop score 6–8. Palatal axis; cumulative spontaneous labor onset rate. Horizontal axis: days since the inspection.
The rate of the occurrence of spontaneous labor within 7 days from the 39-week pregnancy test was high in both VOLUSONS6 and ARIETTA60 compared to the soft tissue group and the hard tissue + medium-hard tissue group (p = 0.03 and p = 0.07, respectively; Supplementary Figure S3).
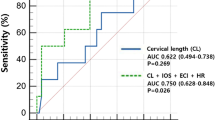
We performed a multivariate analysis using the Cox proportional hazard model to assess age, height, weight, BMI at the time of the examination at 39 gestational weeks, primipara vs. multipara, Bishop score (0–2 vs. 3–5 vs. 6–8), and elastography (hard tissue vs. medium-hard tissue vs. soft tissue) (Table 2). We found that the Bishop score (HR 1.81, 95% CI 1.40–2.34, p < 0.0001) and elastography (HR 1.86, 95% CI 1.46–2.35, p < 0.0001) were independently related to labor onset rate within 1 week after the examination.
Even in cases where cervical ripening was considered favorable based on elastography and the Bishop score, there were cases in which a cesarean section was performed due to fetal dysfunction or cephalopelvic disproportion. Therefore, no significant correlation was observed between elastography and the vaginal delivery rate (data not shown).
Discussion
Although shear wave elastography using acoustic radiation force impulse (ARFI) has recently been developed as a method of elastography, the use of ARFI on the gestational uterus is not acceptable in Japan due to concerns about the safety of the fetus9,10. Therefore, strain elastography was used in this study. A qualitative assessment of cervical elastography by color has been reported11,12,13, but an attempt has recently been reported to quantitatively assess one area of the cervical canal as a strain ratio by comparing it with other areas, in order to determine its association with pregnancy outcome14. At the start of the present study, an attempt was also made to assess quantitative elastography. However, the results were not reproducible between different examiners (data not shown). To date, most cervical elastography studies have been reported as data from one or two examiners14, and validation of the interobserver variation was considered inadequate. Therefore, in the present study, we assessed the endometrium by color, similar to the method reported by Wozniak et al.13. This simple method had very little interobserver variation, and all six of the testers had consistent results within the first five rounds. A study15 involving seven centers and 602 patients to evaluate thyroid nodules by strain elastography also conducted a qualitative evaluation by color, and at the moment, qualitative evaluation by color might be the method that is less prone to interobserver variation problems and is easier to apply clinically.
Some articles have highlighted the usefulness of cervical elastography for the prediction of the preterm birth rate13,16,17, and others have discussed the relationship between cervical elastography before labor induction and the success rate of transvaginal delivery18,19. However, some authors have questioned the usefulness of cervical elastography during pregnancy14. We believe that preterm birth rates and success rates of vaginal delivery are easy-to-understand indicators of clinical benefit, but they are affected by factors other than cervical ripening, such as treatment, bony birth canal, and fetal status. In addition, those studies include bias because physicians know the results of cervical elastography and then perform the preterm birth treatment or made the delivery-style decision. Thus, whether cervical elastography can be a truly reliable test to determine the degree of cervical ripening has not yet been fully evaluated. One of the reasons why the value of cervical elastography is questioned is that the cervix is rarely biopsied during pregnancy, making it impossible to directly examine whether cervical elastography is correlated with histological cervical ripening findings. Therefore, in this study, we decided to compare cervical elastography with the Bishop score at term and the time to spontaneous labor.
Dilatation, station, and position in pregnancy pelvic examinations have been reported to be correlated with dilatation, fetal head-perineum distance, and posterior cervical angle by transvaginal ultrasonography, respectively20, but no direct comparison of cervical elastography and pelvic findings during pregnancy has been reported. We found that cervical elastography during pregnancy was strongly correlated with cervical stiffness at pelvic examination (Table 1). This result was not affected by the difference in the ultrasonic model, and our results show the reliability of cervical elastography. Interestingly, cervical elastography was strongly correlated with effacement and dilation but weakly correlated with station and position. This indicates that cervical elastography is more strongly correlated with factors that indicate cervical ripening than factors that indicate fetal position.
In this study, we have shown that cervical elastography can predict the time of onset of spontaneous labor, and cervical elastography at 39 weeks of pregnancy is correlated with the incidence of spontaneous labor within 7 days after the test, regardless of whether the woman is primipara or multipara for the first time (Figs. 3 and 4). We also found that adding cervical elastography to the Bishop score at 39 weeks gestation can be useful for predicting the incidence of spontaneous labor (Fig. 5). This result is thought to occur because only information on the surface can be obtained through palpation, while information on the hardness inside the cervical canal is added by performing elastography. Panelli et al. reported that women with > 1-cm dilation were more likely to experience spontaneous labor than those with < 1-cm dilation at 39 weeks21. Rozenberg et al. reported that the Bishop score, ultrasonographic measurement of cervical length, and fetal fibronectin are valuable for predicting the onset of spontaneous labor within 7 days between 39 weeks 4 days gestation and 40 weeks 3 days gestation22. These reports support our findings that predicting the onset of spontaneous labor from cervical ripening was possible only at 39 weeks. Limitations include: (1) a relatively small sample size; (2) the instrument changed midway through although the same trend was obtained; and (iii) the elastography was evaluated qualitatively and could not be analyzed as precisely as the cut-off setting by strain ratio.
In conclusion, we directly compared cervical elastography with the Bishop score and evaluated its significance using the bias-free index of the time to the onset of spontaneous labor at term. We have shown that cervical elastography at 39 weeks of gestation is useful for predicting the onset of spontaneous labor. Predicting the time of the onset of spontaneous labor is helpful in preparing for and planning scheduled deliveries. A limitation of this study is that the sample size is relatively small. Thus, to incorporate the results of this study as a standard clinical method in the future, a prospective study with a greater sample size is now required.
Materials and methods
Patients
The subjects included 147 primiparas and 91 multiparas who delivered at our hospital during the 2 years from January 2017 to December 2018. Sixteen additional cases were added in July 2020 to assess the reproducibility of elastography. Informed consent was obtained from all subjects with the approval of our ethics committee. This study was approved by the Institutional Review Board of Kindai University Faculty of Medicine (28–180). All research was performed in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects.
A pelvic examination was conducted at weekly pregnancy checkups from 36 to 40 weeks of gestation, and elastography was used to evaluate cervical stiffness by transvaginal ultrasonography. From 2017 to 2018, a total of 769 examinations were performed by Y.Y., M.S., R.S., K.Y., R.F., and A.S. Before starting this study, Y.Y. and M.S. performed elastography examinations together using a transvaginal probe in ten pregnant women to ensure that the results in the same case were stable and consistent with each other. Subsequently, when R.S., K.Y., R.F., and A.S. participated in the study, they (also together with Y.Y. or M.S.) performed elastography examinations using a transvaginal probe on five or more pregnant women to ensure that the results in the same case were consistently obtained and that the results were consistent across examiners. It was also confirmed that there was no difference in the results between examiners when the ultrasonic equipment was changed. In addition, in July 2020, we examined the concordance rate of elastography assessments between Y.Y. and M.S., R.S., or K.Y. in 16 cases. The number of observed agreements was 88%, and the weighted Kappa value was 0.862 (Supplementary Table S1)23.
The inclusion criteria were cases in which the management of pregnancy and delivery was performed at our department after 36 weeks. Exclusion criteria included patients diagnosed with threatened preterm labor by 36 weeks and treated with ritodrine hydrochloride or magnesium sulfate, and/or patients with multiple pregnancies.
Elastography and scoring of pelvic examination findings
Until May of 2018, VOLUSONS6 (GE Healthcare, Japan, Tokyo) was used, and beginning in June of 2018, ARIETTA60 (Hitachi, Tokyo) was used to replace the ultrasonic equipment at the facility. Both are strain elastography devices.
Elastography was qualitatively assessed by color. First, a transvaginal probe was placed on the anterior surface of the cervix as a lithotripsy with the bladder emptied, and a sagittal section of the cervix was obtained. The mucosa in the cervix was drawn using an echo along the length of the cervix. The probe was moved approximately one centimeter four to five times, and the cycle of compression and decompression was repeated. The region of interest was determined by the dominant color of the cervical gland as a whole and at 1 cm in diameter on the side of the inner uterus, according to the manufacturer’s protocol, with a pressure indicator bar (VOLUSONS6) and a waveform display (ARIETTA60).
In VOLUSONS6, green indicates hard tissue, yellow indicates medium-hard tissue, and red indicates soft tissue (Fig. 1). In ARIETTA60, blue indicates hard tissue, green indicates medium-hard tissue, and red indicates soft tissue. Elastography was assessed using the qualitative results.
To perform Spearman rank correlation analysis, the numbers zero for hard tissue, 1 for medium-hard tissue, and 2 for soft tissue were used.
Stiffness was not measured numerically among the findings of the pelvic examination; thus, it was quantified as follows: zero for hardness, 1 for moderate, and 2 for soft. Furthermore, the position of the cervix was quantified numerically: zero for posterior, 1 for the middle, and 2 for anterior. The effacement (%), dilation (cm), station (cm), and Bishop score1 of the pelvic examination findings were used as their actual values. The correlation between elastography and the pelvic examination findings from the same examination were analyzed using a Spearman’s correlation (Table 1).
Comparison of the number of days from the examination date to the onset of natural labor
In Japan, pregnancy screening is performed weekly after 36 weeks of pregnancy24. In this study, we analyzed the incidence of spontaneous labor within 7 days after the examination, starting at the consultation between 36 and 40 weeks. Among the cases without spontaneous labor, the cases in which labor was induced were treated as censored (i.e., no event) at the beginning of labor induction. Similarly, the cases in which a cesarean section was performed (without spontaneous labor) were treated as censored at the start of the cesarean section.
Statistical analysis
Spearman’s correlation coefficient was used for the correlation analysis between the elastography and pelvic findings, which included stiffness, hardness, effacement, dilatation, station, and the Bishop score. The Kaplan–Meier curve approach was used to estimate the rate of cumulative spontaneous labor (Figs. 2, 3, 4 and 5), and the log-rank test was performed to compare the groups stratified by elastography findings (hard tissue, medium-hard tissue, or soft tissue) and the Bishop score (0–2, 3–5, or 6–8).
Also, to identify the factors involved in the time to labor onset, variates such as maternal age, height, weight (at the time of examination), and BMI were treated as continuous variables, obstetrical history (primipara vs. multipara) was treated as a dichotomous variable, and the Bishop scores (0–2 vs. 3–5 vs. 6–8) were treated as scale variables, which were generally known as maternal factors. Clinical findings associated with the time to labor onset were applied to the univariate Cox proportional hazards model along with the color from the elastography. Then, we calculated the hazard ratios (HRs), which indicated the ratio of labor onset rate per unit of time or per change or per unit of variable or across groups. To consider the confounding factors, the covariates described above were applied to the multivariate Cox proportional hazards model to examine the association with the color from the elastography in regard to the time to labor onset (after these covariates were adjusted).
The analysis using the Cox proportional hazard model was performed using R version 3.5.3 (https://www.R-project.org/). Other statistical analyses were performed using Prism Version 6.0 (GraphPad Software, San Diego). A p-value of < 0.05 was considered statistically significant.
References
Bishop, E.H. Pelvic scoring for elective induction. Obstet. Gynecol. 24, 266–268 (1964).
Akgul, Y., Holt, R., Mummert, M., Word, A. & Mahendroo, M. Dynamic changes in cervical glycosaminoglycan composition during normal pregnancy and preterm birth. Endocrinology 153, 3493–3503 (2012).
Yoshida, K., et al. Quantitative evaluation of collagen crosslinks and corresponding tensile mechanical properties in mouse cervical tissue during normal pregnancy. PLoS One. 9,e112391. https://doi.org/https://doi.org/10.1371/journal.pone.0112391 (2014).
Breuiller-Fouche, M. & Germain, G. Gene and protein expression in the myometrium in pregnancy and labor. Reproduction 131, 837–850 (2006).
Agarwal, S., Agarwal, A., Joon, P., Saraswat, S. & Chandak, S. Fetal adrenal gland biometry and cervical elastography as predictors of preterm birth: a comparative study. Ultrasound. 26, 54–62 (2018).
Su, Y. et al. Evaluation of cervical cancer detection with acoustic radiation force impulse ultrasound imaging. Exp. Ther. Med. 5, 1715–1719 (2013).
Agarwal, A., Agarwal, S. & Chandak, S. Role of acoustic radiation force impulse and shear wave velocity in prediction of preterm birth: a prospective study. Acta Radiol. 59, 755–762 (2018).
Gultekin, S. et al. Comparison of elastosonography and digital examination of cervix for consistency to predict successful vaginal delivery after induction of labor with oxytocin. J. Matern. Fetal Neonatal Med. 30, 2795–2799 (2017).
Issaoui, M. et al. Shear wave elastography safety in fetus: a quantitative health risk assessment. Interv Imaging. 99, 519–524 (2018).
Kudo, M. The Japan Society of Ultrasonics in Medicine. https://www.jsum.or.jp/committee/uesc/pdf/ARFI_Safety.pdf [Effects of ultrasound with acoustic radiation force impulses on tissue (written in Japanese)].
Yamaguchi, S., Kamei, Y., Kozuma, S. & Taketani, Y. Tissue elastography imaging of the uterine cervix during pregnancy. J. Med. Ultrason. 2001(34), 209–210 (2007).
Swiatkowska-Freund, M. & Preis, K. Elastography of the uterine cervix: implications for success of induction of labor. Ultrasound. Obstet. Gynecol. 38, 52–56 (2011).
Wozniak, S. et al. Elastography in predicting preterm delivery in asymptomatic, low-risk women: a prospective observational study. BMC Pregnancy Childbirth. 14, 238 (2014).
Fruscalzo, A., Mazza, E., Feltovich, H. & Schmitz, R. Cervical elastography during pregnancy: a critical review of current approaches with a focus on controversies and limitations. J. Med. Ultrason. 2001(43), 493–504 (2016).
Friedrich-Rust, M. et al. Evaluation of strain elastography for differentiation of thyroid nodules: results of a prospective DEGUM multicenter study. Ultraschall Med. 37, 262–270 (2016).
von Schöning, D. et al. Cervical sonoelastography for improving prediction of preterm birth compared with cervical length measurement and fetal fibronectin test. J. Perinat. Med. 43, 531–536 (2015).
Oturina, V. et al. Assessment of cervical elastography strain pattern and its association with preterm birth. J. Perinat. Med. 45, 925–932 (2017).
Gultekin, S. et al. Comparison of elastosonography and digital examination of cervix for consistency to predict successful vaginal delivery after induction of labor with oxytocin. J. Matern. Fetal. Neonatal Med. 30, 2795–2799 (2017).
Hwang, H. S., Sohn, I. S. & Kwon, H. S. Imaging analysis of cervical elastography for prediction of successful induction of labor at term. J. Ultrasound. Med. 32, 937–946 (2013).
Eggebø, T. M. et al. Can ultrasound measurements replace digitally assessed elements of the Bishop score?. Acta Obstet. Gynecol. Scand. 88, 325–331 (2009).
Panelli, D.M. et al. Using cervical dilation to predict labor onset: a tool for elective labor induction counseling. Am. J. Perinatol. 36, 1485–1491 (2019)
Rozenberg, P., Goffinet, F. & Hessabi, M. Comparison of the Bishop score, ultrasonographically measured cervical length, and fetal fibronectin assay in predicting time until delivery and type of delivery at term. Am. J. Obstet. Gynecol. 182, 108–113 (2000).
Landis, J. R. & Koch, G. G. The measurement of observer agreement for categorical data. Biometrics 33, 159–174 (1977).
Minakami, H. et al. Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2014 edition. J Obstet Gynaecol Res. 40, 1469–1499(2014)
Author information
Authors and Affiliations
Contributions
Y.Y., M.S., and Y.K. designed the study and prepared the manuscript draft. H.T. and N.M. contributed to analyzing the patients’ data as well as in drafting the manuscript. Y.Y., M.S., R.S., K.Y., R.F., and A.S. collected and interpreted the clinical data and conducted a comprehensive literature review related to this project. All authors thoroughly reviewed the manuscript. All authors read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yo, Y., Kotani, Y., Shiro, R. et al. Relationship between cervical elastography and spontaneous onset of labor. Sci Rep 10, 19685 (2020). https://doi.org/10.1038/s41598-020-76753-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-76753-4
This article is cited by
-
Advances in the clinical application of ultrasound elastography in uterine imaging
Insights into Imaging (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.