Abstract
The protective role of preoperative beta-blocker in patients undergoing non-cardiac surgery is unknown. We aimed to evaluate the effects of beta-blocker on perioperative myocardial injury in patients undergoing non-cardiac surgery. We consecutively enrolled 112 patients undergoing non-cardiac surgery. They were randomly allocated to receive bisoprolol or placebo given at least 2 days preoperatively and continued until 30 days after surgery. The primary outcome was incidence of perioperative myocardial injury defined by a rise of high-sensitive troponin-T (hs-TnT) more than 99th percentile of upper reference limit or a rise of hs-TnT more than 20% if baseline level is abnormal. Baseline characteristics were comparable between bisoprolol and placebo in randomized cohort Mean age was 62.5 ± 11.8 years and 76 (67.8%) of 112 patients were male. Among 112 patients, 49 (43.8%) underwent vascular surgery and 63 (56.2%) underwent thoracic surgery. The median duration of assigned treatment prior to surgery was 4 days (2–6 days). We did not demonstrate the significant difference in the incidence of perioperative myocardial injury [52.6% (30 of 57 patients) vs. 49.1% (27 of 55 patients), P = 0.706]. In addition, the incidence of intraoperative hypotension was higher in bisoprolol group than placebo group in patients undergoing non-cardiac surgery [70.2% (40 of 57 patients) vs. 47.3% (26 of 55 patients), P = 0.017]. We demonstrated that there was no statistically significant difference in perioperative myocardial injury observed between patients receiving bisoprolol and placebo who had undergone non-cardiac surgery.
Similar content being viewed by others
Introduction
Perioperative cardiac complications are of significant concern in patients undergoing non-cardiac surgery1. It has been shown that cardiac troponins have a high sensitivity and specificity in detecting myocardial injury. The prevalence of perioperative myocardial injury evaluated by high-sensitive troponin T (hs-TnT) was reported to be as high as 45% in patients undergoing non-cardiac surgery2. Previous studies have demonstrated that an elevated postoperative cardiac troponin level, irrespective of clinical symptoms, is associated with high risk of short-term and long-term major cardiovascular events and cardiovascular death3. Therefore, prevention of a perioperative myocardial injury is essential to improve the overall postoperative outcomes.
Beta-blocker has been described as a potential measure to prevent perioperative myocardial injury. Previous animal study has shown that early administration of metoprolol after ST-segment elevation myocardial infarction (STEMI) could diminish the progression of ischemic injury4. This finding was confirmed in randomized human study which demonstrated that intravenous metoprolol administration in patients with anterior STEMI improved ECG markers of myocardial ischemia before reperfusion5. The precise mechanism by which beta-blocker decreases perioperative myocardial ischemia has been proposed. Beta-blocker improves oxygen balance of myocardium by negative inotropic effect and the reduction in blood pressure and heart rate. Furthermore, beta-blocker may attenuate the risk for plaque rupture by decreasing circumferential stress on the atherosclerotic plaques6,7. Previous study have shown that patients receiving bisoprolol at least 7 days before the intermediate-risk surgery had a significant decrease in 30-day nonfatal myocardial infarction and cardiovascular mortality8. However, POISE study has shown that perioperative high-dose metoprolol beginning within 24 h prior to non-cardiac surgery is associated with the increased risk of bradycardia, hypotension, stroke and mortality9. With this regard, international guidelines state that beta-blocker treatment is not advised to start within one day before the surgery10,11. The optimal duration of beta-blockers given before the surgery and their benefits, in patients at intermediate or high surgery risk, have not been clearly elucidated. It has been suggested by the guidelines that starting beta-blocker more than 1 day may be considered10,11, despite the unclear benefit of short-term of beta-blocker12,13. Previous cohort studies have shown that short-term beta-blocker given less than 1 week before surgery may be harmful12,13. Nevertheless, no randomized control trials have been conducted to clarify this issue. The European perioperative guideline suggested bisoprolol or atenolol if beta-blocker is considered before the surgery based on observational studies10,14. Therefore, we aimed to investigate whether the short-term oral bisoprolol given at least 2 days preoperatively could prevent myocardial injury after surgery in patients undergoing non-cardiac surgery as compared to placebo.
Materials and methods
Study populations
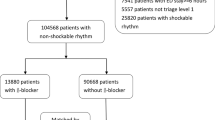
The present study was a randomized, prospective, double-blinded, placebo-controlled trial performed at Maharaj Nakorn Chiang Mai Hospital, Chiang Mai University. The study was approved by the ethics committee of the Faculty of Medicine, Chiang Mai University (MED-2558-03128) and registered on 29/03/2018 to http://www.clinicaltrials.in.th/ which submission number TCTR20180329005. The investigations were carried out in accordance with the Declaration of Helsinki, including written informed consent of all participants. During a period of November 2012 to January 2017, we had prospectively enrolled 112 consecutive patients, aged more than 18 years (Fig. 1), who underwent elective non-cardiac thoracic or vascular surgery. Informed consent was attained from each patient to take part in the study. The treatment allocation was done by block of four-randomization. To ensure the blinding situation during the trial, the research assistance performed randomization and assigned patients to intervention. The primary care team including surgeons, anesthesiologists, nurses; and patients were blinded from study treatment allocation. The medication was delivered to the patients by the blinded nurses. The outcome of the studies were assessed by the investigators who were unaware of the assigned treatment. All the biomarkers were tested immediately after sampling. The results of all the biomarkers were reported to the primary care surgeons. The management of the myocardial infarction and stroke after surgery were left at the discretion of the primary care team.
Bisoprolol tablets were purchased from Maharaj Nakorn Chiang Mai hospital. Placebo tablets were provided by Department of Pharmaceutical Sciences, Faculty of Pharmacy, Chiang Mai University. One bisoprolol tablet contained 2.5 mg of bisoprolol. The placebo tablet was made from maize starch with comparable appearance to bisoprolol tablet.
The enrolled patients were randomly assigned to receive bisoprolol or placebo given at least 2 days preoperatively and continued until 30 days after surgery. The patients were excluded if they had been taking beta-blockers, had contraindication of the use of beta-blockers including asthma, acute decompensated heart failure, second or third degree AV block, had baseline resting heart rate (HR) < 60 beats per minute (bpm), had baseline systolic blood pressure (SBP) < 100 mmHg, had plan to use beta–blocker before surgery or during the first 30 postoperative days for other reasons, had concurrent use of verapamil, diltiazem or amiodarone, urgent or emergency surgery within 24 h, refused to participate in the randomized study.
Bisoprolol was started at the dose of 2.5 mg orally per day (1.25 mg per day if left ventricular ejection fraction was less than 40%)15. During hospitalization, resting heart rate was daily evaluated and the dose of assigned drug was adjusted with stages of 1.25 or 2.5 mg per day. The maximum dose was 10 mg per day, targeting at a heart rate of 50 to 70 bpm. The same dose of studied drug was maintained if HR 50–69 bpm and/or SBP 90–99 mmHg. A 1.25 mg of studied drug was added if HR 70–80 bpm and/or SBP 100–119 mmHg. A 2.5 mg of studied drug was added if HR ≥ 81 bpm and SBP ≥ 120 mmHg. The administration of studied drug was temporarily stopped if any of the following occurred; systolic blood pressure less than 90 mmHg, resting heart rate less than 50 bpm, heart failure or bronchospasm, PR interval ≥ 0.30 s, second or third degree atrioventricular block.
An electrocardiograph (ECG) (HP M1700A, Hewlett Packard, Palo Alto, CA, USA) was recorded before surgery and on the first, second, and third and 30th days after surgery. The hs-TnT level was measured before surgery and on the first, second, and third days after surgery. The level of N-terminal-pro B-type natriuretic peptide (NT-proBNP) and high-sensitive C-reactive protein (hs-CRP) was also assessed before and after surgery. An echocardiography (Phillips Sonos 7500 Ultrosounds) was performed at baseline before surgery to evaluate left ventricular ejection fraction (LVEF). LVEF were measured using modified biplane Simpson’s methods. NT-proBNP and hs-TnT were evaluated with electrochemiluminescence immunoassay by using the Cobas e601 system (Roche Diagnostics). The detection limit of hs-TnT was 3 ng/L, a cut-off point at 99th percentile was 14 ng/L, and a coefficient of variation of less than 10% was at 13 ng/L. The analytical measurement range of NT-proBNP was 5–35,000 pg/mL. Hs-CRP was assessed with particle-enhanced immunoturbidimetric assay by using the Cobas c502 system (Roche Diagnostic) with an analytical measurement range of 0.15–20 mg/L.
The outcomes were determined by 2 independent cardiologists who were blinded to treatment allocation. The study protocol was approved by Institutional Review Board of Faculty of Medicine, Chiang Mai University.
The primary endpoint of our study was the incidence of perioperative myocardial injury that occurred within 3 days after surgery. The secondary endpoints of the study were the incidence of perioperative myocardial infarction, postoperative stroke or all-cause death that occurred within 30 days after surgery.
Definitions
-
Perioperative myocardial injury was defined as a rise of hs-TnT more than the 99th percentile of the upper reference limit or a rise of hs-TnT more than 20% if baseline level is elevated (> 14 ng/L)16.
-
The diagnosis of myocardial infarction required at least two of the followings16.
-
(1)
Chest pain (angina symptom) lasting more than 20 min.
-
(2)
ECG alterations including acute ST-segment elevation followed by appearance of Q waves or loss of R waves, or new left bundle branch block, or new ST segment depression, or new persistent T wave inversion for at least 24 h, which sustains for at least 24 h.
-
(3)
A positive hs-TnT measurement with characteristic rise and fall.
-
(1)
-
Non-cardiac thoracic surgery is defined as the procedure to diagnosis and therapy of the diseased conditions of the trachea, lungs, esophagus and mediastinum include by thoracotomy or video-assisted thoracic surgery.
-
Non-cardiac vascular surgery is defined as the vascular surgery including percutaneous vascular intervention except arteriovenous shunt and vein stripping procedures.
-
Revised cardiac risk index comprised five variables including the history of coronary artery disease, heart failure, diabetes currently taking insulin therapy, preoperative serum creatinine more than 2.0 mg/dL or glomerular filtration rate less than 60 mL/min and history of transient ischemic attack or stroke10,11,17.
-
Intraoperative hypotension is defined as systolic blood pressure less than 90 mmHg during surgery18,19.
Statistical analysis
All analyses were done on the modified intention to treat basis, excluding the randomized patients who neither underwent surgery nor had hs-TnT levels after surgery. Demographic and perioperative variables were compared between groups with a t test for normally distributed values; otherwise, the Mann–Whitney U test was used. Proportions were compared by Chi-square test or Fisher exact test when appropriate. Repeated measures analysis of variance was used to compare the differences of hs-TnT level, heart rate and blood pressure before and after surgery. Continuous variables with normal distribution were presented as means ± standard deviation. Results with non-normal distribution are expressed as median ± interquartile range. The Kolmogorov–Smirnov test was used to assess normality of the data. Categorical variables were displayed as percentages. A probability values < 0.05 (2-tailed) was considered significant. Hazard ratios (HRs) and 95% confidence intervals (CIs) to assess the risk of the primary end point according to potential confounding variables were determined by logistic regression.
Sample size calculation
We calculated the sample size at the power of 80% with level of statistical significant at 95%. The incidence of perioperative myocardial injury (hs-TnT ≥ 14 ng/L) was estimated at 50%2. We estimated a 50% relative risk reduction associated with bisoprolol therapy8,20. The estimated total sample size was 116 patients (58 patients in each group). We initially enrolled a total of 118 patients in the study. However, 6 patients were excluded due to the cancellation of surgery and the lack of hs-TnT data. In this regard, a total of 112 patients who had the preoperative and postoperative hs-TnT data were included in the final modified intention to treat analysis as mentioned above (Fig. 1).
Results
We prospectively enrolled 112 consecutive patients who underwent elective non-cardiac surgery and met inclusion criteria in the present study. Baseline characteristics were comparable between bisoprolol and placebo, with respect to age, gender, comorbidities, concomitant medications, and type of surgery. The mean age was 62.5 ± 11.8 years in bisoprolol group and 64.4 ± 13.1 years in placebo group. The majority of patients (70.2%) group had no clinical risk factors according to revised cardiac risk index (RCRI). Only 7 (6.3%) patients had more than 1 RCRI (Tables 1, 2). Among 112 patients, 49 (43.8%) underwent vascular surgery and 63 (56.2%) underwent thoracic surgery. The patient’s risk status was also assessed by American Society of Anesthesiologists Physical Status Classification System (ASA scores). Majority of the patients in both groups had ASA score I and II, indicating the low-risk status of studied population (Table 1).
The median duration of preoperative bisoprolol and placebo therapy was 3 ± 4 days and 4 ± 2 days, respectively (P = 0.669). The mean dose of bisoprolol before surgery was 4.7 ± 2.6 mg. Among patients receiving bisoprolol, the mean heart rate decreased from 80 ± 12 bpm at baseline to 75 ± 12 bpm on operative day. It then increased to 81 ± 11 bpm, 82 ± 10 bpm and 80 ± 11 bpm on the first, second and third day after surgery (P = 0.008). On the contrary, in patients receiving placebo, the mean heart rate increased from 79 ± 10 bpm at baseline to 83 ± 15 bpm on the operative day, then continued to increase to 86 ± 13 bpm, 86 ± 15 bpm and 85 ± 11 bpm on the first, second and third day after surgery (P = 0.003). Compared between bisoprolol and placebo, the heart rate on operative day and postoperative day 1–3 was significantly lower in bisoprolol group (Fig. 2).
The effect of bisoprolol on heart rate during perioperative period compared to placebo. Among patient receiving bisoprolol (solid line), the mean heart rate was significantly reduced on operative day compared to baseline. It then significantly increased after surgery. On the contrary, in patients receiving placebo (dashed line), the mean heart rate increased on the operative day, the continued to increase after surgery. The heart rate on operative day and postoperative day 1–3 was significantly lower in bisoprolol group. *Statistically significant P < 0.05, compared to placebo.
The significantly lower systolic blood pressure after surgery compared to baseline was observed in both bisoprolol and placebo groups. Among patients receiving bisoprolol, the mean systolic blood pressure decreased from 125 ± 17 mmHg at baseline to 120 ± 15 mmHg on operative day. It then continued to decrease to 117 ± 14 mmHg, 117 ± 16 mmHg and 117 ± 14 mmHg on the first, second and third day after surgery (P < 0.001). Similarly, in patients receiving placebo, the mean systolic blood pressure decreased from 130 ± 17 mmHg at baseline to 126 ± 14 mmHg on operative day. It then decreased to 121 ± 20 mmHg, 123 ± 19 mmHg and 119 ± 18 mmHg on the first, second and third day after surgery (P < 0.001).When compared between 2 groups, the systolic blood pressure on operative day was significantly lower in bisoprolol compared to placebo (Fig. 3).
The effects of bisoprolol on systolic blood pressure during perioperative period compared to placebo. The systolic blood pressure was significantly reduced after surgery compared to baseline in both bisoprolol (solid line), and placebo (dashed line) groups. When compared between 2 groups, the systolic blood pressure on operative day was significantly lower in bisoprolol compared to placebo. *Statistically significant P < 0.05, compared to placebo.
We demonstrated that incidence of perioperative myocardial injury did not differ between patients receiving bisoprolol and placebo [52.6% (30 of 57 patients) vs. 49.1% (27 of 55 patients), P = 0.706, respectively]. Figure 4 shows the median hs-TnT level before and after surgery between bisoprolol and placebo groups. The median postoperative hs-TnT level was not different between 2 groups. Among 31 patients with elevated baseline hs-TnT level, 9 of 15 (60%) patients in bisoprolol group and 12 of 16 (75%) patients in placebo group developed perioperative myocardial injury (P = 0.458). Of 81 patients with normal baseline hs-TnT level, there was also no difference of perioperative myocardial injury between bisoprolol and placebo groups [50.0% (21 of 42 patients) vs. 38.5% (15 of 39 patients), P = 0.372, respectively]. Four of 57 patients in bisoprolol group and two of 55 patients in placebo group developed perioperative myocardial infarction (7.0% vs. 3.6%, P = 0.679). Only one patient in bisoprolol group died during hospitalization due to sepsis. No stroke occurred in both groups of patients. In addition, preoperative and postoperative levels of hs-TnT, hs-CRP and NT-BNP were comparable between bisoprolol and placebo groups.
Incidence of serious adverse events and drug discontinuation was not different between bisoprolol and placebo groups (Table 3). However, the incidence of intraoperative hypotension was significantly higher in bisoprolol group than placebo group [70.2% (40 of 57 patients) vs. 47.3% (26 of 55 patients), P = 0.017].
Discussion
Perioperative cardiac complications increase the risk of short-term and long-term morbidity and mortality in patients undergoing non-cardiac surgery and remain a significant concern in this group of patients. Nevertheless, the detection of myocardial infarction occurring after surgery has become a challenge due to the presence of postoperative analgesic agent that may obscure the ischemic symptoms. In addition, the high prevalence of ECG abnormalities in patients after non-cardiac surgery has made ECG findings less specific in the diagnosis of myocardial infarction. Several investigators have shown that the elevation of perioperative troponin level, irrespective of symptoms, is associated with increased risk of death at 30 days21. As a result, perioperative myocardial injury detected by the elevation of perioperative troponin level can be a predictor of adverse postoperative outcomes.
POISE study has shown that beta blocker started within 24 h or less before non-cardiac surgery decreases risk of nonfatal myocardial infarction but increases risk of bradycardia, hypotension, stroke, and mortality9. Perioperative mortality in patients randomized to metoprolol succinate was associated with perioperative bradycardia, hypotension, and stroke. The use of a high dose of metoprolol without dose titration in POISE study may lead to higher risk of perioperative hypotension. On the contrary, DECREASE-IV study has demonstrated that the patients receiving bisoprolol at least 7 days before surgery (an average of 34 days before surgery) had a significant reduction in 30-day cardiovascular death and nonfatal myocardial infarction8. However, the validity of the results from DECREASE trials led by Poldermans has been scrutinized because of concerns about scientific misconduct.
The meta-analysis by Bouri et al. which excluded all DECREASE trials showed the significant 27% increase in mortality from the initiation of perioperative beta-blocker22. However, all the trials in this meta-analysis initiated beta-blocker within 1 day or less prior to surgery. As the evidence pointed out toward the harmful effect of high-dose beta-blocker started within 24 h or less before the surgery, beta-blocker started within 24 h before non-cardiac surgery is discouraged by international guidelines10,11.
A series of meta-analyses showed the conflicting outcomes on the safety and efficacy of pre-operative beta-blockers7,22,23,24. Nevertheless, their findings were relatively consistent in demonstrating that the use of perioperative beta-blockers had significant harmful associations with bradycardia, hypotension and stroke. However, they could reduce perioperative myocardial infarction. The systematic review by Wijeysundera and colleagues demonstrated that without the controversial DECREASE studies, there were insufficient data on beta-blocker started 2 or more days prior to surgery7. With this regard, the 2014 AHA/ACC guidelines have stated that it may be reasonable to begin perioperative beta-blockers long enough in advance to assess safety and tolerability, preferably more than 1 day before surgery as a class IIb indication. In addition, they have stated that in patients with intermediate- or high-risk preoperative tests, it may be reasonable to begin beta-blockers as a class IIb indication. They concluded that randomized control trials were needed to address this knowledge gap7,11. Aside from the controversial DECREASE trials, to the best of our knowledge, our study is the first randomized controlled trial to examine the effect of beta-blocker given more than 1 day before surgery in patients undergoing non-cardiac thoracic and vascular surgery.
In the present study, we demonstrated that there was no statistically significant difference in perioperative myocardial injury and myocardial infarction between patients receiving short-term beta-blocker and those receiving placebo who had undergone non-cardiac surgery. Of importance, we observed the higher incidence of intraoperative hypotension in bisoprolol group. This may suggest the possible harmful effect of short-term beta-blocker, similar to those observed in the POISE study9.
At the time of the enrollment, the international guidelines stated that perioperative beta-blocker was discouraged in patients undergoing the low-risk surgery. Therefore, in this study, we enrolled only patients scheduled for elective non-cardiac thoracic and vascular surgery which was considered as the intermediate- and high-risk surgery. We did not exclude the low-risk patients with 0 revised cardiac risk index from our study due to the fact that the effect of perioperative beta-blocker in low-risk population had not been elucidated at the time of study start.
The majority of patients in our study had no clinical risk factors regarding revised cardiac risk index. Results of our study are in accordance with the observational data obtained by Jørgensen et al. The investigators have demonstrated the possible harmful effect of perioperative beta-blocker in patients with 0–1 RCRI25,26. In this regard, our findings reinforce the possible harmful effect of perioperative beta-blocker in low-risk patients, irrespective of the risk of surgery.
Nevertheless, the potential benefit of longer duration of beta-blocker and in higher-risk population is still unknown. The preventive effect of beta-blocker on the coronary plaque rupture may require some times to develop. It has been described that prolonged beta-blocker treatment decreases inflammatory cytokines and impedes coronary atherosclerosis progression. Previous study has demonstrated the preferential neutrophil stunning by metoprolol which may reduce coronary microvascular obstruction27. As a result, the duration of preoperative beta-blocker may affect the postoperative outcomes.
The different beta-blockers may have different effects on perioperative myocardial injury. Previous animal study demonstrated that only metoprolol, but not atenolol or propranolol, reduced infarct size and inflammation a rat model of MI28. Furthermore, beta-blockers which exert ancillary cardioprotective properties such as carvedilol through alpha 1-adrenoceptor blockade and antineutrophil and antioxidative actions, or nebivolol which enhances nitric oxide signalling may have additional benefit on cardioprotection29. Importantly, the interference of co-morbidities and co-medications with cardioprotection has been established30. Therefore, these confounders of cardioprotection may attenuate the potential benefit of beta-blocker in patients undergoing non-cardiac injury.
In addition, it has been demonstrated that discontinuation of beta-blocker treatment early after surgery correlates with higher risk of 1-year death compared with patients not using beta-blockers31. Therefore, it is crucial to continue beta-blocker in patients with pre-existing beta-blocker therapy.
The major limitation of the present study was the small sample size of the studied population and the inadequate statistical power to exclude a Type II error. The calculated sample size of 116 patients was insufficient because we overestimated the benefit of preoperative bisoprolol, based on DECREASE trials which are currently considered as the scientific misconduct studies8,20. The sample size of nearly 4000 patients are needed to declare the difference between 2 groups with adequate statistical power. Therefore, the results of the study should be interpreted with caution. In addition, our studied population had high baseline hs-TnT, NT-proBNP and hs-CRP despite the relatively low RCRI. The high level of these biomarkers usually indicate the high risk population with multiple co-morbidities. It is possible that the co-morbidities in our patients might have been underreported or underdiagnosed. Also, the interpretation of changes in troponin levels in the post-operative period, can be quite challenging such as presence of renal dysfunction after surgery. Furthermore, it is not clear whether the effect of bisoprolol used in our studied population can be applied to other beta blockers.
Conclusions
We demonstrated that there was no statistically significant difference in perioperative myocardial injury observed between patients receiving bisoprolol and placebo who had undergone non-cardiac thoracic or vascular surgery. In addition, the incidence of intraoperative hypotension was higher in bisoprolol group than placebo group in patients undergoing non-cardiac surgery.
Data availability
The informed consent given by Effects of short-term bisoprolol on perioperative myocardial injury in patients undergoing non-cardiac surgery: a randomized control study does not cover data posting in public databases. However, data are available upon request from Effects of short-term bisoprolol on perioperative myocardial injury in patients undergoing non-cardiac surgery: a randomized control study should be sent to arintaya.p@cmu.ac.th and are subject to approval by the Faculty of Medicine, Chiang Mai University Ethics Committee.
References
Weiser, T. G. et al. An estimation of the global volume of surgery: A modelling strategy based on available data. Lancet 372, 139–144. https://doi.org/10.1016/S0140-6736(08)60878-8 (2008).
Kavsak, P. A. et al. High sensitivity troponin T concentrations in patients undergoing noncardiac surgery: A prospective cohort study. Clin. Biochem. 44, 1021–1024. https://doi.org/10.1016/j.clinbiochem.2011.05.017 (2011).
Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA 307, 2295–2304. https://doi.org/10.1001/jama.2012.5502 (2012).
Lobo-Gonzalez, M. et al. Metoprolol blunts the time-dependent progression of infarct size. Basic Res. Cardiol. 115, 55. https://doi.org/10.1007/s00395-020-0812-4 (2020).
Diaz-Munoz, R. et al. Intravenous metoprolol during ongoing STEMI ameliorates markers of ischemic injury: A METOCARD-CNIC trial electrocardiographic study. Basic Res. Cardiol. 116, 45. https://doi.org/10.1007/s00395-021-00884-6 (2021).
Priebe, H. J. Triggers of perioperative myocardial ischaemia and infarction. Br. J. Anaesth. 93, 9–20. https://doi.org/10.1093/bja/aeh147 (2004).
Wijeysundera, D. N. et al. Perioperative beta blockade in noncardiac surgery: A systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130, 2246–2264. https://doi.org/10.1161/CIR.0000000000000104 (2014).
Dunkelgrun, M. et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: A randomized controlled trial (DECREASE-IV). Ann. Surg. 249, 921–926. https://doi.org/10.1097/SLA.0b013e3181a77d00 (2009).
POISE Study Group et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): A randomised controlled trial. Lancet 371, 1839–1847. https://doi.org/10.1016/S0140-6736(08)60601-7 (2008).
Kristensen, S. D. et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: Cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: Cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur. Heart J. 35, 2383–2431. https://doi.org/10.1093/eurheartj/ehu282 (2014).
Fleisher, L. A. et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130, e278-333. https://doi.org/10.1161/CIR.0000000000000106 (2014).
Flu, W. J. et al. Timing of pre-operative Beta-blocker treatment in vascular surgery patients: Influence on post-operative outcome. J. Am. Coll. Cardiol 56, 1922–1929. https://doi.org/10.1016/j.jacc.2010.05.056 (2010).
Wijeysundera, D. N. et al. Duration of preoperative beta-blockade and outcomes after major elective noncardiac surgery. Can. J. Cardiol. 30, 217–223. https://doi.org/10.1016/j.cjca.2013.10.011 (2014).
Ashes, C. et al. Selective beta1-antagonism with bisoprolol is associated with fewer postoperative strokes than atenolol or metoprolol: A single-center cohort study of 44,092 consecutive patients. Anesthesiology 119, 777–787. https://doi.org/10.1097/ALN.0b013e3182a17f12 (2013).
CIBIS II investigators. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): A randomised trial. Lancet 353, 9–13 (1999).
Thygesen, K. et al. Fourth universal definition of myocardial infarction. J. Am. Coll. Cardiol. 72, 2231–2264. https://doi.org/10.1016/j.jacc.2018.08.1038 (2018).
Lee, T. H. et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 100, 1043–1049 (1999).
Franck, M. et al. Documented intraoperative hypotension according to the three most common definitions does not match the application of antihypotensive medication. J. Int. Med. Res. 39, 846–856. https://doi.org/10.1177/147323001103900318 (2011).
Bijker, J. B. et al. Incidence of intraoperative hypotension as a function of the chosen definition: Literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 107, 213–220. https://doi.org/10.1097/01.anes.0000270724.40897.8e (2007).
Poldermans, D. et al. The effect of bisoprolol on perioperative mortality and myocardial infarction in high-risk patients undergoing vascular surgery. Dutch Echocardiographic Cardiac Risk evaluation applying stress echocardiography study group. N. Engl. J. Med. 341, 1789–1794. https://doi.org/10.1056/NEJM199912093412402 (1999).
Botto, F. et al. Myocardial injury after noncardiac surgery: A large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 120, 564–578. https://doi.org/10.1097/ALN.0000000000000113 (2014).
Bouri, S., Shun-Shin, M. J., Cole, G. D., Mayet, J. & Francis, D. P. Meta-analysis of secure randomised controlled trials of beta-blockade to prevent perioperative death in non-cardiac surgery. Heart 100, 456–464. https://doi.org/10.1136/heartjnl-2013-304262 (2014).
Schouten, O. et al. A meta-analysis of safety and effectiveness of perioperative beta-blocker use for the prevention of cardiac events in different types of noncardiac surgery. Coron Artery Dis. 17, 173–179. https://doi.org/10.1097/00019501-200603000-00012 (2006).
Talati, R. et al. Outcomes of perioperative beta-blockade in patients undergoing noncardiac surgery: A meta-analysis. Ann. Pharmacother. 43, 1181–1188. https://doi.org/10.1345/aph.1L706 (2009).
Jorgensen, M. E. et al. beta-blocker-associated risks in patients with uncomplicated Hypertension undergoing noncardiac surgery. JAMA Intern. Med. 175, 1923–1931. https://doi.org/10.1001/jamainternmed.2015.5346 (2015).
Jorgensen, M. E., Andersson, C., Venkatesan, S. & Sanders, R. D. Beta-blockers in noncardiac surgery: Did observational studies put us back on safe ground? Br. J. Anaesth. 121, 16–25. https://doi.org/10.1016/j.bja.2018.02.004 (2018).
Heusch, G. Coronary microvascular obstruction: The new frontier in cardioprotection. Basic Res. Cardiol. 114, 45. https://doi.org/10.1007/s00395-019-0756-8 (2019).
Clemente-Moragon, A. et al. Metoprolol exerts a non-class effect against ischaemia-reperfusion injury by abrogating exacerbated inflammation. Eur. Heart J. 41, 4425–4440. https://doi.org/10.1093/eurheartj/ehaa733 (2020).
Heusch, G. & Kleinbongard, P. Is metoprolol more cardioprotective than other beta-blockers? Eur. Heart J. 41, 4441–4443. https://doi.org/10.1093/eurheartj/ehaa764 (2020).
Kleinbongard, P., Botker, H. E., Ovize, M., Hausenloy, D. J. & Heusch, G. Co-morbidities and co-medications as confounders of cardioprotection-Does it matter in the clinical setting? Br. J. Pharmacol. 177, 5252–5269. https://doi.org/10.1111/bph.14839 (2020).
van Lier, F. et al. Impact of prophylactic beta-blocker therapy to prevent stroke after noncardiac surgery. Am. J. Cardiol. 105, 43–47. https://doi.org/10.1016/j.amjcard.2009.08.646 (2010).
Acknowledgements
This work was supported by Grants from the Thailand Research Fund MRG RSA5780039 (W.W.), MRG RSA5780040 (A.P.), and the Faculty of Medicine Endowment Fund for medical research (29/2557), Chiang Mai University, Thailand (W.W., A.P.). Κ.R. was supported by Chiang Mai University. All the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
W.W. designed study, recruited patients, performed the statistical analyses, evaluated the results and drafted the paper. T.C., K.C., A.T., S.S., S.A. and K.R. collected the data and contributed substantially to data preparation and quality assurance. A.P. participated in the conception and design of the study revised the paper for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wongcharoen, W., Chotayaporn, T., Chutikhongchalermroj, K. et al. Effects of short-term bisoprolol on perioperative myocardial injury in patients undergoing non-cardiac surgery: a randomized control study. Sci Rep 11, 22006 (2021). https://doi.org/10.1038/s41598-021-01365-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01365-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.