Abstract
Our objective was to quantify the differences in the outcomes from childhood bacterial meningitis (BM) and to describe the factors associated with them in different parts of the world. This study is a secondary analysis of prospectively collected data from five clinical BM trials conducted in Finland, Latin America (LatAm), and Angola between 1984 and 2017. As all data were collected uniformly, direct comparison of the series was possible. Associations between patient characteristics and death or dismal outcome—the triad of death, severe neurological sequelae, or deafness—were explored. In all, data on 2123 children with BM were analyzed. Etiology was confirmed in 95%, 83%, and 64%, in Finland, LatAm and Angola, respectively. The leading agents were Haemophilus influenzae, Streptococcus pneumoniae, and Neisseria meningitidis. Dismal outcome was the end result for 54%, 31%, and 5% of children in Angola, LatAm, and Finland, respectively. Although underweight, anemia, and tardy arrival worsened prognoses in Angola and LatAm, it was the presenting condition that was central in terms of outcome. In multivariate analysis, the factors independently associated with dismal outcome were the study site (Angola vs. Finland, OR 11.91, 95% CI 5.54–25.63, p < 0.0001 or LatAm vs. Finland, OR 9.46, 95% CI 4.35–20.61, p < 0.0001), Glasgow Coma Score < 13 (OR 4.58, 95% CI 3.31–6.32, p < 0.0001), seizures (OR 1.96, 95% CI 1.43–2.69), age < 1 year (OR 1.55, 95% CI 1.13–2.14, p = 0.007), and pneumococcal etiology (OR 1.49, 95% CI 1.08–2.06, p = 0.015). Greatly dissimilar outcomes from BM reflected the findings on admission on all three continents. Optimizing growth, preventing anemia, and prompt treatment may improve outcomes in resource poor areas.
Similar content being viewed by others

Introduction
Despite effective Haemophilus influenzae type b (Hib), Streptococcus pneumoniae, and Neisseria meningitidis vaccinations in many countries, bacterial meningitis (BM) remains a major problem in children across the world1. It is the 10th most common cause of death among those under 5 years old, with around 150.000 succumbing from BM annually2. Unfavorable outcomes are especially common in Africa3 and Latin America (LatAm)4. The topicality of BM is by no means over.
With the aim of easing the burden of childhood BM using treatments sufficiently straightforward to deploy in resource-poor settings, our group has carried out five large, prospective randomized trials on three continents. The then new third-generation cephalosporins were first compared with chloramphenicol and ampicillin in Finland in 1984–19915. No major difference in performance was found.
In the second trial ceftriaxone was used, mainly because it is simple to administer. This study focused on the adjuvant dexamethasone versus oral glycerol6, an agent used to reduce increased intracranial pressure especially after neurosurgery7,8. Glycerol showed encouraging effects, but the study had to be curtailed as the Hib polysaccharide9 and conjugate10 vaccines arrived to eliminate the leading agent of pediatric BM in Finland11. Nevertheless, those two studies included 351 cases.
The third trial was carried out in six countries of LatAm (Argentina, Brazil, Dominican Republic, Ecuador, Paraguay, and Venezuela) in 1995–200312,13,14. The main lesson from the largest (N 654) ever randomized BM study performed at the time was that severe neurological sequelae were prevented with glycerol (in recipients 15/276 vs. non-recipients 29/273, odds ratio 0.5, p 0.02), but not with dexamethasone alone12. This important observation obliged us ethically to use glycerol as adjuvant in our subsequent trials.
Finally, two studies with a total of 1118 patients took place in Luanda, Angola, in 2005–201715,16,17. In the first study cefotaxime was given by bolus or slow infusion, with participants also receiving concomitantly, at random, oral acetaminophen (paracetamol), or placebo. Our interest in paracetamol was raised by positive effects obtained in bacteremic adult patients18. The series of 723 children15 showed highly significant benefit with the regimen of oral paracetamol plus cefotaxime infusion during six to 600 h from institution of therapy, but significance was lost afterwards. The second Angolan study on 375 patients17, in which a prolonged cefotaxime infusion plus paracetamol regimen was tested, failed to confirm these encouraging results.
These five prospective BM studies generated an exceptionally large dataset. Notwithstanding the prolonged timespan, having the same information on the same devastating disease in dissimilar conditions on three continents offered the possibility that overall analysis of this data would allow us to observe conclusive trends. Our hypothesis was that besides the children's general condition upon arrival at hospital, local conditions would play a major role in their prognosis.
Methods
Trial designs, participants, and diagnosis
The clinical trial data used in this manuscript has been published before5,6,12,15,17. The setup of each study has been detailed earlier5,6,12,15,17. In short, after approval of the protocol by the relevant Ethics Committees, children aged from two months to 15 years with symptoms and signs compatible with BM were included, after obtaining consent from the legal guardian. In case of illiteracy, a finger print was required. The study outline was explained to guardians by the attending physician. Using a computer-generated list, participants were randomized to different groups according to the protocol. All methods were carried out in accordance with the Declaration of Helsinki. After becoming a practice, the two Angolan studies were registered with the International Standard Randomized Controlled Trial Number Register, number ISRCTN62824827, 22 August 2005, and with ClinicalTrials.gov, identifier NCT 01540838, 29 February 2012, respectively. In Finland, the patients were enrolled between 30 October 1984 and 19 December 1986, and between 21 April 1987 and 11 November 1990, in LatAm between 10 January 1996 and 20 December 2003, and in Luanda between 18 July 2005 and 26 June 2008, and between 22 January 2012 and 21 January 2017.
While examining the patient, the on-call doctor assessed the child's condition using the age-adjusted Glasgow Coma Scale, performed a lumbar puncture, ordered pre-determined samples, instituted treatment according to the protocol, and began to complete the specially designed forms. The questionnaires were in Finnish, Spanish, or Portuguese, depending on the location. Basic bacteriology and chemistry were performed in local laboratories using standard techniques.
BM was deemed confirmed if (1) cerebrospinal fluid (CSF) culture proved positive, (2) patient showed compatible symptoms and signs and a positive blood culture, or (3) at least two of the following criteria were fulfilled: CSF leukocytes ≥ 100/mm3 (predominantly polymorphs), positive Gram stain, positive latex agglutination test, or serum C-reactive protein (CRP) ≥ 40 mg/Liter. Exclusion criteria were age less than two months, trauma, intracranial shunt, previous hearing impairment or neurological disease, and immunosuppression, except in potential HIV-infection (relevant mainly in Angola). Pretreatment antimicrobials prevented enrollment if more than one parenteral dose had been administered. Malnourishment was graded according to z-scores following WHO guidelines14.
Monitoring the disease, analysis of data
Data were compiled on the ward administering the treatment. The course of illness was monitored daily using the dedicated forms. Since consecutive CRP measurements offer a yardstick for monitoring BM19, CRP was quantified by at least day 4 (+/− 1 day), after which values exceeding 62 mg/l are associated with slow recovery and problems such as hearing impairment20. After the child was discharged from hospital, all data were sent to Finland to be digitized and analyzed.
Outcomes were assessed at discharge. Between uneventful recovery and death as the extreme outcomes there were further categories: survival with mild hearing deficit (better ear threshold 41–79 dB), deafness (threshold ≥ 80 dB), and mild or severe neurological sequelae. Sequelae were deemed mild if the patient showed any abnormality, such as hemiparesis, monoparesis, psychomotor retardation, or ataxia, whereas severe sequelae included blindness, quadriplegia/paresis, hydrocephalus requiring a shunt, or severe psychomotor retardation. Finally, the triad of severe neurological sequelae, deafness, or death comprised a dismal outcome. All these categories are summarized in the footnote of Table 1. The best available audiological techniques were used, with traditional audiometry recommended. For small children, brain evoked response audiometry (BERA) was the preferred method of choice.
All data were computed and analyzed using JMP ® Pro 14.1.0 (SAS Institute Inc, Cary, NC, USA) for Windows. Contingency analysis was used to examine relationships between two categorial variables, and Pearson´s chi-square test to calculate p values. Associations with continuous characteristics were assessed using One-Way Anova. We used nominal logistic analysis and calculated odds ratios (OR) with 95% confidence intervals (95% CI) for death and dismal outcome. For multivariate analysis of prognostic factors, we used clinical characteristics that in univariate analysis showed p value < 0.0001.
Ethics approval
All the studies were approved by the relevant Ethics Committees or the Hospitals’ Board. The children were enrolled after their guardian´s informed consent was obtained.
Results
Patient characteristics on arrival
The total number of cases was 2123, of which 1597 (75%) were confirmed bacteriologically. The Finnish series comprised 351 (confirmed 334, 95%) cases, the LatAm series 654 (543, 83%) cases, and the two trials in Angola 1118 (720, 64%) cases. Genders presented fairly evenly overall: 56% were boys and 44% girls. Also, the age distribution of the three series was rather similar, except that while the majority in LatAm and Angola were infants, the one-year-olds slightly preponderated in Finland (p < 0.0001).
Table 1 characterizes the patients by 21 covariates and outcomes. There were significant differences between the sites, except in gender distribution (p = 0.69). Altered consciousness, an important signal of degree of inflammation in the central nervous system, was recorded in 71–76% across the series (p = 0.048). Regarding the Glasgow Coma Scale scores, levels under 13, which indicates severe disease, were shown by 40–41% of patients in Finland and LatAm vs. by 58% of those in Angola (p < 0.0001).
Some characteristics in Table 1 deserve further attention. Median time with symptoms and signs suggestive of commencing or overt BM was 4.0 (quartile 2.0–7.0) days overall, though this varied significantly from 1.2 (0.8–2.0) days in Finland, to 3.0 (2.1–5.0) days in LatAm, and 5.0 (3.0–7.0) days in Angola (p < 0.0001). Pretreatment antibiotics had been given to 18% of children in Finland compared to 36% in LatAm and 43% in Angola (p < 0.0001). The agents used were mostly oral β-lactams, such as amoxicillin (data not shown).
Anemia was common in Angola and LatAm. A median hemoglobin level of 8.5 g/dL was not achieved by 67% of Angolan and 35% of LatAm patients, compared to just one percent in Finland (p < 0.0001). A similar trend was observed in the weight for age z-score of below -2, which suggests at least moderate underweight. This was the case for 31% of children in Angola, 13% in LatAm and 3% in Finland (p < 0.0001).
In Angola, 57 (8%) of 737 children had positive HIV antibody test result. Malaria thick film was positive in 29% (311/1055) of Angolan children. In Latin America and Finland there were no known cases with HIV or malaria.
Findings during treatment, outcomes
Etiology reflected the continent (Table 1). Initially, Hib was the leading causative agent in Finland and LatAm, with 218 (65%) of 334 bacteriologically identified cases vs. 243 (45%) of 543 cases, respectively. In Angola, H. influenzae was not invariably typed, but once done, Hib predominated overwhelmingly. There S. pneumoniae dominated with 334 (46%) of the 720 confirmed cases. N. meningitidis ranked second in Finland and third in LatAm and Angola, the respective case numbers being 80, 115, and 90.
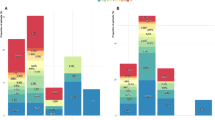
A change in etiology occurred over time. The year of BM diagnosis was earlier for patients with H. influenzae or N. meningitidis than for patients with S. pneumoniae or other bacteria (p < 0.0001). This was the case also when all the areas were analyzed separately (p < 0.001). Figure 1 shows etiology in the three series as a function of age.
The highest CRP values around day four were observed in Angola (p < 0.0001) (Table 1). This was an omen of the poorer outcomes there20. Length of hospital stay did not differ greatly, the median being 11 days in Angola and Finland vs. 8 days in LatAm (p < 0.0001).
Overall, 524 (25%) children died, one-quarter of the entire series, the percentages being 3, 13, and 38 in Finland, LatAm, and Angola, respectively (p < 0.0001). Of the total 1599 survivors, 1234 (77%) were fully neurologically and audiologically examined, of whom only 569 (46%) recovered uneventfully, whereas 441 (36%) survived with mild, and 224 (18%) with severe sequelae. In Finland the respective figures were 226/297 (76%), 67 (23%) and 4 (1%); in LatAm 230/460 (50%), 154 (33%), and 76 (17%); and in Angola 113/477 (24%), 220 (46%), and 144 (30%) (p < 0.0001). Figure 2 summarizes the overall outcomes at the three investigation sites. There were major differences between North and South in terms of uneventful recovery and death.
Total deafness, a daunting disorder especially for a child in the developing world, hit 10–11% of those in Angola and LatAm, compared to none in Finland (p < 0.0001). Similarly, 15–8% of patients in Angola and LatAm were left with severe neurological sequelae vs. one percent in Finland (p < 0.0001). Dismal outcome (death, severe neurological sequelae, or deafness) was the fate of 54%, 31%, and 5% of patients in Angola, LatAm, and Finland, respectively (p < 0.0001) (Table 1).
Figure 3 shows the outcomes of 1435 children site-wise. Pneumococcal meningitis was especially deleterious in Angola, with a fatality rate of 41% (137/334), vs. 22% (31/144) in LatAm and 4% (1/27) in Finland (p < 0.0001). The overall mortality from pneumococcal meningitis was 33% (169/505).
Associations with death and dismal outcome
Children scoring low on the Glasgow Coma Scale, and those seizing at arrival or with a seizure history showed the highest risk of succumbing (Table 2). For scores under 13, the odds ratios were 4.21, 6.57, and 4.23, in Finland, LatAm and Angola, respectively. Similarly, for children having seizure prior to or on admission, the odds ratios were 8.88, 3.50, and 2.37, respectively.
In LatAm and Angola, underweight, late arrival, and pretreatment antibiotics also associated with higher mortality. With a weight/age z-score below -2, the odds ratio was 2.60 in LatAm vs. 1.48 in Africa. Having been ill for more than three days increased the odds ratio to 2.47 vs. 2.06, whereas pretreatment antibiotics increased the odds ratio to 1.21 vs. 1.42, respectively. Among the Finnish children, underweight, late arrival, or pretreatment antibiotics did not associate with death (wide 95%, CIs crossed 1). Controversially, age under one year increased fatality in LatAm, while it decreased it in Angola (OR 1.93 vs. 0.77). Anemia with hemoglobin less than 8.5 g/dl increased mortality in LatAm (OR 2.14).
Compared to death, the odds for dismal outcome were somewhat differentiated. While seizures increased the odds for dismal outcome in all sites (OR 6.87 in Finland, 3.33 in LatAm and 2.76 in Angola), in Finland a low Glasgow Coma score lost its significance, whereas weight/age z-score gained in significance. S. pneumoniae meningitis and anemia increased dismal outcome in LatAm and Angola, but not in Finland (OR in LatAm and Angola in pneumococcal meningitis 1.97 and 1.52; and when hemoglobin was < 8.5 g/dl 2.60 and 1.28).
Table 3 shows a multivariate regression analysis of prognostics factors for death and dismal outcome including study site as a categorical variable on the whole series. Study site, GCS < 13, seizures, and pneumococcal etiology were independent predictors of death. Study site, GCS < 13, seizures, age < 1 year, and pneumococcal etiology associated independently with dismal outcome.
In Angola, the outcome of the small group of HIV positive children did not differ from the outcome of children with negative HIV test. Neither did the result of the malaria test affect the outcome.
Discussion
The motive for our five trials that formed the study data was to improve prognosis of BM by modifying treatment. Since no real change in outcomes was observed, except for the notable finding of a significant reduction of severe neurological sequelae with glycerol in LatAm12, the accumulated dataset could be scrutinized as one, despite the treatments not being exactly the same. The long timespan may be seen as problematic, but a caveat is warranted: to our knowledge only one industrialized vs. non-industrialized country comparison on childhood BM has ever been published before21. So what conclusions can be drawn from our material?
First, no less than 11 of the 13 patient characteristics at arrival (Table 1) not only varied significantly between the sites, but most of them also associated with the outcomes. Altered consciousness was frequently observed across all series and demonstrated that children with BM generally arrived clinically very ill. More patients in Angola than LatAm scored under 13 on the Glasgow Scale, while the body temperature in Africa was lower. One may query whether widely used antibiotics in Luanda had already mitigated the disease, or if severe underweight in a third of the Angolan children had retarded adequate host response. For better or worse, dismal outcome was the sad fate for 54% of children in Angola, 31% in LatAm, and 5% in Finland—truly a somber finding. That seizures link to both death and dismal outcome is a lesser-known risk, whereas underweight14, delayed arrival16, and scoring low on the Glasgow Scale13 are among the recognized hazards for poor outcomes.
Second, three agents, Hib, S. pneumoniae and N. meningitidis held the same leading positions on all continents until vaccinations sharply reduced the role of Hib and pneumococci, first in Finland11 and a few years later in LatAm and Angola22,23. Since the African meningitis belt does not extend to Angola, an effective group A meningococcal conjugate24 has not been deployed there. Even fewer reasons for its use have been found in LatAm or Finland.
Third, pneumococcal meningitis was unsurprisingly more devastating than Hib or meningococcal meningitis (Fig. 3). However, our earlier analysis13 showed that more than etiology per se, it was the child's presenting condition that predicted the outcomes of BM. Since S. pneumoniae triggers a fierce inflammatory response25, pneumococcal meningitis often leads to terrible consequences. This would happen with any agent that caused an equally violent host response.
Fourth, tardy arrival to hospital worsened outcomes, especially in Angola, where median delay was five days, and a week not uncommon. This is almost incredible for such a life-threatening and often rapidly progressing disease as BM. Median delay in LatAm was three days, which is still longer than in Finland where patients usually arrived within 24 h or so. Interestingly, the pre-hospital duration of signs suggesting BM does not necessarily relate to outcome. In our group's earlier study on 325 patients from Finland26, no less than 26% of children had been sent home after a doctor's examination. Their outcomes did, however, not differ from the patients with swift diagnosis, no matter whether the delay had been 1 day, or 2 to 4 days.
Fifth, the negative effect of underweight, and to a slightly lesser extent of anemia, on dismal outcome were clear; obviously the lower the hemoglobin level, the poorer the outcome. Furthermore, AIDS, sickle cell disease, and parasitic infections are widely acknowledged problems, especially in Angola27,28. No wonder the risk of dying from BM in Malawi was five-fold compared to that in UK21.. Here it was four-fold between LatAm (13%) and Finland (3.4%), and 11-fold between Angola (38%) and Finland. Such differences are unacceptable.
Sixth, performance of antibiotics was compared only in our first study in Finland5, but it is notable that new antibiotics have not improved the prognosis of BM, except in cases of resistance. Inexpensive ampicillin, and to a great extent even chloramphenicol—agents from the 1960s—successfully challenged third-generation cephalosporins5. Thus, local resistance pattern allowing, inexpensive β-lactams are still valid choices for at least pneumococcal and meningococcal meningitis. Costly antibiotics should be used only when truly needed. This is good news for resource-poor settings, where the incidence of BM remains highest.
Our analysis has expected limitations. The very prolonged timespan of data collection was a problem, but the rather stable nature of BM disease, and the prospective and uniform data recording was unlikely to have materially distorted the information obtained. Underlying diseases were potential confounding factors, especially in Angola. Ideally, all patients would have had full clinical and audiological investigation, up to perhaps one year post-hospitalization, as some problems may abate over time29. In the prevailing circumstances, however, late follow-up visits were feasible only in Finland. One may also argue that Finland does not represent all of Europe, nor Angola the whole of Africa. We deem those countries to be good representatives of their continents, however, despite the inter-country differences that certainly exist. The generalizability of the results was broadest for LatAm because several countries participated in the study. In general, the generalizability of our results corresponded to the time periods of the data collection, and may differ according to social and epidemiological circumstances. All patients did not always have 100% of the results from the analyzed variables. Therefore, exact numbers are presented in the Tables. Missing results were few and occurred at random and thus did not constitute a systemic selection bias.
Five large prospective studies using similar data collection protocols carried out in Scandinavia, Latin America and Africa generated a dataset of 2123 cases. Despite profound dissimilarities between the sites in their economies, resources and community life overall, as well as in availability of and access to health care, the causative agents were much the same. However, significant differences prevailed in some prognostically pivotal issues, such as days of illness before arrival to hospital, pre-treatment antibiotic use, history of seizures, altered consciousness, scoring on the Glasgow Coma Scale, severe anemia, and being underweight, all these being most frequent in Angola. Here, the children performed worst, as all these factors are associated significantly with adverse outcomes. Dismal outcome, comprising the triad of full deafness, severe neurological sequelae, or death, was the fate of 40% of children overall: for 54% of those in Angola, 31% in Latin America, and 5% in Finland. Poor outcomes in BM and their clear associations with local conditions persist as a major problem in resource-deficient settings. Fortunately, we are not without weapons, and so the fight must continue.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
GBD. Neurology Collaborators (2019) Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18(5), 459–480 (2016).
GBD. Meningitis Collaborators (2018) Global, regional, and national, burden of meningitis 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 17(12), 1061–1082 (2016).
Peltola, H. Burden of meningitis and other severe bacterial infections of children in Africa: Implications for prevention. Clin. Infect. Dis. 31, 64–75 (2001).
Fink, E. L. et al. International survey of critically ill children with acute neurologic insults: The PANGEA study. Pediatr. Crit. Care Med. 18(4), 330–342 (2017).
Peltola, H., Anttila, M., Renkonen, O.-V. & The Finnish Study Group. Randomised comparison of chloramphenicol, ampicillin, cefotaxime and ceftriaxone for childhood bacterial meningitis. Lancet 1(8650), 1281–1287 (1989).
Kilpi, T. et al. Oral glycerol and intravenous dexamethasone in preventing neurologic and audiologic sequelae of childhood bacterial meningitis. Pediatr. Infect. Dis. J. 14(4), 270–278 (1995).
Cantore, G., Guidetti, B. & Virno, M. Oral glycerol for the reduction of intracranial pressure. J. Neurosurg. 21(4), 278–283 (1964).
Tourtelotte, W. W., Reinglass, J. L. & Newkirk, T. A. Cerebral dehydration action of glycerol. Clin. Pharmacol. Ther. 13(2), 159–171 (1972).
Peltola, H., Käyhty, H., Sivonen, A. & Mäkelä, P. H. Haemophilus influenzae type b capsular polysaccharide vaccine in children: A double-blind field study of 100,000 vaccinees 3 months to 5 years of age in Finland. Pediatrics 60(5), 730–737 (1977).
Eskola, J. et al. A randomized, prospective field trial of a conjugate vaccine in the protection of infants and young children against invasive Haemophilus influenzae type b disease. N. Engl. J. Med. 323(20), 1381–1387 (1990).
Peltola, H., Kilpi, T. & Anttila, M. Rapid disappearance of Haemophilus influenzae type b meningitis after routine childhood immunisation with conjugate vaccines. Lancet 340(8819), 592–594 (1992).
Peltola, H. et al. Adjuvant glycerol and/or dexamethasone to improve the outcomes of childhood bacterial meningitis: A prospective, randomized, double-blind, placebo-controlled trial. Clin. Infect. Dis. 45(10), 1277–1286 (2007).
Roine, I. et al. Influence of admission findings on death and neurological outcome from childhood bacterial meningitis. Clin. Infect. Dis. 46(8), 1248–1252 (2008).
Roine, I., Weisstaub, G., Peltola, H. & the LatAm Bacterial Meningitis Study Group. Influence of malnutrition on the course of childhood bacterial meningitis. Pediatr Infect Dis J 29(2), 122–125 (2010).
Pelkonen, T. et al. Slow initial β- lactam infusion and oral paracetamol to treat childhood bacterial meningitis: a randomised, controlled trial. Lancet Infect. Dis. 11(8), 613–621 (2011).
Pelkonen, T. et al. Risk factors for death and severe neurological sequelae in childhood bacterial meningitis in sub-Saharan Africa. Clin. Infect. Dis. 48(8), 1107–1110 (2009).
Savonius, O. et al. Extended continuous β-lactam infusion with oral acetaminophen in childhood bacterial meningitis: A randomised, double-blind clinical trial. Clin. Infect. Dis. 72(10), 1738–1744 (2021).
Kuikka, A. Factors associated with the outcome of bacteraemia during twenty years (1976–1996) with special reference to bacteraemias due to Streptococcus pneumoniae, Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa. Academic dissertation, University of Helsinki, Helsinki (83 p) (1999)
Peltola, H. C-reactive protein for rapid monitoring of infections of the central nervous system. Lancet 319(8279), 980–983 (1982).
Peltola, H., Pelkonen, T., Roine, I., Leite Cruzeiro, M. & Bernardino, L. Predicting outcome of childhood bacterial meningtis with a single measurement of C-reactive protein. Pediatr. Infect. Dis. J. 35(6), 617–621 (2016).
Molyneux, E., Riordan, F. A. I. & Walsh, A. Acute bacterial meningitis in children presenting to the Royal Liverpool Children’s Hospital, Liverpool, UK and the Queen Elizabeth Central Hospital in Blantyre, Malawi: a world of difference. Ann. Trop. Paediatr. 26(1), 29–37 (2006).
Peltola, H. et al. Vaccine-induced waning of Haemophilus influenzae empyema and meningitis in Angola. Emerg. Infect. Dis. 6(11), 1887–1890 (2014).
Urtti, S. et al. Surveillance of bacterial meningitis in an Angolan pediatric hospital after the introduction of pneumococcal conjugate vaccine. J. Global Health Rep. 3, e2019091 (2019).
Trotter, C. L. et al. Impact of MenAfriVac in nine countries of the African meningitis belt, 2010–15: an analysis of surveillance data. Lancet Infect Dis 17(8), 867–872 (2017).
Mook-Kanamori, B. B., Madelijn Geldhoff, M., van der Poll, T. & van de Beek, D. Pathogenesis and pathophysiology of pneumococcal meningitis. Clin. Microbiol. Rev. 24(3), 557–591 (2011).
Kallio, M. J. T., Kilpi, T., Anttila, M. & Peltola, H. The effect of a recent previous visit to a physician on outcome after childhood bacterial meningitis. JAMA 272(10), 787–791 (1994).
Sousa-Figueiredo, J. C. et al. Epidemiology of malaria, schistosomiasis, geohelminths, anemia and malnutrition in the context of a demographic surveillance system in northern Angola. PLoS ONE 7(4), e33189 (2012).
McGann, P. T. et al. A prospective newborn screening and treatment program for sickle cell anemia in Luanda Angola. Am. J. Hematol. 88(12), 984–989 (2013).
Roine, I. et al. Fluctuation in hearing thresholds during recovery from childhood bacterial meningitis. Pediatr. Infect. Dis. J. 33(3), 253–257 (2014).
Acknowledgements
We are indebted to so many colleagues and other collaborators in Finland, LatAm, and Angola, that listing all their names would be unfeasible. Therefore, a deep bow of gratitude to all of you, who certainly deserve it! Our thanks extend to the participating children's parents, who realized the importance of these studies.
Funding
The authors received no funding for this analysis. The original studies in Finland were funded with grants from the Paediatric Research Foundation, Helsinki, Finland. The study in LatAm was funded with grants from the Päivikki and Sakari Sohlberg Foundation, Helsinki; the Alfred Kordelin Foundation, Helsinki; the Sigfrid Jusélius Fundation, Helsinki. GlaxoSmithKline and Farmacia Ahumada donated glycerol and placebo preparations. Laboratorio de Chile partly donated ceftriaxone. The studies in Luanda were funded with grants from the Päivikki and Sakari Sohlberg; the Sigrid Jusélius; the Paediatric Research Foundation, the daily newspaper Helsingin Sanomat, Helsinki; Finska Läkaresällskapet, Helsinki; Stiftelsen Dorothea Olivia, Karl Walter och Jarl Walter Perkléns minne, Helsinki; and the Orion Research Foundation, Espoo, Finland.
Author information
Authors and Affiliations
Contributions
H.P. drafted the manuscript for intellectual content; major role in acquisition of data. I.R. major role in acquisition of data; revised the manuscript for intellectual content. M.K. major role in acquisition of data; revised the manuscript for intellectual content. T.P. major role in acquisition of data; analyzed the data; revised the manuscript for intellectual content.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peltola, H., Roine, I., Kallio, M. et al. Outcome of childhood bacterial meningitis on three continents. Sci Rep 11, 21593 (2021). https://doi.org/10.1038/s41598-021-01085-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01085-w
This article is cited by
-
Determinants of mortality among pediatric patients admitted to Wolaita Sodo University Comprehensive Specialized Hospital with acute bacterial meningitis, Southern Ethiopia: an unmatched case–control study
BMC Pediatrics (2023)
-
Clinical blindness in conjunction with childhood bacterial meningitis
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.